Abstract
Background
Rapid diagnostic tests (RDTs) are effective tools to diagnose and inform the treatment of malaria in adults and children. The recent development of a highly sensitive rapid diagnostic test (HS-RDT) for Plasmodium falciparum has prompted questions over whether it could improve the diagnosis of malaria in pregnancy and pregnancy outcomes in malaria endemic areas.
Methods
This landscape review collates studies addressing the clinical performance of the HS-RDT. Thirteen studies were identified comparing the HS-RDT and conventional RDT (co-RDT) to molecular methods to detect malaria in pregnancy. Using data from five completed studies, the association of epidemiological and pregnancy-related factors on the sensitivity of HS-RDT, and comparisons with co-RDT were investigated. The studies were conducted in 4 countries over a range of transmission intensities in largely asymptomatic women.
Results
Sensitivity of both RDTs varied widely (HS-RDT range 19.6 to 85.7%, co-RDT range 22.8 to 82.8% compared to molecular testing) yet HS-RDT detected individuals with similar parasite densities across all the studies including different geographies and transmission areas [geometric mean parasitaemia around 100 parasites per µL (p/µL)]. HS-RDTs were capable of detecting low-density parasitaemias and in one study detected around 30% of infections with parasite densities of 0–2 p/µL compared to the co-RDT in the same study which detected around 15%.
Conclusion
The HS-RDT has a slightly higher analytical sensitivity to detect malaria infections in pregnancy than co-RDT but this mostly translates to only fractional and not statistically significant improvement in clinical performance by gravidity, trimester, geography or transmission intensity. The analysis presented here highlights the need for larger and more studies to evaluate incremental improvements in RDTs. The HS-RDT could be used in any situation where co-RDT are currently used for P. falciparum diagnosis, if storage conditions can be adhered to.
Similar content being viewed by others
Background
Malaria in pregnancy (MiP) is associated with increased risk of poor maternal and infant health outcomes, including fetal loss, maternal anaemia, pre-term birth, low birthweight and intrauterine growth retardation, which in turn increase the risk of infant morbidity and mortality [1]. Modelled estimates indicate that in 2019, 35% of pregnancies in sub-Saharan Africa (or 11.6 million expectant mothers) were exposed to malaria infections, leading to 0.8 million low birthweight newborns [2, 3]. Malaria prevalence is highest in women who are primigravid and who are in the first or second trimester of pregnancy [4]. To protect against MiP, a strategy of routine intermittent preventative treatment during pregnancy (IPTp) with sulfadoxine-pyrimethamine (SP) is recommended at each scheduled antenatal care visit in the second and third trimester, at a minimum of monthly intervals [5]. However, IPTp with SP is contraindicated in the first trimester of pregnancy, is threatened by parasite resistance to SP, is only recommended in moderate and high transmission areas of sub-Saharan Africa, and the uptake is poor [3], limiting the effectiveness of this intervention.
WHO has reviewed different ‘Test and Treat’ strategies in the context of MiP, such as Intermittent Screening and Treatment (ISTp) at the first antenatal care (ANC) visit [6]. Although wide-scale deployment of rapid diagnostic tests (RDTs) for the detection of malaria has been largely successful in control efforts in the general population, pooled analyses have shown that interventions based on maternal screening with conventional RDTs (co-RDT) did not provide any additional benefit as compared to routine IPTp-SP [6, 7].
IPTp is contra-indicated in the first trimester of pregnancy, yet a high proportion of women are infected in the first trimester [8], which can have devasting consequences for the pregnancy [9,10,11]. Early detection and treatment of infections is, therefore, essential. However, detection is difficult as pregnant women infected with Plasmodium falciparum are commonly asymptomatic and have low density infections [12], and infected erythrocytes that sequester in the placenta escape detection in peripheral blood [9]. An important proportion of these low-density malaria infections remain undetected by light microscopy or co-RDTs [13]. A modelling study on malaria screening strategies at ANC visits suggested that more sensitive RDTs could provide incremental improvements in ISTp strategies over IPTp-SP in terms of reducing infection prevalence at delivery, with presumably better outcomes for mother and child [8]. It also highlighted that ISTp during the first trimester could improve pregnancy outcomes [8]. Improved point-of-care diagnostics that can detect more cases of maternal infections and in particular placental malaria may thus contribute to a reduction of adverse clinical outcomes for mothers and newborns in malaria endemic settings.
A highly sensitive RDT (HS-RDT) based on detection of Histidine-Rich Protein 2 (HRP2) was developed (NxTek™ Eliminate malaria Pf, Abbott Diagnostics) to improve the identification of P. falciparum infections below the detection limit of co-RDTs. The HS-RDTs enable point-of-care testing with an analytical sensitivity (limit of detection (LOD)) that is ten-fold lower than that reported for current best-in-class co-RDTs, at 80 pg of HRP2 per mL of blood [14] compared to 800-1000 pg for co-RDTs [15] as tested in vitro in malaria-negative blood. A recent review of data across multiple studies in different settings show that this improvement in analytical performance consistently results in an improvement in sensitivity and prevalence estimates as compared to PCR reference testing. The significance of this improvement varies from setting to setting [16,17,18].
In June 2018, the WHO Global Malaria Programme convened a technical consultation to identify the evidence required to develop recommendations on the use of the HS-RDT in different contexts including the detection of MiP [19]. The lack of results from prospective longitudinal studies or trials assessing the clinical impact of the HS-RDT as part of interventions to prevent MiP was noted. It was concluded that diagnostic accuracy studies comparing the HS-RDT to co-RDT are of high priority, and that these should reflect a range of different conditions (e.g. transmission intensities, target populations). This review compiles all existing evidence to date on the performance and use case scenarios of the HS-RDT in the context of pregnancy to inform policy makers and the research community on existing evidence and knowledge gaps.
Methods
This evidence review encompassed both published articles in peer-reviewed journals as well as other grey literature such as technical reports or presentations at scientific conferences.
Collection of data through online resources
Information was gathered on completed and ongoing research projects or grants reported between January 2017 to December 2020 in the following databases: MEDLINE–Pubmed Central, Malaria in Pregnancy Library (Malaria in Pregnancy Consortium), Cochrane Library, MESA Track database, Conference books (MIM, ECTMIH, ASTMH), ClinicalTrials.gov, WHO–International Clinical Trials Registry Platform, ICH GCP–Clinical Trials Registry, Grantome.com, Europe PMC Grant Finder, National Institutes of Health (NIH). The keywords used for the project search were: malaria, pregnant/pregnancy, RDT, diagnostic, (highly/ultra)-sensitive, HS-RDT, hsRDT, uRDT, Alere.
Contact with experts and stakeholders
Experts and stakeholders were contacted to further identify ongoing studies. This included 25 active researchers in the field of MiP or malaria diagnostics, as well as focal persons in international organizations working in these fields. Each contact was also asked to name other experts in the field who were then contacted. All Principal Investigators of identified eligible studies were contacted in order to confirm their study details and the accuracy of the data included in the comparative analyses presented in this review.
Study inclusion criteria
Prospective studies of any design were eligible if they included pregnant women during pregnancy (any trimester) or at delivery, used the NxTek™ Eliminate malaria Pf RDT by Abbott Diagnostics (formerly the Alere Malaria Ag Pf (05FK140)), and reported P. falciparum detection using any reference assay.
Analysis of methodology
The product disclosure statements were assessed for all co-RDTs used in the trials and all were assessed to be of high quality. All studies used the recommended 5 µL of blood to perform the RDT. The molecular reference standards used in the completed studies were quantitative PCR (qPCR; 3), quantitative Reverse Transcription PCR (qRT–PCR; 2), Photo-induced-electron-transfer PCR (PET–PCR; 1), nested PCR (nPCR; 1) and a composite qPCR + Loop-mediated isothermal DNA amplification (LAMP; 1). The equivalent volume of blood from which DNA was extracted and used for the molecular methods varied and was not known for most studies, however the Benin study used 1.7 µL blood equivalent. LOD or limit of quantification (LOQ) were used as determined and reported in the study where possible, or based on the reference for the technique.
Data analysis
Quantitative and qualitative data from all the eligible studies were collected in multiple Excel spreadsheets. Figures were prepared with Graphpad Prism 8.1. (GraphPad Software, Inc., CA, US), and additional test performance analyses (i.e. not provided in published articles) of Pearson and Spearman correlations and paired t-test were conducted with STATA version 11 software (StataCorp LP, College Station, TX, USA). Efforts were made to perform meta-analyses, but the heterogeneity of the studies was too great to provide meaningful results.
Results
Eligible studies
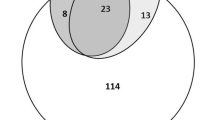
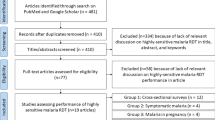
A total of 13 studies addressing HS-RDT use in pregnancy were identified as of December 2020 (Table 1). Eight studies were completed by this date. A further three studies had completed field activities, but the data were not available for this review, and five studies were ongoing.
The eight completed studies included all malaria endemic WHO regions except EMRO and transmission intensities ranging from low (n = 3, prevalence 4–7%) and medium (n = 1, prevalence 9.4%), to high (n = 4, prevalence > 25% or entomological inoculation rate (EIR) > 5 per year). Malaria transmission was determined by P. falciparum prevalence by PCR in the parent study, or by EIR. Prevalence was determined as low transmission < 9%, moderate 9–25%, and high > 25%. Prevalence by EIR was only used to determine high transmission areas. Samples were taken during regular ANC visits (7/8) and at delivery (3/8) and from symptomatic and asymptomatic individuals (Table 1). All studies compared the HS-RDT to a co-RDT and to a molecular test as a reference standard, though the type of co-RDT and molecular test used varied (Additional file 1: Table S1). The reference standards ranged in LOD from 0.02 to 6 parasites/μL. Two of the studies also quantified HRP2 concentrations present in the samples, using different methods [20, 21].
Data sets for five of the eight completed studies were available and included in this review. The sample size of the five studies ranged from 270 to 942, with the Benin study [22] sampling the same women more than once (Table 1). At least 80% of women were asymptomatic in all studies, and in Indonesia the study excluded symptomatic women [23] (Fig. 1A). Febrile proportion data refers to the number of tests conducted in women with fever or a recent history of fever, divided by the total number of tests conducted. Most studies included women in all trimesters, except the study in Benin which sampled women only during 1st and 3rd trimesters and sampled the placenta at delivery (Fig. 1B). The Benin results are presented from the same women repeatedly tested at different timepoints and peripheral and placental results were included for the overall sensitivity estimations. All studies except Indonesia collected gravidity and trimester data of pregnant women. The study in Benin had a low percentage of primigravid women (7.7%; Fig. 1C). Although the Indonesian study did not provide details on the trimester or gravidity the gravidity in the parent study [24] was 27% primigravid, 30% secundigravid, and 43% multigravida. A significant difference for the Indonesia study is that samples were reconstructed from blood pellets and plasma.
The studies included high malaria infection prevalence areas (Benin [22] and Kenya [25] 18–36%), moderate (Indonesia 9% [23]) and low prevalence (Colombia 4–5% [26, 27]). The studies in low prevalence areas used reference standards with the lowest limits of detection (0.02–1 parasites/μL (p/μL)). The study in Indonesia (moderate transmission) had an intermediate prevalence in the overall study population of 9.4%, however a subset of these patients was selected for the HS-RDT evaluation study, hence the high PCR positivity rate of 58.5% from the study samples.
Using molecular methods, the geometric mean parasitaemia, where available, ranged between 13 and 71 p/μL (Fig. 2). Mean parasite densities were lowest in the low transmission settings. While the geometric mean parasite density (GMPD) detected by molecular methods varied between studies, the GMPD of samples positive by HS-RDT was stable at around 100 p/μL (based on reference assay measurement) with no significant differences between studies. The lowest reported parasitaemias detected using HS-RDT were 2 and 5.14 p/μL in Benin and Kenya (1) studies, respectively. The GMPD detected by co-RDT was higher in both studies where these data were available (Benin 532 (95% CI 324–874) p/μL, and Colombia (2) 200 (95% CI 114–350) Fig. 2).
Geometric mean parasite densities and 95% CI of P. falciparum in samples positive by PCR or HS-RDT or co-RDT (for studies which calculated parasite density). The PCR Limit of Detection-Quantification reported by the different studies was: 2–5 p/ul (Benin), 0.02 p/ul (Colombia(2)), 3.2 p/ul (Kenya(1))*. *based on reference publication (not in-house estimation). Number of P. falciparum positive PCR and HS-RDT and co-RDT (when available) samples respectively per study: Benin = 179 and 153 and 76, Colombia (2) = 38 and 24 and 20, Kenya (1) = 172 and 107
Comparison of the performance of the HS-RDT and the co-RDT
Sensitivity, or the ability of the HS- and co-RDTs to detect true positives as determined by molecular testing, varied widely between studies from approximately 20 to 90% (Table 2; Fig. 3). In all studies the sensitivity of the co-RDT and HS-RDT were similar despite a wide difference between studies; while 4/5 of the studies showed a higher mean sensitivity of the HS-RDT compared to the co-RDT, in only one study was this a statistically significant difference (Table 2; Fig. 3). With the available data from three studies it is not possible to determine a relationship between sensitivity and parasite density (Additional file 1: Fig. S1). Specificity of both the HS-RDT and co-RDT was > 90% for all studies, with no significant difference between the HS-RDT and co-RDT (Table 2; Fig. 3). Heterogeneity between the studies was too great to allow a meta-analysis to be performed.
Sensitivity and specificity of the HS-RDT and the co-RDT for the detection of P. falciparum infection in pregnant women. The highly-sensitive rapid diagnostic test (HS-RDT: filled circles) was manufactured by Alere™, now Abbott. The conventional RDTs (co-RDT: unfilled circles) used in the different studies were manufactured by SD Bioline (Benin and Colombia (1)–(2)), Access Bio (Indonesia) and Premier Medical Corporation (Kenya (1)). Mean and 95% CI
HS-RDT performance compared with co-RDT according to population and infection characteristics
The HS-RDT was compared to the co-RDT to determine whether there were use cases where the HS-RDT could bring additional benefit. Sensitivity of both tests was higher in febrile compared to afebrile women as expected. In afebrile women, while 4/4 of the studies showed a higher mean sensitivity of the HS-RDT compared to the co-RDT, there was no statistical difference in sensitivity (Fig. 4).
The sensitivity of the co-RDT and HS-RDT by pregnancy trimester was investigated in Fig. 5. In high transmission settings (Benin and Kenya) both RDTs appeared to be more sensitive in later trimesters, but this was not significant. In low transmission settings the reverse was observed with highest sensitivity in 1st trimester, again there was no statistical difference.
Sensitivity of the HS-RDT and the co-RDT for the detection of malaria by trimester of pregnancy in different transmission areas. Highly-sensitive rapid diagnostic test (HS-RDT); conventional RDT (co-RDT). Evaluations conducted in high-transmission settings (Benin and Kenya (1)) are represented by circles, and in low-transmission settings are represented by squares; black: HS-RDT; white; co-RDT. Mean and 95% CI
There was no consistent pattern observed in sensitivity when compared by gravidity. The studies in Colombia (2) and Kenya showed decreasing sensitivity with increasing gravidity, and the study in Benin showed an increasing difference in sensitivity between the HS-RDT and co-RDT with increasing gravidity (Fig. 6).
HS-RDT sensitivity was not associated with P. falciparum prevalence reported in the studies (Spearman correlation r = − 0.314, p = 0.6), nor with the LOD of the reference method (Spearman correlation r = − 0.493, p = 0.3).
Other evaluations of the use of HS-RDT for MiP
Clinical outcomes were investigated only in the Benin study, where the effect of the RDT used on maternal and birth outcomes was evaluated. The results from this single study investigating clinical outcomes indicated that infections detected with the HS-RDT but not with the co-RDT were associated with maternal anaemia, suggesting that testing based on the HS-RDT might be clinically relevant in this specific context and provide a direct health benefit for the pregnant women.
Different use cases were investigated in studies in Benin, Colombia and Malawi where the HS-RDT was used to detect placental infections from either placental or peripheral blood at delivery. The sensitivity of HS-RDT compared to co-RDT to detect infections from peripheral blood compared to placental blood was significantly higher in Benin, but both tests showed poor sensitivity in Colombia to detect parasites in placental blood (Additional file 1: Fig. S2). In the placental blood samples in Benin the HS-RDT detected double the number of positive samples compared to the qPCR reference standard (20 compared to 10). This could either be a low specificity of the HS-RDT in placental blood due to sustained presence of HRP2 following clearance of active infections or, the authors note, a low sensitivity of the qPCR in the placental blood due to possible inhibitors not present in the peripheral blood.
All studies identified the GMPD of samples which tested positive by HS-RDT at around 100p/µL (as calculated by extrapolation of qPCR Ct values or by microscopy). The study in Benin calculated the parasitaemia level at which samples were HS-RDT positive and co-RDT negative (N = 28) to have a mean density of 20.7 p/µL with HRP2 levels at a mean of 1049 pg/mL.
Discussion
This paper describes the evidence landscape of HS-RDT performance compared with co-RDTs to diagnose P. falciparum malaria in pregnancy. In the reported studies HS-RDT does detect some very low parasitaemias, with the lowest density detected being ~ 2 parasite/μL. In the two studies with available data on parasitaemia the HS-RDT detected lower parasitaemias than the co-RDT. Overall, the detection of parasites is consistent across studies (~ 100 parasite/μL), therefore the variability in HS-RDT sensitivity is likely due to variations in epidemiological context such as parasite density distributions. Sensitivity of HS-RDTs ranged widely from 20 to 86% compared to molecular methods. The HS-RDT showed a slightly higher analytical sensitivity than the co-RDT in most studies but this difference was only statistically significant in the study from Benin.
The five studies with available data were heterogenous both geographically and by transmission intensity, aiding generalizability of the results. A key assumption is that molecular testing of peripheral blood can detect placental malaria, making these data comparable between sites [28]. Despite the limitations of using different PCR assays across studies infections in the low transmission sites tended towards lower parasite densities, supporting previous observations that there are more low-density infections in low transmission regions (< 100 parasite/μL [29, 30]). Walker et al. [8] showed that sensitivity decreased with decreasing parasite prevalence and hypothesized that HS-RDTs may have more impact than co-RDTs in low transmission areas with lower parasitaemias. The reviewed studies with the lowest transmission were in Colombia, and HS-RDTs were not significantly more sensitive than co-RDTs. However, looking at low density infections (parasite densities of ~ 10–100 p/μL), the HS-RDT identifies double the number of infections (26/44) as the co-RDT (13/44) in Benin [22], while in Colombia (2) the HS-RDT identifies 9/9 infections yet the co-RDT identifies only 6/9. This suggests an advantage to using HS-RDT to detect lower density infections.
Another source of variability in sensitivity is likely to be the samples used: although the RDTs are intended for use with fresh blood, the studies in Benin, Colombia (1), and Indonesia all used thawed blood, which may affect RDT performance. The study in Indonesia used thawed red blood cell pellets (stored: ~ 1 year), reconstituted with plasma to 30% haematocrit. This off-label use might account for the very low sensitivity of both the co-RDT and HS-RDT in this study. A further source of variation in sensitivity could be the reference standard used and its associated LOD. LODs ranged from ~ 0.02–6 parasite/μL. Across the five studies included in this analysis however, there was no trend for sensitivity to be associated with reference assay LOD.
Both RDTs tended to have higher sensitivity in febrile women compared with afebrile women, as expected. Prevalence of malaria infection is known to be highest at first ANC visit, and declines with gravidity by both PCR and co-RDT [4, 8]. The included studies did not show a clear relationship between HS-RDT sensitivity and gravidity, nor did this appear to be affected by transmission intensity. A recent modelling-based analysis [8] indicated that the main gain in sensitivity in using HS-RDTs among pregnant women should be expected when infections tend to have lower parasitaemias. When exploring this in the current review of limited studies, the clinical performance of the HS-RDT compared to co-RDTs only suggests a slight increase in analytical sensitivity in the 1st trimester in high-transmission settings, or the 2nd trimester in low transmission settings. One of the reasons behind this discrepancy is that the ‘better performing RDTs’ considered in these models are assumed to provide a 75% to 90% sensitivity, while most of the sensitivities observed in the HS-RDT field evaluations in the context of MiP fall below this range. The only study in which HS-RDT sensitivity significantly outperformed co-RDTs was in the first trimester in a high transmission setting (Benin) with a low proportion of primigravid women (8%). A major limitation of the analyses for febrility, gravidity and trimester are the low numbers of parasite positive women, limiting the statistical power of comparing sensitivities between the tests.
Another reason for minimal differences between HS-RDT and co-RDT could be that co-RDTs have a lower LOD than expected. While the criteria of detection of at least 200 parasite/μL is required for pre-qualification by WHO, the exact LOD is unknown and for some may approach the LOD of HS-RDT (i.e., they may detect lower numbers of parasites/uL). The SD Bioline Pf co-RDT was tested against the HS-RDT by Das et. al [14] and was found to be reactive to cultured parasites at ~ 49 parasite/µL compared to ~ 3.13 parasite/µL by the HS-RDT, i.e., in laboratory tests the LOD of this co-RDT was about four times more sensitive than the minimum required for WHO pre-qualification.
The main limitation of this evidence review is the difficulty of pooling data due to the heterogeneity of the studies, difference in reference assays and reporting formats, and small numbers of studies included. In turn, this heterogeneity is also a benefit to describe the potential advantages of the HS-RDTs in different situations. The main goal of diagnosing MiP is to reduce adverse clinical outcomes for women and their children. The study in Benin [22] identified that those infections in women that were detected with the HS-RDT but not by the co-RDT were more likely to suffer anaemia during pregnancy and suggested a higher risk of LBW, although this interaction is likely underpowered. It may also be due to the study design which treated any microscopy positive patients, which therefore identifies and treats those patients who would also be identified by co-RDT, while lower parasitaemic infections (i.e. those detected by HS-RDT) remain undetected and untreated which may lead to anaemia over time. The ongoing study in Burkino Faso [31] will investigate the impact of screening with HS-RDTs and treating women on placental malaria and LBW. These analyses of clinical outcomes are important as it is still unclear whether identifying more (low density) infections will make a difference to health outcomes. For example Rogerson et al. [9] identify four studies where infections detected by PCR but not by co-RDT were not associated with poorer outcomes in infants [32,33,34,35], and only one study in which infections detected by PCR and missed by microscopy were associated with LBW or prematurity [10], while a meta-analysis linked the presence of infections below co-RDT detection with clinical impacts [7]. More studies linking the use of more sensitive diagnostic tests with clinical outcomes are required.
Using HS-RDT in a similar manner to co-RDTs is supported, for example, using HS-RDT instead of co-RDT at ANC visits to assess community malaria transmission will provide more accurate prevalence estimates. However, other factors to consider in procurement include that HS-RDT has limited temperature stability and shelf-life claims compared to most co-RDT, and the costs of tests. Both tests will be limited in impact by the emergence of hrp2/hrp3 deletion parasites that escape detection [30].
Conclusion
Overall, the studies confirmed that the HS-RDT has a slightly higher analytical sensitivity than co-RDTs in various MiP epidemiological contexts. The use of the HS-RDT could be recommended in all cases where co-RDTs are currently used in ANC settings, although factors other than analytical sensitivity must be weighed in each context.
Availability of data and materials
The data that support the findings of this study are available from the lead authors of the individual studies, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request.
References
Saito M, Briand V, Min AM, McGready R. Deleterious effects of malaria in pregnancy on the developing fetus: a review on prevention and treatment with antimalarial drugs. Lancet Child Adolesc Health. 2020;4:761–74.
Walker PGT, Floyd J, ter Kuile F, Cairns M. Estimated impact on birth weight of scaling up intermittent preventive treatment of malaria in pregnancy given sulphadoxine-pyrimethamine resistance in Africa: a mathematical model. PLoS Med. 2017;14: e1002243.
WHO. World malaria report 2020. Geneva: World Health Organization; 2020. https://www.who.int/publications/i/item/9789240015791. Accessed 26 January 2023.
Desai M, ter Kuile FO, Nosten F, McGready R, Asamoa K, Brabin B, et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007;7:93–104.
WHO. Policy brief for the implementation of intermittent preventive treatment of malaria in pregnancy using sulfadoxine-pyrimethamine (IPTp-SP). Geneva: World Health Organization; 2013. https://www.who.int/publications/i/item/WHO-HTM-GMP-2014.4 Accessed: 26 January 2023
WHO Malaria Policy Advisory Committee and Secretariat. Malaria Policy Advisory Committee to the WHO: conclusions and recommendations of eighth biannual meeting (September 2015). Malar J. 2016;15:117.
Gutman JR, Khairallah C, Stepniewska K, Tagbor H, Madanitsa M, Cairns M, et al. Intermittent screening and treatment with artemisinin-combination therapy versus intermittent preventive treatment with sulphadoxine-pyrimethamine for malaria in pregnancy: a systematic review and individual participant data meta-analysis of randomised clinical trials. EClinicalMedicine. 2021;41: 101160.
Walker PGT, Cairns M, Slater H, Gutman J, Kayentao K, Williams JE, et al. Modelling the incremental benefit of introducing malaria screening strategies to antenatal care in Africa. Nat Commun. 2020;11:3799.
Rogerson SJ, Desai M, Mayor A, Sicuri E, Taylor SM, van Eijk AM. Burden, pathology, and costs of malaria in pregnancy: new developments for an old problem. Lancet Infect Dis. 2018;18:e107–18.
Cottrell G, Moussiliou A, Luty AJF, Cot M, Fievet N, Massougbodji A, et al. Submicroscopic Plasmodium falciparum infections are associated with maternal anemia, premature births, and low birth weight. Clin Infect Dis. 2015;60:1481–8.
Weckman AM, Ngai M, Wright J, McDonald CR, Kain KC. The impact of infection in pregnancy on placental vascular development and adverse birth outcomes. Front Microbiol. 2019;10:1924.
Fried M, Muehlenbachs A, Duffy PE. Diagnosing malaria in pregnancy: an update. Expert Rev Anti Infect Ther. 2012;10:1177–87.
Slater HC, Ross A, Felger I, Hofmann NE, Robinson L, Cook J, et al. The temporal dynamics and infectiousness of subpatent Plasmodium falciparum infections in relation to parasite density. Nat Commun. 2019;10:1433.
Das S, Peck RB, Barney R, Jang IK, Kahn M, Zhu M, et al. Performance of an ultra-sensitive Plasmodium falciparum HRP2-based rapid diagnostic test with recombinant HRP2, culture parasites, and archived whole blood samples. Malar J. 2018;17:118.
Jimenez A, Rees-Channer RR, Perera R, Gamboa D, Chiodini PL, González IJ, et al. Analytical sensitivity of current best-in-class malaria rapid diagnostic tests. Malar J. 2017;16:128.
Slater HC, Ding XC, Knudson S, Bridges DJ, Moonga H, Saad NJ, et al. Performance and utility of more highly sensitive malaria rapid diagnostic tests. BMC Infect Dis. 2022;22:121.
Danwang C, Kirakoya-Samadoulougou F, Samadoulougou S. Assessing field performance of ultrasensitive rapid diagnostic tests for malaria: a systematic review and meta-analysis. Malar J. 2021;20:245.
Yimam Y, Mohebali M, Abbaszadeh Afshar MJ. Comparison of diagnostic performance between conventional and ultrasensitive rapid diagnostic tests for diagnosis of malaria: a systematic review and meta-analysis. PLoS ONE. 2022;17: e0263770.
WHO. Technical consultation on research requirements to support policy recommendations on highly sensitive point-of-care diagnostics for P. falciparum malaria. Geneva: World Health Organization; 2018. https://www.who.int/publications/m/item/WHO-CDS-GMP-MPAC-2018.17
Rogier E, Plucinski M, Lucchi N, Mace K, Chang M, Lemoine JF, et al. Bead-based immunoassay allows sub-picogram detection of histidine-rich protein 2 from Plasmodium falciparum and estimates reliability of malaria rapid diagnostic tests. PLoS ONE. 2017;12: e0172139.
Martiáñez-Vendrell X, Jiménez A, Vásquez A, Campillo A, Incardona S, González R, et al. Quantification of malaria antigens PfHRP2 and pLDH by quantitative suspension array technology in whole blood, dried blood spot and plasma. Malar J. 2020;19:12.
Briand V, Cottrell G, Tuike Ndam N, Martiáñez-Vendrell X, Vianou B, Mama A, et al. Prevalence and clinical impact of malaria infections detected with a highly sensitive HRP2 rapid diagnostic test in Beninese pregnant women. Malar J. 2020;19:188.
Unwin VT, Ahmed R, Noviyanti R, Puspitasari AM, Utami RAS, Trianty L, et al. Use of a highly-sensitive rapid diagnostic test to screen for malaria in pregnancy in Indonesia. Malar J. 2020;19:28.
Ter Kuile F. Intermittent screening and treatment or intermittent preventive therapy for the control of malaria in pregnancy in Indonesia (STOPMiP-Indonesia). https://mesamalaria.org/mesa-track/intermittent-screening-and-treatment-or-intermittent-preventive-therapy-control-malaria. Accessed: 1 Feb 2022
Samuels A, Towett O, Seda B, Wiegand RE, Otieno K, Chomba M, et al. Diagnostic performance of loop-mediated isothermal amplification and ultra-sensitive rapid diagnostic tests for malaria screening among pregnant women in Kenya. J Infect Dis. 2022;226:696–707.
Vásquez AM, Medina AC, Tobón-Castaño A, Posada M, Vélez GJ, Campillo A, et al. Performance of a highly sensitive rapid diagnostic test (HS-RDT) for detecting malaria in peripheral and placental blood samples from pregnant women in Colombia. PLoS ONE. 2018;13: e0201769.
Vásquez AM, Vélez G, Medina A, Serra-Casas E, Campillo A, Gonzalez IJ, et al. Evaluation of highly sensitive diagnostic tools for the detection of P. falciparum in pregnant women attending antenatal care visits in Colombia. BMC Pregnancy Childbirth. 2020;20:440.
Kattenberg JH, Ochodo EA, Boer KR, Schallig HD, Mens PF, Leeflang MM. Systematic review and meta-analysis: rapid diagnostic tests versus placental histology, microscopy and PCR for malaria in pregnant women. Malar J. 2011;10:321.
Okell LC, Ghani AC, Lyons E, Drakeley CJ. Submicroscopic infection in Plasmodium falciparum—endemic populations: a systematic review and meta-analysis. J Infect Dis. 2009;200:1509–17.
Cheng Q, Gatton ML, Barnwell J, Chiodini P, McCarthy J, Bell D, et al. Plasmodium falciparum parasites lacking histidine-rich protein 2 and 3: a review and recommendations for accurate reporting. Malar J. 2014;13:283.
Institut de Recherche en Sciences de la Santé, Burkina Faso. Additional screening with sensitive RDTs and malaria (ASSERMalaria). https://clinicaltrials.gov/ct2/show/NCT04147546. Accessed: 1 Feb 2022
Singh N, Bharti PK, Singh MP, Singh R, Yeboah-Antwi K, Desai M, et al. What is the burden of submicroscopic malaria in pregnancy in central India? Pathog Glob Health. 2015;109:30–8.
Cohee LM, Kalilani-Phiri L, Boudova S, Joshi S, Mukadam R, Seydel KB, et al. Submicroscopic malaria infection during pregnancy and the impact of intermittent preventive treatment. Malar J. 2014;13:274.
Taylor SM, Madanitsa M, Thwai KL, Khairallah C, Kalilani-Phiri L, van Eijk AM, et al. Minimal impact by antenatal subpatent Plasmodium falciparum infections on delivery outcomes in Malawian women: a cohort study. J Infect Dis. 2017;216:296–304.
Williams JE, Cairns M, Njie F, Laryea Quaye S, Awine T, Oduro A, et al. The performance of a rapid diagnostic test in detecting malaria infection in pregnant women and the impact of missed infections. Clin Infect Dis. 2016;62:837–44.
FIND. Clinical Performance of the Histidine Rich Protein 2 (HRP2) highly sensitive rapid diagnostic test (HS-RDT) for malaria diagnosis in pregnant women in Papua New Guinea. Geneva: Foundation for Innovative New Diagnostics; 2018. https://clinicaltrials.gov/ct2/show/NCT03462615?term=RDT%2C+pregnancy&cond=Malaria&draw=2&rank=3. Accessed: 1 Feb 2022
IMPROVE trial. https://www.improve-consortium.org/projects/improve-trial. Accessed 20 Jul 2021.
Gutman J, Mathanga D. IPTp study: highly-sensitive RDT diagnostic efficacy in placental blood. MESA track. https://mesamalaria.org/mesa-track/iptp-study-highly-sensitive-rdt-diagnostic-efficacy-placental-blood Accessed: 1 Feb 2022
Efficacy and safety of IPTp-DP versus IPTp-SP in Malawi (STOPMIP-MW). clinicaltrials.gov. https://clinicaltrials.gov/ct2/show/NCT03009526. Accessed: 1 Feb 2022
Maketa V. Comparison of ISTp- PYRAMAX-US-RDT to IPTp-SP to prevent malaria in pregnant women in DRC (ULTRAPYRAPREG). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT04783051?term=pregnancy&cond=Malaria&cntry=CD&draw=2&rank=1. Accessed: 1 Feb 2022
Acknowledgements
All respondents to the stakeholder surveys, and study PIs for verifying the accuracy of the reported data.
Funding
FIND received funding for evidence generation and collation from the Bill and Melinda Gates Foundation and the Australian government.
Author information
Authors and Affiliations
Contributions
XD, SI, SD conceptualized the study. ESC, SCC, HCS, GJD, ERA, FOK, AMS collected, collated, analysed, and visualized the data. ESC and SCC wrote early drafts of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Testing characteristics of the completed studies evaluating the use of the HS-RDT for the detection of MiP. Table S2. True and False positives and negatives by study. Figure S1. Sensitivity of the HS-RDT and parasite density of the maternal infections detected by the reference standard in each study. Densities represented as geometrical mean + confidence interval (p/μL). Figure S2. Sensitivity of HS-RDT at delivery in peripheral and placental blood.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ding, X.C., Incardona, S., Serra-Casas, E. et al. Malaria in pregnancy (MiP) studies assessing the clinical performance of highly sensitive rapid diagnostic tests (HS-RDT) for Plasmodium falciparum detection. Malar J 22, 60 (2023). https://doi.org/10.1186/s12936-023-04445-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-023-04445-1