Abstract
Background
The increasing resistance of Acinetobacter baumannii to antibiotics has recently been regarded as a notable therapeutic difficulty. Evaluating resistance rates of some A. baumannii isolates to tetracyclines had an impact on understanding the antibiotic resistance dissemination. By comparing genetic characteristics and relatedness of A. baumannii isolates, we are able to determine the transition dynamics of outbreak isolates.
Methods
A total of 72 non-duplicate isolates of A. baumannii were recovered in 2011 and 2015 and minimum inhibitory concentration (MIC) range distribution of the isolates to tetracyclines was performed by broth micro dilution (BMD) assay, and to determine the lineage relatedness of the outbreak isolates repetitive extragenic palindromic element based on polymerase chain reaction (rep-PCR) and international clonal (ICs) investigations were performed.
Results
Resistance rates to tetracycline, doxycycline and minocycline in 2011 were 73, 2 and 0%, while these rates in 2015 increased up to 90, 84 and 52%, respectively. The tetB existed in 100% of all the isolates of both years. tetA was not found in any of the isolates. According to the rep-PCR assays, up to 83% of all isolates clustered distinctly and only 6% of isolates had a common root. The percentage rates of IC1 decreased from 42% in 2011 to 22% in 2015, while those of IC2 increased from 28 to 36%, from 2011 to 2015.
Conclusions
Our data showed that resistance to the first and second generations of tetracyclines is on the rise and the clonal transition dynamics of isolates are in progress in our hospital.
Similar content being viewed by others
Background
Acinetobacter baumannii as an opportunistic pathogen has recently been known as a nosocomial pathogen which is associated with health care infections [1]. Due to the increasing antimicrobial resistance, A. baumannii has emerged as a life-threatening pathogen in the three past decades. The most important mechanisms of resistance to tetracyclines in A. baumannii isolates are efflux pumps followed by ribosomal protections and enzymatic inactivation. To date, tetracyclines were considered as a second-line therapy for Acinetobacter infections. However, due to the lack of any new under-development antibiotics and decreased effectiveness of the first-line antibiotics, older ones (e.g. tetracyclines) have been taken into consideration again [2]. Streptomyces species were the source of tetracycline, which is considered as the first generation of tetracyclines. Semisynthetic tetracyclines, doxycycline and minocycline, as the second generation of this group have wider spectrum. Tigecycline, a glycylcycline, has recently approved by US Food and Drug Administration (FDA) antibacterial agent. This minocycline structural analogue is indicated intravenously for the treatment of complicated infections [3].
Resistance to the first and second generations of tetracyclines in A. baumannii isolates mainly resulted from the acquired major facilitator superfamily (MFS) efflux pumps, including tetA, tetB, tetG, tetH, tetL, and tet39, resistance nodulation division family (RND) efflux pumps nominated as adeABC, adeIJK, adeFGH, adeM, adeDE [4], and finally ribosomal protections and enzymatic inactivation [5]. tetA is responsible for the resistance to tetracycline and doxycycline whereas tetB has been found in the isolates that were also resistant to minocycline [6]. Notably, the main resistance mechanisms of tetracyclines are ade efflux systems while coexistence with tetA and tetB determinants resulted in increasing MIC values [7].
Due to the lack of accuracy in disc diffusion method, determining susceptibility to doxycycline and minocycline was recommended to be carried out by Epsilometric test (E-test) or broth microdilution assays [8].
Regarding the impact of A. baumannii in healthcare—associated infections and rapid spreading of antibiotic-resistant strains, epidemiological investigation and determination of the clonal relationships among A. baumannii isolates should be considered. Some molecular techniques are currently at our disposal for typing and to clonal relatedness among clinically isolates of A. baumannii. The most common assay is the repetitive extragenic palindromic polymerase chain reaction-based (rep-PCR) that is simple, rapid and reliable compared to PFGE. Determining international clonal lineages (ICs) in A. baumanii is a useful tool for showing widespread distribution of global distributed clones [9]. Outbreak strains which are more resistant to antibiotics and might be associated with specific clinical syndromes, could be identified by such aforementioned studies [10]. The present study aimed to compare the resistance range of tetracycline, doxycycline and minocycline in the two periods of 2011 and 2015. Moreover, resistance determinants tetA and tetB were screened in clinical isolates of A. baumannii. Also, to determine the clonal transition dynamics and relatedness of isolates, international clonal lineage investigation and rep-PCR assays were performed in Ghaem Hospital, Mashhad, Iran.
Methods
Bacterial isolates and hospital setting
A total of 72 non-duplicate isolates of carbapenem resistant A. baumannii (CRAB) were collected from admitted patients at the Intensive Care Units (ICUs) of Ghaem Hospital (1000-bed referral university hospital, with NICU, PICU and adult’s ICU wards). The ethics committee of hospital and institutional review boards approved this study, and recommendations by STROBE were considered to report the results [11]. Thirty-six isolates were collected in 2011, and the other 36 isolates were obtained in 2015. In the first stage, these isolates were identified by API20NE as Acinetobacter baumannii-calcoaceticus complex, and for confirming as A. baumannii, all of the isolates were investigated by OXA-51-like β-lactamase and gyrB multiplex PCR amplification according to previous studies [12]. The isolates were stored in 30% v/v glycerol/triptic soy broth medium at −70 °C.
Antibacterial susceptibility testing and efflux pump activity evaluation
In order to evaluate antimicrobial susceptibility to doxycycline, minocycline and tetracycline, broth micro dilution method was used according to CLSI M07-A9 instructions [13] and the results were interpreted according to CLSI M100-S25 guidelines [14]. In this study, the intermediate isolates were also considered as resistant. All antibiotic chemicals were purchased from Sigma Chemicals Co., Inc. (St. Louis, USA). Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were used as reference strains.
For tetracyclines resistant isolates, MICs of the three aforementioned antibacterials were repeated in the presence of the following efflux pump inhibitors (EPIs) by broth microdilution method. Carbonyl cyanide 3-chlorophenylhydrazone (CCCP), phenyl-arginine-β-naphthylamide (PAβN), 1-(1-naphthylmethyl)-piperazine (NMP), reserpine and verapamil (Sigma), CCCP, PAβN, NMP, reserpine, and verapamil were added to the broth at the final concentrations of 5, 70, 100, 50, and 100 g/L, respectively [4]. A fourfold or greater decrease in the MIC values in the presence of EPIs was considered as significant inhibition.
PCR amplification of tetA and tetB
The existence of tetracycline resistant determinants, tetA and tetB, were detected by the PCR assay according to previous studies with some modifications [15]. Briefly, the template DNA for PCR reactions was obtained from heating 200 μL suspension of overnight bacterial cultures for 10 min at 95 °C and quickly refrigerating for 10 min followed by centrifugation at 15,000g for 5 min, and then discarding the supernatant. PCR products were analyzed by electrophoresis on agarose gels 2% using a 100plus DNA ladder Fermentase (Thermo Fisher Scientific, Germany) as a size marker.
Clonal and international lineage relatedness
To discover clonal relationships among the isolates of A. baumannii, we exploited two molecular typing methods. All the isolates were subjected to rep-PCR and international clonal lineage (IC) investigations.
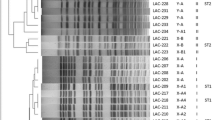
A pair of primers with indication for REP sequences of A. baumannii were used as amplification primers, as described previously. The concentration of REP primers, REP1 and REP2, were 50 pmol/mL [16]. PCR products were detected by electrophoresis on 2% agarose using a 100 bp plus DNA ladder (Thermo Fisher Scientific, Germany), as a size marker. GelJ software (v. 1.3) was utilized in order to analyze the band patterns, considering dice tolerance 2.0 and UPGMA method to depict dendrogram. Isolates with at least 95% similarity were considered related and defined as the same rep-PCR cluster. IC lineages detection was done by a multiplex PCR assay of all the strains to find csuE, OXA-66/69 and ompA genes [9].
Statistical study
All statistical analyses were performed using SPSS v.16.0. A univariate analysis was carried out using Pearson’s Chi square test for nominal variables in two independent groups. A P value of <0.05 was considered significant.
Results
Antimicrobial susceptibility and molecular detection of tetA and tetB
In two periods of 2011 and 2015, 72 CRAB isolates (36 isolates per year) were collected. The percentages of tetracyclines resistant isolates in 2015 were obviously higher than those in 2011. About 70% (26 of 36) of isolates in 2011 were resistant to tetracycline, while in 2015, the resistance rates were increased up to 90% (32 of 36). The increasing rates were also observed for doxycycline and minocycline. In 2011, 2.7% (1 of 36) of the isolates were resistant to doxycycline versus 84.2% (30 of 36) in 2015. None of the isolates were resistant to minocycline in 2011, but the resistance rate increased to 52.6% (19 of 36) after 4 years (Table 1).
MIC90 of minocycline, doxycycline and tetracycline were dramatically increased after passing 4 years (Fig. 1). MICs90 for minocycline, doxycycline and tetracycline in 2011 were 2, 4 and 32 mg/L, respectively, whereas in 2015 they obviously increased to 16, 64 and 1024 mg/L, respectively. The MICs of resistant isolate for these antibacterials in the presence of EPIs were significantly changed. About 88% of tetracycline resistant isolates (51 out of 58) showed decreasing MIC when tetracycline was presented with EPIs. The effect of EPIs on the MICs of doxycycline and minocycline resistant isolates (31 and 19 out of 72, respectively), was reduced in 26% (8 of 31) and 47% (9 of 19) of doxycycline and minocycline, respectively. The tetracycline resistance determinant tetB was detected in all of the isolates of both years, however, tetA was not found in any of the isolates.
Epidemiological investigations and international clonal lineages
About 10 distinctive rep-PCR clusters (named A to J) and eight singleton isolates were inferred from the band patterns (Fig. 2). Clusters A–E and G consisted of representatives of strains of 2011, and clusters H, I and J indicated strains of 2015. Cluster F consisted of strains of both years of 2011 and 2015. Our data showed that up to 94% of all the strains were included in nine distinct clusters and only 6% of them had common roots.
Results from Multiplex PCR revealed that 42% of strains in 2011 were IC1, 28% were IC2 and 30% were unknown, while only 22% of strains in 2015 were attributed to IC1, 36% to IC2 and 42% were unknown.
Discussion
This integrative study provides concerns about a formidable increase in drug resistance to A. baumannii concomitant with prospects to clonal transmission dynamics of outbreak isolates over a 4-year interval between 2011 and 2015.
Due to the increase in resistance to majority of antibiotics in A. baumannii, evaluating antimicrobial susceptibility of older agents that was not used in clinical practice is of interest to overcome the Acinetobacter infections. A previous study showed the satisfying effectiveness of tetracyclines against A. baumannii in vitro [15]. In this regard, our data showed that the resistance rates for tetracycline, doxycycline and minocycline in 2011 were 73, 2 and 0%, respectively. Meanwhile, these resistance rates increased to 90, 84.2 and 52.6% in the case of the noted antibiotics in 2015. Because of not using tetracyclines in clinical practice of A. baumannii infections in our hospitalized patients, the increased resistance to these three agents was not expected. Significant increasing resistance in our hospital setting is in correlation with another previous study in Iran [17]. Being consistent with our study, Maleki et al. reported that resistance rates of tetracycline, minocycline and doxycycline to A. baumannii isolates in Tehran in 2013 were 89, 35 and 25%, respectively.
The tetA and tetB determinants are common in tetracyclines resistant A. baumannii isolates [6]. Our results are also in agreement with a previous study by Farsiani et al. [18] in 2015 who reported that the tetA gene was not found in any of the strains whereas tetB was detected in 100% of the strains. In our study, the increased level of resistance to tetracyclines was observed in spite of any detectable differences in prevalence of tetA and tetB in all of the isolates. The effect of EPIs herein on most of the tetracycline resistant strains can explain that the increasing resistance is related to efflux pumps activity.
By using molecular typing methods, we are able to discriminates widespread clonal lineages of A. baumannii responsible for hospital clonal transition dynamics in outbreaks worldwide [19]. Amongst ten clusters obtained from evaluating all of the strains by rep-PCR, six clusters (A–E and G) included representatives of strains of 2011. The 2015 strains were classified in three clusters (H, I and J), and one cluster (F) contained strains of both years. At a glance, it can be inferred that more than 94% of all the strains were classified in distinct clusters and less than 6% of the strains are in a common (F) cluster. Furthermore, up to 91% of the strains in 2015 were classified in three clusters. Considering the decrease in the number of clusters from 2011 to 2015, it certainly indicated that new lineages with different resistance patterns were replaced over 4 years.
In this study, the percentage rates of IC1 and IC2 in the strains of 2011 were 42 and 28%, whereas in the strains of 2015 they were 22 and 36%, respectively. Higher prevalence of IC2 strains in 2015 compared with 2011, is consistent with the previous reports which state that in the recent years IC2 was a more common lineage in antibiotic-rich environments of hospitals [20]. A pervious study by Turton et al. [9] showed that IC1 strains have been prevalent in the past years. Therefore, it can be concluded that the clonal transition dynamics of strains in our hospital is in progress. The increased prevalence of IC2 in our hospital concomitant with elevated resistance to the first and second generations of tetracycline strengthens the fact that the IC 2 strains have higher resistance genetic determinants than IC1 strains. This consequence is in accordance with the previous study where IC 2 strains were relatively older than the other ICs which have been undergoing extensive diversification [21].
Conclusions
With the best of our knowledge, this study is the first comparison of clinical strains of CRAB strains in the same location in two periods in Iran. Our data indicates that despite not using tetracyclines in treatment of Acinetobacter infections, the increased resistance to tetracyclines is likely duo to the clonal transition dynamics of strains with replacement of IC2 clones which contain higher prevalence of resistance determinants. Molecular detection of tetracycline resistance determinants in our hospital is due to the other efflux pumps rather than tetA and tetB efflux pumps. Eventually, to overcome the increasing resistance to antibiotics, some prerequisites should be considered e.g., improving antibiotic stewardship programs (ASPs), hygienic surveillance programs, epidemiological study of outbreak strains, and concrete infection control.
References
Towner K. Acinetobacter: an old friend, but a new enemy. J Hosp Infect. 2009;73(4):355–63.
Viehman JA, Nguyen MH, Doi Y. Treatment options for carbapenem-resistant and extensively drug-resistant Acinetobacter baumannii infections. Drugs. 2014;74(12):1315–33.
Doan T-L, Fung HB, Mehta D, Riska PF. Tigecycline: a glycylcycline antimicrobial agent. Clin Ther. 2006;28(8):1079–106.
Deng M, Zhu MH, Li JJ, Bi S, Sheng ZK, Hu FS, et al. Molecular epidemiology and mechanisms of tigecycline resistance in clinical isolates of Acinetobacter baumannii from a Chinese University Hospital. Antimicrob Agents Chemother. 2014;58(1):297–303.
Chopra I, Roberts M. Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol Mol Biol Rev. 2001;65(2):232–60.
Marti S, Fernandez-Cuenca F, Pascual A, Ribera A, Rodriguez-Bano J, Bou G, et al. Prevalence of the tetA and tetB genes as mechanisms of resistance to tetracycline and minocycline in Acinetobacter baumannii clinical isolates. Enfermedades infecciosas y microbiología clínica. 2006;24(2):77.
Huys G, Cnockaert M, Vaneechoutte M, Woodford N, Nemec A, Dijkshoorn L, et al. Distribution of tetracycline resistance genes in genotypically related and unrelated multiresistant Acinetobacter baumannii strains from different European hospitals. Res Microbiol. 2005;156(3):348–55.
Wang P, Bowler SL, Kantz SF, Mettus RT, Guo Y, McElheny CL, et al. Comparison of minocycline susceptibility testing methods for carbapenem-resistant Acinetobacter baumannii. J Clin Microbiol. 2016;54:2937–41.
Turton J, Gabriel S, Valderrey C, Kaufmann M, Pitt T. Use of sequence-based typing and multiplex PCR to identify clonal lineages of outbreak strains of Acinetobacter baumannii. Clin Microbiol Infect. 2007;13(8):807–15.
Dijkshoorn L, Aucken H, Gerner-Smidt P, Janssen P, Kaufmann M, Garaizar J, et al. Comparison of outbreak and nonoutbreak Acinetobacter baumannii strains by genotypic and phenotypic methods. J Clin Microbiol. 1996;34(6):1519–25.
Malmivaara A. Benchmarking controlled trial—a novel concept covering all observational effectiveness studies. Ann Med. 2015;47(4):332–40.
Higgins P, Wisplinghoff H, Krut O, Seifert H. A PCR-based method to differentiate between Acinetobacter baumannii and Acinetobacter genomic species 13TU. Clin Microbiol Infect. 2007;13(12):1199–201.
Standard A, Edition N. CLSI document M07-A9. Wayne: Clinical and Laboratory Standards Institute; 2012.
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fifth Informational Supplement. CLSI document M100-S25. Wayne: Clinical and Laboratory Standards Institute; 2015.
Miranda CD, Kehrenberg C, Ulep C, Schwarz S, Roberts MC. Diversity of tetracycline resistance genes in bacteria from Chilean salmon farms. Antimicrob Agents Chemother. 2003;47(3):883–8.
Snelling AM, Gerner-Smidt P, Hawkey PM, Heritage J, Parnell P, Porter C, et al. Validation of use of whole-cell repetitive extragenic palindromic sequence-based PCR (REP-PCR) for typing strains belonging to the Acinetobacter calcoaceticus-Acinetobacter baumannii complex and application of the method to the investigation of a hospital outbreak. J Clin Microbiol. 1996;34(5):1193–202.
Asadollahi P, Akbari M, Soroush S, Taherikalani M, Asadollahi K, Sayehmiri K, et al. Antimicrobial resistance patterns and their encoding genes among Acinetobacter baumannii strains isolated from burned patients. Burns. 2012;38(8):1198–203.
Farsiani H, Mosavat A, Soleimanpour S, Nasab MN, Salimizand H, Jamehdar SA, et al. Limited genetic diversity and extensive antimicrobial resistance in clinical isolates of Acinetobacter baumannii in north-east Iran. J Med Microbiol. 2015;64(7):767–73.
Ecker JA, Massire C, Hall TA, Ranken R, Pennella TTD, Ivy CA, et al. Identification of Acinetobacter species and genotyping of Acinetobacter baumannii by multilocus PCR and mass spectrometry. J Clin Microbiol. 2006;44(8):2921–32.
Higgins PG, Janßen K, Fresen MM, Wisplinghoff H, Seifert H. Molecular epidemiology of Acinetobacter baumannii bloodstream isolates from the United States 1995-2004 using rep-PCR and multilocus sequence typing. J Clin Microbiol. 2012:JCM. 01759-12.
Nemec A, Dolzani L, Brisse S, van den Broek P, Dijkshoorn L. Diversity of aminoglycoside-resistance genes and their association with class 1 integrons among strains of pan-European Acinetobacter baumannii clones. J Med Microbiol. 2004;53(12):1233–40.
Authors’ contributions
Concepts: ZM, YA, AN. Design: ZM, HS, YA, HF, KG, AN. Definition of intellectual content: ZM, HF, KG, AN. Literature search: HS, HF, AN. Clinical studies: HS, YA, KG. Experimental studies: HS, MK, DM, AN. Data acquisition: HS, YA, MK, AN. Data analysis: ZM, HS, DM, HF, AN. Statistical analysis: AN. Manuscript preparation: ZM, HS, YA, MK, DM, HF, KG, AN. Manuscript editing: ZM, HS, YA, MK, DM, HF, KG, AN. Manuscript review: ZM, HS, YA, MK, DM, HF, KG, AN. Guarantor: ZM. All authors read and approved the final manuscript.
Acknowledgements
The authors appreciate the Ghaem laboratory staff for preparing the isolates.
Competing interests
The authors declare that they have no competing interests.
Funding
Financial support of Mashhad University of Medical Sciences are appreciated (Grant Number: Grant No. 931486).
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Meshkat, Z., Salimizand, H., Amini, Y. et al. Molecular characterization and genetic relatedness of clinically Acinetobacter baumanii isolates conferring increased resistance to the first and second generations of tetracyclines in Iran. Ann Clin Microbiol Antimicrob 16, 51 (2017). https://doi.org/10.1186/s12941-017-0226-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-017-0226-9