Abstract
Background
Long-lasting insecticidal nets (LLINs) have been the primary vector control strategy until indoor residual spraying (IRS) was added in Homa Bay and Migori Counties in western Kenya. The objective of this study was to evaluate the impact of LLINs integrated with IRS on the prevalence of asymptomatic and submicroscopic Plasmodium infections in Homa Bay County.
Methods
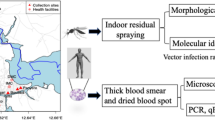
A two-stage cluster sampling procedure was employed to enroll study participants aged ≥ 6 months old. Four consecutive community cross-sectional surveys for Plasmodium infection were conducted in residents of Homa Bay county, Kenya. Prior to the start of the study, all study households received LLINs, which were distributed between June 2017 and March 2018. The first (February 2018) and second (June 2018) surveys were conducted before and after the first round of IRS (Feb–Mar 2018), while the third (February 2019) and fourth (June 2019) surveys were conducted before and after the second application of IRS (February–March 2019). Finger-prick blood samples were obtained to prepare thick and thin smears for microscopic determination and qPCR diagnosis of Plasmodium genus.
Results
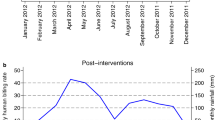
Plasmodium spp. infection prevalence by microscopy was 18.5% (113/610) before IRS, 14.2% (105/737) and 3.3% (24/720) after the first round of IRS and 1.3% (11/849) after the second round of IRS (p < 0.0001). Submicroscopic (blood smear negative, qPCR positive) parasitaemia reduced from 18.9% (115/610) before IRS to 5.4% (46/849) after IRS (p < 0.0001). However, the proportion of PCR positive infections that were submicroscopic increased from 50.4% (115/228) to 80.7% (46/57) over the study period (p < 0.0001). Similarly, while the absolute number and proportions of microscopy positives which were asymptomatic decreased from 12% (73/610) to 1.2% (9/849) (p < 0.0001), the relative proportion increased. Geometric mean density of P. falciparum parasitaemia decreased over the 2-year study period (p < 0.0001).
Conclusions
These data suggest that two annual rounds of IRS integrated with LLINs significantly reduced the prevalence of Plasmodium parasitaemia, while the proportion of asymptomatic and submicroscopic infections increased. To reduce cryptic P. falciparum transmission and improve malaria control, strategies aimed at reducing the number of asymptomatic and submicroscopic infections should be considered.
Similar content being viewed by others
Background
Despite increased malaria control interventions, malaria morbidity and mortality remain high, making the disease a major public health concern in sub-Saharan Africa [1,2,3]. Out of the 229 million malaria cases in 2019, 94% of them were from sub-Saharan Africa. In Kenya, malaria remains a major public health challenge, with approximately 70% of the population at risk, resulting in about 13–15% of outpatient consultations [4]. Malaria transmission is perennial with parasite prevalence consistently above 20% in the Lake Victoria Basin region [5,6,7]. Morbidity and mortality mostly in young children and pregnant women remains prevalent along the lake region [5, 6]. Plasmodium falciparum is the most abundant species (92%) accompanied by Plasmodium malariae (6%) and Plasmodium ovale at 2% [8].
The fight against malaria has been scaled up along the Lake Victoria Basin region, where the infection rates remain high. For instance, mass distribution of LLINs occurs every 3 years [9]. Besides, indoor residual spraying (IRS) was initiated in 2008 [10], but due to reports of emerging resistance to pyrethroid insecticides by malaria vectors, IRS was suspended in endemic parts of Kenya in 2012 [5, 6, 11]. Since then, Kenya has relied on long-lasting insecticidal nets as the primary vector control until February 2018 when IRS was re-introduced using Actellic 300 CS, an organophosphate insecticide. These control strategies toward malaria in Kenya have been intensified to minimize malaria burden in most affected regions. However, this may be undermined by the residual proportions of both asymptomatic and submicroscopic Plasmodium infections in low transmission areas [12, 13]. These infections act as major reservoirs of malaria parasites, thus will sustain transmission. Therefore, formulation of sustainable control strategies to mitigate challenges fueling transmission is very critical and should be regarded as a priority investment.
While the impact of long-lasting insecticidal nets on malaria has been well documented in western Kenya, little is known on the impacts of the addition of IRS on parasite profiles at the population level. Therefore, a study targeting the entire community to identify the prevalence of malaria parasites, asymptomatic and submicroscopic infections was undertaken before the application of indoor residual spraying (IRS, Actellic 300 CS) and during IRS intervention period. Highly sensitive molecular tools were used to detect submicroscopic parasites and improve species identification. Results of this study will guide policy makers in the health, and other concerned stakeholders with regard to enhanced malaria control and management.
Methods
Study site
The study was undertaken in Rachuonyo South and Rangwe sub-counties of Homa Bay County, Kenya located at 0o15′–0o52′ South latitude and 34°–35° east longitude. The area has two rainy seasons: “long rains” (April–July) and “short rains” (September–November). Annual rainfall is 250 to 1000 mm. The study area is comprised of irrigated and non-irrigated settings. In irrigated area, a concrete channel based multi-crop irrigation scheme was constructed in 2012 to boost subsistence farming. Non-irrigated areas are located 5–10 km away from irrigated areas as indicated in Fig. 1. Between June 2017 and March 2018, the Kenyan Ministry of Health distributed long-lasting insecticidal nets (LLINs) to all malaria endemic and epidemic areas [9]. Following the mass distribution campaign, approximate 85% of all households in the Lake Victoria Basin region owned at least one LLINs [9]. In addition to LLINs, the Ministry implemented annual IRS with the organophosphate pirimiphos methyl 300 CS for concerted malaria vector control in February–March 2018, 2019 and 2020 [10, 14]. Before the introduction of IRS, the Kenyan Ministry of Health estimated the annual P. falciparum infection prevalence was 27% [6].
Sample size determination
The formula proposed by Naing et al. [15] was used to determine sample size. Briefly, assuming malaria prevalence (p) of 27% [6], precision (d) of 0.05 and level of confidence (z) as 1.96, the minimum number of study participants needed was 303. This was arrived at as follows:
Due to the cluster sampling procedure, the sample size was multiplied by a design effect as proposed by Cochran [16]. The design effect in most cluster surveys has been reported to be 2 [17] Hence, the minimum number of study participants required was 606. To prevent survey attrition, we decided to recruit 4 participants per family because the average number per household was 4.4, resulting in 80 individuals per cluster and 960 for the entire study region. However, only 610, 737, 720, and 849 participants were tested during the first, second, third and fourth surveys, respectively, due to participants’ unavailability during surveys.
Cross-sectional surveys
Four community cross-sectional surveys were conducted from February 2018 to June 2019. The first survey was in February 2018 before the first IRS, and the second in June 2018. A similar schedule was executed in 2019 before and after the second IRS. Selection for study participation was based on a two-stage procedure similar to that described by Galway et al. [18]. The first stage involved identification of clusters (essentially villages) as primary sampling units. For example, with the help of chiefs and village heads the study team identified the total number of clusters (30). Based on the number of participants required, 12 clusters were randomly selected from the previously identified 30 clusters. In the second stage, the total number of households in each cluster was determined and assigned unique identification numbers. Twenty households from each cluster were then randomly selected provided the household head accepted to participate. The study team recruited 80 permanent dwellers from each cluster. In every household, 4 participants, aged 6 months and above, who were permanent dwellers and who were willing to participate and sign the informed consent or assent forms (for participants < 18 years), were recruited. In case there were more than 4 eligible participants in a household, the 4 participants were randomly selected. However, in households with less than 4 eligible participants, the next household was selected. A questionnaire was used to collect information such as gender, age and body temperature. An infrared thermometer was aimed at the forehead to capture the body temperature. Individuals who had a fever in the previous 48 h were also recorded in the questionnaire. During the survey period, any study participant who had a fever or tested positive for Plasmodium infection was referred to the nearest health center for further examination and treatment.
Sample collection and microscopic examination
Finger-prick blood samples were obtained from study participants to screen for Plasmodium infections by microscopy. Briefly, thick and thin blood smears were stained with 10% Giemsa for 15 min and examined using a microscope. A total of 200 microscopic fields containing leukocytes in the thick smear were examined before declaring a slide negative. For quality control, each slide was examined by two independent microscopists, In the case of discrepancy, a third reader was involved. To estimate the P. falciparum density, the number of parasites observed in microscopic fields containing based on the 200 leucocytes on a thick smear. This number was then multiplied by 40 assuming 8000 leukocytes/µL blood [19]. The parasite density was further classified as either low (< 1000 parasites/µL), moderate (1000–4999 parasites/µL), high (5000–99,999 parasites/µL) or hyperparasitaemia (≥ 100,000 parasites/µL) [20].Gametocyte density was also estimated by counting gametocytes against 500 leukocytes in thick smear [21]. This was then converted to gametocytes/µl of blood by multiplying with the standard count of 8000 white blood cells/µl.
DNA extraction and qPCR detection of parasite infections
Dry blood spots were collected from study participants as described (Wampfler et al. [22]). Briefly, 50 µL of finger-prick blood was spotted on Whatman® 3MM filter paper (3 spots). Filter paper was air dried and kept at 4 °C in sealed plastic bags with a desiccant. DNA was extracted from each filter paper using Chelex resin (chelex -100) as described previously [23] with minor modifications [24]. The study focused on examination of the three Plasmodium species (P. falciparum, P. malariae, and P. ovale) since they had been previously reported as the most possible species to exist in study area [8]. Malaria parasite detection was performed on all extracted DNA (all blood smear positives and negatives) using multiplex real-time PCR (qPCR) targeting 18S rRNA gene as described elsewhere [25, 26] with modifications. Briefly, the probes and primers of three species (P. falciparum, P. malariae, and P. ovale) were used for multiplex qPCR. The qPCR was run on the Applied Biosystems QuantStudio 3 Real-Time PCR System (Thermo Fisher Scientific Inc. USA) in a final volume containing 6 µl of PerfeCTa® qPCR ToughMix™, Low ROX™ Master mix (2X), 0.4 µl of the species specific forward and reverse primers (10 µM), 0.5 µl of the species-specific probe, 0.1 µl of double-distilled water and 2 µl of sample DNA. The thermo profile was set as follows; 50 °C for 2 min, (95 °C for 2 min, 95 °C for 3 s and 58 °C for 30 s) for 45 cycles.
Data analysis
An asymptomatic infection was defined as a Plasmodium positive test result with the body temperature below 37.5 °C during the time of blood sample collection or in the last 48 h. Blood samples testing negative by microscopy but positive by qPCR were considered to be submicroscopic. All data collected was entered in Excel spreadsheet, cleaned and malaria prevalence from the study area analysed using GraphPad Prism version 8. Differences in prevalence among 4 cross-sectional surveys and age sets were determined using inferential statistics (Pearson χ2). Parasite densities were logarithm-transformed (log (x + 1) and mean difference among age groups or survey periods determined using analysis of variance (ANOVA).
Results
Demographic characteristics of participants
The study team approached 600 households in the study area during the recruitment stage. However, 42 household heads refused to participate, and 70 household stated that they did not have LLINs and were, therefore, excluded. A total of 240 households were chosen at random from the remaining 498 households to participate in the study. These 240 households had a total population of 1060 people. However, 24 of them refused to participate, 40 children under the age of 6 months were excluded, and 36 people from households with more than 4 eligible participants were also excluded. Finally, the total number of participants who met the inclusion criteria was 960 as indicated in Fig. 2. Due to unavailability of participants during surveys, the participants who were tested for Plasmodium species infections during the first, second, third, and fourth survey, were 610, 737, 720, and 849 study participants respectively. Age group distribution during the survey period are shown in Table 1.
Parasite prevalence
During the first survey (dry season), conducted in February 2018, the parasite prevalence by microscopy and qPCR was 18.5% (113/610) and 37.4% (228/610), respectively. A significant reduction in prevalence was recorded during the second cross-sectional survey (wet season) by both microscopy and qPCR. For instance, parasite prevalence reduced to 14.2% (105/737) (χ2 = 5.117, df = 1, p = 0.02) by microscopy and 25.1% (185/737) (χ2 = 23.08, df = 1, p < 0.0001) by qPCR. Further decline in parasite prevalence was reported in the third survey with microscopy and qPCR recording 3.3% (24/720) and 10.4% (75/720) respectively. During the last survey, malaria parasite prevalence was finally reduced to 1.3% (11/849) and 6.7% (57/849) by microscopy and qPCR respectively. Overall, the reduction in parasite prevalence during the 4 cross-sectional surveys was significant by microscopy (χ2 = 186.9, df = 3, p < 0.0001) and by qPCR (χ2 = 266.2, df = 3, p < 0.0001) as indicated in Table 1.
Parasite prevalence as determined by both microscopy and qPCR, varied significantly among age groups during the first, second and third survey. For instance, during the first survey, Plasmodium infection rate among participants aged < 5, 5–14 and ≥ 15 years old by microscopy was 24% (23/96), 28.1% (59/210), and 10.2% (31/304), respectively (χ2 = 28.6, df = 2, p < 0.0001). During the second survey, parasite prevalence among children aged below 5, 5–14 and those aged ≥ 15 years was 15.8% (22/139), 20.7% (59/285), and 7.7% (24/313), respectively (χ2 = 25.1, df = 2, p < 0.0001). Similarly, during the third survey, Plasmodium infection rate among < 5, 5–14, and ≥ 15 years old was 2.4% (4/163), 6% (15/250) and 1.6% (5/307), respectively (χ2 = 8.6, df = 2, p = 0.01). However, during the fourth survey, the parasite prevalence among < 5, 5–14, and ≥ 15 years old was 1.4% (2/144), 2.3% (6/260), and 0.7% (3/445), respectively (χ2 = 1.9, df = 2, p = 0.39) (Fig. 3). A similar pattern of variation in parasite prevalence among age groups was recorded by qPCR during the 4 cross-sectional surveys as shown in Fig. 3A.
Plasmodium falciparum parasite density and category
The 4 cross-sectional surveys indicated significant reductions in parasite burden among the study population. The overall geometric mean parasite densities (GMPD) during first, second, third and fourth survey were 2229 infected red blood cells (irb)/µl, 353 irb/µl, 578 irb/µl and 184 irb/µl, respectively (ANOVA, F = 28.95, df = 3, 243, p < 0.0001) (Table 1). Geometric mean parasite density varied significantly among age groups during the first (ANOVA, F = 4.142, df = 2, 110, p = 0.018) and the third survey (ANOVA, F = 5.463, df = 2, 21, p = 0.012 (Fig. 3B). During the first and third surveys, children aged below 5 years old, had highest mean parasite densities compared to other age groups. However, during the second and fourth surveys, geometric mean parasite density did not vary significantly among age groups (ANOVA, F = 1.361, df = 2, 96, p = 0.26) and (ANOVA, F = 0.67, df = 2, 8, p = 0.54), respectively. The parasite density during each survey was categorized into low, moderate, high and hyperparasitaemia. The findings indicated elimination of high and hyperparasitaemia during the 4 cross-sectional surveys. For example, the study reported zero prevalence rates of hyperparasitaemia during the second, third and the fourth survey. Equally, during survey 3 and 4, there were no cases of high parasite density. With the onset of indoor residual spray program, most infections were due to low parasite densities as illustrated in Table 1.
Plasmodium species distribution and P. falciparum gametocyte prevalence
Three malaria species were found in the study population with P. falciparum being most prevalent, followed by P. malariae and P. ovale as the least prevalent, as shown in Table 1. Both P. malariae and P. ovale occurred at low parasite densities hence mostly detected by PCR. Considering the prevalence of mono-infections during the 4 cross-sectional surveys, Plasmodium falciparum accounted for 94.3% (215/228), 81.6% (151/185), 68% (51/75) and 87.7% (50/57) of all infections during the first, second, third and fourth survey respectively. Similarly, the proportion of P. malariae during survey 1, 2, 3 and 4 was 0.9% (2/228), 8.6% (16/185), 10.7% (8/75) and 1.8% (1/57) respectively. The infections due to P. ovale only occurred during the first (0.4% (1/228), second (1.6% (3/185), and fourth survey (5.3% (3/57). Mixed species infections due to P. falciparum and P. malariae mostly occurred throughout the study period. Mixed infections involving P. ovale were rare and were reported during the first and second surveys, as illustrated in Table 2 below. Results further indicated lowest levels of gametocyte prevalence during survey periods. The declining trend of gametocyte prevalence was 1.3% (8/610), 0.5% (4/737), 0.14% (1/720) and 0.12% (1/849) during the first, second, third and the fourth survey respectively (χ2 = 12.97, df = 3, p = 0.005). The geometric mean gametocyte density was: 66.6, 35.9, 48 and 16 gametocytes/µl of blood during survey 1, 2, 3 and 4 respectively (ANOVA, F = 1.24, df = 3, 10, p = 0.35).
Submicroscopic, asymptomatic and symptomatic Plasmodium infections
The absolute numbers of submicroscopic (qPCR positive alone) infections decreased during the four cross-sectional studies. For instance, the proportion of submicroscopic infections was 18.9% (115/610), 10.9% (80/737), 7.1% (51/720), and 5.4% (46/849) (χ2 = 80.2, df = 3, p < 0.0001) for the first, second, third and fourth surveys, respectively (Fig. 4). However, the relative proportion of submicroscopic infections increased during the four cross-sectional surveys. For example, the proportion of PCR positive infections that were submicroscopic increased from 50.4% (115/228) to 80.7% (46/57) over the study period (χ2 = 31.98, df = 3, p < 0.0001).
The rate of symptomatic infections as determined by microscopy decreased during the survey period. For instance, the rate of microscopy positive that were symptomatic during the first, second, third, and fourth surveys, was 6.6% (40/610), 4.6% (44/737), 0.8% (6/720), and 0.2% (2/849), respectively (χ2 = 78.6, df = 3, p < 0.0001) (Fig. 4). Similarly, the absolute numbers of microscopy positive that were asymptomatic during surveys 1,2,3 and 4, decreased from 12% (73/610) to 1.2% (9/849) (χ2 = 110.4, df = 3, p < 0.0001).. However, the relative proportions of microscopy positive that were asymptomatic increased from 64.6% (73/113) to 83.3% (9/11) (χ2 = 1.349, df = 3, p = 0.7). The detection of Plasmodium species infection rate by qPCR was significantly higher than that of microscopy as illustrated in Fig. 5.
Discussion
This study was undertaken to document the impact of IRS and LLINs on parasitological profiles of malaria parasites in a human population in an endemic site in western Kenya. Accurate determination of Plasmodium infection rates is key towards monitoring the progress of malaria intervention programmes initiated within endemic regions [27]. To accurately document malaria prevalence rates within populations, more sensitive detection tools are essential. This will help detect infections including those with very low parasite densities which mostly go undetected by microscopy [28]. The present study investigated the prevalence rates of malaria parasites, asymptomatic and submicroscopic Plasmodium infections before the introduction of IRS and during two rounds of IRS in an area where LLINs were widely used. Four cross-sectional surveys were conducted and findings indicated a sustained reduction in Plasmodium infection rates especially after the rollout of IRS programme. Just before the onset of IRS, the Plasmodium prevalence rate by both microscopy and qPCR was at 18.5% and 37.4%, respectively. However, during the last survey, the prevalence of malaria parasites had declined to 1.3% by microscopy and 6.7% by qPCR.
The geometric mean parasite density significantly declined from 2229 parasites/µl of blood before intervention to 184 parasites/µl of blood after 2 rounds of IRS. The most plausible explanation to such a drastic reduction in parasite prevalence and parasite density could be due to very low parasite transmission after the application of IRS. For instance, in a neighboring Migori county, where a similar intervention was initiated, malaria transmission was reported to have declined significantly [29]. Furthermore, in Uganda [30], Mali [31] and Tanzania [32, 33] where IRS was initiated as a vector control strategy, the Plasmodium infection rate and parasite density decreased significantly.
Parasite prevalence determined by both microscopy and qPCR were reported to be highest among the age group 5–14 years old. This is in agreement with other previous studies [34,35,36]. A likely explanation to this trend has been highlighted in past studies [37,38,39]. For instance, majority in this age group are not under direct care of parents as compared to under 5 years old. They tend to be independent and most often may not sleep under bed nets or nets poorly placed, leaving them vulnerable to infectious mosquito bites. Poor health-seeking pattern has also been reported as a possible challenge in this age group, leading to more parasite infections [40], possibly because they have mild clinical symptoms. Unlike parasite prevalence, parasite density was highest in children under the age of 5, but decreased with age. Antiparasitic immunity develops with age, providing protection against high malaria parasite density [41, 42]. Due to repeated Plasmodium infections, older children, for example, develop an improved immune response that significantly suppresses the multiplication of asexual parasites.
The prevalence of asymptomatic and symptomatic cases decreased during the study period. This could be due to sustained malaria vector control in the study area through the use of IRS and LLINs. It was important to note, however, that the relative proportions of microscopy positives that were asymptomatic increased with each subsequent survey. This observed trend could be explained by a significant decrease in parasite prevalence and density. For example, the study revealed a complete elimination of hyperparasitaemia and high parasite density infections during the third and fourth survey. Likewise, there was a significant decrease in infections with moderate parasitaemia. As a result, the few existing Plasmodium infections with low parasite densities may be easily tolerated, increasing the number of asymptomatic cases. Similarly, the current study area has historically been a malaria endemic region. Areas undergoing perennial Plasmodium infections endure elevated rates of asymptomatic infections [43, 44]. This is due to increased tolerance towards parasite density [45]. Frequent exposure to Plasmodium infections may trigger strong immune modulation resulting in reduced clinical symptoms [46,47,48,49]. However, rising asymptomatic rates are likely to negate the gains and jeopardize vector control efforts in the study area.
The absolute number of submicroscopic infections decreased with decrease in Plasmodium infection rate. However, the relative proportion of submicroscopic infections increased during study period. As the parasite densities decrease, submicroscopic infections may increase due to microscopy’s low detection limit [12, 27]. This is comparable to previous studies, which reported high submicroscopic infections in low-transmission settings [50]. Submicroscopic infections are of public health interest as they pose serious health challenge to pregnant women [51] as well as causing mild anaemia [52]. The prevalence and density of gametocytes were extremely low and steadily declined with subsequent surveys. Although infectious gametocyte carriage is modulated by a variety of factors including immune response, treatment, and transmission intensity [53], the current study’s reduced levels of gametocytes could be attributed to a sustained vector control programme within the study area.
Plasmodium species detected in the current study varied with P. falciparum accounting for the highest proportions. This is consistent with other observations along the lake region, western Kenya [34, 54]. The study further reported existence of P. malariae and P. ovale. While the number of P. falciparum infection cases reduced, the proportion of P. malariae cases remained relatively stable over the course of four surveys. Most importantly, these P. malariae infections occurred at very minimal parasite densities, hence the majority of cases were diagnosed using qPCR. This is similar to a previous study which reported subpatent P. malariae with low parasite densities [55]. Low parasite density in P. malariae infections may be a challenge to microscopy based diagnosis leading to misdiagnosis or underreporting of malaria cases [55]. Accurate detection and treatment of P. malariae infections is paramount to minimize cases of nephrotic syndrome, which are associated with excessive mortality [56].
Detection rate of Plasmodium species by qPCR was significantly higher compared to that of microscopy. This is consistent with previous studies which compared the two diagnostic tools [57, 58]. Molecular based detection tools are known to be very sensitive hence able to identify cases with lowest parasite densities [59, 60]. Highly sensitive detection tools may be useful especially in settings where submicroscopic infections or co-infections with low parasite density P. malariae are common.
The study was limited to two sub-counties, hence the findings cannot not be generalized to the entire county. Besides, the study did not include the Plasmodium infection rate prior to net interventions. Finally, due to the study's cross-sectional design, it was difficult to directly link the lower Plasmodium infections to LLINs and IRS interventions.
Conclusion
The study findings report significant reduction in Plasmodium infection rates and parasite densities following the introduction of the indoor residual spray programme. The reports also show that, while the absolute number of asymptomatic and submicroscopic infections decreased in the study area, the relative proportion of both asymptomatic and submicroscopic infections increased. This is likely to negate the progress achieved towards vector control. The study also demonstrated a large reduction in clinical malaria, which is an important public health benefit.
Availability of data and materials
The dataset used in this study is available from the corresponding author upon reasonable request.
Abbreviations
- LLINs:
-
Long-lasting insecticidal nets
- IRS:
-
Indoor residual spray
- DNA:
-
Deoxyribonucleic acid
- qPCR:
-
Qualitative polymerase chain reaction
- ICEMR:
-
International center of excellence for malaria research
- MoH:
-
Ministry of Health
References
Ochwedo KO, Omondi CJ, Magomere EO, Olumeh JO, Debrah I, Onyango SA, et al. Hyper-prevalence of submicroscopic Plasmodium falciparum infections in a rural area of western Kenya with declining malaria cases. Malar J. 2021;20:472.
Otambo WO, Omondi CJ, Ochwedo KO, Onyango PO, Atieli H, Lee MC, et al. Risk associations of submicroscopic malaria infection in lakeshore, plateau and highland areas of Kisumu County in western Kenya. PLoS ONE. 2022;17: e0268463.
WHO. World malaria report. 20 years of global progress and challenges. Geneva: World Health Organization; 2020. p. 2020.
MoH. Kenya malaria indicator survey 2020. Nairobi, Kenya and Rockville, Maryland, USA: DNMP and ICF: Division of National malaria programme, 2021.
Bashir IM, Nyakoe N, van der Sande M. Targeting remaining pockets of malaria transmission in Kenya to hasten progress towards national elimination goals: an assessment of prevalence and risk factors in children from the Lake endemic region. Malar J. 2019;18:233.
MoH. Malaria indicator survey 2015. Nairobi: National malaria control; 2016.
Otambo WO, Olumeh JO, Ochwedo KO, Magomere EO, Debrah I, Ouma C, et al. Health care provider practices in diagnosis and treatment of malaria in rural communities in Kisumu County, Kenya. Malar J. 2022;21:129.
MoH. Malaria epidemiology and control profile of malaria in Kenya: reviewing the evidence to guide the future vector control Nairobi, Kenya. Kenya: Ministry of Health; 2016.
MoH. Post mass long Lasting Insecticidal nets survey; 2018. Nairobi: Kenya Ministry of Health, Division of National malaria programme; 2019.
PMI. Kenya end of spray report 2018. Rockville: The PMI Africa IRS; 2018.
Ochomo E, Bayoh NM, Kamau L, Atieli F, Vulule J, Ouma C, et al. Pyrethroid susceptibility of malaria vectors in four districts of Western Kenya. Parasit Vectors. 2014;7:310.
Bousema T, Okell L, Felger I, Drakeley C. Asymptomatic malaria infections: detectability, transmissibility and public health relevance. Nat Rev Microbiol. 2014;12:833–40.
Almeida ACG, Kuehn A, Castro AJM, Vitor-Silva S, Figueiredo EFG, Brasil LW, et al. High proportions of asymptomatic and submicroscopic Plasmodium vivax infections in a peri-urban area of low transmission in the Brazilian Amazon. Parasit Vectors. 2018;11:194.
PMI. Kenya end of spray report 2020: Spray campaign Rockville, MD, USA: The PMI vector link project, Abt Associates Inc., 2020.
Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Arch Orofacial Sci. 2006;1:9–14.
Cochran WG. Sampling techniques. New York: Wiley; 1997.
Macfarlane SB. Conducting a descriptive surveys: 2. Choosing a sampling strategy. Trop Doctor. 1997;27:8.
Galway L, Bell N, Sae AS, Hagopian A, Burnham G, Flaxman A, et al. A two-stage cluster sampling method using gridded population data, a GIS, and Google Earth (TM) imagery in a population-based mortality survey in Iraq. Int J Health Geogr. 2012;11:12.
McKenzie FE, Prudhomme WA, Magill AJ, Forney JR, Permpanich B, Lucas C, et al. White blood cell counts and malaria. J Infect Dis. 2005;192:323–30.
Chipwaza B, Sumaye RD. High malaria parasitemia among outpatient febrile children in low endemic area, East-Central Tanzania in 2013. BMC Res Notes. 2020;13:251.
Subussa BW, Eshetu T, Degefa T, Ali MM. Asymptomatic Plasmodium infection and associated factors among pregnant women in the Merti district, Oromia, Ethiopia. PLoS ONE. 2021;16: e0248074.
Wampfler R, Mwingira F, Javati S, Robinson L, Betuela I, Siba P, et al. Strategies for detection of Plasmodium species gametocytes. PLoS ONE. 2013;8: e76316.
Wooden J, Kyes S, Sibley CH. PCR and strain identification in Plasmodium falciparum. Parasitol Today. 1993;9:303–5.
Onyango SA, Ochwedo KO, Machani MG, Omondi CJ, Debrah I, Ogolla SO, et al. Genetic diversity and population structure of the human malaria parasite Plasmodium falciparum surface protein Pfs47 in isolates from the lowlands in Western Kenya. PLoS ONE. 2021;16: e0260434.
Veron V, Simon S, Carme B. Multiplex real-time PCR detection of P. falciparum, P. vivax and P. malariae in human blood samples. Exp Parasitol. 2009;121:346–51.
Shokoples SE, Ndao M, Kowalewska-Grochowska K, Yanow SK. Multiplexed real-time PCR assay for discrimination of Plasmodium species with improved sensitivity for mixed infections. J Clin Microbiol. 2009;47:975–80.
Okell LC, Bousema T, Griffin JT, Ouedraogo AL, Ghani AC, Drakeley CJ. Factors determining the occurrence of submicroscopic malaria infections and their relevance for control. Nat Commun. 2012;3:1237.
Wu L, van den Hoogen LL, Slater H, Walker PG, Ghani AC, Drakeley CJ, et al. Comparison of diagnostics for the detection of asymptomatic Plasmodium falciparum infections to inform control and elimination strategies. Nature. 2015;528:S86-93.
Abong’o B, Gimnig JE, Torr SJ, Longman B, Omoke D, Muchoki M, et al. Impact of indoor residual spraying with pirimiphos-methyl (Actellic 300CS) on entomological indicators of transmission and malaria case burden in Migori County, western Kenya. Sci Rep. 2020;10:4518.
Tukei BB, Beke A, Lamadrid-Figueroa H. Assessing the effect of indoor residual spraying (IRS) on malaria morbidity in Northern Uganda: a before and after study. Malar J. 2017;16:4.
Wagman J, Cisse I, Kone D, Fomba S, Eckert E, Mihigo J, et al. Rapid reduction of malaria transmission following the introduction of indoor residual spraying in previously unsprayed districts: an observational analysis of Mopti Region, Mali, in 2017. Malar J. 2020;19:340.
Mashauri FM, Kinung’hi SM, Kaatano GM, Magesa SM, Kishamawe C, Mwanga JR, et al. Impact of indoor residual spraying of lambda-cyhalothrin on malaria prevalence and anemia in an epidemic-prone district of Muleba, north-western Tanzania. Am J Trop Med Hyg. 2013;88:841–9.
Mashauri FM, Manjurano A, Kinung’hi S, Martine J, Lyimo E, Kishamawe C, et al. Indoor residual spraying with micro-encapsulated pirimiphos-methyl (Actellic® 300CS) against malaria vectors in the Lake Victoria basin. Tanzania PLoS One. 2017;12: e0176982.
Idris ZM, Chan CW, Kongere J, Gitaka J, Logedi J, Omar A, et al. High and heterogeneous prevalence of asymptomatic and sub-microscopic malaria infections on Islands in Lake Victoria. Kenya Sci Rep. 2016;6:36958.
Omondi CJ, Onguru D, Kamau L, Nanyingi M, Ong’amo G, Estambale B. Perennial transmission of malaria in the low altitude areas of Baringo County, Kenya. Malar J. 2017;16:257.
Sultana M, Sheikh N, Mahumud RA, Jahir T, Islam Z, Sarker AR. Prevalence and associated determinants of malaria parasites among Kenyan children. Trop Med Health. 2017;45:25.
Desai M, Buff AM, Khagayi S, Byass P, Amek N, van Eijk A, et al. Age-specific malaria mortality rates in the KEMRI/CDC health and demographic surveillance system in western Kenya, 2003–2010. PLoS ONE. 2014;9: e106197.
Gitonga CW, Edwards T, Karanja PN, Noor AM, Snow RW, Brooker SJ. Plasmodium infection, anaemia and mosquito net use among school children across different settings in Kenya. Trop Med Int Health. 2012;17:858–70.
Iwashita H, Dida G, Futami K, Sonye G, Kaneko S, Horio M, et al. Sleeping arrangement and house structure affect bed net use in villages along Lake Victoria. Malar J. 2010;9:176.
Bigogo G, Audi A, Aura B, Aol G, Breiman RF, Feikin DR. Health-seeking patterns among participants of population-based morbidity surveillance in rural western Kenya: implications for calculating disease rates. Int J Infect Dis. 2010;14:e967–73.
Doolan DL, Dobano C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev. 2009;22:13–36.
Moormann AM. How might infant and paediatric immune responses influence malaria vaccine efficacy? Parasite Immunol. 2009;31:547–59.
Badiane AS, Ndiaye T, Thiaw AB, Binta DA, Diallo MA, Seck MC, et al. High prevalence of asymptomatic Plasmodium infection in Bandafassi. South-East Senegal Malar J. 2021;20:218.
Imwong M, Stepniewska K, Tripura R, Peto TJ, Lwin KM, Vihokhern B, et al. Numerical distributions of parasite densities during asymptomatic malaria. J Infect Dis. 2016;213:1322–9.
Ademolue TW, Aniweh Y, Kusi KA, Awandare GA. Patterns of inflammatory responses and parasite tolerance vary with malaria transmission intensity. Malar J. 2017;16:145.
Kamau A, Mtanje G, Mataza C, Mwambingu G, Mturi N, Mohammed S, et al. Malaria infection, disease and mortality among children and adults on the coast of Kenya. Malar J. 2020;19:210.
McQueen PG, Williamson KC, McKenzie FE. Host immune constraints on malaria transmission: insights from population biology of within-host parasites. Malar J. 2013;12:206.
White NJ. Malaria parasite clearance. Malar J. 2017;16:88.
Frosch AE, John CC. Immunomodulation in Plasmodium falciparum malaria: experiments in nature and their conflicting implications for potential therapeutic agents. Expert Rev Anti Infect Ther. 2012;10:1343–56.
Harris I, Sharrock WW, Bain LM, Gray KA, Bobogare A, Boaz L, et al. A large proportion of asymptomatic Plasmodium infections with low and sub-microscopic parasite densities in the low transmission setting of Temotu Province, Solomon Islands: challenges for malaria diagnostics in an elimination setting. Malar J. 2010;9:254.
Arango EM, Samuel R, Agudelo OM, Carmona-Fonseca J, Maestre A, Yanow SK. Molecular detection of malaria at delivery reveals a high frequency of submicroscopic infections and associated placental damage in pregnant women from northwest Colombia. Am J Trop Med Hyg. 2013;89:178–83.
Ladeia-Andrade S, Ferreira MU, de Carvalho ME, Curado I, Coura JR. Age-dependent acquisition of protective immunity to malaria in riverine populations of the Amazon Basin of Brazil. Am J Trop Med Hyg. 2009;80:452–9.
Bousema T, Drakeley C. Epidemiology and infectivity of Plasmodium falciparum and Plasmodium vivax gametocytes in relation to malaria control and elimination. Clin Microbiol Rev. 2011;24:377–410.
Olanga EA, Okombo L, Irungu LW, Mukabana WR. Parasites and vectors of malaria on Rusinga Island, Western Kenya. Parasit Vectors. 2015;8:250.
Mueller I, Zimmerman PA, Reeder JC. Plasmodium malariae and Plasmodium ovale–the “bashful” malaria parasites. Trends Parasitol. 2007;23:278–83.
Eiam-Ong S. Malarial nephropathy. Semin Nephrol. 2003;23:21–33.
Wang B, Han SS, Cho C, Han JH, Cheng Y, Lee SK, et al. Comparison of microscopy, nested-PCR, and Real-Time-PCR assays using high-throughput screening of pooled samples for diagnosis of malaria in asymptomatic carriers from areas of endemicity in Myanmar. J Clin Microbiol. 2014;52:1838–45.
Kang JM, Cho PY, Moe M, Lee J, Jun H, Lee HW, et al. Comparison of the diagnostic performance of microscopic examination with nested polymerase chain reaction for optimum malaria diagnosis in Upper Myanmar. Malar J. 2017;16:119.
Jones S, Sutherland CJ, Hermsen C, Arens T, Teelen K, Hallett R, et al. Filter paper collection of Plasmodium falciparum mRNA for detecting low-density gametocytes. Malar J. 2012;11:266.
Kuamsab N, Putaporntip C, Pattanawong U, Jongwutiwes S. Simultaneous detection of Plasmodium vivax and Plasmodium falciparum gametocytes in clinical isolates by multiplex-nested RT-PCR. Malar J. 2012;11:190.
Acknowledgements
Special thanks goes to the study participants, the community members and their leaders who accepted, participated and supported the study to realize its objectives. We also appreciate the support from the field assistants during data collection and the technical staff. Lastly, we greatly thank the Ministry of Health, Homa Bay county for the permission to carry out this research in this region.
Funding
This study was by grants from the National Institutes of Health (U19 AI129326, D43 TW001505 and R01 AI050243).
Author information
Authors and Affiliations
Contributions
CJO designed the study, collected, analyzed and interpreted the data, drafted and reviewed the manuscript, OD and OA assisted in developing the study design and reviewed the manuscript, WOO, SAO, PO, BMO assisted in data collection, ML drafted the map of study area, CJO, KOO and DZ laboratory analysis and reviewed the manuscript, JWK, AKG and GY helped develop the study design and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was partial of a ICEMR project titled on “Environmental modifications in sub-Saharan Africa: Changing Epidemiology, Transmission and Pathogenesis of Plasmodium falciparum and P. vivax malaria” whose ethical review and approval (MSU/DRPI/MUERC/00456/17) was obtained from Maseno University (Kenya) Ethics and Research Committees and University of California, USA. All study participants signed the informed consent or assent forms.
Consent for publication
Not applicable.
Competing interests
The authors do hereby declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Omondi, C.J., Otambo, W.O., Odongo, D. et al. Asymptomatic and submicroscopic Plasmodium infections in an area before and during integrated vector control in Homa Bay, western Kenya. Malar J 21, 272 (2022). https://doi.org/10.1186/s12936-022-04288-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04288-2