Abstract
Background
Despite advances in therapeutic strategies, resistance to immunotherapy and the off-target effects of targeted therapy have significantly weakened the benefits for patients with melanoma.
Main body
Alternative splicing plays a crucial role in transcriptional reprogramming during melanoma development. In particular, aberrant alternative splicing is involved in the efficacy of immunotherapy, targeted therapy, and melanoma metastasis. Abnormal expression of splicing factors and variants may serve as biomarkers or therapeutic targets for the diagnosis and prognosis of melanoma. Therefore, comprehensively integrating their roles and related mechanisms is essential. This review provides the first detailed summary of the splicing process in melanoma and the changes occurring in this pathway.
Conclusion
The focus of this review is to provide strategies for developing novel diagnostic biomarkers and summarize their potential to alter resistance to targeted therapies and immunotherapy.
Similar content being viewed by others
Background
Melanoma is not as common as other skin cancers; however, it is more lethal, resulting in approximately 75% of skin cancer-related deaths [1]. The rapidly increasing incidence of melanoma and the high lethality of advanced disease have prompted efforts to identify factors that drive melanoma development and progression [2, 3]. The approval of several therapeutic agents against melanoma has revolutionized the treatment of patients with advanced‑stage disease [4]. Compared with a decade ago, the 5-year survival rate for patients with advanced melanoma treated with BRAF inhibitors, MEK inhibitors, or single PD-1 antibodies has improved from 5% to approximately 30% [5,6,7]. However, transcriptional reprogramming allows heterogeneous tumors to pass through different stages of melanoma progression and adapt to drug exposure during treatment [8,9,10], leading to targeted therapy and immunotherapy resistance.
Alternative splicing is a mode of transcriptional reprogramming and can change the stability, transport, and translation efficiency of mRNA through different splice forms, thereby directly or indirectly affecting gene regulation [11]. Dysregulation of RNA splicing is generally a hallmark of almost all tumors [12]. Cancer-associated splicing alterations are caused by repetitive mutations and the altered expression of transport factors that control splicing, catalysis, and regulation [13]. Aberrant alternative splicing can promote tumorigenesis through various mechanisms, including increased cell proliferation, decreased apoptosis, increased migration and metastatic potential, resistance to chemotherapy, and immune surveillance evasion [14, 15]. The generation of new abnormal proteins in the context of splicing events may render these cells vulnerable to pharmacological and immunological drugs that target these proteins or their associated pathways [16,17,18].
The evolution of high-throughput analysis techniques and the increasing availability of transcriptome data have led to an increased number of detected splicing variants and aberrant splicing events [19, 20]. However, how alternative splicing regulates drug resistance in targeted therapy and immunotherapy in melanoma is unclear. This review summarizes and discusses the mechanism of alternative splicing in the pathogenesis and progression of melanoma to address the current clinical dilemma of targeted therapy and immunotherapy resistance.
Altered expression of splicing factors in melanoma
Splicing factors participate in life activities throughout the body and act like “scissors” to accurately repair pre-mRNA, remove redundant parts, form multiple mRNA sequences, and translate them into protein isomers with different biological functions [21]. The pre-mRNA splicing pathway is a complex cycle involving the assembly, activation, splicing, and depolymerization of multiple RNA and protein components. Each splicing cycle comprises two consecutive transesterification steps. In the first step, the 5′-exon is released, forming an intron chain intermediate, often referred to as the branching process. The second step is exon ligation, where the 5′-exon is interconnected with the 3′-exon [22]. Splicing factors facilitate spliceosome splicing by stabilizing the active site and forming part of the dynamic spliceosome complex.
Alterations in splicing factors are associated with tumor development and progression in various cancer types [13, 14, 23]. The following sections describe the presence and roles of several splicing factors from different protein families in melanomas.
Serine/arginine-rich proteins
Most serine/arginine-rich (SR) proteins are splicing activators in tumor pathology [24]. They bind to the pre-mRNA of the exon splicing enhancer and enable exon recognition through spliceosomes, facilitating exon inclusion [25,26,27]. SR proteins interact with other spliceosomal components via the SR structural domain, linking the 5′- and 3′-splice site binding components, U1 small nuclear ribonucleoproteins complex (U1 snRNP) and U2AF to trigger U1 snRNP, the combination of pre-mRNA containing the 5′-splice site (Table 1) [28, 29].
SR splicing factor 1 (SRSF1) is an oncoprotein that positively regulates circMYC expression, potentially affecting melanoma cells [30]. Its phosphorylated isoform, SRPK1, controls pre-mRNA splicing by regulating pro-angiogenic isoforms [31]. In addition, an increased number of immune cells were observed in biopsies of mice treated with SRPK1/2 pharmacological inhibitors of metastatic melanoma [32,33,34]. In vitro assays indicated that inhibitors increase immunological sensitivity by intensifying the expression of antigen-presenting major histocompatibility complex (MHC) I and MHC II molecules and splenocyte recruitment [34]. This revealed that the antimetastatic effects of SRPK1/2 inhibition may also include enhanced immune responses, suggesting a possible additional functional role of SRSF1/2 in tumor biology [32,33,34].
SRSF3 regulates the p53-mediated process to suppress tumorigenesis [35]. SRSF3 is a critical enhancer of alternative splicing, inhibits melanoma growth, and amplifies sensitivity to MAPK-targeted therapies via the p53-MDM4 axis in different human melanoma cell lines and xenograft mouse models derived from patients with melanoma [36, 37].
SRSF6 is necessary to increase the Bim variant (a proapoptotic member of the BCL-2 family) splicing [38]. Considering that SRSF6 is upregulated, inhibiting it with small interfering RNA using vemurafenib intercepts Bim variant mediation and apoptosis [39]. Therefore, rendering melanoma cells susceptible to BRAF V600E inhibitors is essential.
In summary, the SR family plays a crucial role in melanoma development and progression by promoting and regulating splice variant synthesis and acting as drug induction mediators or regulators. Although SR proteins have been extensively described in cancer, SR protein dysregulation in melanomas is still unclear and requires further investigation.
Heterogeneous nuclear ribonucleoproteins
Heterogeneous nuclear ribonucleoproteins (hnRNPs) are a protein superfamily that binds to pre-mRNAs through RNA-binding regions to form complexes and participate in alternative splicing [40, 41]. hnRNPs are strongly associated with the pathogenesis and development of various cancers; high hnRNP expression levels can promote the proliferation, invasion, and metastasis of cancer cells and influence patient prognosis [42,43,44,45]. In addition, high hnRNP expression may participate in tumor resistance through damage repair mechanisms (Table 2) [46].
The absence of polypyrimidine tract-binding protein 1 (PTBP1; hnRNP I) in dendritic cells can increase MHC II expression and disrupt T cell homeostasis without involving dendritic cell progression [47]. PTBP1 deficiency in dendritic cells can increase antitumor immunity [48, 49] and is also relevant to the CD44v6 variant expression in melanoma brain metastasis [50]. Therefore, PTBP1 is a leading factor in regulating immune responses.
Other hnRNPs also play a major role in alternative splicing and influence tumor development; however, no related studies have been conducted on melanoma treatment. hnRNP A1 combines with and activates the internal ribosomal entry sequence of melanoma stress-induced antigens. Endoplasmic reticulum stress agonists promote hnRNP A1 translocation and enhance stress-induced antigen translation and recognition by T-lymphocytes in melanoma cells [51]. hnRNP A2B1 is upregulated in melanoma stem cells and may act through post-transcriptional regulation to block melanoma stem cell apoptosis [52]. hnRNP C directly binds to the cis-element of the 5′ coding region of p53 mRNA, promoting p53 translation [53]. hnRNP U is a protein chaperone of protein kinase B (AKT) that interacts and cooperates with nuclear actin in transcriptional regulation; however, additional biochemical examination is needed to verify the assemblage of nuclear AKT and hnRNP in the cell system [54].
The influence of hnRNPs on melanoma has not been extensively explored; however, these findings provide a unique direction for melanoma treatment.
Splicing factor 3B subunit 1
Splicing factor 3B subunit 1 (SF3B1) encodes subunit 1 of the splicing factor 3b protein complex, which is involved in pre-mRNA splicing. Splicing factor 3b forms the U2 snRNP with splicing factor 3a and a 12 S RNA unit [55, 56].
SF3B1 is the most commonly mutated splicing factor, with approximately 15–20% of mutations occurring in uveal melanoma. SF3B1 mutations in cancers are primarily missense mutations, with three mutation hotspots targeting the R625, K666, and K700 codon positions [55, 57]. K700 mutations are common in hematopoietic malignancies [58], whereas R625 mutations are the most frequent in uveal melanoma [59]. However, codon R625 repeat mutations in SF3B1 in uveal melanomas are absent in most cutaneous melanomas [60]. These findings suggest that the pathogenesis of the mutated genes is distinct; therefore, the target hotspots for each disease are different, or diverse disease biology possibly drives the selection of individual mutations. This emphasizes the genetic diversity between cutaneous and uveal melanomas, and the demand for subtype-specific therapeutics.
Mutations in spliceosomal components alter intragenic splicing, causing intron retention or aberrant alternative splicing, disrupting the balance of protein isoforms and regulating cell growth and differentiation [61]. In in vivo studies, mutant SF3B1 stimulates aberrant splicing and represses downstream genes by negatively regulating AKT and nuclear factor kappa B (NF-κB) [62, 63]. In in vitro knock-in models, cell migration, tumorigenesis, and hypersensitivity to AKT kinase inhibitors were driven through coordinated NF-κB and AKT signaling activation [62]. In uveal melanomas with SF3B1 mutations, these splicing patterns induce the formation of tumor-specific immunogenic neoepitopes [64]. Neoepitopes are attractive targets for adjuvant therapy, in which soluble biospecific reagents are used to redirect the activity of effector T cells with antibodies or affinity-matured T-cell receptors to tumor cells expressing neoepitopes [65, 66].
SF3B1 binds to cyclin-dependent kinase 11 and phosphorylates its N-terminal threonine residue to activate the spliceosome [67]. Phosphorylation is critical for the association of SF3B1 with U5 and U6 snRNAs in activated spliceosomes; therefore, inhibiting SF3B1 phosphorylation is a novel direction for tumor therapy.
Aberrant alternative splicing variants in melanoma
RNA splicing plays a pivotal role in melanoma [16, 68], and multi-omics approaches have pinpointed it as one of the most unregulated pathways in melanoma [69]. Additionally, a close association exists between alternative splicing and melanoma prognosis [70]. Therefore, alternative splicing in melanomas should be examined to develop new strategies for reversing drug resistance. Aberrant expression or variation in specific mRNA splicing variants is related to cancer initiation, progression, aggressiveness, and drug resistance due to alternative splicing of critical genes [15, 17, 18]. The importance of specific SVs in melanomas is summarized in Table 3. Genes encoded by BRAF, neuroblastoma RAS (NRAS), the BCL-2 family, MDM4, and CD44 have been the most studied.
BRAF
BRAF encodes a serine/threonine kinase that is regulated by the MAP kinase pathway [71]. As a direct RAS effector, BRAF dimerizes to catalyze MEK and extracellular-signal-regulated kinase phosphorylation and activation [72]. Approximately 40–60% of melanomas carry mutations in BRAF [73]. The most common mutation is the valine replacement at codon 600 (V600E) with glutamic acid [74]. Vemurafenib and dabrafenib are BRAF V600E inhibitors approved for treating V600E-mutated melanomas [75]. Although 63–76% of patients with advanced melanoma and BRAF V600E mutations benefited clinically from combination therapy, the median progression-free survival was only approximately 9 months, and 90% of patients experienced resistance within one year [75]. One mechanism of resistance to vemurafenib is a point mutation in intron 8, which leads to exons 4–8 being skipped, thereby eliminating the RAS-binding domain (Fig. 1) [76, 77].
The intricacy and heterogeneity of the pathways associated with the development of resistance to BRAF inhibitors make it challenging to defeat acquired resistance with a “one-size-fits-all” approach. Several studies are currently underway to identify new therapeutic combinations that can restrict or prevent the development of resistance to BRAF inhibitors or overcome already-developed resistance. Most findings indicate that disrupting the BRAF–MEK association during BRAF inhibitor therapy is a probable pharmacological target [73, 76,77,78,79]. PLX7904 and its clinical analog, PLX8394, inhibit MEK–ERK1/2 signaling and G1/S cell cycle events, effectively blocking the survival and growth of vemurafenib-resistant cells with diverse BRAF V600E splice variants [79]. These inhibitors are effective in vemurafenib-resistant tumors that express BRAF splice mutations and reduce the homodimerization of splice variants. They are currently undergoing preclinical trials and may be second-line treatment options for patients unresponsive to vemurafenib or dabrafenib.
Two conserved phosphorylated residues exist in RAF regulation: serine 365 (S365) within CR2 and serine 729 (S729) in the BRAF C-terminus [80,81,82]. The mutation of S729 to a non-phosphorylatable residue reduces the interaction between the BRAF V600E splicing variant and MEK, decreases dimerization or oligomerization, and promotes RAF inhibitor sensitivity [83, 84]. Conversely, the S365 mutation increases BRAF V600E homodimerization [83, 85]. Therefore, the induced S729 site mutation or removal of the S365 site may contribute to the resistance to RAF inhibitors [86]. These outcomes provide evidence for aberrantly spliced forms of BRAF V600E to target resistance.
NRAS
NRAS encodes a small GTP-binding protein associated with the cell membrane that links cell surface receptor tyrosine kinases to nuclear transcription factors [87]. NRAS is the second most frequently mutated oncogene in melanoma [88]; however, no effective treatment for NRAS mutations exists [89]. Immunotherapy with programmed cell death protein checkpoint inhibitors, such as nivolumab or pembrolizumab, is the first line of treatment for surgically incurable stage III/IV melanoma with NRAS mutations [90]. However, the efficacy of immunotherapies for treating melanomas with NRAS mutations is contentious [91, 92]. Second-line treatments for melanomas with NRAS mutations include inhibiting the MAPK signaling pathway, MEK, or a combination with other drugs [93, 94]. However, the therapeutic potency of existing drugs against melanomas with NRAS mutations is insufficient [94], highlighting the need to identify novel targets.
Since 2014, five NRAS isoforms have been shown to have different expression subtypes, enzymatic activities, and downstream oncogenicity [95]. Based on canonical form 1, the remaining four forms were created by inserting the previously unknown exon 3(b) into form 2, skipping exon 3 into form 3, skipping exons 3 and 4 into form 4, and fusing the start of exon 2 with the end of exon 5 into form 5 (Fig. 2).
NRAS cDNAs. This figure schematically depicts the five main linear alternative splicing events and protein amino acid length of NRAS. Based on the canonical form 1, the remaining four forms are created by inserting the previously unknown exon 3(b) into form 2, skipped exon 3 into form 3, skipped exons 3 and 4 into form 4, and fused the start of exon 2 with the end of exon 5 into form 5
Notably, only isoforms 1 and 2 contain codon 61 (exon 3) that can activate constitutive RAS GTPases and switch their conformation toward the GTP-bound active state [96]. The proliferative activity of human melanomas with BRAF V600E mutations increases with NRAS isoform 2 overexpression and concomitant resistance to BRAF inhibitor therapy [97]. Increased PI3K activity in cells expressing isoform 2 is a fundamental mechanism of resistance. Unexpectedly, isoform 5 is localized in the nucleus and lacks GTPase activity, thereby increasing the activity of all downstream target proteins [98] and resistance to vemurafenib [99]. The mechanism of this resistance is unclear; hence, overcoming it requires further exploration. However, in some follow-up samples, the expression of all five NRAS isoforms was detected in the primary tumor and its metastases, which may act as negative prognostic indicators [100].
These new isoforms generate splicing variants that are more immunogenic than a typical protein with a missense mutation encoded by the same gene [99]. Regardless of whether melanoma with NRAS mutations has been deemed hopeless to treat, there is no doubt that novel splice variants inject new energy into targeted therapy or therapeutic resistance [101, 102].
BCL-2 family
Members of the BCL-2 protein family control apoptotic pathways [103] and are identified by the appearance of at least one of four BCL-2 homology (BH) domains [104]. This family is divided into a pro-survival and two pro-apoptotic groups. BCL-2, BCL-XL, BCL-W, MCL-1, and BCL2A1 constitute the pro-survival group. The pro-apoptotic subgroups include apoptosis effectors with multi-BH domains (BAX, BAK, and BOK) and apoptosis initiators with mono-BH3 domains (BIM and BAD) [105]. Pro-apoptotic and pro-survival members function through the binding of the BH3 domain to a groove on the surface, which is the switch to apoptosis [106,107,108,109].
BCL-XL displays high conformational flexibility with strict regulation of alternative splicing and post-transcriptional induction by transcription factors or microRNAs [110, 111]. Alternative splicing via 5′ splice site selection with exon 2 regulates BCL-XL expression to produce two isoforms [112]. The expression of the MCL splice variant is related to the BRAF mutational status in melanoma cell lines; MCL1L and MCL1S mRNA expression is increased in BRAF V600E mutant melanoma cells [113]. Furthermore, PLX4720 is a selective BRAF inhibitor that upregulates BimS isoform expression to mediate BRAF V600E melanoma cell apoptosis [38]. These findings provide a basis for developing small molecules that directly target BCL-2 proteins in melanoma treatment.
Using BCL-2 family proteins-specific inhibitors is inefficient owing to drug resistance mediated by the overexpression of other BCL-2 proteins. Higher MCL1 and BCL2A1 expression invalidate BCL-2/BCL-XL inhibitors (e.g., ABT199 and ABT263) in clinical and preclinical observations, emphasizing the necessity of associating BCL-2/BCL-XL inhibitors with those of MCL1 or BCL2A1 [114]. In addition, splicing modulators, such as E7107, are ideal combination partners with BCL-2/BCL-XL inhibitors, as they can efficiently modulate MCL1 and BCL2A1 [115]. This combination strategy is under investigation and can effectively inhibit most cancer-related anti-apoptotic BCL-2 family members, thereby expanding to heterogeneous indications and overcoming resistance to current BCL-2/BCL-XL-targeted therapies [116].
These studies show that the BCL-2 family has great latent capacity as a novel approach to cancer treatment. Combination therapies can reverse incomplete responses and treatment resistance to single-agent cancer therapy; however, the development of small molecules that target the BCL-2 family remains challenging.
MDM4
As a critical upstream negative regulator of the tumor suppressor p53 [117], MDM4 is not expressed in most normal tissues but is upregulated in cancer cells to promote overgrowth and inhibit apoptosis [118,119,120,121]. Notably, MDM4 exon 6 is skipped in most normal tissues and may act as a switch for the formation of degraded transcription products [122]. This means that the production of the MDM4-S isoform by skipping exon 6 occurs through the nonsense-mediated mRNA degeneration pathway in normal adult tissues. In contrast, the increased inclusion of exon 6 causes the expression of full-length MDM4 in many human cancers [37]. Mechanistically, some SR proteins may be involved in regulating MDM4 splicing variants; however, SRSF3 is one of the most essential enhancers of exon 6 in melanoma cells (Fig. 3) [37, 123].
The selective CDK4/6 inhibitor palbociclib indirectly blocks MDM4 pre-mRNA splicing, thereby reducing its expression and activating p53 [124]. Conversely, inactivating p53 reduces CDK2 inhibition, which replaces CDK4/6 and is a key driver of palbociclib resistance [125, 126]. Thus, inhibiting MDM4-p53 axis regulation can lead to the development of palbociclib resistance [124]. In addition, double targeting effects on CDK4/6 and mutant-BRAF or MEK can regress strong and persistent melanomas with BRAF- and NRAS-mutations in preclinical studies [89, 127,128,129,130]. The interaction of MDM4-p53 can promote functional restoration in melanoma cells and sensitize BRAF V600E oncogene inhibitors [131]. However, fluoroquinolones interfere with alternative splicing, causing MDM4 splicing to downregulate MDM4 expression and activate p53 [132].
In summary, MDM4 is a critical factor in p53 functional impairment in human melanoma [131]. Understanding the regulatory mechanism of MDM4 protein levels in cancer is of therapeutic significance. Nevertheless, small molecules or stapled peptides have not been able to selectively and potently disrupt the MDM4-p53 association in clinical trials [37]. However, combining them with fluoroquinolones is a bold new attempt, providing a prospective combination approach that can improve the efficacy of immunotherapy or targeted therapy and reverse resistance.
CD44
CD44 is a cell surface glycoprotein involved in cell adhesion and migration [133]. CD44 expression is also upregulated in cancer cell subpopulations and is a molecular hallmark of cancer stem cells [134]. The full-length CD44 gene contains 20 exons. All CD44 family members have homologous domains with exons 1–5 at the N-terminus and exons 16–20 at the C-terminus [135]. CD44 can be divided into two isoforms: standard CD44 (CD44s), which comprises ten constant exons with no variant exons [136], and variant CD44 (CD44v), which has alternatively spliced exons deleted or inserted between the N- and C-terminal domains (Fig. 4) [137].
CD44 splicing events. This figure schematically depicts the main linear alternative splicing events of CD44. The full length of the CD44 gene includes 20 exons. The standard CD44 (CD44s) consists of ten constant exons with no variant exons. The variant CD44 (CD44v) has alternative splicing exons deleted or inserted between the N- and C-terminal domains, such as CD44v4-10, CD44v8-10, CD44v3, CD44v6
CD44v is extensively overexpressed in pan-cancer, inducing tumor cell proliferation and drug resistance, hallmarks of cancer stem cells [138]. High expression levels of CD44v6 have been reported in primary melanoma with a propensity for brain metastasis [50]. In primary melanoma, a close correlation exists between splicing factors, such as ESRP1, ESRP2, PTBP1, and U2 snRNP auxiliary factor (U2AF2), and the expression of CD44v6 [50]. In addition, the expression levels of CD44v8-10 and U2AF2 are significantly higher in primary melanoma than in dysplastic nevi and are further increased in metastatic melanoma [139], a crucial milestone during melanoma progression [140]. Mechanistically, U2AF2 facilitates CD44v8-10 alternative splicing in malignant melanoma [139]. In vitro research has provided evidence of the dependence of CD44 expression levels on survival upon vemurafenib treatment [141]. Although animal experiments supported the effect of hyaluronic acid (HA)-modified liposomes on the delivery of chemotherapeutic agents to cancer cells with high CD44 expression, research on targeted therapy and immunotherapy is lacking [142].
Therapeutic approaches include natural selective CD44 inhibition, CD44 decoys, and HA-targeted couples, and these have been studied in different periods of preclinical and clinical trials [143]. Thus, CD44 is a promising therapeutic target for melanoma.
Discussion
Alternative splicing is a complex cellular mechanism that plays a crucial role in maintaining cell and tissue differentiation and normal cell function [20]. These factors closely regulate splicing events. For example, U2AF2 promotes the alternative splicing of CD44v8-10 in malignant melanoma [139]. Additionally, SRSF3 is a crucial enhancer of MDM4 exon 6 [37, 123]. Furthermore, complex interactions exist between splicing factors; SF3B1 can form spliceosomes with rRNA and inactivate them via phosphorylation [67]. SR proteins and hnRNPs are antagonistic interacting proteins that antagonize the action of hnRNPs in a concentration-dependent manner, preventing exon skipping (164). These complex interactions and tissue-specific roles of splicing factors leave many gaps in research that need to be addressed.
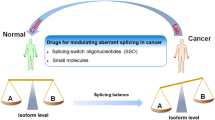
Aberrant alternative splicing is a double-edged sword with completely different effects on various targets. For example, BRAF V600E confers resistance to vemurafenib through exon skipping [76, 77]. In contrast, NRAS increases vemurafenib resistance via aberrant splicing, generating isoforms 2 and 5 [97, 99]. Notably, the BRAF S729 mutation increases sensitivity to RAF inhibitors [86]. Apoptosis in BRAF V600E melanoma cells can be mediated by upregulating BimS isoform expression [38]. However, MDM4 upregulation sensitizes BRAF V600E oncogenic inhibitors [131]. Therefore, individualized evaluation and the design of targeted therapy and immunotherapy must be strictly followed (Fig. 5).
Alternative splicing in targeted therapy resistance. SRSF3 enhances the splicing event of MDM4 to combine with p53. SRSF6 regulates the splicing event of Bim. Both of them can assist BRAF inhibitors to block the process of the dimerization of BRAF and the combination with MEK. Conversely, NRAS increases resistance to BRAF inhibitors through aberrant splicing to generate isoforms II and V
Most researchers expect to limit, prevent, or overcome targeted therapy and immunotherapy resistance in the form of combination therapy. Oncogenic splicing errors can be alleviated by oligonucleotide-mediated gene therapy (siRNA or SSO), small molecule inhibitors targeting aberrant protein isoforms, and upstream splicing factors [144]. For example, small-molecule inhibitors targeting SF3B1 overcome BRAF V600E-driven vemurafenib resistance by competitively binding to SF3B1, preventing the formation of the U2 snRNP-SF3B1 complex with precursor mRNAs and inhibiting BRAF V600E exon jumping [77, 145]. SRPK is a member of the SR family, whose inhibitors enhance immune sensitivity by enhancing antigen-presenting MHC I and MHC II expression and recruiting splenocytes [34]. Specific deletion of PTBP1 in the hnRNP family in melanoma enhances MHC II expression and disrupts T-cell homeostasis [47], and hnRNP A1 assists in T-lymphocyte recognition in melanoma cells [51]. In addition, oligonucleotide-based therapy is an effective strategy for targeting wild-type or aberrant splicing variants with high selectivity or specificity. SSO has been used to modify MDM4 and BCL2L1 splicing (Fig. 6) [37, 146]. In summary, combination therapies can support the reversal of incomplete responses and treatment resistance in single-dose cancer therapies; however, the complexity and heterogeneity of the pathways involved in their development prevent them from reaching the standard for clinical use, which remains an urgent challenge.
Alternative splicing in targeted therapy resistance. SRPK inhibitors enhance immune sensitivity by enhancing the expression of antigen-presenting MHCI and MHCII molecules and the recruitment of splenocytes. The deletion of PTBP1 can enhance MHC II expression and disrupt T cell homeostasis, and hnRNP A1 assists T lymphocyte recognition of melanoma cells
Alternative splice-derived neoepitopes may also serve as potential therapeutic targets [65, 66]. NRAS produces splice variants that are more immunogenic than canonical proteins encoded by the same gene with missense mutations [99], and the number of CD44 variants is further increased in metastatic melanoma [50]. However, many barriers still exist to implementing therapeutic strategies that specifically target these antigens. First, determining whether neoantigens are tumor-specific is crucial. Second, analyzing whether alternative splicing events within a tumor occur elsewhere in the body and not only in the healthy tissue surrounding the tumor is essential [21]. Furthermore, identifying alternative splicing events at the subclonal level in tumors is challenging [147]. These findings indicate the great potential of splice variants in melanoma-targeted therapy and immunotherapy.
In conclusion, this review is the first to summarize the splicing process in melanoma and the changes occurring in this pathway. Alternative splicing is associated with resistance to immunotherapy and targeted therapy in melanomas. With the continuous improvement in science and technology, an in-depth study of the molecular mechanism of alternative splicing in melanoma and continuous exploration of potential novel therapeutic targets can lead to newer and better treatment options for patients with drug resistance.
Data availability
Not available.
Abbreviations
- AKT:
-
protein kinase B
- BH:
-
BCL-2 homology
- CD44s:
-
standard CD44
- CD44v:
-
variant CD44
- HA:
-
hyaluronic acid
- hnRNPs:
-
heterogeneous nuclear ribonucleoproteins
- MHC:
-
major histocompatibility complex
- NF-κB:
-
nuclear factor kappa B
- NRAS:
-
neuroblastoma RAS
- PTBP1:
-
polypyrimidine tract-binding protein 1
- SF3B1:
-
splicing factor 3B subunit 1
- SR:
-
serine/arginine-rich
- SRSF1:
-
SR splicing factor 1
- SSO:
-
Semi-Synthetic Organism
- U1 snRNP:
-
U1 small nuclear ribonucleoproteins complex
- U2AF2:
-
U2 snRNP auxiliary factor
- V600E:
-
valine replacement at codon 600
References
Eggermont AM, Spatz A, Robert C. Cutaneous melanoma. Lancet. 2014;383(9919):816–27.
Kabbarah O, Chin L. Revealing the genomic heterogeneity of melanoma. Cancer Cell. 2005;8(6):439–41.
Hodis E, Watson IR, Kryukov GV, Arold ST, Imielinski M, Theurillat JP, et al. A landscape of driver mutations in melanoma. Cell. 2012;150(2):251–63.
Leonardi GC, Falzone L, Salemi R, Zanghì A, Spandidos DA, Mccubrey JA, et al. Cutaneous melanoma: from pathogenesis to therapy (review). Int J Oncol. 2018;52(4):1071–80.
Robert C, Grob JJ, Stroyakovskiy D, Karaszewska B, Hauschild A, Levchenko E, et al. Five-year outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N Engl J Med. 2019;381(7):626–36.
Hamid O, Robert C, Daud A, Hodi FS, Hwu WJ, Kefford R, et al. Five-year survival outcomes for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001. Ann Oncol. 2019;30(4):582–8.
Dickson PV, Gershenwald JE. Staging and prognosis of cutaneous melanoma. Surg Oncol Clin N Am. 2011;20(1):1–17.
Arozarena I, Wellbrock C. Phenotype plasticity as enabler of melanoma progression and therapy resistance. Nat Rev Cancer. 2019;19(7):377–91.
Benito-Jardón L, Díaz-Martínez M, Arellano-Sánchez N, Vaquero-Morales P, Esparís-Ogando A, Teixidó J. Resistance to MAPK inhibitors in Melanoma involves activation of the IGF1R-MEK5-Erk5 pathway. Cancer Res. 2019;79(9):2244–56.
Lee JH, Shklovskaya E, Lim SY, Carlino MS, Menzies AM, Stewart A, et al. Transcriptional downregulation of MHC class I and melanoma de- differentiation in resistance to PD-1 inhibition. Nat Commun. 2020;11(1):1897.
Kahles A, Lehmann KV, Toussaint NC, Hüser M, Stark SG, Sachsenberg T, et al. Comprehensive Analysis of Alternative Splicing Across Tumors from 8,705 patients. Cancer Cell. 2018;34(2):211–224e6.
Bradley RK, Anczuków O. RNA splicing dysregulation and the hallmarks of cancer. Nat Rev Cancer. 2023;23(3):135–55.
Dvinge H, Kim E, Abdel-Wahab O, Bradley RK. RNA splicing factors as oncoproteins and tumour suppressors. Nat Rev Cancer. 2016;16(7):413–30.
Takeiwa T, Mitobe Y, Ikeda K, Horie-Inoue K, Inoue S. Roles of splicing factors in hormone-related Cancer Progression. Int J Mol Sci. 2020;21(5):1551.
Sciarrillo R, Wojtuszkiewicz A, Assaraf YG, Jansen G, Kaspers GJL, Giovannetti E, et al. The role of alternative splicing in cancer: from oncogenesis to drug resistance. Drug Resist Updat. 2020;53:100728.
North K, Benbarche S, Liu B, Pangallo J, Chen S, Stahl M, et al. Synthetic introns enable splicing factor mutation-dependent targeting of cancer cells. Nat Biotechnol. 2022;40(7):1103–13.
Bonnal SC, López-Oreja I, Valcárcel J. Roles and mechanisms of alternative splicing in cancer - implications for care. Nat Rev Clin Oncol. 2020;17(8):457–74.
mRNA splicing variants. : exploiting modularity to outwit cancer therapy - PubMed [Internet]. [cited 2023 May 14]. Available from: https://pubmed.ncbi.nlm.nih.gov/23970479/.
Sebestyén E, Singh B, Miñana B, Pagès A, Mateo F, Pujana MA, et al. Large-scale analysis of genome and transcriptome alterations in multiple tumors unveils novel cancer-relevant splicing networks. Genome Res. 2016;26(6):732–44.
Stark R, Grzelak M, Hadfield J. RNA sequencing: the teenage years. Nat Rev Genet. 2019;20(11):631–56.
Baralle FE, Giudice J. Alternative splicing as a regulator of development and tissue identity. Nat Rev Mol Cell Biol. 2017;18(7):437–51.
Zhang X, Yan C, Hang J, Finci LI, Lei J, Shi Y. An atomic structure of the human spliceosome. Cell. 2017;169(5):918–929e14.
Anczuków O, Krainer AR. Splicing-factor alterations in cancers. RNA. 2016;22(9):1285–301.
Graveley BR. Sorting out the complexity of SR protein functions. RNA. 2000;6(9):1197–211.
Fu XD, Ares M. Context-dependent control of alternative splicing by RNA-binding proteins. Nat Rev Genet. 2014;15(10):689–701.
Änkö ML. Regulation of gene expression programmes by serine-arginine rich splicing factors. Semin Cell Dev Biol. 2014;32:11–21.
Long JC, Caceres JF. The SR protein family of splicing factors: master regulators of gene expression. Biochem J. 2009;417(1):15–27.
Busch A, Hertel KJ. Evolution of SR protein and hnRNP splicing regulatory factors. Wiley Interdiscip Rev RNA. 2012;3(1):1–12.
Lam BJ, Hertel KJ. A general role for splicing enhancers in exon definition. RNA. 2002;8(10):1233–41.
Jin C, Dong D, Yang Z, Xia R, Tao S, Piao M. CircMYC regulates glycolysis and cell proliferation in Melanoma. Cell Biochem Biophys. 2020;78(1):77–88.
Gammons MV, Lucas R, Dean R, Coupland SE, Oltean S, Bates DO. Targeting SRPK1 to control VEGF-mediated tumour angiogenesis in metastatic melanoma. Br J Cancer. 2014;111(3):477–85.
Moreira GA, Lima GD, de Siqueira A, Barros RP, de Adjanohoun MV, Santos ALM. Antimetastatic effect of the pharmacological inhibition of serine/arginine-rich protein kinases (SRPK) in murine melanoma. Toxicol Appl Pharmacol. 2018;356:214–23.
Caetano MMM, Moreira GA, da Silva MR, Guimarães GR, Santos L, de de O, Pacheco A. Impaired expression of serine/arginine protein kinase 2 (SRPK2) affects melanoma progression. Front Genet. 2022;13:979735.
Moreira GA, Caetano MMM, do Vale JA, de Paiva JC, Gonçalves VHS, Almeida AA, et al. The SRPK inhibitor N-(2-(piperidin-1-yl)-5-(trifluoromethyl)phenyl) isonicotinamide (SRPIN340) increases the immune response against metastatic melanoma in mice. Biochem Pharmacol. 2022;203:115161.
Tang Y, Horikawa I, Ajiro M, Robles AI, Fujita K, Mondal AM, et al. Downregulation of splicing factor SRSF3 induces p53β, an alternatively spliced isoform of p53 that promotes cellular senescence. Oncogene. 2013;32(22):2792–8.
Corbo C, Orrù S, Salvatore F. SRp20: an overview of its role in human diseases. Biochem Biophys Res Commun. 2013;436(1):1–5.
Dewaele M, Tabaglio T, Willekens K, Bezzi M, Teo SX, Low DHP, et al. Antisense oligonucleotide-mediated MDM4 exon 6 skipping impairs tumor growth. J Clin Invest. 2016;126(1):68–84.
Jiang CC, Lai F, Tay KH, Croft A, Rizos H, Becker TM, et al. Apoptosis of human melanoma cells induced by inhibition of B-RAFV600E involves preferential splicing of bimS. Cell Death Dis. 2010;1(9):e69.
Lai F, Jiang CC, Farrelly ML, Zhang XD, Hersey P. Evidence for upregulation of Bim and the splicing factor SRp55 in melanoma cells from patients treated with selective BRAF inhibitors. Melanoma Res. 2012;22(3):244–51.
Geuens T, Bouhy D, Timmerman V. The hnRNP family: insights into their role in health and disease. Hum Genet. 2016;135(8):851–67.
Dreyfuss G, Matunis MJ, Piñol-Roma S, Burd CG. hnRNP proteins and the biogenesis of mRNA. Annu Rev Biochem. 1993;62:289–321.
Golan-Gerstl R, Cohen M, Shilo A, Suh SS, Bakàcs A, Coppola L, et al. Splicing factor hnRNP A2/B1 regulates tumor suppressor gene splicing and is an oncogenic driver in glioblastoma. Cancer Res. 2011;71(13):4464–72.
Clower CV, Chatterjee D, Wang Z, Cantley LC, Vander Heiden MG, Krainer AR. The alternative splicing repressors hnRNP A1/A2 and PTB influence pyruvate kinase isoform expression and cell metabolism. Proc Natl Acad Sci U S A. 2010;107(5):1894–9.
Babic I, Anderson ES, Tanaka K, Guo D, Masui K, Li B, et al. EGFR mutation-induced alternative splicing of Max contributes to growth of glycolytic tumors in brain cancer. Cell Metab. 2013;17(6):1000–8.
David CJ, Chen M, Assanah M, Canoll P, Manley JL. HnRNP proteins controlled by c-Myc deregulate pyruvate kinase mRNA splicing in cancer. Nature. 2010;463(7279):364–8.
Sl YL. S. The roles of hnRNP A2/B1 in RNA biology and disease. Wiley interdisciplinary reviews RNA [Internet]. 2021 Mar [cited 2023 May 14];12(2). Available from: https://pubmed.ncbi.nlm.nih.gov/32588964/.
Geng G, Xu C, Peng N, Li Y, Liu J, Wu J, et al. PTBP1 is necessary for dendritic cells to regulate T-cell homeostasis and antitumour immunity. Immunology. 2021;163(1):74–85.
Huang Q, Gu S, Fang J, Li X, Lin L. A pan-cancer analysis of the oncogenic role of polypyrimidine tract binding protein 1 (PTBP1) in human tumors. Med (Baltim). 2022;101(52):e32428.
Ladányi A, Rásó E, Barbai T, Vízkeleti L, Puskás LG, Kovács SA, et al. Identification of a Tumor Cell Associated Type I IFN Resistance Gene expression signature of human melanoma, the components of which have a predictive potential for Immunotherapy. Int J Mol Sci. 2022;23(5):2704.
Marzese DM, Liu M, Huynh JL, Hirose H, Donovan NC, Huynh KT, et al. Brain metastasis is predetermined in early stages of cutaneous melanoma by CD44v6 expression through epigenetic regulation of the spliceosome. Pigment Cell Melanoma Res. 2015;28(1):82–93.
Charpentier M, Dupré E, Fortun A, Briand F, Maillasson M, Com E, et al. hnRNP-A1 binds to the IRES of MELOE-1 antigen to promote MELOE-1 translation in stressed melanoma cells. Mol Oncol. 2022;16(3):594–606.
Chu M, Wan H, Zhang X. Requirement of splicing factor hnRNP A2B1 for tumorigenesis of melanoma stem cells. Stem Cell Res Ther. 2021;12(1):90.
Mo L, Meng L, Huang Z, Yi L, Yang N, Li G. An analysis of the role of HnRNP C dysregulation in cancers. Biomark Res. 2022;10(1):19.
Coa LL, Abreu TF, Tashima AK, Green J, Pascon RC, Vallim MA, et al. AKT/protein kinase B associates with β-actin in the nucleus of melanoma cells. Biosci Rep. 2019;39(1):BSR20181312.
Cretu C, Schmitzová J, Ponce-Salvatierra A, Dybkov O, De Laurentiis EI, Sharma K, et al. Molecular Architecture of SF3b and Structural consequences of its Cancer-related mutations. Mol Cell. 2016;64(2):307–19.
Will CL, Urlaub H, Achsel T, Gentzel M, Wilm M, Lührmann R. Characterization of novel SF3b and 17S U2 snRNP proteins, including a human Prp5p homologue and an SF3b DEAD-box protein. EMBO J. 2002;21(18):4978–88.
Inoue D, Abdel-Wahab O. Modeling SF3B1 mutations in Cancer: advances, challenges, and opportunities. Cancer Cell. 2016;30(3):371–3.
Kanagal-Shamanna R, Montalban-Bravo G, Sasaki K, Darbaniyan F, Jabbour E, Bueso-Ramos C, et al. Only SF3B1 mutation involving K700E independently predicts overall survival in myelodysplastic syndromes. Cancer. 2021;127(19):3552–65.
Harbour JW, Roberson EDO, Anbunathan H, Onken MD, Worley LA, Bowcock AM. Recurrent mutations at codon 625 of the splicing factor SF3B1 in uveal melanoma. Nat Genet. 2013;45(2):133–5.
Kong Y, Krauthammer M, Halaban R. Rare SF3B1 R625 mutations in cutaneous melanoma. Melanoma Res. 2014;24(4):332–4.
Nguyen JQN, Drabarek W, Yavuzyigitoglu S, Medico Salsench E, Verdijk RM, Naus NC, et al. Spliceosome mutations in Uveal Melanoma. Int J Mol Sci. 2020;21(24):9546.
Liu B, Liu Z, Chen S, Ki M, Erickson C, Reis-Filho JS, et al. Mutant SF3B1 promotes AKT- and NF-κB-driven mammary tumorigenesis. J Clin Invest. 2021;131(1):e138315.
Field MG, Harbour JW. Recent developments in prognostic and predictive testing in uveal melanoma. Curr Opin Ophthalmol. 2014;25(3):234–9.
Bigot J, Lalanne AI, Lucibello F, Gueguen P, Houy A, Dayot S, et al. Splicing patterns in SF3B1-Mutated Uveal Melanoma Generate Shared Immunogenic Tumor-Specific Neoepitopes. Cancer Discov. 2021;11(8):1938–51.
Harper J, Adams KJ, Bossi G, Wright DE, Stacey AR, Bedke N, et al. An approved in vitro approach to preclinical safety and efficacy evaluation of engineered T cell receptor anti-CD3 bispecific (ImmTAC) molecules. PLoS ONE. 2018;13(10):e0205491.
Liddy N, Bossi G, Adams KJ, Lissina A, Mahon TM, Hassan NJ, et al. Monoclonal TCR-redirected tumor cell killing. Nat Med. 2012;18(6):980–7.
Hluchý M, Gajdušková P, Ruiz de Los Mozos I, Rájecký M, Kluge M, Berger BT, et al. CDK11 regulates pre-mRNA splicing by phosphorylation of SF3B1. Nature. 2022;609(7928):829–34.
Burbage M, Rocañín-Arjó A, Baudon B, Arribas YA, Merlotti A, Rookhuizen DC, et al. Epigenetically controlled tumor antigens derived from splice junctions between exons and transposable elements. Sci Immunol. 2023;8(80):eabm6360.
Yang HD, Nam SW. Pathogenic diversity of RNA variants and RNA variation-associated factors in cancer development. Exp Mol Med. 2020;52(4):582–93.
Song WM, Agrawal P, Von Itter R, Fontanals-Cirera B, Wang M, Zhou X, et al. Network models of primary melanoma microenvironments identify key melanoma regulators underlying prognosis. Nat Commun. 2021;12(1):1214.
Wellbrock C. MAPK pathway inhibition in melanoma: resistance three ways. Biochem Soc Trans. 2014;42(4):727–32.
Lavoie H, Sahmi M, Maisonneuve P, Marullo SA, Thevakumaran N, Jin T, et al. MEK drives BRAF activation through allosteric control of KSR proteins. Nature. 2018;554(7693):549–53.
Pupo GM, Boyd SC, Fung C, Carlino MS, Menzies AM, Pedersen B, et al. Clinical significance of intronic variants in BRAF inhibitor resistant melanomas with altered BRAF transcript splicing. Biomark Res. 2017;5:17.
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–54.
Roskoski R. Targeting oncogenic raf protein-serine/threonine kinases in human cancers. Pharmacol Res. 2018;135:239–58.
Poulikakos PI, Persaud Y, Janakiraman M, Kong X, Ng C, Moriceau G, et al. RAF inhibitor resistance is mediated by dimerization of aberrantly spliced BRAF(V600E). Nature. 2011;480(7377):387–90.
Salton M, Kasprzak WK, Voss T, Shapiro BA, Poulikakos PI, Misteli T. Inhibition of vemurafenib-resistant melanoma by interference with pre-mRNA splicing. Nat Commun. 2015;6:7103.
Hartsough EJ, Kugel CH, Vido MJ, Berger AC, Purwin TJ, Goldberg A, et al. Response and resistance to Paradox-breaking BRAF inhibitor in Melanomas in vivo and Ex vivo. Mol Cancer Ther. 2018;17(1):84–95.
Basile KJ, Le K, Hartsough EJ, Aplin AE. Inhibition of mutant BRAF splice variant signaling by next-generation, selective RAF inhibitors. Pigment Cell Melanoma Res. 2014;27(3):479–84.
Roy S, McPherson RA, Apolloni A, Yan J, Lane A, Clyde-Smith J, et al. 14-3-3 facilitates ras-dependent Raf-1 activation in vitro and in vivo. Mol Cell Biol. 1998;18(7):3947–55.
Hekman M, Wiese S, Metz R, Albert S, Troppmair J, Nickel J, et al. Dynamic changes in C-Raf phosphorylation and 14-3-3 protein binding in response to growth factor stimulation: differential roles of 14-3-3 protein binding sites. J Biol Chem. 2004;279(14):14074–86.
Hmitou I, Druillennec S, Valluet A, Peyssonnaux C, Eychène A. Differential regulation of B-raf isoforms by phosphorylation and autoinhibitory mechanisms. Mol Cell Biol. 2007;27(1):31–43.
Ritt DA, Monson DM, Specht SI, Morrison DK. Impact of feedback phosphorylation and raf heterodimerization on normal and mutant B-Raf signaling. Mol Cell Biol. 2010;30(3):806–19.
Yao Z, Torres NM, Tao A, Gao Y, Luo L, Li Q, et al. BRAF mutants evade ERK-Dependent feedback by different mechanisms that determine their sensitivity to pharmacologic inhibition. Cancer Cell. 2015;28(3):370–83.
Park E, Rawson S, Li K, Kim BW, Ficarro SB, Pino GGD, et al. Architecture of autoinhibited and active BRAF-MEK1-14-3-3 complexes. Nature. 2019;575(7783):545–50.
Vido MJ, Rock J, Aplin AE. Role of serine 365 in BRAF V600E sensitivity to RAF inhibition. Pigment Cell Melanoma Res. 2021;34(4):696–702.
McCormick F. Ras-related proteins in signal transduction and growth control. Mol Reprod Dev. 1995;42(4):500–6.
Jakob JA, Bassett RL, Ng CS, Curry JL, Joseph RW, Alvarado GC, et al. NRAS mutation status is an independent prognostic factor in metastatic melanoma. Cancer. 2012;118(16):4014–23.
Kwong LN, Costello JC, Liu H, Jiang S, Helms TL, Langsdorf AE, et al. Oncogenic NRAS signaling differentially regulates survival and proliferation in melanoma. Nat Med. 2012;18(10):1503–10.
Michielin O, van Akkooi ACJ, Ascierto PA, Dummer R, Keilholz U, ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Cutaneous melanoma: ESMO Clinical Practice guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2019;30(12):1884–901.
Guida M, Bartolomeo N, Quaglino P, Madonna G, Pigozzo J, Di Giacomo AM, et al. No impact of NRAS Mutation on features of primary and metastatic melanoma or on outcomes of checkpoint inhibitor immunotherapy: an Italian Melanoma Intergroup (IMI) Study. Cancers (Basel). 2021;13(3):475.
Thomas NE, Edmiston SN, Alexander A, Groben PA, Parrish E, Kricker A, et al. Association between NRAS and BRAF Mutational Status and Melanoma-Specific Survival among patients with higher-risk primary melanoma. JAMA Oncol. 2015;1(3):359–68.
Dummer R, Schadendorf D, Ascierto PA, Arance A, Dutriaux C, Di Giacomo AM, et al. Binimetinib versus dacarbazine in patients with advanced NRAS-mutant melanoma (NEMO): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18(4):435–45.
Randic T, Kozar I, Margue C, Utikal J, Kreis S. NRAS mutant melanoma: towards better therapies. Cancer Treat Rev. 2021;99:102238.
Ak E, Kw SS, Cj H. W, S L, R P, NRAS isoforms differentially affect downstream pathways, cell growth, and cell transformation. Proceedings of the National Academy of Sciences of the United States of America [Internet]. 2014 Mar 18 [cited 2023 May 15];111(11). Available from: https://pubmed.ncbi.nlm.nih.gov/24586049/.
Burd CE, Liu W, Huynh MV, Waqas MA, Gillahan JE, Clark KS, et al. Mutation-specific RAS oncogenicity explains NRAS codon 61 selection in melanoma. Cancer Discov. 2014;4(12):1418–29.
Identification of NRAS isoform. 2 overexpression as a mechanism facilitating BRAF inhibitor resistance in malignant melanoma - PubMed [Internet]. [cited 2023 May 15]. Available from: https://pubmed.ncbi.nlm.nih.gov/28827320/.
Markowitz J, Mal TK, Yuan C, Courtney NB, Patel M, Stiff AR, et al. Structural characterization of NRAS isoform 5. Protein Sci. 2016;25(5):1069–74.
Duggan MC, Regan-Fendt K, Olaverria Salavaggione GN, Howard JH, Stiff AR, Sabella J, et al. Neuroblastoma RAS viral oncogene homolog mRNA is differentially spliced to give five distinct isoforms: implications for melanoma therapy. Melanoma Res. 2019;29(5):491–500.
Rásó E. Splice variants of RAS-translational significance. Cancer Metastasis Rev. 2020;39(4):1039–49.
Posch C, Ortiz-Urda S. NRAS mutant melanoma–undrugable? Oncotarget. 2013;4(4):494–5.
Mandalà M, Merelli B, Massi D. Nras in melanoma: targeting the undruggable target. Crit Rev Oncol Hematol. 2014;92(2):107–22.
Youle RJ, Strasser A. The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol. 2008;9(1):47–59.
Eberle J, Hossini AM. Expression and function of bcl-2 proteins in melanoma. Curr Genomics. 2008;9(6):409–19.
Kale J, Osterlund EJ, Andrews DW. BCL-2 family proteins: changing partners in the dance towards death. Cell Death Differ. 2018;25(1):65–80.
Liu Q, Moldoveanu T, Sprules T, Matta-Camacho E, Mansur-Azzam N, Gehring K. Apoptotic regulation by MCL-1 through heterodimerization. J Biol Chem. 2010;285(25):19615–24.
Ku B, Liang C, Jung JU, Oh BH. Evidence that inhibition of BAX activation by BCL-2 involves its tight and preferential interaction with the BH3 domain of BAX. Cell Res. 2011;21(4):627–41.
Czabotar PE, Westphal D, Dewson G, Ma S, Hockings C, Fairlie WD, et al. Bax crystal structures reveal how BH3 domains activate Bax and nucleate its oligomerization to induce apoptosis. Cell. 2013;152(3):519–31.
Moldoveanu T, Grace CR, Llambi F, Nourse A, Fitzgerald P, Gehring K, et al. BID-induced structural changes in BAK promote apoptosis. Nat Struct Mol Biol. 2013;20(5):589–97.
Lucianò AM, Pérez-Oliva AB, Mulero V, Del Bufalo D. Bcl-xL: a focus on Melanoma Pathobiology. Int J Mol Sci. 2021;22(5):2777.
Cui J, Placzek WJ. Post-transcriptional regulation of anti-apoptotic BCL2 family members. Int J Mol Sci. 2018;19(1):308.
Moore MJ, Wang Q, Kennedy CJ, Silver PA. An alternative splicing network links cell-cycle control to apoptosis. Cell. 2010;142(4):625–36.
McKee CS, Hill DS, Redfern CPF, Armstrong JL, Lovat PE. Oncogenic BRAF signalling increases Mcl-1 expression in cutaneous metastatic melanoma. Exp Dermatol. 2013;22(11):767–9.
Tseng HY, Dreyer J, Emran AA, Gunatilake D, Pirozyan M, Cullinane C, et al. Co-targeting bromodomain and extra-terminal proteins and MCL1 induces synergistic cell death in melanoma. Int J Cancer. 2020;147(8):2176–89.
Aird D, Teng T, Huang CL, Pazolli E, Banka D, Cheung-Ong K, et al. Sensitivity to splicing modulation of BCL2 family genes defines cancer therapeutic strategies for splicing modulators. Nat Commun. 2019;10(1):137.
Sale MJ, Minihane E, Monks NR, Gilley R, Richards FM, Schifferli KP, et al. Targeting melanoma’s MCL1 bias unleashes the apoptotic potential of BRAF and ERK1/2 pathway inhibitors. Nat Commun. 2019;10(1):5167.
Marine JC, Jochemsen AG. Mdmx as an essential regulator of p53 activity. Biochem Biophys Res Commun. 2005;331(3):750–60.
D D, E M, D P, D M, M C, R F, et al. Amplification of Mdmx (or Mdm4) directly contributes to tumor formation by inhibiting p53 tumor suppressor activity. Molecular and cellular biology [Internet]. 2004 Jul [cited 2023 May 15];24(13). Available from: https://pubmed.ncbi.nlm.nih.gov/15199139/.
Gm FT. W. Regulating the p53 pathway: in vitro hypotheses, in vivo veritas. Nature reviews Cancer [Internet]. 2006 Dec [cited 2023 May 15];6(12). Available from: https://pubmed.ncbi.nlm.nih.gov/17128209/.
Yc MW, Gm L. W. MDM2, MDMX and p53 in oncogenesis and cancer therapy. Nature reviews Cancer [Internet]. 2013 Feb [cited 2023 May 15];13(2). Available from: https://pubmed.ncbi.nlm.nih.gov/23303139/.
Jc M. MDM2 and MDMX in cancer and development. Current topics in developmental biology [Internet]. 2011 [cited 2023 May 15];94. Available from: https://pubmed.ncbi.nlm.nih.gov/21295684/.
Boutz PL, Bhutkar A, Sharp PA. Detained introns are a novel, widespread class of post-transcriptionally spliced introns. Genes Dev. 2015;29(1):63–80.
Zhou Z, Fu XD. Regulation of splicing by SR proteins and SR protein-specific kinases. Chromosoma. 2013;122(3):191–207.
AbuHammad S, Cullinane C, Martin C, Bacolas Z, Ward T, Chen H, et al. Regulation of PRMT5-MDM4 axis is critical in the response to CDK4/6 inhibitors in melanoma. Proc Natl Acad Sci U S A. 2019;116(36):17990–8000.
Dean JL, McClendon AK, Hickey TE, Butler LM, Tilley WD, Witkiewicz AK, et al. Therapeutic response to CDK4/6 inhibition in breast cancer defined by ex vivo analyses of human tumors. Cell Cycle. 2012;11(14):2756–61.
Herrera-Abreu MT, Palafox M, Asghar U, Rivas MA, Cutts RJ, Garcia-Murillas I, et al. Early Adaptation and Acquired Resistance to CDK4/6 inhibition in Estrogen receptor-positive breast Cancer. Cancer Res. 2016;76(8):2301–13.
Yadav V, Chen SH, Yue YG, Buchanan S, Beckmann RP, Peng SB. Co-targeting BRAF and cyclin dependent kinases 4/6 for BRAF mutant cancers. Pharmacol Ther. 2015;149:139–49.
Mahgoub T, Eustace AJ, Collins DM, Walsh N, O’Donovan N, Crown J. Kinase inhibitor screening identifies CDK4 as a potential therapeutic target for melanoma. Int J Oncol. 2015;47(3):900–8.
Yoshida A, Lee EK, Diehl JA. Induction of therapeutic senescence in Vemurafenib-Resistant melanoma by extended inhibition of CDK4/6. Cancer Res. 2016;76(10):2990–3002.
Martin CA, Cullinane C, Kirby L, Abuhammad S, Lelliott EJ, Waldeck K, et al. Palbociclib synergizes with BRAF and MEK inhibitors in treatment naïve melanoma but not after the development of BRAF inhibitor resistance. Int J Cancer. 2018;142(10):2139–52.
Gembarska A, Luciani F, Fedele C, Russell EA, Dewaele M, Villar S, et al. MDM4 is a key therapeutic target in cutaneous melanoma. Nat Med. 2012;18(8):1239–47.
Valianatos G, Valcikova B, Growkova K, Verlande A, Mlcochova J, Radova L, et al. A small molecule drug promoting miRNA processing induces alternative splicing of MdmX transcript and rescues p53 activity in human cancer cells overexpressing MdmX protein. PLoS ONE. 2017;12(10):e0185801.
Thapa R, Wilson GD. The importance of CD44 as a stem cell biomarker and therapeutic target in Cancer. Stem Cells Int. 2016;2016:2087204.
Chen C, Zhao S, Karnad A, Freeman JW. The biology and role of CD44 in cancer progression: therapeutic implications. J Hematol Oncol. 2018;11(1):64.
Loh TJ, Moon H, Cho S, Jang H, Liu YC, Tai H, et al. CD44 alternative splicing and hnRNP A1 expression are associated with the metastasis of breast cancer. Oncol Rep. 2015;34(3):1231–8.
Rall CJ, Rustgi AK. CD44 isoform expression in primary and metastatic pancreatic adenocarcinoma. Cancer Res. 1995;55(9):1831–5.
Mishra MN, Chandavarkar V, Sharma R, Bhargava D. Structure, function and role of CD44 in neoplasia. J Oral Maxillofac Pathol. 2019;23(2):267–72.
Dzobo K, Sinkala M. Cancer stem cell marker CD44 plays multiple key roles in human cancers: Immune Suppression/Evasion, Drug Resistance, epithelial-mesenchymal transition, and Metastasis. OMICS. 2021;25(5):313–32.
Zhang P, Feng S, Liu G, Wang H, Fu A, Zhu H, et al. CD82 suppresses CD44 alternative splicing-dependent melanoma metastasis by mediating U2AF2 ubiquitination and degradation. Oncogene. 2016;35(38):5056–69.
Mackereth CD, Madl T, Bonnal S, Simon B, Zanier K, Gasch A, et al. Multi-domain conformational selection underlies pre-mRNA splicing regulation by U2AF. Nature. 2011;475(7356):408–11.
Weitzenböck HP, Gschwendtner A, Wiesner C, Depke M, Schmidt F, Trautinger F, et al. Proteome analysis of NRF2 inhibition in melanoma reveals CD44 up-regulation and increased apoptosis resistance upon vemurafenib treatment. Cancer Med. 2022;11(4):956–67.
Qian Y, Liang X, Yang J, Zhao C, Nie W, Liu L, et al. Hyaluronan reduces Cationic Liposome-Induced toxicity and enhances the Antitumor Effect of targeted gene delivery in mice. ACS Appl Mater Interfaces. 2018;10(38):32006–16.
Hassn Mesrati M, Syafruddin SE, Mohtar MA, Syahir A. CD44: a multifunctional mediator of Cancer Progression. Biomolecules. 2021;11(12):1850.
Hammond SM, Wood MJA. Genetic therapies for RNA mis-splicing diseases. Trends Genet. 2011;27(5):196–205.
Lee SCW, Abdel-Wahab O. Therapeutic targeting of splicing in cancer. Nat Med. 2016;22(9):976–86.
Bauman JA, Li SD, Yang A, Huang L, Kole R. Anti-tumor activity of splice-switching oligonucleotides. Nucleic Acids Res. 2010;38(22):8348–56.
Bernard A, Boidot R, Végran F. Alternative splicing in Cancer and Immune cells. Cancers (Basel). 2022;14(7):1726.
Acknowledgements
The authors sincerely thank all participants in the study.
Funding
This study was supported by the National Natural Science Foundation of China (No. 82071101, 82002068 and 82272281); Natural Science Foundation of Guangdong Province (No. 2021A1515010949 and 2021A1515011142); Shantou Science and Technology Project (No. 200624095260243).
Author information
Authors and Affiliations
Contributions
XPZ, WCZ and SJT designed the study; XPZ, WXC, XSH, XFC and QHX analyzed and interpreted the data; XPZ, DYG and GHG wrote the main manuscript text and edited various parts of the manuscript text. SJT and JSC supervised the data analysis and prepared the final draft. All authors were involved in the initial drafting, review, and approval of the manuscript and the decision to submit it for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, W., Geng, D., Chen, J. et al. Roles and mechanisms of aberrant alternative splicing in melanoma — implications for targeted therapy and immunotherapy resistance. Cancer Cell Int 24, 101 (2024). https://doi.org/10.1186/s12935-024-03280-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-024-03280-x