Abstract
Background
Acinetobacter baumannii (A. baumannii) is a common opportunistic pathogen in hospitals that causes nosocomial infection. In order to understand the phenotypic and genotypic characteristics of A. baumannii isolates, we sequenced and analyzed 62 A. baumannii isolates from a hospital in Gansu province.
Results
Non-repeated 62 A. baumannii isolates were collected from August 2015 to November 2021. Most isolates (56/62) were resistant to multiple drugs. All the 62 A. baumannii isolates were resistant to aztreonam and contained blaADC-25 gene which exists only on chromosome contigs. The 62 isolates in this study were not clustered in a single clade, but were dispersed among multiple clades in the common genome. Seven sequence types were identified by Multilocus sequence type (MLST) analysis and most isolates (52/62) belonged to ST2. The plasmids were grouped into 11 clusters by MOB-suite.
Conclusions
This study furthers the understanding of A. baumannii antimicrobial-resistant genotypes, and may aid in prevention and control nosocomial infection caused by drug-resistant A. baumannii.
Similar content being viewed by others
Background
Acinetobacter baumannii (A. baumannii) is a Gram-negative opportunistic pathogen, which can cause pneumonia, meningitis, wound infection, urinary tract infection, bacteremia and so on [1]. In all kinds of hospital-acquired infections caused by Gram-negative bacteria, A. baumannii accounted for 2%-10% [2, 3]. According to the declaration from the World Health Organization (WHO), A. baumannii has become one of the most threatening pathogens and an important focus of public health field and clinical research [4].
In recent years, the infection and drug resistance rates of A. baumannii have been increasing due to various factors, including the widespread use of antibiotics, the treatment of related immunosuppressants and invasive intervention. Some studies show that A. baumannii has the highest multidrug resistance (MDR) and extensive drug resistance (XDR) spectrum [5, 6]. According to the latest data report of China Antimicrobial Surveillance Network (CHINET, http://www.chinets.com/) in 2022, A. baumannii accounted for 7.5% of clinical isolates in China, ranking fifth among them [7]. The management of infected patients is difficult because of its complex drug-resistance mechanisms, the most worrying of which is carbapenem-resistant A. baumannii (CRAB). It is worth noting that the drug resistance rate of A. baumannii to antibiotics commonly used is basically increasing in China year by year. For example, the carbapenem-resistance rate of A. baumannii isolates such as imipenem and meropenem increased from 32.9% and 41.3% in 2005 to 77.7% and 79% in 2019, respectively. After 2019, the carbapenem-resistance rate decreased slightly, but remained above 70% [7].
According to the 2021 report from China Antimicrobial Resistance Surveillance System (CARSS, http://www.carss.cn/Report), he resistance rate of A. baumannii to carbapenem (imipenem or meropenem) was 54.3% on average, which was 0.6% higher than that in 2020 [8]. There are some differences in drug resistance rates among different regions. The average carbapenem-resistance rate of A. baumannii in Gansu province is 48.9% ranking in the middle level in China, which has also attracted our attention.
With the wide application and development of sequencing technology, many studies have focused on the genome-wide characteristics of A. baumannii isolates, including not only drug resistance and drug resistance genes, but also sequence types, plasmids, phylogenetic relationships and so on [9,10,11,12]. However, there are different characteristics in A. baumannii isolates from different hospitals.
Our study first analyzed the distribution and drug resistance characteristics, then clarified genomic characteristics of A. baumannii isolates from a hospital in Gansu province through whole-genome sequencing (WGS) technology, which could help guide infection control measures, prevention, and targeted antimicrobial therapy.
Method
Bacterial classification and antimicrobial susceptibility testing
Sixty-two non-repeated isolates were collected from Qingyang people's hospital in Gansu province, China, from August 2015 to November 2021. Bacterial isolates were initially subjected to identification using the VITEK-2 Compact system. Subsequently, the phenotypic identification was corroborated by whole-genome sequencing (WGS), where the genomic data obtained were compared against reference databases to validate and refine the taxonomic classification at the species or subspecies level. Antimicrobial susceptibility test to common clinical antibiotics was also detected by VITEK-2 compact system. Except the minimum inhibitory concentration (MIC) value of polymyxin was determined by the broth microdilution method. Escherichia coli ATCC25922 was used as a quality control strain. Seventeen common antibiotics include ticarcillin/clavulanic acid, piperacillin/tazobactam, ceftazidime, cefoperazone/sulbactam, cefepime, aztreonam, imipenem, meropenem, amikacin, tobramycin, ciprofloxacin, levofloxacin, doxycycline, minocycline, tigecycline, polymyxin, compound sulfamethoxazole.
The antimicrobial susceptibility test results were interpreted according to the Clinical and Laboratory Standards Institute (CLSI, 2021 version, https://clsi.org) unified protocol. Defining MDR, XDR and Pandrug resistant (PDR) criteria according to an international expert proposal for interim standard definitions for acquired resistance [13].
Whole-genome sequencing
Genomic DNA was extracted from bacterial cultures using the QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. DNA concentration and purity were measured using Qubit 4.0 (Thermo Fisher Scientific) and Nanodrop One (Thermo Fisher Scientific) at the same time. Sequencing libraries were generated using NEB Next Ultra DNA Library Prep Kit for Illumina (New England Biolabs) following the manufacturer's recommendations. The library quality was assessed on the Qubit 4.0 Fluorometer (Life Technologies) and Qsep400 High-Throughput Nucleic Acid Protein Analysis System (Houze Biological Technology Co.). DNA libraries were constructed with 150-bp paired-end fragments and sequenced on the HiSeq 2500 sequencer at Novogene Company (Beijing, China).
Bioinformatics analysis
Sequencing reads were quality filtered using the FastQC v0.11.8 software [14], adapters and low-quality reads were removed and filtered out using Trimmomatic with default parameters [15]. The A. baumannii strain XH731 (NZ_CP021321.1) was selected as the best-matching chromosomal reference by the genomic distance estimation tool Mash v2.3 [16]. Assembly of sequencing reads was carried out with Unicycler v0.4.8 in normal mode [17]. Then the quality of the acquired genome was assessed by QUAST v5.2.0 [18]. Genome assemblies was annotated by Prokka v1.12 [19]. Then a core-genome alignment was derived by Panaroo v1.2.10 [20]. GTR + I + G4 was selected as the best evolutionary model by using Modeltest-ng v0.1.7 [21]. The maximum likelihood phylogenetic tree was constructed by IQ-TREE v2.2.2 with 1000 bootstrap replicates [22]. The tree was midpoint-rooted and visualized by Figtree v1.4.4 (http://tree.bio.ed.ac.uk/software/figtree/).
Sequence types (STs) and unknown STs were verified by MLST v2.23.0 [23] and MLST server v2.0 via the online service of the Center for Genomic Epidemiology of the Danish University of Technology (CGE) [24] respectively. The MLST analysis of these two software was based on the Institute Pasteur MLST schemes. The capsular polysaccharides loci (KL) and lipooligosaccharides outer core loci (OCL) were detected using the A. baumannii KL and OCL reference sequence databases by Kaptive v2.0.6 [25]. Resistance genes was identified with Abricate v0.8 (https://github.com/tseemann/abricate) using resfinder database [26]. The genotypic structure surrounding the special resistance gene was annotated by RAST (http://rast.nmpdr.org/) [27] and Easyfig v2.2.5 [28] was used to visualize the multiple sequence alignment. As a set of modular tools, the MOB-suite was used to reconstruct and type plasmids [29].
Results
General features of the patients and A. baumannii isolates
From August 2015 to November 2021, A. baumannii isolates was obtained from 62 samples including catheter (1/62), cerebrospinal fluid (1/62), urine (1/62), skin (1/62), wound secretion (3/62), sputum (54/62) and pleural effusion (1/62). Isolates were obtained from 47 (75.8%) men between 36 and 81 years old and 15 (24.2%) women between 12 days and 70 years old. The wards mainly include the intensive care unit (ICU), infection ward, orthopedic ward, respiratory ward, surgery ward, neonatal ward and traditional Chinese medicine ward. The detailed clinical information from patients with A. baumannii isolates was shown in Supplementary Table S1.
Antimicrobial susceptibility testing
As shown in Table 1, 62 A. baumannii isolates were resistant to aztreonam (100%). Most isolates (56/62) were resistant to multiple drugs. Most isolates were resistant to piperacillin/tazobactam (88.71%), ceftazidime (88.71%), imipenem (85.48%), meropenem (85.48%), ciprofloxacin (82.26%), ticarcillin/clavulanic acid (80.65%), cefepime (79.03%), doxycycline (77.42%) and tobramycin (74.19%), but most isolates were sensitive to tigecycline (96.87%), polymyxin (95.16%) and minocycline (79.03%). Among 62 A. baumannii isolates, 55 MDR and 1 XDR A. baumannii isolates were identified, respectively. The MIC values of the 62 isolates were provided in Supplementary Table S2.
Genomic characterization of A. baumannii
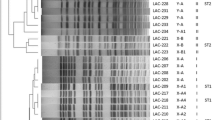
The genome sequences of 62 A. baumannii were obtained by whole-genome sequencing (Supplementary Table S3). Reads mapping to A. baumannii reference genome XH731 showed an average of 97.8% coverage among all 62 genomes. Seven sequence types were identified (Fig. 2 and Supplementary Table S1). Most of these A. baumannii isolates belonged to ST2 (52/62), which mainly isolated from ICU (27/52) and neurosurgery ward (12/52). ST2 A. baumannii isolates isolated in 2015, 2016 and 2021, with the largest number in 2016 (29/52). Others belonged to ST34 (1/62), ST40 (3/62), ST104 (1/62), ST132 (2/62) ST1108 (1/62), and ST1376 (2/62).
Thirteen distinct KL (KL3, KL161, KL230, KL47, KL61, KL72, KL106, KL160, KL22, KL33, KL34, KL45, KL9) configurations and five OCL (OCL1, OCL6, OCL21, OCL15, OCL18) configurations were detected among the isolates (Fig. 2 and Supplementary Table S1). The most common KL loci and OCL loci were KL3 (38/62) and OCL1(54/62), respectively.
Phylogenetic analysis
In order to explore the relationship between the A. baumannii isolates collected in this study and those previously studied, genome sequences of 567 A. baumannii isolates (Supplementary Table S4) were downloaded from the Bacterial and Viral Bioinformatics Resource Center (BV-BRC, https://www.bv-brc.org/), which were combined with 62 isolates in this study for the phylogenetic analysis. Figure 1 showed that the 62 isolates in this study did not cluster completely by source, but were dispersed among multiple clades in the common genome. Among the 52 ST2 strains collected in this study, phylogenetic analysis revealed that despite being isolated from the same hospital, they did not cluster on the same branch. Instead, they formed two main branches, comprising 38 and 9 isolates respectively, with the remaining 5 isolates scattered across different branches.
Phylogenetic analysis map of 629 A. baumannii isolates. The phylogenetic tree contains 567 A. baumannii isolates (ab_number) from BV-BRC and 62 A. baumannii isolates in this study (gs_number), annotating the isolation time, country, and host origin of the A. baumannii isolates from the inner ring to the outer ring. The black block means NA (Not available). The blue blocks on the tree branches signifies 62 A. baumannii isolates in this study
Antibiotic resistance gene profiles of A. baumannii
The distribution of antibiotic resistance genes (ARGs) of different STs A. baumannii isolates was shown in Fig. 2. A total 27 types of ARGs were identified, conferring resistance to 7 classes of antibiotic including aminoglycosides, beta-lactams, lincomycin, sulphonamide, phenicols, macrolides, tetracycline. Among them, blaTEM-1D (51/61) and blaADC-25 (62/62) genes were the most prevalent on the putative plasmid and chromosomal contigs, respectively. The blaADC-25 gene only on the chromosomal contigs was further explored carried by all strains.
The phylogenetic tree and distribution of STs, KL types, OCL types, plasmids and ARGs among 62 A. baumannii isolates. On the left half, a phylogenetic tree was generated using IQ-TREE v2.2.2 software and midpoint-rooted for improved visualization using Figtree v1.4.4. Isolates are color-coded according to their STs, capsular polysaccharide (KL) types, and lipooligosaccharides outer core loci (OCL). Fifty-two ST2 and one ST1108 isolates were clustered into two monophyletic clades, referred to as Clade1 and Clade2. On the right, four frames provide information about plasmid carriage and distribution of Antibiotic Resistance Genes (ARGs). Frame1 indicates the distribution of plasmids; Frame 2 highlights ARGs found only on plasmid contigs; Frame 3 focuses on ARGs present on both plasmid and chromosome contigs; Frame 4 shows ARGs exclusive to chromosome contigs, the light blue squares represent the absence of plasmid or ARGs, dark blue and purple squares represent one and two plasmids or ARGs, respectively
In order to understand the surrounding environment of blaADC-25 gene, we randomly selected a representative isolate of each ST type. Then the blaADC-25-containing contig sequences were extracted from the genome data, among which seven contigs from isolates gs18, 28, 29, 45, 55, 58 and 65. However, no mobile genetic element, such as a transposon or insertion sequence (IS), was found surrounding the blaADC-25, as shown in Fig. 3.
Analysis of blaADC-25 surrounding environment. Each arrow represents an open reading frame (ORF). The red arrows represent blaADC-25 gene, the orange arrows represent putative outer membrane protein and the gray arrows represent hypothetical proteins and others. The grey shaded areas represent highly homologous regions between contigs. The two overly long contigs of gs58 and gs28 have been truncated to improve the figure visualization
Plasmid carriage profile
Plasmids were detected in 61 of 62 A. baumannii isolates (98.4%), totaling 110 putative plasmids (median: 2 per isolate; range: 1–5). The putative plasmids were grouped into 11 clusters by mob suite, including rep_cluster_586, rep_cluster_639, rep_cluster_650, rep_cluster_734, rep_cluster_718, rep_cluster_1118, rep_cluster_1172, rep_cluster_1226, rep_cluster_1254, rep_cluster_1259, rep_cluster_1281. A. baumannii ST2 isolates mainly carried rep_cluster_1172 (40/52) and rep_cluster_734 (20/52). In addition, no virulence genes were found in the 110 putative plasmid contigs.
Discussion
Phylogenetic analyses combined with BV-BRC and the data in this study showed that the 629 isolates were derived from 34 countries, with most of them being from Asia. A review summarizes Acinetobacter accounts for approximately 2% of nosocomial infections in the USA but these rates are doubled in Asia and the Middle East [30]. A. baumannii infection in Asia is a considerable challenge to healthcare professionals in hospitals.
According to the source distribution of 62 A. baumannii isolates in this study, the main specimen type was sputum, which is consistent with the results of previous studies [31, 32]. The wards distribution showed that the isolates mainly from ICU and neurosurgery ward. Especially for patients in the ICU, the establishment of artificial airway operations such as ventilator invasion may form biofilms on the surfaces, thus increasing the risk of infection and antibiotic resistance of A. baumannii [2, 33,34,35]. Therefore, patients in the ICU and neurosurgery ward are more infected with A. baumannii and medical staff should pay attention to the standardization of invasive operations.
Although previous studies have shown that A. baumannii can produce wide-spectrum beta-lactamases, which affected the resistance of A. baumannii to β-lactam antibiotics by hydrolysis of beta-lactams [36, 37]. However, as wide-spectrum antibiotics, carbapenem antibiotics are widely used in clinic treatment, causing high drug resistance. In this study, A. baumannii isolates showed high-level resistance to carbapenem antibiotics and high-level sensitivity to tigecycline, polymyxin and minocycline, which was similar to the results from Italy [38] and China [39]. Therefore, carbapenem antibiotics in combination with polymyxin or tigecycline should be considered to in clinical treatment of MDR A. baumannii infection [40]. If there are co-infections, polymyxin will be used to treat patients [41, 42].
Seven STs in the study belonged to known A. baumannii international clones (ICs). The analysis of all publicly available genome sequences in 2019 indicated that ST2, ST1, ST79 and ST25 account for more than 71% of all sequenced genomes, with ST2 by far the most dominant type [43]. The results of MLST typing of 62 A. baumannii isolates showed that ST2 accounted for 83.9% (52/62), which was the dominant ST type in this study. The results are consistent with other related researches in China [44, 45]. The reason why ST2 isolates have become the dominant ST type may be due to its strong biofilm formation ability, high serum resistance, and high pathogenicity [45].
Several studies have proved that the prevalence of A. baumannii is associated with blaADC-25 [12, 44], blaOXA-23 and blaOXA-66 genes [46]. This has also been proved in our study, which exhibited all A. baumannii isolates have blaADC-25 gene, which are dominant in cephalosporins and carbapenems resistance in A. baumannii ST2 isolates. Insertion sequences (ISs) was responsible for the overexpression of the chromosomally encoded blaADC gene [47]. There are no ISs in the blaADC-25 surrounding environment in the selecting representative isolates per ST, suggesting that the gene is an inherent drug resistance gene located on chromosomes.
The MOB-suite identified contigs of plasmid origin showed both high sensitivity and specificity (95 and 88%, respectively) [27]. Therefore, we used the software for clustering, reconstruction and typing of plasmids from assemblies. Unfortunately, these rep_clusters are not identified to specific known replicators. But our focus is mainly to understand the plasmids sequences for ARGs-carrying contigs.
The phylogenetic analysis of the 62 strains revealed that among the 52 ST2 strains, two distinct monophyletic clades were formed on the phylogenetic tree. Clade1 predominantly harbored the rep_cluster_1172 plasmid along with the aph (3')-Ia resistance gene, whereas clade2 was characterized by the presence of the rep_cluster_1226 plasmid and lacked the aph (3')-Ia resistance gene. This finding illuminated the underlying relationship between different genetic lineages and their associations with specific plasmids as well as antibiotic resistance profiles.
There are some limitations in this study. The number of other types of specimens apart from sputum was very small. The number of specimens such as pleural effusion and urine can be increased in follow-up study. Although we used the cluster codes provided by MOB-cluster for description of plasmids that share significant sequences without the need for defined biomarkers. Only rep_clusters were obtained which cannot be identified to specific known replication factors. We mainly focused on studying resistance gene carrier, and virulence and detailed transmission routes of A. baumannii isolates need to be understand in the future.
To sum up, A. baumannii isolates in this study are resistant to most antibiotics and carries a variety of drug resistance genes, indicating the severe situation of drug resistance. The surveillance of drug resistance and active screening of A. baumannii should be strengthened for curbing the spread of A. baumannii in hospitals. There are few previous studies about phenotypic and molecular characteristics of A. baumannii in Gansu province. Our study provided implications to further explore the main genotypic and phenotypic characteristics of A. baumannii in Gansu province.
Conclusions
Our study reveals genotypic and phenotypic characteristics of A. baumannii isolates from a hospital in Gansu Province, China, offering reference into further exploring the main characteristics of A. baumannii.
Availability of data and materials
Data is deposited in National Microbiology Data Center (NMDC) with accession numbers NMDC10018764 (https://nmdc.cn/resource/genomics/project/detail/NMDC10018764).
Abbreviations
- A. baumannii :
-
Acinetobacter baumannii
- MLST:
-
Multilocus sequence type
- WHO:
-
World Health Organization
- MDR:
-
Multidrug resistance
- XDR:
-
Extensive drug resistance
- CHINET:
-
China Antimicrobial Surveillance Network
- CRAB:
-
Carbapenem-resistant A. baumannii
- CARSS:
-
China Antimicrobial Resistance Surveillance System
- WGS:
-
Whole-genome sequencing
- MIC:
-
Minimum inhibitory concentration
- CLSI:
-
Clinical and Laboratory Standards Institute
- PDR:
-
Pandrug resistant
- STs:
-
Sequence types
- CGE:
-
Genomic Epidemiology of the Danish University of Technology
- KL:
-
Capsular polysaccharides loci
- OCL:
-
Lipooligosaccharides outer core loci
- BV-BRC:
-
Bacterial and Viral Bioinformatics Resource Center
- ARGs:
-
Antibiotic resistance genes
- ICs:
-
International clones
References
Petrosillo N, Granata G. Gram negatives and antimicrobial resistance: two faces of the same coin. J Clin Med. 2022;11:5574.
Gedefie A, Demsis W, Ashagrie M, Kassa Y, Tesfaye M, Tilahun M, et al. Acinetobacter baumannii biofilm formation and its role in disease pathogenesis: a review. Infect Drug Resist. 2021;14:3711–9.
Joly-Guillou M-L. Clinical impact and pathogenicity of Acinetobacter. Clin Microbiol Infect. 2005;11:868–73.
De Oliveira DMP, Forde BM, Kidd TJ, Harris PNA, Schembri MA, Beatson SA, et al. Antimicrobial resistance in ESKAPE pathogens. Clin Microbiol Rev. 2020;33:e00181-e219.
Mohamed AH, Mohamud HA, Arslan E. Epidemiological characteristics and predisposing factors for surgical site infections caused by bacterial pathogens exhibiting multidrug-resistant patterns. Antibiotics (Basel). 2021;10:622.
Adan FN, Jeele MOO, Omar NMS. Epidemiology of multidrug resistant non-fermentative gram negative bacilli in patients with hospital acquired Pneumonia: an alarming report from Somalia. Infect Drug Resist. 2022;15:6297–305.
Antimicrobial surveillance results on China Antimicrobial Surveillance Network (CHINET) in 2022. https://www.chinets.com/Documentlast accessed July 2023.
China Antimicrobial Resistance Surveillance System (CARSS) Report in 2021 (brief version). https://www.carss.cn/Report/Details/862last accessed July 2023.
Bian X, Liu X, Zhang X, Li X, Zhang J, Zheng H, et al. Epidemiological and genomic characteristics of Acinetobacter baumannii from different infection sites using comparative genomics. BMC Genomics. 2021;22:530.
Gu Y, Zhang W, Lei J, Zhang L, Hou X, Tao J, et al. Molecular epidemiology and carbapenem resistance characteristics of Acinetobacter baumannii causing bloodstream infection from 2009 to 2018 in northwest China. Front Microbiol. 2022;13:983963.
Chukamnerd A, Singkhamanan K, Chongsuvivatwong V, Palittapongarnpim P, Doi Y, Pomwised R, et al. Whole-genome analysis of carbapenem-resistant Acinetobacter baumannii from clinical isolates in Southern Thailand. Comput Struct Biotechnol J. 2022;20:545–58.
Wareth G, Linde J, Nguyen NH, Nguyen TNM, Sprague LD, Pletz MW, et al. WGS-based analysis of carbapenem-resistant acinetobacter baumannii in Vietnam and molecular characterization of antimicrobial determinants and MLST in Southeast Asia. Antibiotics (Basel). 2021;10:563.
Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81.
Babraham Bioinformatics. Fastqc: a quality control tool for high throughput sequence data. http://www.bioinformatics.babraham.ac.uk/projects/fastqc/.
Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–20.
Ondov BD, Treangen TJ, Melsted P, Mallonee AB, Bergman NH, Koren S, et al. Mash: fast genome and metagenome distance estimation using MinHash. Genome Biol. 2016;17:132.
Wick RR, Judd LM, Gorrie CL, Holt KE. Unicycler: Resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput Biol. 2017;13:e1005595.
Mikheenko A, Prjibelski A, Saveliev V, Antipov D, Gurevich A. Versatile genome assembly evaluation with QUAST-LG. Bioinformatics. 2018;34:i142–50.
Seemann T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 2014;30:2068–9.
Tonkin-Hill G, MacAlasdair N, Ruis C, Weimann A, Horesh G, Lees JA, et al. Producing polished prokaryotic pangenomes with the Panaroo pipeline. Genome Biol. 2020;21:180.
Darriba D, Posada D, Kozlov AM, Stamatakis A, Morel B, Flouri T. ModelTest-NG: a new and scalable tool for the selection of DNA and protein evolutionary models. Mol Biol Evol. 2020;37:291–4.
Nguyen L-T, Schmidt HA, von Haeseler A, Minh BQ. IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol Biol Evol. 2015;32:268–74.
Jolley KA, Bray JE, Maiden MCJ. Open-access bacterial population genomics: BIGSdb software, the PubMLST.org website and their applications. Wellcome Open Res. 2018;3:124.
Larsen MV, Cosentino S, Rasmussen S, Friis C, Hasman H, Marvig RL, et al. Multilocus sequence typing of total-genome-sequenced bacteria. J Clin Microbiol. 2012;50:1355–61.
Lam MMC, Wick RR, Judd LM, Holt KE, Wyres KL. Kaptive 2.0: updated capsule and lipopolysaccharide locus typing for the Klebsiella pneumoniae species complex. Microb Genom. 2022;8:000800.
Zankari E, Hasman H, Cosentino S, Vestergaard M, Rasmussen S, Lund O, et al. Identification of acquired antimicrobial resistance genes. J Antimicrob Chemother. 2012;67:2640–4.
Aziz RK, Bartels D, Best AA, DeJongh M, Disz T, Edwards RA, et al. The RAST Server: rapid annotations using subsystems technology. BMC Genomics. 2008;9:75.
Sullivan MJ, Petty NK, Beatson SA. Easyfig: a genome comparison visualizer. Bioinformatics. 2011;27:1009–10.
Robertson J, Nash JHE. MOB-suite: software tools for clustering, reconstruction and typing of plasmids from draft assemblies. Microb Genom. 2018;4:e000206.
Bartal C, Rolston KVI, Nesher L. Carbapenem-resistant Acinetobacter baumannii: Colonization, infection and current treatment options. Infect Dis Ther. 2022;11:683–94.
Lin J, Gao X, Cui Y, Sun W, Shen Y, Shi Q, et al. Increased multidrug resistant isolates: new clinical burdens for 66 hospitals in Shanghai, 2015 to 2017. Ann Transl Med. 2020;8:112.
Ren G, Zhou M, Ding N, Zhou N, Li Q. Analysis on distribution features and drug resistance of clinically isolated Acinetobacter baumannii. Exp Ther Med. 2016;12:1715–8.
Smitran A, Lukovic B, Bozic Lj, Jelic D, Jovicevic M, Kabic J, et al. Carbapenem-resistant acinetobacter baumannii: biofilm-associated genes, biofilm-eradication potential of disinfectants, and biofilm-inhibitory effects of selenium nanoparticles. Microorganisms. 2023;11:171.
Eze EC, Chenia HY, El Zowalaty ME. Acinetobacter baumannii biofilms: effects of physicochemical factors, virulence, antibiotic resistance determinants, gene regulation, and future antimicrobial treatments. Infect Drug Resist. 2018;11:2277–99.
Han L, Gao Y, Liu Y, Yao S, Zhong S, Zhang S, et al. An Outer Membrane Protein YiaD Contributes to Adaptive Resistance of Meropenem in Acinetobacter baumannii. Microbiol Spectr. 2022;10(2):e0017322.
Peterson LR. Bad bugs, no drugs: no ESCAPE revisited. Clin Infect Dis. 2009;49:992–3.
Lee C-R, Lee JH, Park M, Park KS, Bae IK, Kim YB, et al. Biology of Acinetobacter baumannii: Pathogenesis, Antibiotic Resistance Mechanisms, and Prospective Treatment Options. Front Cell Infect Microbiol. 2017;7:55.
Floridia M, Giuliano M, Monaco M, Palmieri L, Lo Noce C, Palamara AT, et al. Microbiologically confirmed infections and antibiotic-resistance in a national surveillance study of hospitalised patients who died with COVID-19, Italy 2020–2021. Antimicrob Resist Infect Control. 2022;11:74.
Luo XQ, Gong YL, Zhang C, Liu MX, Shi YL, Peng YZ, et al. Analysis of distribution and drug resistance of pathogens isolated from 159 patients with catheter-related bloodstream infection in burn intensive care unit. Zhonghua Shao Shang Za Zhi. 2020;36:24–31.
Lee K, Kim M-N, Hong HL, Kang JO, Shin JH, et al. Further increases in carbapenem-, amikacin-, and fluoroquinolone-resistant isolates of Acinetobacter spp. and P. aeruginosa in Korea: KONSAR study 2009. Yonsei Med J. 2011;52:793–802.
Mohd R, Nesam T, Kamaruzaman L, Cader RA, Mustafar R, Kong W-Y. Community acquired multi drug resistant (MDR) Acinetobacter baumannii pneumonia in Malaysia – A case report. Respir Med Case Rep. 2018;24:147–9.
Falagas ME, Rafailidis PI, Matthaiou DK, Virtzili S, Nikita D, Michalopoulos A. Pandrug-resistant Klebsiella pneumoniae, Pseudomonas aeruginosa and Acinetobacter baumannii infections: characteristics and outcome in a series of 28 patients. Int J Antimicrob Agents. 2008;32:450–4.
Hamidian M, Nigro SJ. Emergence, molecular mechanisms and global spread of carbapenem-resistant Acinetobacter baumannii. Microb Genom. 2019;5(10):e000306. https://doi.org/10.1099/mgen.0.000306.
Wei C, Chen J, Anwar TM, Huang L, Yang W, Dong X, et al. Genomic determinants of pathogenicity and antimicrobial resistance of nosocomial acinetobacter baumannii clinical isolates of hospitalized patients (2019–2021) from a Sentinel hospital in Hangzhou. China Infect Drug Resist. 2023;16:2939–52.
Yu K, Zeng W, Xu Y, Liao W, Xu W, Zhou T, et al. Bloodstream infections caused by ST2 Acinetobacter baumannii: risk factors, antibiotic regimens, and virulence over 6 years period in China. Antimicrob Resist Infect Control. 2021;10:16.
Li J, Li Y, Cao X, Zheng J, Zhang Y, Xie H, et al. Genome-wide identification and oxacillinase OXA distribution characteristics of Acinetobacter spp. based on a global database. Front Microbiol. 2023;14:1174200.
Lopes BS, Amyes SGB. Role of ISAba1 and ISAba125 in governing the expression of blaADC in clinically relevant Acinetobacter baumannii strains resistant to cephalosporins. J Med Microbiol. 2012;61:1103–8.
Acknowledgements
The authors wish to thank healthcare professionals and the patients who provided samples and data for this study.
Funding
This work was supported by grants from Chinese National Natural Science Foundation (Grant No. 31900151), Health Scientific Research Project Foundation of Gansu Province (No: GSWSQN2022-09) and the Natural Science Foundation of Qingyang City (No: QY2021A-F024).
Author information
Authors and Affiliations
Contributions
Xiong Liu and Juan Li designed the study. Yang Wang and Juan Li collected the isolates and detailed clinical information from patients. Na Zhang completed related experiments. Xiong Liu and Jiali Chen carried out the WGS analysis, related bioinformatics analysis and visualization. Jiali Chen performed the analysis and drafted the manuscript. All authors reviewed and agreed on the final version for submission.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
In this study, all clinical samples were collected during routine patient care and diagnostic procedures at the Qingyang People's Hospital in Gansu Province. We confirm that all experimental protocols were approved by the ethics committees of Qingyang People’s hospital. As all data were anonymously collected and interpreted, and the study involved only the analysis of bacterial isolates that were de-identified and not linked to any personal information, thus the need for written informed consent was waived by the ethics committees of Qingyang People’s hospital. This waiver is consistent with national legislation and ethical standards pertaining to the secondary use of clinical isolates. The study was also supervised by Chinese PLA Center for Disease Control and Prevention. Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12864_2024_10601_MOESM1_ESM.xls
Supplementary Material 1. Supplementary Table S1. Detailed clinical information from patients with A. baumannii isolates. (1) Only the gs65 patient is 12 days old; (2) ICU: intensive care unit. Supplementary Table S2. Antimicrobial susceptibilities of sixty-two Acinetobacter baumannii isolates. R: Resistant; I: Intermediate; S: Susceptible. Supplementary Table S3. Quality assessment information for genome assemblies. Supplementary Table S4. Basic information of 567 Acinetobacter baumannii isolates from BV-BRC. NA means not available.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, J., Wang, Y., Zhang, N. et al. Genotypic and phenotypic characteristics of Acinetobacter baumannii isolates from the people’s hospital of Qingyang City, Gansu province. BMC Genomics 25, 727 (2024). https://doi.org/10.1186/s12864-024-10601-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12864-024-10601-x