Abstract
Background
In Ethiopia there is no complete registration system to measure disease burden and risk factors accurately. In this study, the 2015 global burden of diseases, injuries and risk factors (GBD) data were used to analyse the incidence, prevalence and mortality rates of malaria in Ethiopia over the last 25 years.
Methods
GBD 2015 used verbal autopsy surveys, reports, and published scientific articles to estimate the burden of malaria in Ethiopia. Age and gender-specific causes of death for malaria were estimated using cause of death ensemble modelling.
Results
The number of new cases of malaria declined from 2.8 million [95% uncertainty interval (UI) 1.4–4.5 million] in 1990 to 621,345 (95% UI 462,230–797,442) in 2015. Malaria caused an estimated 30,323 deaths (95% UI 11,533.3–61,215.3) in 1990 and 1561 deaths (95% UI 752.8–2660.5) in 2015, a 94.8% reduction over the 25 years. Age-standardized mortality rate of malaria has declined by 96.5% between 1990 and 2015 with an annual rate of change of 13.4%. Age-standardized malaria incidence rate among all ages and gender declined by 88.7% between 1990 and 2015. The number of disability-adjusted life years lost (DALY) due to malaria decreased from 2.2 million (95% UI 0.76–4.7 million) in 1990 to 0.18 million (95% UI 0.12–0.26 million) in 2015, with a total reduction 91.7%. Similarly, age-standardized DALY rate declined by 94.8% during the same period.
Conclusions
Ethiopia has achieved a 50% reduction target of malaria of the millennium development goals. The country should strengthen its malaria control and treatment strategies to achieve the sustainable development goals.
Similar content being viewed by others
Background
Ethiopia has registered remarkable progress in reducing the burden of malaria and other major communicable diseases over the last two decades [1, 2]. Over the last decade, the burden of malaria has declined significantly, which could be the result of improved coverage of high impact interventions, such as prompt treatment of cases using artemisinin-based combination therapy (ACT), prevention and control of malaria among pregnant women using intermittent preventive therapy (IPT), use vector control methods including insecticide-treated bed nets (ITNs), and indoor residual spray (IRS) [3,4,5]. Malaria deaths and admissions in children age under-5 fell by 81 and 73%, respectively, after the scale-up of ITNs, IRS and ACT interventions between 2006 and 2011 [4]. However, malaria remains a major health problem for Ethiopia where only 25% of the population live in areas that are free from malaria [6, 7]. It is still among the ten top leading causes of morbidity and mortality in children under-5 years [8].
The World Health Organization (WHO) recently launched the global technical strategy (GTS) for malaria, which aims to reduce the incidence and mortality rates of malaria at least by 90% by 2030 [9]. Reducing the burden of malaria particularly in sub-Saharan Africa is linked to several of the sustainable development goals (SDG) [10]. To achieve the GTS and SDG malaria targets, malaria-endemic countries should have robust surveillance and health management information systems to monitor mortality and incidence rates of malaria [9]. However, Ethiopia, like many of the sub-Saharan African countries, does not strong surveillance and health management information systems to accurately measure mortality and incidence rates of malaria. In this study, the 2015 global burden of diseases, injuries and risk factors (GBD) data [11,12,13,14] were used to measure the incidence, prevalence, mortality, and disability-adjusted life years lost (DALY) rates of malaria during 1990–2015. The study has provided evidence of the performance by Ethiopia on the three MDG diseases and it can serve as a benchmark to track future progress during the SDG era.
Methods
Ethiopia, with a population of nearly 100 million, is the second most populous country in Africa with diverse population mix and unique cultural heritage [1]. Nearly 60% of the Ethiopian population lives in malarious areas and 68% of the country’s landmass is favourable to malaria transmission [15, 16]. Malaria transmission in Ethiopia is seasonal and unstable and peaks of malaria incidence follow the major rainfall season, from July to September [15, 16].
Data sources
The GBD 2015 utilizes comprehensive sources of data and rigorous analysis to estimate trends of cause-specific mortality rates and risk factors for 188 countries [13]. The key sources of data to model the burden of malaria in Ethiopia included verbal autopsy (VA) from the health and demographic surveillance sites (HDSS), Ethiopian Demographic and Health Surveys (EDHS), other surveys such as malaria indicator surveys (MIS) of Ethiopia and Ministry of Health reports submitted to UN agencies and published scientific articles [13].
Causes of death modelling
Causes of death by age groups, gender and year for malaria were measured using ensemble modelling (CODEm). A detailed description of CODEm is reported elsewhere [11, 13, 17, 18]. In brief, CODEm tests a wide range of models, such as mixed effects linear models and spatial–temporal Gaussian process regression (ST-GPR) models and constructs an ensemble model based on the performance of the different models [13]. Out-of-sample predictive validity test was used to select the ensemble model for estimation of mortality rate [13]. In this model, uncertainty intervals (UI) are generated by sampling the posterior distribution of each component model in proportional to the weight of each model in the ensemble. Vital registration and VA data were corrected for garbage codes based on the GBD algorithm [13].
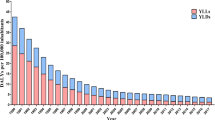
DALY, due to malaria, was measured by summing years of life lost (YLL) due to premature mortality and years lived with disability (YLD), a measure of non-fatal health loss, in a single metric. One DALY can be thought of as one lost year of healthy life. YLL were estimated using standard GBD methods whereby each death is multiplied by the normative standard life expectancy at each age. YLD were estimated using sequelae prevalence and disability weights derived from population-based surveys of the general public to assign disability weights to each sequela and combination of sequelae [19, 20].
Results
The number of new cases of malaria declined from 2.8 million (95% UI 1.4–4.5 million) in 1990 to 621,345 (95% UI 462,230–797,442) in 2015. Age-standardized incidence rate among all ages and gender declined by 88.7% over the 25 years with an annualized rate of change (ARC) of 8.7%. Malaria caused an estimated 30,323.9 deaths (95% UI 11,533.3–61,215.3) in 1990 and 1561.7 deaths (95% UI 752.8–2660.5) in 2015, a 94.8% reduction over the 25 years. Age-standardized mortality rate of malaria has declined by 96.5% between 1990 and 2015 with an ARC of 13.4% (Table 1).
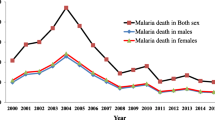
Malaria mortality rate was highest among neonates (7–27 days), post-neonatal infants (28–364 days) and older individuals (≥65 years) and lowest among individuals 10–14 years in both gender (Fig. 1). The reduction of age-standardized incidence and mortality rates of malaria were more marked between 2005 and 2010. Unlike mortality and incidence rates, little reduction (5%) was observed for the age-standardized prevalence rate over the last 25 years (Fig. 2).
The number of DALY due to malaria decreased from 2.2 million (95% UI 0.76–4.7 million) in 1990 to 0.18 million (95% UI 0.12–0.26 million) in 2015 with a total reduction of 91.7%. Similarly, age-standardized DALY rate declined by 94.8% during the same period (Table 1). The reduction of age-standardized DALY rate was marked during 2005 and 2010 (Fig. 3). The age-standardized DALY rate was higher among neonatal and post-neonatal period compared to the other age groups (Fig. 1).
Discussion
The MDG targets of halving mortality rate from malaria by 2015 and efforts to reverse the incidence of this disease have been encouraging globally although there were variations among regions and countries [10]. Ethiopia has shown remarkable progress in reversing the burden and epidemics of malaria in the last two decades. Mortality and incidence rates of malaria declined by 96 and 89%, respectively, between 1990 and 2015.
Other reports also show that Ethiopia has achieved the MDG targets of malaria [1, 6, 21]. The WHO report showed a 50–75% decline in incidence and mortality rates of malaria between 2000 and 2013 [6, 21]. Between 2010 and 2015, malaria incidence and mortality rates, particularly due to Plasmodium falciparum, have declined by more than 50% in Ethiopia [21]. However, Ethiopia still accounts for 6% of malaria cases globally and about 12% of the global cases and deaths due to Plasmodium vivax occurs in Ethiopia [21]. More than 75% of deaths and cases of P. vivax occur in four countries: Ethiopia, Indonesia, India, and Pakistan [21].
The performance of Ethiopia in reducing the burden of malaria and reversing malaria epidemics is better than many sub-Saharan African countries [13]. Several factors could have helped Ethiopia to achieve the MDG targets. Strong government leadership in designing and implementing primary healthcare could have helped [22]. The country has implemented an innovative community-based health service delivery called health extension programme (HEP) since 2003 [22]. The HEP has trained and salaried female healthcare workers who provide basic primary healthcare services at community level. The HEP uses a Family Folder, which is a low cost and high impact health management information system at Kebele (lowest administrative unit) level to monitor the health service delivery and health status of the population. It contains basic household characteristics such as availability of clean drinking water, sanitation, and bed nets to prevent malaria [23]. The HEP and the Family Folder have been instrumental in making health services accessible to the poor [22,23,24]. The marked decline of incidence and mortality rates due to malaria since 2005 could be the effect of the HEP.
On the other hand, the significant decline of malaria incidence and mortality rates could be attributable to the effective implementation of the malaria control strategies at grassroots level. Aregawi et al. shows that malaria cases and deaths in Ethiopia substantially declined after the introduction of ACT and ITNs [4]. However, the malaria control strategy also faces several challenges to achieve WHO’s GTS targets to reduce malaria mortality and incidence rates by at least 90% by 2030 [9]. Some evidence showed that malaria transmission and incidence rate were higher in communities living around hydro-electric dams and irrigation areas in Ethiopia [25,26,27]. The higher prevalence of malaria in 2015 compared to that of the previous years could be the result of high malaria burden in high-risk geographic areas. This might be a challenge for a country that has a development strategy of building irrigation systems and mega-dams [28]. Although evidence shows that malaria mosquitoes are resistant to common insecticides that are used to treat bed nets [29], ITNs are still the main malaria control strategy. Hence, it is timely to consider other innovative approaches and tools to control malaria in Ethiopia. Poor community perception and awareness is also one of the main barriers to control and prevent malaria in Ethiopia which requires effective behavioural change interventions [30].
This study is based on the GBD 2015 which uses comprehensive data sources and rigorous analysis. However, the study has some limitations. First, the use of VA data in mortality estimation may introduce misclassification bias. For instance, VA could over-diagnose malaria cases [31] and exaggerate malaria deaths [32, 33]. Use of published articles could introduce publication bias since unfavorable findings may not be published.
Conclusions
Ethiopia has achieved MDG targets related to malaria. Malaria control and treatment strategies should be intensified during the SDG-era focusing on high-risk groups and geographic areas.
Abbreviations
- ACT:
-
artemisinin-combination therapy
- ARC:
-
annualized rates of change
- CODEm:
-
causes of death ensemble modelling
- DALY:
-
disability-adjusted life years lost
- EDHS:
-
Ethiopian Demographic and Health Survey
- GBD:
-
global burden of diseases
- GTS:
-
global technical strategy for malaria
- HDSS:
-
health and demographic surveillance system
- HEP:
-
health extension programmes
- HEW:
-
health extension workers
- IPT:
-
intermittent preventive therapy
- IRS:
-
indoor residual spray
- ITN:
-
insecticide-treated bed nets
- MDG:
-
millennium development goals
- SDG:
-
sustainable development goals
- VA:
-
verbal autopsy
- WHO:
-
World Health Organization
- YLD:
-
years of lived with disability
- YLL:
-
years of life lost due to premature mortality
References
Federal Democratic Republic of Ethiopia, Ministry of Health. Health sector transformation plan. Addis Ababa. http://www.moh.gov.et/documents/26765/0/Health+Sector+Transformation+Plan/5542a23a-9bc7-46a2-8c1f-8b32c2603208?version=1.0. Accessed 13 Jan 2016.
UNDP. 2014 MDG report-Ethiopia. http://www.et.undp.org/content/ethiopia/en/home/library/mdg/EthiopiaMDG2014.html. Accessed 12 Jan 2016.
Abeku TA, Helinski ME, Kirby MJ, Kefyalew T, Awano T, Batisso E, et al. Monitoring changes in malaria epidemiology and effectiveness of interventions in Ethiopia and Uganda: beyond Garki project baseline survey. Malar J. 2015;14:337.
Aregawi M, Lynch M, Bekele W, Kebede H, Jima D, Taffese HS, et al. Time series analysis of trends in malaria cases and deaths at hospitals and the effect of antimalarial interventions, 2001–2011, Ethiopia. PLoS ONE. 2014;9:e106359.
Yimer F, Animut A, Erko B, Mamo H. Past five-year trend, current prevalence and household knowledge, attitude and practice of malaria in Abeshge, south-central Ethiopia. Malar J. 2015;14:230.
WHO. World Malaria report 2014. Geneva: World Health Organization; http://www.who.int/malaria/publications/world_malaria_report_2014/report/en. Accessed 14 Jan 2016.
Adhanom T, Witten HK, Getachew A, Seboxa T. Malaria. In: Berhane Y, Hailemariam D, Kloos H, editors. The epidemiology and ecology of health and disease in Ethiopia. Addis Ababa: Shama PLC; 2006. p. 556–76.
Deribew A, Tessema GA, Deribe K, Melaku YA, Lakew Y, Amare AT, et al. Trends, causes, and risk factors of mortality among children under 5 in Ethiopia, 1990–2013: findings from the Global Burden of Disease Study 2013. Popul Health Metr. 2016;14:42.
WHO. Global technical strategy for malaria 2016–2030. Geneva: World Health Organization. http://www.who.int/malaria/publications/atoz/9789241564991/en/. Accessed 12 June 2017.
WHO. Health in 2015, from MDG to SDG. Geneva: World Health Organization; 2015. http://apps.who.int/iris/bitstream/10665/200009/1/9789241565110_eng.pdf?ua=1. Accessed 19 Jan 2016).
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128.
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71.
Murray CJ, Ortblad KF, Guinovart C, Lim SS, Wolock TM, Roberts DA, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:1005–70.
Wang H, Liddell CA, Coates MM, Mooney MD, Levitz CE, Schumacher AE, et al. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:957–79.
Ethiopian Public Health Institute. Ethiopian Malaria Indicator Survey 2015. http://www.ephi.gov.et/images/pictures/download2009/MIS-2015-Final-Report-December-_2016.pdf. Accessed 12 June 2017.
Federal Ministry of Health. National strategic plan for malaria prevention, control and elimination in Ethiopia: 2014–2020. Addis Ababa: Addis Ababa; 2014.
Foreman KJ, Lozano R, Lopez AD, Murray CJ. Modeling causes of death: an integrated approach using CODEm. Popul Health Metr. 2012;10:1.
Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–6.
GBD 2013 DALYs and HALE Collaborators, Murray CJ, Barber RM, Foreman KJ, Ozgoren AA, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386:2145–91.
GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603–58.
WHO. World Malaria Report 2016. Geneva: World Health Organization; http://apps.who.int/iris/bitstream/10665/252038/1/9789241511711-eng.pdf?ua=1. Accessed 11 Apr 2016.
Wakabi W. Extension workers drive Ethiopia’s primary health care. Lancet. 2008;372:880.
MEASURE Evaluation. Family folders: low-resource health data with a big impact. http://www.cpc.unc.edu/measure/resources/publications/fs-15-138. Accessed 28 Jan 2016.
Yassin MA, Datiko DG, Tulloch O, Markos P, Aschalew M, Shargie EB, et al. Innovative community-based approaches doubled tuberculosis case notification and improve treatment outcome in Southern Ethiopia. PLoS ONE. 2013;8:e63174.
Deribew A, Birhanu Z, Sena L, Dejene T, Reda AA, Sudhakar M, et al. The effect of household heads training about the use of treated bed nets on the burden of malaria and anaemia in under-five children: a cluster randomized trial in Ethiopia. Malar J. 2012;11:8.
Kibret S, Wilson GG, Ryder D, Tekie H, Petros B. Malaria impact of large dams at different eco-epidemiological settings in Ethiopia. Trop Med Health. 2017;45:4.
Yewhalaw D, Legesse W, Van Bortel W, Gebre-Selassie S, Kloos H, Duchateau L, et al. Malaria and water resource development: the case of Gilgel-Gibe hydroelectric dam in Ethiopia. Malar J. 2009;8:21.
Ministry of Finance and Economic Development. Growth and transformation plan (GTP), 2010–2015. http://www.iea.org/media/pams/ethiopia/Ethiopia_GTP_2010to2915.pdf. Accessed 25 Jan 2015.
Yewhalaw D, Wassie F, Steurbaut W, Spanoghe P, Van Bortel W, Denis L, et al. Multiple insecticide resistance: an impediment to insecticide-based malaria vector control program. PLoS ONE. 2011;6:e16066.
Mitiku I, Assefa A. Caregivers’ perception of malaria and treatment-seeking behaviour for under five children in Mandura District, West Ethiopia: a cross-sectional study. Malar J. 2017;16:144.
Reyburn H, Mbatia R, Drakeley C, Carneiro I, Mwakasungula E, Mwerinde O, et al. Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study. BMJ. 2004;329:1212.
Shah NK. Defining & counting malaria deaths. Indian J Med Res. 2012;135:270–2.
Shah NK, Dhariwal AC, Sonal GS, Gunasekar A, Dye C, Cibulskis R. Malaria-attributed death rates in India. Lancet. 2011;377:991 (author reply 994–5).
Authors’ contributions
AD, AM, KD, GAT, YAM, and JDS designed the study. AD and SDG analysed and interpreted the data. AD wrote the manuscript. All authors assisted in the design, provided data, assisted in data interpretation, and critically reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We are grateful to the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, which helped us form the Ethiopian National Burden of Diseases team (ENBD) and use GBD data to generate national estimates for Ethiopia.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The GBD 2015 data are available and can be accessed at the GBD website (https://vizhub.healthdata.org/gbd-compare/).
Ethical consideration
The study utilized existing data from the GBD 2015 study and does not require ethical approval.
Funding
Kebede Deribe is funded by a Wellcome Trust Intermediate Fellowship in Public Health and Tropical Medicine (Grant Number 201900).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Deribew, A., Dejene, T., Kebede, B. et al. Incidence, prevalence and mortality rates of malaria in Ethiopia from 1990 to 2015: analysis of the global burden of diseases 2015. Malar J 16, 271 (2017). https://doi.org/10.1186/s12936-017-1919-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-017-1919-4