Abstract
Background
Plasmodium falciparum genetic polymorphisms that mediate altered drug sensitivity may impact upon virulence. In a cross-sectional study, Ugandan children with infections mutant at pfcrt K76T, pfmdr1 N86Y, or pfmdr1 D1246Y had about one-fourth the odds of symptomatic malaria compared to those with infections with wild type (WT) sequences. However, results may have been confounded by greater likelihood in those with symptomatic disease of higher density mixed infections and/or recent prior treatment that selected for WT alleles.
Methods
Polymorphisms in samples from paired episodes of asymptomatic and symptomatic parasitaemia in 114 subjects aged 4–11 years were followed longitudinally in Tororo District, Uganda. Paired episodes occurred within 3–12 months of each other and had no treatment for malaria in the prior 60 days. The prevalence of WT, mixed, and mutant alleles was determined using multiplex ligase detection reaction-fluorescent microsphere assays.
Results
Considering paired episodes in the same subject, the odds of symptomatic malaria were lower for infections with mutant compared to WT or mixed sequence at N86Y (OR 0.26, 95% CI 0.09–0.79, p = 0.018), but not K76T or D1246Y. However, symptomatic episodes (which had higher densities) were more likely than asymptomatic to be mixed (for N86Y OR 2.0, 95% CI 1.04–4.0, p = 0.036). Excluding mixed infections, the odds of symptomatic malaria were lower for infections with mutant compared to WT sequence at N86Y (OR 0.33, 95% CI 0.11–0.98, p = 0.046), but not the other alleles. However, if mixed genotypes were grouped with mutants in this analysis or assuming that mixed infections consisted of 50% WT and 50% mutant genotypes, the odds of symptomatic infection did not differ between infections that were mutant or WT at the studied alleles.
Conclusions
Although infections with only the mutant pfmdr1 86Y genotype were associated with symptomatic infection, this association could primarily be explained by greater parasite densities and therefore greater prevalence of mixed infections in symptomatic children. These results indicate limited association between the tested polymorphisms and risk of symptomatic disease and highlight the value of longitudinal studies for assessing associations between parasite factors and clinical outcomes.
Similar content being viewed by others
Background
Malaria, in particular infection caused by Plasmodium falciparum, remains an overwhelming problem in most of sub-Saharan Africa [1]. Malaria control is greatly limited by drug resistance. Resistance to a number of drugs is mediated in part by polymorphisms in two putative drug transporters, encoded by the pfcrt and pfmdr1 genes [2]. The pfcrt 76T mutation is the major mediator of resistance to chloroquine and amodiaquine [3]. Polymorphisms in pfmdr1 impact upon sensitivity to a number of drugs [4]. Considering polymorphisms that are common in Africa, the pfcrt 76T and pfmdr1 86Y and 1246Y mutations are associated with decreased sensitivity to chloroquine and amodiaquine, but these same mutations mediate increased sensitivity to lumefantrine and mefloquine [2, 5, 6].
The effects of drug resistance mediating genetic polymorphisms on the fitness and virulence of malaria parasites is of interest. Considering fitness, discontinuation of chloroquine for the treatment of malaria has led to dramatic changes in circulating parasites, with the return of chloroquine-sensitive pfcrt K76 wild type (WT) parasites and also of strong anti-malarial efficacy for chloroquine [7]. Clearly, chloroquine-sensitive parasites with WT sequence at pfcrt have a fitness advantage over resistant parasites. Considering pfmdr1, WT parasites outgrew those with three mutations, only one of which (1246Y) is common in Africa, in in vitro competition experiments [8]. Following mixed clinical isolates in culture over time, modest fitness advantages appeared associated with the mutant 86Y and WT D1246 alleles [9]. In an area with seasonal malaria, the prevalence of parasites with mutant pfcrt 76T and pfmdr1 86Y sequences decreased during the low transmission season, when drug pressure is lowest, implying a fitness advantage for WT parasites [10]. Overall, in most cases parasites with WT sequences in pfcrt and pfmdr1 have appeared to have a fitness advantage over mutant parasites.
It is unclear if P. falciparum drug resistance-mediating polymorphisms also impact on parasite virulence, characterized as the ability to cause symptomatic or severe disease. Studies from India [11] and Mali [12], but not Sudan [13] or Gabon [14], showed associations between presence of the pfcrt 76T mutation and severe malaria, but these associations may have been due to clinical progression after chloroquine treatment failure, rather than variations in parasite virulence. Previously, differences in genotypes between parasites causing symptomatic and asymptomatic infections were studied in samples from a cross-sectional study of children from Tororo, Uganda. Remarkably, children harbouring isolates with mutations at pfcrt K76T, pfmdr1 N86Y, or pfmdr1 D1246Y had about one-fourth the odds of symptomatic malaria compared to those with WT parasites [15]. Similarly, in children in Benin, the prevalence of the pfmdr1 86Y mutation was significantly greater in asymptomatic compared to symptomatic infections, consistent with decreased virulence of parasites with the pfmdr1 86Y mutation [16]. However, the results of these case–control studies may have been confounded by two factors. First, infections associated with symptomatic disease typically have greater parasite densities than those that are asymptomatic, increasing the likelihood of detecting WT genotypes present in mixed infections. Second, children with symptomatic infection may have had a greater likelihood, compared to children presenting with asymptomatic infection, of a recent prior infection treated with artemether/lumefantrine, which selects for WT alleles [17–20]. To further explore relationships between parasite genotype and clinical presentation, samples were utilized from an ongoing longitudinal study and genotypes were compared for parasites in paired samples from Ugandan children with symptomatic and asymptomatic episodes of malaria.
Methods
Longitudinal study
Samples were collected from children enrolled in a cohort study in Nagongera Sub-county, Tororo District, Uganda, an area of high malaria transmission intensity. The cohort study has been described previously [21]. In brief, all households within the sub-county were enumerated and mapped, and 100 randomly selected households were enrolled if they met enrollment criteria of having at least one resident 0.5–10 years of age and at least one adult who provided informed consent. Subjects were encouraged to visit a dedicated study clinic open seven days a week for any illnesses. Febrile subjects (temperature ≥38 °C tympanic or history of fever in the past 48 h) were evaluated at the clinic, and if malaria was diagnosed based on any level of parasitaemia on a Giemsa-stained thick smear, treatment (artemether–lumefantrine for uncomplicated malaria; quinine for complicated malaria) was provided. Subjects also had routine blood smears obtained every 3 months. At the time of blood collection either for symptomatic disease or at routine visits, blood was also spotted onto filter paper and stored. The cohort study was approved by the Makerere University School of Medicine Research and Ethics Committee, the Uganda National Council for Science and Technology, and the University of California, San Francisco Committee on Human Research.
Specimens evaluated for this study
For this sub-study, all subjects who met study criteria were identified. No a priori power calculation was performed for the sub-study. These subjects were aged 4–11 years and had two smear positive specimens, one from an episode of symptomatic (with fever, defined as above) malaria and another from an episode of asymptomatic parasitaemia, with each episode without prior treatment for malaria within 60 days, and the two episodes within 3–12 months of each other. These episodes all occurred between November, 2011 and December, 2014. Samples from each episode were collected and studied.
Characterization of parasite polymorphisms
DNA was extracted from filter paper blood spots into 100 μl of water using Chelex-100 [22]. Gene fragments spanning all loci of interest were amplified, and multiplex ligase detection reaction-fluorescent microsphere assays were performed as previously described [20, 23].
Statistical methods
Data analysis was done using R version 3.3 [24]. The primary outcome was presentation with symptomatic vs. asymptomatic malaria infection. Comparisons of the odds of genotypes present in symptomatic vs. asymptomatic paired isolates was performed grouping mixed infections as mutant, mixed infections as WT, excluding mixed infections from the analysis, or considering mixed samples as consisting of 50% WT and 50% mutant parasites. Analyses were performed using a binomial generalized estimating equations model, to allow for correlation between paired samples from each individual. A p value <0.05 was considered statistically significant.
Results
Characteristics of study subjects and episodes of malaria
Characteristics of the 114 subjects who provided samples for analysis and of the studied malaria infections are shown in Table 1. Similar numbers of children presented first with asymptomatic (54) compared to symptomatic (60) infections, and the mean age of the children when they presented with asymptomatic vs. symptomatic infections was very similar. The mean parasite density was about fourfold higher in symptomatic compared to asymptomatic infections.
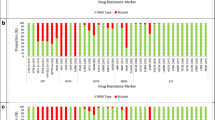
Prevalence of Plasmodium falciparum polymorphisms
Three P. falciparum polymorphisms that are associated with response to multiple anti-malarial drugs were studied [2]. All three of these mutations were previously very common in Ugandan isolates, but prevalence is decreasing, presumably due to decreased usage of chloroquine and increased usage of artemether–lumefantrine to treat malaria in Uganda [20, 24, 25]. Considering all study samples, about half were pure WT for the pfmdr1 N86Y and D1246Y alleles, and <10% were pure WT at pfcrt K76T (Table 2).
Considering paired episodes in the same subject, thus controlling for host factors, the odds of symptomatic malaria were significantly lower for infections with mutant compared to WT or mixed sequence at N86Y (OR 0.26, 95% CI 0.09–0.79, p = 0.018), but not the other alleles (pfmdr1 D1246Y OR 0.69, 95% CI 0.37–1.28, p = 0.24; pfcrt K76T OR 0.77, 95% CI 0.36–1.63, p = 0.49). However, if mixed genotypes were grouped with mutants in this analysis, the odds of symptomatic malaria were similar for mutant and mixed N86Y genotypes compared to pure WT (OR 1.23, 95% CI 0.72–2.10, p = 0.44). This difference was explained by the fact that symptomatic episodes were more likely than asymptomatic to be mixed (for N86Y OR 2.0, 95% CI 1.04–4.0, p = 0.036). Excluding mixed infections, the odds of symptomatic malaria were lower for infections with mutant compared to WT sequence at N86Y (OR 0.33, 95% CI 0.11–0.98, p = 0.046), but not the other alleles (pfmdr1 D1246Y OR 0.82, 95% CI 0.46–1.43, p = 0.48; pfcrt K76T OR 1.08, 95% CI 0.43–2.75, p = 0.87). Assuming arbitrarily that mixed infections consisted of 50% WT and 50% mutant genotypes, the odds of symptomatic infection was 0.89 (95% CI 0.56–1.41, p = 0.61) for infections mutant at pfmdr1 N86Y, 0.92 (95% CI 0.63–1.34, p = 0.66) for infections mutant at pfmdr1 D1246Y, and 0.88 (95% CI 0.40–1.92, p = 0.75) for infections mutant at pfcrt K76T.
Discussion
The prevalence of three P. falciparum polymorphisms associated with drug resistance was compared in children with either asymptomatic or symptomatic malaria infections in a cohort followed longitudinally in Tororo, Uganda. In 114 children with paired samples from episodes of asymptomatic and symptomatic malaria infections that occurred within a year, differences between genotypes of parasites from asymptomatic and symptomatic infections were much less marked than had been seen in prior case–control studies. One mutant genotype, pfmdr1 86Y, was more common in samples from asymptomatic compared to symptomatic infections, but symptomatic infections were more commonly mixed, potentially explaining the association. These results indicate limited association between the tested polymorphisms and clinical outcomes.
Decreased prevalence of pfcrt 76T and pfmdr1 86Y and 1246Y mutant genotypes in symptomatic, compared to asymptomatic infections was previously demonstrated in Ugandan children [15]. A study in Benin found a similar association for pfmdr1 86Y, but not pfcrt 76T [16]. These results suggested that these mutations render parasites less capable than WT parasites of causing clinical illness. However, the prior studies were case–control studies subject to confounding. First, children with symptomatic disease typically have greater parasite densities [15, 26], and thus a greater likelihood of detection of a mixed infection, than asymptomatic children. This was the case in the present study, with an odds ratio of 2.0 for mixed infections in symptomatic, compared to asymptomatic children. The increased prevalence of mixed infections likely at least partially explained the association between mutant genotypes and asymptomatic infection, as a greater likelihood of mixed infection would lead to a greater likelihood of WT parasites being identified in a symptomatic infection. In other words, symptomatic infections would be more likely than asymptomatic to have both WT and mutant parasites identified, thereby increasing the chance of WT being associated with symptomatic infections. Second, children with symptomatic malaria in cross-sectional evaluation were probably more likely to have had a recent prior episode of malaria, and thus more likely to have received recent treatment with artemether-lumefantrine, which selects for WT genotypes at the studied polymorphisms [17–20], and is the national first line regimen to treat malaria in Uganda and Benin [1]. In the present study, the influence of prior treatment was removed by studying only episodes without prior treatment for malaria within 60 days.
This study was designed to limit confounding in the comparison of parasites causing asymptomatic and symptomatic malaria infections. Utilizing samples from a longitudinal study, prior treatment histories were known, and only samples without prior therapy within 60 days, approximately the duration of selective pressure on the studied genotypes of artemether–lumefantrine, were studied [19]. To limit differences related to host immunity, only children over 4 years of age were studied; in this area of very high transmission intensity, children of this age would be expected to all have had numerous prior malaria exposures. To limit differences related to host factors, analysis of matched samples from the same patient was performed; roughly equal numbers of samples were from asymptomatic infections that occurred before or after symptomatic infections. With this study design, associations between parasite genotypes and clinical presentation were much less pronounced than seen previously in cross-sectional studies.
This study had some limitations. The sample size was necessarily limited by strict criteria for inclusion of samples for analysis, and so there may have been inadequate power to identify associations of small magnitude. The molecular assays had limited sensitivity, and so some minority genotypes that might play a role in disease presentation may have been missed. Of note, the molecular methods differed from those used in an earlier cross-sectional analysis in Uganda, but the two methods (restriction fragment length polymorphism analysis and multiplex ligase detection reaction-fluorescent microsphere analysis) have similar sensitivities [23]. Despite these limitations, use of longitudinal samples, with comparisons of samples from the same children, offered a valuable means of considering the impact of parasite genotypes on clinical presentation.
Conclusions
Comparing two episodes of malaria parasitaemia in the same child with a design that limited influences of prior malaria treatment and varied prevalence of mixed infection, studied drug resistance genotypes had modest, if any influence on the risk of symptomatic malaria. Further studies of the impacts of parasite genetic polymorphisms on P. falciparum fitness and virulence are needed. These results highlight the value of longitudinal samples from well-studied subjects to answer questions concerning associations between parasite factors and clinical outcomes.
References
World Health Organization. World malaria report 2016. Geneva: World Health Organization; 2016.
Rosenthal PJ. The interplay between drug resistance and fitness in malaria parasites. Mol Microbiol. 2013;89:1025–38.
Ecker A, Lehane AM, Clain J, Fidock DA. PfCRT and its role in antimalarial drug resistance. Trends Parasitol. 2012;28:504–14.
Ekland EH, Fidock DA. Advances in understanding the genetic basis of antimalarial drug resistance. Curr Opin Microbiol. 2007;10:363–70.
Eyase FL, Akala HM, Ingasia L, Cheruiyot A, Omondi A, Okudo C, et al. The role of pfmdr1 and pfcrt in changing chloroquine, amodiaquine, mefloquine and lumefantrine susceptibility in Western-Kenya P. falciparum samples during 2008–2011. PLoS ONE. 2013;8:e64299.
Tumwebaze P, Conrad MD, Walakira A, LeClair N, Byaruhanga O, Nakazibwe C, et al. Impact of antimalarial treatment and chemoprevention on the drug sensitivity of malaria parasites isolated from Ugandan children. Antimicrob Agents Chemother. 2015;59:3018–30.
Laufer MK, Thesing PC, Eddington ND, Masonga R, Dzinjalamala FK, Takala SL, et al. Return of chloroquine antimalarial efficacy in Malawi. N Engl J Med. 2006;355:1959–66.
Hayward R, Saliba KJ, Kirk K. pfmdr1 mutations associated with chloroquine resistance incur a fitness cost in Plasmodium falciparum. Mol Microbiol. 2005;55:1285–95.
Ochong E, Tumwebaze PK, Byaruhanga O, Greenhouse B, Rosenthal PJ. Fitness consequences of Plasmodium falciparum pfmdr1 polymorphisms inferred from ex vivo culture of Ugandan parasites. Antimicrob Agents Chemother. 2013;57:4245–51.
Ord R, Alexander N, Dunyo S, Hallett R, Jawara M, Targett G, et al. Seasonal carriage of pfcrt and pfmdr1 alleles in Gambian Plasmodium falciparum imply reduced fitness of chloroquine-resistant parasites. J Infect Dis. 2007;196:1613–9.
Ranjit MR, Das A, Chhotray GP, Das BP, Das BN, Acharya AS. The PfCRT (K76T) point mutation favours clone multiplicity and disease severity in Plasmodium falciparum infection. Trop Med Int Health. 2004;9:857–61.
Wele M, Djimde AA, Guindo A, Beavogui AH, Traore IZ, Sadou A, et al. High frequency of PfCRT 76T in two Malian villages and its prevalence in severe relative to non-severe malaria. Acta Trop. 2011;119:11–3.
Giha HA, Elbashir MI, A-Elbasit IE, A-Elgadir TM, ElGhazali GE, Mackinnon MJ, et al. Drug resistance-virulence relationship in Plasmodium falciparum causing severe malaria in an area of seasonal and unstable transmission. Acta Trop. 2006;97:181–7.
Mayengue PI, Kalmbach Y, Issifou S, Kremsner PG, Ntoumi F. No variation in the prevalence of point mutations in the Pfcrt and Pfmdr1 genes in isolates from Gabonese patients with uncomplicated or severe Plasmodium falciparum malaria. Parasitol Res. 2007;100:487–93.
Tukwasibwe S, Mugenyi L, Mbogo GW, Nankoberanyi S, Maiteki-Sebuguzi C, Joloba ML, et al. Differential prevalence of transporter polymorphisms in symptomatic and asymptomatic falciparum malaria infections in Uganda. J Infect Dis. 2014;210:154–7.
Ogouyemi-Hounto A, Ndam NT, Kinde Gazard D, d’Almeida S, Koussihoude L, Ollo E, et al. Prevalence of the molecular marker of Plasmodium falciparum resistance to chloroquine and sulphadoxine/pyrimethamine in Benin seven years after the change of malaria treatment policy. Malar J. 2013;12:147.
Sisowath C, Stromberg J, Martensson A, Msellem M, Obondo C, Bjorkman A, et al. In vivo selection of Plasmodium falciparum pfmdr1 86N coding alleles by artemether-lumefantrine (Coartem). J Infect Dis. 2005;191:1014–7.
Zongo I, Dorsey G, Rouamba N, Tinto H, Dokomajilar C, Guiguemde RT, et al. Artemether-lumefantrine versus amodiaquine plus sulfadoxine–pyrimethamine for uncomplicated falciparum malaria in Burkina Faso: a randomised non-inferiority trial. Lancet. 2007;369:491–8.
Baliraine FN, Rosenthal PJ. Prolonged selection of pfmdr1 polymorphisms after treatment of falciparum malaria with artemether–lumefantrine in Uganda. J Infect Dis. 2011;204:1120–4.
Conrad MD, LeClair N, Arinaitwe E, Wanzira H, Kakuru A, Bigira V, et al. Comparative impacts over 5 years of artemisinin-based combination therapies on Plasmodium falciparum polymorphisms that modulate drug sensitivity in Ugandan children. J Infect Dis. 2014;210:344–53.
Kamya MR, Arinaitwe E, Wanzira H, Katureebe A, Barusya C, Kigozi SP, et al. Malaria transmission, infection, and disease at three sites with varied transmission intensity in Uganda: implications for malaria control. Am J Trop Med Hyg. 2015;92:903–12.
Plowe CV, Djimde A, Bouare M, Doumbo O, Wellems TE. Pyrimethamine and proguanil resistance-conferring mutations in Plasmodium falciparum dihydrofolate reductase: polymerase chain reaction methods for surveillance in Africa. Am J Trop Med Hyg. 1995;52:565–8.
Leclair NP, Conrad MD, Baliraine FN, Nsanzabana C, Nsobya SL, Rosenthal PJ. Optimization of a ligase detection reaction fluorescent microsphere assay for the characterization of resistance-mediating polymorphisms in African samples of Plasmodium falciparum. J Clin Microbiol. 2013;51:2564–70.
Mbogo GW, Nankoberanyi S, Tukwasibwe S, Baliraine FN, Nsobya SL, Conrad MD, et al. Temporal changes in prevalence of molecular markers mediating antimalarial drug resistance in a high malaria transmission setting in Uganda. Am J Trop Med Hyg. 2014;91:54–61.
Tumwebaze P, Tukwasibwe S, Taylor AR, Conrad MD, Ruhamyankaka E, Asua V, et al. Changing antimalarial drug resistance patterns identified by surveillance at three sites in Uganda. J Infect Dis. 2016. doi:10.1093/infdis/jiw614.
Owusu-Agyei S, Koram KA, Baird JK, Utz GC, Binka FN, Nkrumah FK, et al. Incidence of symptomatic and asymptomatic Plasmodium falciparum infection following curative therapy in adult residents of northern Ghana. Am J Trop Med Hyg. 2001;65:197–203.
Authors’ contributions
EA, MRK, and GD directed the clinical study that provided samples for analysis. GD, BG, and PJR conceived of the study design. ST, PK, SLN, and PJR designed and carried out the reported laboratory studies. MC and BG performed the data analysis. All authors contributed to the preparation of this manuscript and approve of its content. All authors read and approved the final manuscript.
Acknowledgements
We thank cohort study participants and their parents and guardians; the cohort study team; and the staff of the Infectious Diseases Research Collaboration for administrative and technical support.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets utilized for this study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The cohort study that supplied samples for analysis and this specific study were approved by the Makerere University School of Medicine Research and Ethics Committee, the Uganda National Council for Science and Technology, and the University of California, San Francisco Committee on Human Research.
Funding
This study was funded by grants from the National Institutes of Health (AI089674 and AI075045).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tukwasibwe, S., Tumwebaze, P., Conrad, M. et al. Drug resistance mediating Plasmodium falciparum polymorphisms and clinical presentations of parasitaemic children in Uganda. Malar J 16, 125 (2017). https://doi.org/10.1186/s12936-017-1777-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-017-1777-0