Abstract
Objective
We aimed to examine the association of triglyceride-glucose index (TyG) with risk for cardiovascular disease (CVD) among postmenopausal women.
Methods
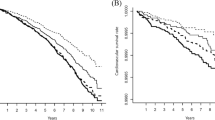
A total of 7741 participants met the inclusion criteria, and were included in the analysis. The TyG index was calculated as ln (triglyceride [mg/dL] × fasting blood glucose [mg/dL]/2). The participants were classified into four groups by the quartiles of TyG index, and the Q1 group was used as the reference group. The cumulative incidence of CVD for the groups were compared using the Kaplan–Meier curves. The association between the TyG index and risk of CVD among postmenopausal women was assessed by the Cox proportional hazards models (hazard ratio [HR], 95% confidence intervals [CI]).
Results
During a median follow-up of 12 years, a total of 383 (4.95%) participants developed incident CVD. After adjusting for potential confounding factors, a high baseline TyG index (Q4 group) was associated with higher future risk of CVD, the HR (95% CI) of CVD risk was 1.70 (1.21–2.38) in Q4 group compared with the Q1 group. Subgroup analyses showed the Q4 group was significantly associated with the risk of CVD, regardless of age at menopause (younger than 50 years; 50 years and older) and obesity status.
Conclusions
Higher TyG index at baseline as a marker of insulin resistance (IR), is associated with higher risk of future CVD among postmenopausal women. The TyG index may serve as a simple and easy marker for early identification of high-risk individuals in the postmenopausal women.
Similar content being viewed by others
Introduction
The Lancet women and cardiovascular disease Commission reported that the prevalence of cardiovascular disease (CVD) increased by 7.5% in Chinese women during the past the 30 years. CVD is the leading cause of death in women worldwide, and accounts for nearly 35% of all global deaths in women [1]. It is critically significant for a focus on women’s health, exploring influencing factors and preventive strategies of CVD to delay and lower risk for CVD, thus alleviating the global burden of CVD. Several studies have showed that insulin resistance (IR), which is defined as a reduced efficiency of promoting glucose uptake to tissue and inhibiting hepatic glucose production, is a significant risk factors for CVD [2,3,4]. The menopausal transition is associated with an increase in IR and contributes to deteriorate cardiometabolic transition. Therefore, menopausal transition is associated with increased risk for cardiometabolic disease such as CVD [5, 6]. Focusing on IR in postmenopausal women and implementing early intervention strategies may be key for postmenopausal women to lower the risk of future CVD. A prospective cohort studies including 15,288 postmenopausal women indicates that IR, which is assessed by homeostasis model assessment of IR (HOMA-IR) based on fasting glucose and insulin levels, is associated with the risk for the development of CVD [7]. However, IR measured by insulin concentrations is not measured routinely in clinical practice, which is not suitable for daily large-scale clinical studies. Previous studies had found triglyceride–glucose (TyG) index was suggested as a non-invasive, simple, reliable and effective surrogate marker of IR [8, 9]. And TyG index have been shown to be associated with higher risk of CVD in the general population [10]. However, to the best of our knowledge, no relevant studies have investigated the association between the TyG index and CVD in postmenopausal women. Thus, we aimed to investigated the association between the TyG index and future CVD among postmenopausal women based on Kailuan Study.
Methods
Study population and design
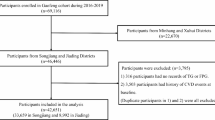
The Kailuan study, an ongoing prospective cohort study, was initiated in 2006 years and conducted follow-up every 2 years and biannually thereafter [11, 12]. A total of 101,510 participants (81,110 men and 20,400 women) aged 18–98 years old completed the first health examination and collected related information in the Kailuan general hospital and its 10 affiliated hospitals.
A total of 9407 participants who participated in the health examinations from 2006 to 2015 and with complete menopausal information were included. We excluded 1666 participants who could meet the following criteria: (1) 27 participants with history of cardiovascular disease; and (2) 1639 participants with missing data of triglyceride (TG) and/or fasting blood glucose (FBG) at baseline. Therefore, a total of 7741 participants were finally included in the analysis (Additional file 1: Figure S1).
This study was approved by the ethics committees of Kailuan General Hospital (Approval Number: 2006-05) and informed consent had been obtained from all the participants. The study was performed according to the guidelines of the Helsinki Declaration.
Data collection and definitions
Information on participants’ sociodemographic characteristics, history of CVD, medication use, and lifestyle, including age, gender, smoking status, drinking status, physical activity, educational status, menopausal information, and so on, were collected using questionnaires by professionally trained employees, details are provided in reference [13]. Smoking and drinking status were classified into current, former or never smokers. Physical activity was defined as exercising at least 4 times a week, with at least 20 min each time. Salt intake was classified as < 6 g/day, 6–12 g/day, and > 12 g/day according to questions related to salt intake. Education status was categorized as illiterate, primary school, junior high school, high school, and college degree or above. Body mass index (BMI, kg/m2) was calculated as weight (kg) divided by height2 (m2). Systolic blood pressure and diastolic blood pressure were measured 3 times repeatedly by qualified medical personnel using standard methods, and the results were averaged [14]. Menopausal information included menopausal or not, age at menarche, age at menopause, and menstrual cycle. Self-reported menopausal status was categorized as postmenopausal and premenopausal, whether it was natural or surgical induced.
Blood samples were drawn on the day of physical examination after at least 8 h of fasting. The biochemical index, including total cholesterol (TC), FBG, TG, low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C), high sensitive C-reactive protein (Hs-CRP), and so on, were measured on the Hitachi automatic biochemical analyzer (Hitachi 747, Tokyo, Japan) [15].
We defined hypertension as self-reported use of antihypertensive medication or a BP measurement ≥ 140/90 mm Hg (1 mm Hg = 0.133 kPa) or a self-reported history [16].
Diabetes was defined as FBG ≥ 7 mmol/L or a self-reported use of anti-diabetic drugs or medical history of diabetes [17]. Dyslipidemia was defined as non-HDL cholesterol level ≥ 4.9 mmol/L or self-reported use of lipid-lowering drugs.
Assessment of TyG index
The TyG index was calculated as ln (TG [mg/dL] × FBG [mg/dL]/2) [9]. The TyG index at baseline was calculated from the date on TG and FBG first measured from 2006 to 2015 years. The participants were classified into four groups (Q1, Q2, Q3, Q4) by the quartiles of TyG index, and the Q1 group was used as the reference group.
Outcomes and follow-up
This study took the date of first physical examination in postmenopausal women as baseline, and the date of follow-up was 31 December 2020. The study endpoint was the first incident CVD, death or 31 December 2020, whichever came first. The CVD included myocardial infarction (MI) and stroke according to the World Health Organization criteria [18, 19]. The CVD events were diagnosed by trained medical staff through the hospital’s electronic medical records review and medical insurance system. Information on death was collected from death certificates from state vital statistics offices and discharge electronic medical records.
Statistical analysis
Continuous variables of normal distribution were described using mean and standard deviation (SD). Skewed variables were presented as median and interquartile range (M [P25, P75]). Categorical variables were expressed by the number of case and percentage. The cumulative incidence of CVD for the groups were compared using the Kaplan–Meier curves. The Cox proportional hazards models were applied to assess the association between the TyG index and risk of CVD among postmenopausal women. Model 1 was adjusted for age at baseline; model 2 included the covariates in model 1, BMI, education status, current drinker, current smoker, and physical activity; model 3 included the covariates in model 2, salt intake, LDL-C, HDL-C, hypertension, and diabetes; model 4 further adjusted for age at menopause.
We conducted several stratified and sensitivity analyses to test the stability of our results. First, we conducted analyses stratified by hypertension status (yes or no), age at menopause (< 50 years or ≥ 50 years), diabetes status (yes or no), BMI level (< 28 kg/m2 or ≥ 28 kg/m2), and evaluated the interaction via a likelihood ratio test. Second, we carried out sensitivity analysis after excluding those who used anti-diabetic drugs, antihypertensive drugs, or lipid-lowering drugs. Another sensitivity analyses were conducted after excluding participants with diabetes or severe dyslipidemia. Sensitivity analyses were also conducted by subtypes of CVD (MI and stroke).
All statistical analyses were conducted using SAS 9.4 (SAS Institute, Inc., Cary, NC, USA), and a two-tailed P < 0.05 was considered statistically significant.
Results
Baseline characteristics
The baseline characteristics of the participants by the quartiles of the TyG index are shown in Table 1. A total of 7741 participants were included in the study, with a mean age of 55.49 (SD = 6.24) years at baseline and 50.19 (SD = 3.41) years at menopause.
Association between TyG index and risk of cardiovascular disease among postmenopausal women
During a median follow-up of 12 years, a total of 383 (4.95%) participants developed incident CVD. The Kaplan–Meier survival curves showed the participants in Q4 group had a higher cumulative incidence for CVD compared with those of other groups over follow-up time (log-rank test, P < 0.01; Fig. 1).
Table 2 showed the association between a high baseline TyG index (Q4 group) and future risk of CVD after adjusting for potential confounding factors. In model 1, the HR (95%CI) of CVD risk was 2.76 (2.02–3.75) in Q4 group compared with the Q1 group. After adjusting for variables in model 1 plus BMI, education status, current drinker, current smoker, physical activity at baseline, the Q4 group showed an increased risk of developing CVD (HR [95% CI], 2.40 [1.75–3.29]) compared to the Q1 group. In model 3, the Q4 group had a 70% increased risk of CVD compared with Q1 group. Further adjustment for age at menopause yielded similar results (Q4 HR: 1.70, 95% CI 1.21–2.38).
Subgroup analyses
Table 3 showed the results of the subgroup analyses. Among postmenopausal women, the Q4 group was significantly associated with the risk of CVD, regardless of age at menopause (younger than 50 years; 50 years and older) and BMI level (< 28 and ≥ 28 kg/m2). The highest quartile of baseline TyG index was associated with an increased risk of CVD in participants without a history of diabetes mellitus or hypertension. The highest quartile of baseline TyG index was not associated with CVD in participants with a history of diabetes mellitus or hypertension. There was no interaction in the all subgroups.
Sensitivity analyses
After adjustment for variables in the model 2, compared with participants in the Q1 group, the adjusted HR (95% CI) for MI in the highest quartile of baseline TyG index was 2.98 (1.34–6.64). However, there were no significant associations between baseline TyG index and MI, after adjusting for variables in the model 3 or 4. After adjusting for variables in the model 2, 3 or 4, there were a significant association between the highest quartile of TyG index and risk of stroke (Additional file 2: Table S1).
The associations between the highest quartile of baseline TyG index and risk of CVD were similar after excluding participants who received anti-diabetic drugs, lipid-lowering drugs, or antihypertensive drugs (Additional file 2: Table S2).
Discussion
In the Kailuan study, we observed that higher TyG index at baseline, was associated with higher risk of future CVD and stroke among postmenopausal women regardless age at menopause and obesity status. However, the association between the TyG index and MI was not significant.
Previous several studies revealed that TyG index was associated with an increased CVD risk [20]. And one study indicated stronger association between TyG index and MI risk in females than in males [21]. A prospective cohort study demonstrated higher levels of fasting serum insulin and HOMA-IR were associated with hypertension in women whereas hypertension in men [22]. A protection cardiovascular effect by estrogen decreases and IR increases in postmenopausal women [23]. As a result, monitoring the association between TyG index and risk of CVD in postmenopausal women has implications for the prevention of CVD. Our study found that higher TyG index has significant association with increased risk of future CVD, and this association was attenuated but remained significant after adjusting for HDL-C. The result which derived from a retrospective study including 869 postmenopausal women is similar with our result, and demonstrated that the TyG index may be a predictor of coronary artery disease risk [24]. We found a study including 15,288 postmenopausal women who had a median age of 64 years showed HOMA-IR remained associated with high risk of CVD after adjusting for most CVD risk factors, whereas this association was not significant after adjusting for HDL-C (HR, 1.06; 95% CI 0.98–1.15) [7]. The possible cause that our study differs from our results was racial and residence difference. Thus, our findings might be more applicable to population in northern China.
In model 2 of our study, the highest quartile of baseline TyG index was associated with higher risk of developing MI. However, the association between baseline TyG index and risk of MI was not statistically significant in the full model. But the study result indicated the higher the quartile of Tyg index, the higher the HR. A study including 6093 participants from the third National Health and Nutrition Examination Survey demonstrated the TyG index > 9 was associated with increased risk of subclinical myocardial damage (odd ratio [OR] = 1.21, 95% CI 1.03–1.43) [25]. Several other studies have shown that an elevated TyG index at baseline is associated with risk of MI [26, 27]. Onset age of coronary heart disease was later in women than in men [28]. This lack of statistical significance in the full model of study may be the low numbers of MI events. Incidence rate has shown an increasing trend, and continuous follow-up is necessary. Hypertension is a major risk factor for CVD and contributes a larger proportion at baseline 3270 (42.24%), which might be another cause for the lack of statistical significance [29, 30].
A study including 1250 participants without cardiovascular risk factors showed that the TyG index was an independent marker to predict subclinical coronary disease [31]. We found similar results in the participants without hypertension or diabetes. Compared with the lowest quartile of TyG index, participants in the highest quartile of TyG index were at a 102% (95% CI 1.18–3.46), 61% (95% CI 1.12–2.32) higher risk of CVD, respectively. This suggests that even in healthy population, high TyG index might have a significant impact on identifying population at high risk of CVD. And this has important significance for primary prevention of CVD.
The significance of this study is that our study found the TyG index might be recognized as a risk factor for CVD incident. The TyG index as a surrogate marker of IR was closely linked with the onset and progression of risk factors for cardiovascular such as diabetic, dyslipidemia, high baPWV and so on [13, 32]. These findings demonstrated the TyG index can identify individuals who are at high risk of developing CVD and have CV risk factors. Thus, early intervention including lifestyles intervention in high-risk individuals might prevent the onset of future CVD.
The main strengths of this study include large sample community population-based, prospective design, and IR reflected by TyG index. Nevertheless, this study involves some limitations. First, as an observational study, we cannot confirm the causal-relationship between TyG index and risk of CVD. In addition, our study population were postmenopausal northern Chinese women, further studies are needed to confirm our findings in other racial/ethnic or regions populations. Third, we cannot assess IR (HOMA) due to the lack of fasting insulin level, we could not compare the roles of TyG index with HOMA for the development of CVD.
Conclusion
In conclusion, our study implies that participants with high TyG index are at a higher risk of developing CVD among postmenopausal women. Our findings indicate the TyG index may serve as a simple and easy marker for early identification of high-risk individuals in the postmenopausal women. Lifestyle changes including physical exercise may be useful for prevention CVD incidence and development in high-risk individuals, which may reduce the burden on societies and families.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- CI:
-
Confidence interval
- DBP:
-
Diastolic blood pressure
- FBG:
-
Fasting blood glucose
- Hs-CRP:
-
High sensitive C-reactive protein
- HR:
-
Hazard ratio
- HOMA-IR:
-
Homeostasis model assessment of IR
- HDL-C:
-
High density lipoprotein cholesterol
- IR:
-
Insulin resistance
- LDL-C:
-
Low density lipoprotein cholesterol
- MI:
-
Myocardial infarction
- OR:
-
Odd ratio
- SD:
-
Standard deviation
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- TyG:
-
Triglyceride-glucose
References
Vogel B, Acevedo M, Appelman Y, Bairey Merz CN, Chieffo A, Figtree GA, et al. The Lancet women and cardiovascular disease commission: reducing the global burden by 2030. Lancet. 2021;397(10292):2385–438. https://doi.org/10.1016/S0140-6736(21)00684-X.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122. https://doi.org/10.1186/s12933-018-0762-4.
Laakso M. Is insulin resistance a feature of or a primary risk factor for cardiovascular disease? Curr Diab Rep. 2015;15(12):105. https://doi.org/10.1007/s11892-015-0684-4.
Bersch-Ferreira ÂC, Sampaio GR, Gehringer MO, Torres EAFDS, Ross-Fernandes MB, da Silva JT, et al. Association between plasma fatty acids and inflammatory markers in patients with and without insulin resistance and in secondary prevention of cardiovascular disease, a cross-sectional study. Nutr J. 2018;17(1):26. https://doi.org/10.1186/s12937-018-0342-1.
Endocrinology TLD. Menopause: a turning point for women’s health. Lancet Diabetes Endocrinol. 2022;10(6):373. https://doi.org/10.1016/S2213-8587(22)00142-5.
Nappi RE, Chedraui P, Lambrinoudaki I, Simoncini T. Menopause: a cardiometabolic transition. Lancet Diabetes Endocrinol. 2022;10(6):442–56. https://doi.org/10.1016/S2213-8587(22)00076-6.
Schmiegelow MD, Hedlin H, Stefanick ML, Mackey RH, Allison M, Martin LW, Robinson JG, Hlatky MA. Insulin resistance and risk of cardiovascular disease in postmenopausal women: a cohort study from the women’s health initiative. Circ Cardiovasc Qual Outcomes. 2015;8(3):309–16. https://doi.org/10.1161/CIRCOUTCOMES.114.001563.
Sánchez-García A, Rodríguez-Gutiérrez R, Mancillas-Adame L, González-Nava V, Díaz González-Colmenero A, Solis RC, Álvarez-Villalobos NA, González-González JG. Diagnostic accuracy of the triglyceride and glucose index for insulin resistance: a systematic review. Int J Endocrinol. 2020;2020:4678526. https://doi.org/10.1155/2020/4678526.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6(4):299–304. https://doi.org/10.1089/met.2008.0034.
Cui H, Liu Q, Wu Y, Cao L. Cumulative triglyceride-glucose index is a risk for CVD: a prospective cohort study. Cardiovasc Diabetol. 2022;21(1):22. https://doi.org/10.1186/s12933-022-01456-1.
Wu S, An S, Li W, Lichtenstein AH, Gao J, Kris-Etherton PM, et al. Association of trajectory of cardiovascular health score and incident cardiovascular disease. JAMA Netw Open. 2019;2(5):e194758. https://doi.org/10.1001/jamanetworkopen.2019.4758.
Zhang X, Liu Y, Li S, Lichtenstein AH, Chen S, Na M, et al. Alcohol consumption and risk of cardiovascular disease, cancer and mortality: a prospective cohort study. Nutr J. 2021;20(1):13. https://doi.org/10.1186/s12937-021-00671-y.
Wu S, Xu L, Wu M, Chen S, Wang Y, Tian Y. Association between triglyceride-glucose index and risk of arterial stiffness: a cohort study. Cardiovasc Diabetol. 2021;20(1):146. https://doi.org/10.1186/s12933-021-01342-2.
Huang S, Li J, Shearer GC, Lichtenstein AH, Zheng X, Wu Y, Jin C, Wu S, Gao X. Longitudinal study of alcohol consumption and HDL concentrations: a community-based study. Am J Clin Nutr. 2017;105(4):905–12. https://doi.org/10.3945/ajcn.116.144832.
Jin C, Chen S, Vaidya A, Wu Y, Wu Z, Hu FB, Kris-Etherton P, Wu S, Gao X. Longitudinal change in fasting blood glucose and myocardial infarction risk in a population without diabetes. Diabetes Care. 2017;40(11):1565–72. https://doi.org/10.2337/dc17-0610.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, National High Blood Pressure Education Program Coordinating Committee, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. https://doi.org/10.1001/jama.289.19.2560.
Zhao M, Song L, Sun L, Wang M, Wang C, Yao S, et al. Associations of type 2 diabetes onset age with cardiovascular disease and mortality: the Kailuan study. Diabetes Care. 2021. https://doi.org/10.2337/DC20-2375.
Stroke 1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO task force on stroke and other cerebrovascular disorders. Stroke. 1989;20(10):1407–31. https://doi.org/10.1161/01.str.20.10.1407.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–64. https://doi.org/10.1016/j.jacc.2018.08.1038.
Mao Q, Zhou D, Li Y, Wang Y, Xu SC, Zhao XH. The triglyceride-glucose index predicts coronary artery disease severity and cardiovascular outcomes in patients with non-ST-segment elevation acute coronary syndrome. Dis Markers. 2019;2019:6891537. https://doi.org/10.1155/2019/6891537.
Tian X, Zuo Y, Chen S, Liu Q, Tao B, Wu S, Wang A. Triglyceride-glucose index is associated with the risk of myocardial infarction: an 11-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2021;20(1):19. https://doi.org/10.1186/s12933-020-01210-5.
Arshi B, Tohidi M, Derakhshan A, Asgari S, Azizi F, Hadaegh F. Sex-specific relations between fasting insulin, insulin resistance and incident hypertension: 8.9 years follow-up in a Middle-Eastern population. J Hum Hypertens. 2015;29(4):260–7. https://doi.org/10.1038/jhh.2014.70.
Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes. 2008;32(6):949–58. https://doi.org/10.1038/ijo.2008.25.
Liu J, Bu H, Ding Z, Zhang Y, Chen Y, Gao Y. The association of triglyceride glucose index for coronary artery disease in postmenopausal women. Clin Appl Thromb Hemost. 2022;28:10760296221094030. https://doi.org/10.1177/10760296221094030.
Liu Y, Wu M, Xu J, Sha D, Xu B, Kang L. Association between triglyceride and glycose (TyG) index and subclinical myocardial injury. Nutr Metab Cardiovasc Dis. 2020;30(11):2072–6. https://doi.org/10.1016/j.numecd.2020.06.019.
da Silva A, Caldas APS, Hermsdorff HHM, Bersch-Ferreira ÂC, Torreglosa CR, Weber B, Bressan J. Triglyceride-glucose index is associated with symptomatic coronary artery disease in patients in secondary care. Cardiovasc Diabetol. 2019;18(1):89. https://doi.org/10.1186/s12933-019-0893-2.
Xu X, Huang R, Lin Y, Guo Y, Xiong Z, Zhong X, et al. High triglyceride-glucose index in young adulthood is associated with incident cardiovascular disease and mortality in later life: insight from the CARDIA study. Cardiovasc Diabetol. 2022;21(1):155. https://doi.org/10.1186/s12933-022-01593-7.
Kannel WB, Hjortland MC, McNamara PM, Gordon T. Menopause and risk of cardiovascular disease: the Framingham study. Ann Intern Med. 1976;85(4):447–52. https://doi.org/10.7326/0003-4819-85-4-447.
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–49. https://doi.org/10.1016/S0140-6736(20)30752-2.
Wu S, Song Y, Chen S, Zheng M, Ma Y, Cui L, Jonas JB. Blood pressure classification of 2017 associated with cardiovascular disease and mortality in young Chinese adults. Hypertension. 2020;76(1):251–8. https://doi.org/10.1161/HYPERTENSIONAHA.119.14239.
Park GM, Cho YR, Won KB, Yang YJ, Park S, Ann SH, et al. Triglyceride glucose index is a useful marker for predicting subclinical coronary artery disease in the absence of traditional risk factors. Lipids Health Dis. 2020;19(1):7. https://doi.org/10.1186/s12944-020-1187-0.
Park B, Lee HS, Lee YJ. Triglyceride glucose (TyG) index as a predictor of incident type 2 diabetes among nonobese adults: a 12-year longitudinal study of the Korean Genome and Epidemiology Study cohort. Transl Res. 2021;228:42–51. https://doi.org/10.1016/j.trsl.2020.08.003.
Acknowledgements
We thank all the members of the Kailuan Study for their contribution and the participants who contribution their data. All authors approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (NSFC 81960086, 82160089), the Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (CY2017-BJ02), and Special Fund Project for Doctoral Training of the Lanzhou University Second Hospital (YJS-BD-24).
Author information
Authors and Affiliations
Contributions
QL contributed to study design, data collection, data analysis and manuscript writing. JY and YW made substantial contributions to study design and intellectual direction. FS and ZL contributed to interpretation of data and revision of the drafting of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was performed according to the guidelines of the Helsinki Declaration and was approved by the Ethics Committee of Kailuan General Hospital (Approval Number: 2006-05). All participants were agreed to take part in the study and signed an informed written consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no potential competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information

Additional file 1: Figure S1
Flowchart of the study.
Additional file 2: Table S1.
Association between TyG index with MI and stroke among postmenopausal women. Table S2. Association between TyG index with cardiovascular disease among postmenopausal women in sensitivity analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Q., Si, F., Liu, Z. et al. Association between triglyceride-glucose index and risk of cardiovascular disease among postmenopausal women. Cardiovasc Diabetol 22, 21 (2023). https://doi.org/10.1186/s12933-023-01753-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01753-3