Abstract
Background
Strokes significantly impair quality of life and incur high economic and societal burdens. The triglyceride and glucose (TyG) index is a biochemical marker of insulin resistance (IR) and may have important value in the prediction of strokes, especially ischemic stroke (IS). Our study aims to investigate the relationship between TyG index and IS and ascertain whether TyG index is independently associated with IS adverse outcomes.
Methods
The Cochrane, Embase, Medline, Web of Science, PubMed, and other relevant English databases and related websites were systematically searched for articles on ‘‘TyG index’’ and "stroke" published from inception to April 4, 2022. We reviewed the available literature on the TyG index and its relation to predicting IS occurrence in the general population and adverse clinical outcomes. We calculated odds ratios (OR) of TyG index and its predictability of IS occurrence and adverse outcomes. Statistical analyses were performed using the Meta Package in STATA, version 12.0.
Results
A total of 18 studies and 592,635 patients were included in our analysis. The pooled effect values of all stroke types showed that higher TyG index was associated with increased the risk of IS in the general population (OR 1.37; 95% CI 1.22–1.54) in a total sample of 554,334 cases with a high level of heterogeneity (P = 0.000, I2 = 74.10%). In addition, compared to IS patients with a lower TyG index, IS patients with a higher TyG index was associated with higher risk of stroke recurrence (OR: 1.50; 95% CI 1.19–1.89) and increased risk of mortality (OR 1.40 95% CI 1.14–1.71). No correlation was found in the effect value combinations of poor functional outcomes (OR 1.12; 95% CI 0.88–1.43) and neurological worsening (OR: 1.76; 95% CI 0.79–3.95) in a total sample of 38,301 cases with a high level of heterogeneity (P = 0.000; I2 = 77.20%).
Conclusions
TyG index has potential value in optimizing risk stratification for IS in the general population. Furthermore, there is a significant association between high TyG index and many adverse outcomes of stroke, especially stroke recurrence and high mortality. Future studies should focus on multi-center and multi-regional designs in order to further explore the relationship between IS and TyG index.
Similar content being viewed by others
Introduction
A stroke is an acute neurologic condition that occurs due to a disruption of cerebral perfusion, resulting in focal or global neurological impairment [1]. Strokes can be broadly classified into ischemic strokes (IS) and hemorrhagic strokes (HS). Approximately 84.4% of strokes are ischemic in origin [1]. Annually, over 13.7 million strokes occur globally and cause 5.5 million deaths per year as well, with a predilection for the elderly population, though increasing prevalence is being reported in younger adults [2, 3]. As stroke causes death, dementia, and disability worldwide, this common condition decreases quality of life and incurs high economic and societal burdens [4,5,6]. Despite the improvement of strategies and techniques towards the management of stroke patients in recent years, recurrence of strokes continue to account for nearly 30% of all strokes and this high rate likely represents unsuccessful secondary prevention [4, 7]. Researchers have recognized that identifying stroke-prone individuals and targeting them effectively remains an important part of stroke management; however, this is not an easy task [4]. Frans Kauwa demonstrated that predictors assessed with magnetic resonance imaging (MRI) including multiple ischemic changes and isolated cortical lesions may have potential, but computed tomography (CT) or ultrasound are not reasonable choices. Unfortunately, overuse of MRI to predict strokes was not found to be feasible, thus portraying the incomplete utility of neuroimaging in this endeavor [8]. There are several validated risk factors as a target for IS prevention, such as hypertension, diabetes mellitus, hyperlipidemia, hypercoagulable states, current smoking, atrial fibrillation (AF), and premature ventricular complexes (PVC). However, these risk factors fail to explain all cases of stroke and lack uniform applicability [4, 9].
The triglyceride-glucose (TyG) index, is a biochemical marker of insulin resistance (IR), and can be calculated as ln (fasting triglycerides (mg/dl)×fasting blood glucose (mg/dl)/2) [10, 11]. IR is known to be a key mediator of the pathogenesis of type 2 diabetes, and thus elevated stroke risk. Hyperinsulinemic-euglycemic clamp (HIEC) is considered the current gold standard to determine IR; however, HIEC is complicated and time-consuming with limited applicability for clinical practice on a large scale [11]. Therefore, the TyG index has been validated as a simple surrogate marker of IR and is cost-effective and reproducible [12]. After initial studies on its use in diabetes, many other publications now have been released which acknowledge its utility in other disorders. The TyG index has been associated with the severity of arterial stiffness, cardiovascular disease (CVD), and metabolic syndrome (MetS) (a cluster of metabolic abnormalities characterized by hypertension, dyslipidemia, obesity, and glucose dysregulation) [10, 12,13,14,15]. More interestingly, Jiao et al. also reported that a high TyG index was associated with a 1.64-fold risk of all-cause mortality and 1.36-fold risk of major adverse cardiac event in elderly acute coronary syndrome patients [10].
Stroke is one of the most significant causes of death and disability, with most of the burden in low-income and middle-income countries. Improving poststroke outcomes is an urgent issue worldwide. Several studies have investigated the association of TyG index with the risk of stroke, and its sub-types [16,17,18]. A prospective study of 54,098 participants demonstrated that patients with higher TyG index experienced a 1.30-fold increased risk of IS [19]. Huang et al. reported that long-term elevated TyG index in hypertensive patients was significantly associated with an increased risk of stroke, especially IS [20]. However, Zhao et al. demonstrated a high TyG index was not associated with nondiabetic patients with non-ST-elevation myocardial infarctions [21]. Additionally, the effect of TyG indices with studying prognosis among patients with IS also attracts great attention. A study of the 16,310 patients from the China National Stroke Registry II found that the TyG index was associated with 1.25-fold increased risk of all-cause mortality and 1.32-fold increased risk of stroke recurrence among patients with ischemic stroke [22]. This association was not found to be consistent in patients with stroke treated with intravenous thrombolysis [23].
Based on these seminal studies, there are strong implications and suggestions that the TyG index may be independently associated with stroke recurrence and clinical outcomes. Therefore, our present systematic review and meta-analysis aims to summarize and pool the current available data in order to analyze this relationship between the TyG index and IS.
Method
The Meta-analysis was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [24]. The study protocol was registered on the International Platform of Registered Systematic Review and Meta-analysis Protocols (registration number: INPLASY2022110145).
Search strategy
We searched the Cochrane Library, Embase, Medline, Web of Science, PubMed, and other relevant English databases and related websites from inception to 4 April 2022. A Google search was also conducted accordingly. We used the following appropriate Medical Subject Headings (Mesh) and free-text words to identify "triglyceride glucose index ‘‘and ’’stroke or cerebrovascular apoplexy or cerebrovascular stroke or cerebral stroke’’. The search terms and algorithm are detailed in Additional file 1: Table S1. There were no additional restrictions on time, country, or language, but ‘‘human only’’ was restricted for subjects. In addition, we manually checked the reference list of all the identified studies to search for other relevant articles.
Study selection
The inclusion criteria of the meta-analysis were as follows: (1) studies investigating the association of TyG index and the risk of IS or investigating the TyG index level with clinical outcome among patients with IS; (2) longitudinal cohort studies or cross-sectional studies; (3) adult (age > 18 years) individuals of any sex or ethnicity. The exclusion criteria of the meta-analysis were as follows: (1) The study participants included only hemorrhagic stroke; (2) conference proceedings; (3) experimental, interventional studies, reviews, case reports; (4) studies with insufficient data; (4) non-English language studies. Two reviewers (YY and HXT) independently screened the literature based on pre-established inclusion and exclusion criteria to initially identify potentially relevant studies. Any difference in the included studies was solved by discussion with another author (WY).
Data extraction
Data were extracted by two researchers (YY and HXT) independently by using the same Excel spreadsheets of related items formulated in advance, including the first author, the year of publication, country, the proportion of males, the mean age, study population, sample size, study design, study follow-up time, the definition of the TyG index, effect sizes for the association of TyG index with risk of IS or the effects of TyG index with prognosis among IS patients. After comparison of the extracted information, any differences were resolved by another author (WY).
Assessment of quality
Appropriate scales were used for quality evaluation according to different study types. The Newcastle–Ottawa Quality Assessment Scale (NOS) was used for cohort studies (scores range from 0 to 9). Studies with a NOS score of ≥ 7 were considered high quality. The Agency for Healthcare Research and Quality (AHRQ) scale used for analysis of any cross-sectional study. Given that the criteria contained 11 items, we considered studies with AHRQ scores ≥8 to be of high quality [25]. Different study types were assessed independently by two researchers (YY and FL) according to the appropriate scale. Similarly, any disagreements were resolved through discussion with another author (WY).
Statistical analysis
STATA 12.0 software was used to perform this systematic evaluation and the statistical analysis for the meta-analysis. We conducted a meta-analysis to investigate the association of TyG index with risk of IS, and determine the effects of TyG index with prognosis among IS patients. For dichotomous data, the odds ratio (OR), and 95% confidence intervals (CI) were calculated. Due to the heterogeneity of the included studies, we used a random-effects model to pool the data for all outcomes. Chi-square tests and I2 statistics were used to determine heterogeneity. A significant difference in a study was considered when P < 0.05 and I2 > 50%. Forest plots were conducted for estimation of effect sizes based on 95% confidence intervals. In order to explore the source of heterogeneity, subgroup analyses were employed for included inter-study heterogeneity and meta-regression analyses tested for the source of covariate heterogeneity between subgroups. A sensitivity analysis was used to further examine the impact of individual studies on the overall outcomes and analyze whether the results were stable and reliable. The risk of bias was evaluated using the Begg's test and Egger’s test [26].
Results
Study selection
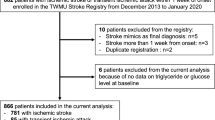
A flow sheet of the literature selection process can be visualized in Fig. 1. Through the database searches, according to the established search strategy, a total of 3468 articles were selected for subsequent filtering. Of these, 755 duplicate articles were excluded and 319 articles were removed because of non-cohort studies, non-case–control studies, and non-cross-sectional studies. After checking the title and abstract of each paper and excluding the inconsistent literature types, 23 studies were found to be pertinent to the research topic. Among them, one article was excluded due to inaccessibility of the full text [27], and four articles were further excluded after detailed review of the full text [28,29,30,31] and were found to not meet the appropriate inclusion criteria. A total of 18 original studies were finalized for inclusion in the meta-analysis, of which 8 studies [19, 21, 29, 31,32,33,34,35] were based on the risk of IS and 10 studies [22, 23, 36,37,38,39,40,41,42,43] were based on the prognosis among IS patients.
Summary of studies
The characteristics of the included studies are summarized in Table 1. 59, 2635 individuals were recorded in the 18 studies, including 38,301 IS patients and 554,334 in the general population (defined as those age ≥ 18 years who have not had a stroke). There were three cross-sectional studies [29, 38, 40] and fifteen cohort studies [19, 21,22,23, 31,32,33,34,35,36,37, 39, 41,42,43], consisting of prospective and retrospective designs, and no randomized controlled trials. The population of the original studies were mainly from China [19, 21,22,23, 29, 31,32,33,34, 36, 39, 41, 43], with three from Korea [37, 38, 40], one from Singapore [42], and one from European [35]. The primary data sources included the eICU (emergency intensive care unit) Collaborative Research Database [36], the China National Stroke Registry [22, 39, 41], the UK Biobank cohort [35], the hospital stroke-related information [21, 23, 34, 37, 38, 40, 42, 43], and the community-based or rural population studies [19, 29, 31,32,33]. IS patients included in the analysis had a larger proportion of males, with a mean age greater than 60 years. The diagnosis of stroke consists of the clinical diagnosis, imaging diagnosis, and comprehensive diagnosis. The TyG index of most articles was calculated by the general formula, which is ln[triglyceride (mg/dL) ×fasting blood glucose (mg/dL)/2] [44]. Twelve studies used TyG index quartiles [19, 22, 29, 31,32,33,34,35,36, 39, 41, 43], two used TyG index tertiles [23, 40] three others followed a TyG index dichotomy [21, 37, 42] and the remaining study did not mention specific TyG index conditions [38]. The main adverse clinical outcomes observed in the ischemic stroke patient population included stroke recurrence, all-cause mortality, impairment in functional outcomes, deterioration in neurological function. The observed outcomes in the general population were the initial occurrence of stroke.
Overall assessment of evidence quality
The cohort studies' quality assessments resulted in NOS scores of 9 for eight studies, 8 for two studies, 7 for one study, and 6 for four studies. Their scores differed in the options of whether confounders were adequately adjusted and follow-up completeness. There were 11 high-quality studies, 4 moderate-quality studies, and no low-quality studies. In the cross-sectional study, one study had an AHRQ score of 10 and two other AHRQ scores of 8, which were unclear on the items of whether subjective and objective indicators were isolated, whether confounders were adequately adjusted, and the completeness of data and follow-up. All three included cross-sectional studies were considered of high quality. Specific scores of each study are listed in Additional files 2, 3: Table S2, S3.
The association of TyG index with risk of IS in the general population
There were 554,334 individuals in the selected eight studies of the general population. TyG index conditions used in the studies included TyG index quartiles and TyG index dichotomy. Compared to the general population with a lower TyG index, the general population with a higher TyG index had a 37.10% increased risk of IS (OR: 1.37; 95%CI 1.22–1.54). Since I2 = 74.1% and P = 0.000, a random effects model was used to aggregate the correlation effect values (Fig. 2).
The subgroup analyses were performed on covariates such as study design, country, the proportion of males, mean age, sample size, study time and participants. The detailed results are described in Table 2. Then, a univariate meta-regression analysis was used to examine the potential source of heterogeneity, and it was found that heterogeneity could be partly explained by sample size (studies with larger sample sizes reported a lower risk of IS development: β = − 0.382, SE = 0.122; p = 0.020). The remaining meta-regression analysis results are presented in Additional file 4: Table S4.
To test the publication bias of the included studies, we used Begg's test (z = 0.12, P = 0.902) and Egger’s test (t = 0.03, P = 0.040), with our results suggesting that there was possible publication bias in the included studies. At the same time, a visual funnel plot revealed that individual studies tilted slightly to the right side of the funnel. Further analysis was then performed by using the clip-and-complement method, indicating that there might be one grey publications (potential/unpublished/negative studies) which had not been found. After cutting and repairing, the distribution of individual studies on both sides of the funnel was found to be more balanced (Additional file 8: Figure S1). Sensitivity analyses were also performed to determine the stability and reliability of the results and the extent in which individual studies influenced the results. The effect size after excluding individual studies was in good agreement with the total combined effect size and confidence interval (OR 1.37, 95% CI 1.22–1.54), indicating that our results were robust to a certain extent (Additional file 9: Figure S2).
The association of TyG index with prognosis among IS patients
A total sample of 38,301 cases was included in the ten IS population studies. In the IS patients, adverse clinical outcomes included stroke recurrence, all-cause mortality, impaired functional outcome, and neurological deterioration, and the same clinical outcomes were analyzed with a combined effect size. Compared with the IS population with a lower TyG index, IS patients with a higher TyG index had a higher risk of stroke recurrence (OR 1.50; 95% CI 1.19–1.89), increased risk of all-cause mortality (OR 1.40; 95% CI 1.14–1,71), while no association was found in the effect value combination of poor functional outcome (OR: 1.12; 95% CI 0.88–1.43) and neurological worsening (OR,1.76; 95% CI 0.79–3.95). Notably, Yimo Zhou's study [22] (OR 1.26; 95% CI 1.02–1.55) and Ki-Woong Nam's study [37] (OR: 2.92; 95% CI 1.35–6.29) reported that poor prognosis of neurological deterioration was associated with TyG index. Due to I2 = 77.20% and P = 0.000, a random effects model was used to aggregate the correlation effect sizes. Subsequently, the effect sizes of all clinical outcomes in ischemic stroke patients were combined, indicating that higher TyG index was associated with an increased risk of adverse clinical outcomes in ischemic stroke patients (OR 1.37; 95% CI 1.19–1.56) (Fig. 3).
In addition, we performed a subgroup analysis and meta-regression on prognosis outcomes available with more than three data items, such as stroke recurrence, all-cause mortality, and impaired functional outcome (See Additional files 5, 6: Table S5, S6 for detailed information). The results showed no publication bias in the included studies on all-cause mortality and impaired functional outcome; however there was a possible risk of publication bias in the studies on stroke recurrence (See Additional file 7: Table S7 for detailed information). We also performed sensitivity analyses on their outcomes to identify the stability of the pooled outcomes of these adverse clinical outcomes (See Additional files 10, 11, 12 Fig. S3, S4 S5 for detailed information).
Discussion
This is the first systematic review and meta-analysis to integrate the association of the TyG index with IS risk in the general population and adverse clinical outcomes in IS patients. We found that there was a positive association between TyG index and increased risk of incident IS and this relationship remained in a stable state even as covariates changed. Meanwhile, TyG index was significantly associated with an increased risk of stroke recurrence and mortality, though not with poor functional outcome and neurologic worsening in stroke patients.
A previous meta-analysis reported an association between TyG index and stroke [18]. This study demonstrated that an increased TyG index was an independent risk factor for stroke; however, this phenomenon was not found in a subgroup analysis for those with hemorrhagic stroke. They also illustrated that TyG index was linearly associated with stroke events only limited to patients with type 2 diabetes or acute coronary syndrome [18]. In contrast, for our study, we only focused on IS in stroke specific studies and those focusing on the general population. Furthermore, we found that the TyG index may be an important predictor of specific clinical adverse outcomes in the setting of IS. The type of study, country of origin, study length, sample size, and definition of the TyG index were also found to have an impact on the association between IS and the TyG index. Thus, lending further data to the current literature as previous studies did not account for these variables.
The TyG index is known as a low-cost and efficient biomarker of insulin resistance (IR) [11], and IR plays an important role in the pathogenesis of IS through various potential mechanisms. IR can interfere with insulin signaling, enhance chronic systemic inflammation, reduce insulin sensitivity, and increase foam cell formation, thereby accelerating the formation of atherosclerosis and advanced plaques [45,46,47,48,49]. IR can also affect the metabolism of insulin-like growth factor-1 (IGF-1), insulin-like growth factor-2 (IGF-2) [50], cyclic guanosine monophosphate (cGMP), and nitric oxide(NO) [51], thus playing key roles in platelet adhesion, activation, and aggregation [52,53,54]. These pathways lead to vascular occlusion and in the pathogenesis of IS [54,55,56]. Furthermore, since IR may affect the cerebrovascular reserve (CVR) through the Baylis effect (myogenic mechanism), chemical, neuronal, and metabolic mechanisms [57,58,59], resulting in impaired cerebral perfusion hemodynamics, this may lead to the hemodynamic disturbances of cerebral perfusion during acute IS [60, 61]. Given these factors, the TyG index reflects the IR level, which can indirectly be used to predict IS.
In both past and present studies, it is well established that elevated IR is a correlative predictor of IS [28,29,30,31,32, 62, 63]. In the general population, the relationship between TyG index and the risk of IS is clear as suggested by our results. However, whether IR can truly guide the clinical outcome of IS patients is controversial. Our analysis showed that TyG index was valuable for predicting recurrent stroke and mortality, but there was no significant correlation found between functional status decline and neurological impairment. Interestingly, previous large prospective studies and meta-analyses supported a significant increase in the risk of stroke recurrence, and all-cause mortality was observed during the 12-month follow-up period, which significantly correlated with IR [22, 64, 65]. Similarly, the interpretation of whether the TyG index can predict poor function or neurological deficits need to be carefully interpreted and studied as well. For example, both Yimo Zhou [22] and Ki-Woong Nam [38] reported that TyG index can predict neurologic worsening, however the combined data was incongruent with this conclusion. This is likely due to unaccounted for heterogeneity. Notably, the severity of functional and neurological deficits of IS affected by many factors, such as robust secondary prevention methods, the presence of CYP2C19 polymorphisms, adequate rehabilitation strategies, excellent family support, the severity of IS itself, and type of emergency treatment approaches [66,67,68,69,70,71,72,73,74,75]. In our meta-analysis, we analyzed the source of heterogeneity via meta-regression analyses, and discovered that variables including country, study design, TyG index conditions, sample size, and follow-up time may each be responsible for the source of heterogeneity. In the future, more accurate TyG measurement methods, cross-validated research designs, larger sample sizes, and multicenter studies are required to further analyze and resolve this conclusion.
Our study had several advantages: First, we divided the study into two types of samples: the general population and the stroke population, which is of great significance for the guidance and application of the TyG index in clinical practice. Second, the association between TyG index and stroke or stroke outcomes was not affected by any single inclusion factor or participant selection according to our sensitivity analysis and subgroup analysis. All of these facets lent evidence to the stability and credibility of our conclusions. Although we conducted study selection, data extraction and quality assessment in strict accordance with established standards, the present study had several limitations. To begin with, most of the literature data are from Asian countries, such as China, South Korea and Singapore, and only one study is from Europe. Although the European research conclusion is consistent with ours, it is questionable whether these results would remain congruent across other countries, regions, and ethnic groups. Additionally, the calculation of TyG index depends on triglyceride and glucose levels which are measured in a non-standardized approach at different institutions. Therefore, measurement errors caused by different detection conditions and levels cannot be fully excluded from the analysis, which may weaken the reliability of the results in our meta-analysis. Last but not least, in the calculation of publication bias, there is a possible inconsistency between the Begg's test and the Egger's test. Although we used different methods to recalculate, it still suggests that the results of the two are different, which means that there is still potential publication bias.
Conclusion and future directions
In conclusion, our meta-analysis reveals that TyG index has potential value in optimizing risk stratification for IS in the general population. Furthermore, there is a significant association between TyG index and major adverse outcomes of strokes. A higher TyG index confers a higher risk of stroke recurrence and risk of death. Notably, no association was found in the effect size combination of poor functional outcomes or neurological worsening. Finally, our subgroup analysis observed that variables such as country, type of stroke, participant, and sample size all contributed an impact to the heterogeneity of the results. Our results suggest that attention should be paid to TyG index screening in the management of stroke patients in the future. Early detection of stroke risk and potential clinical adverse outcomes can delay disease progression and reduce social and economic burdens. TyG index detection is convenient and affordable, however there are relatively few studies on TyG index specifically in relation to IR index and stroke currently. As such, more prospective cohort studies with large sample sizes and multicenter trials using TyG index as a predictor should be carried out to advance our clinical management and utilization of this biomarker in stroke patients. Furthermore, well-designed basic science studies are needed to explore the underlying mechanisms and relationship of TyG index and stroke pathophysiology and sequelae.
Availability of data and materials
Not applicable.
Abbreviations
- AF:
-
Atrial fibrillation
- AHRQ:
-
The agency for healthcare research and quality
- CI:
-
Confidence intervals
- cGMP:
-
Cyclic guanosine monophosphate
- CT:
-
Computed tomography
- CVD:
-
Cardiovascular disease
- CVR:
-
The cerebrovascular reserve
- ES:
-
Effect size
- HS:
-
Hemorrhagic strokes
- HIEC:
-
Hyperinsulinemic-euglycemic clamp
- IGF-1:
-
Insulin-like growth factor-1
- IGF-2:
-
Insulin-like growth factor-2
- IR:
-
Insulin resistance
- IS:
-
Ischemic stroke
- MetS:
-
Metabolic syndrome
- MRI:
-
Magnetic resonance imaging
- NO:
-
Nitric oxide
- NOS:
-
Newcastle–Ottawa quality assessment scale
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PVC:
-
Premature ventricular complexes
- TyG:
-
Triglyceride and glucose
References
Loh HC, Lim R, Lee KW, Ooi CY, Chuan DR, Looi I, et al. Effects of vitamin E on stroke: a systematic review with meta-analysis and trial sequential analysis. Stroke Vasc Neurol. 2021;6:109–20. https://doi.org/10.1136/svn-2020-000519.
Campbell BCV, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nat Rev Dis Primers. 2019;5:70. https://doi.org/10.1038/s41572-019-0118-8.
Ekker MS, Boot EM, Singhal AB, Tan KS, Debette S, Tuladhar AM, et al. Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol. 2018;17:790–801. https://doi.org/10.1016/s1474-4422(18)30233-3.
Hu X, Zan X, Xie Z, Li Y, Lin S, Li H, et al. Association between plasminogen activator inhibitor-1 genetic polymorphisms and stroke susceptibility. Mol Neurobiol. 2017;54:328–41. https://doi.org/10.1007/s12035-015-9549-8.
Zhang W, Zhou F, Huang H, Mao Y, Ye D. Biomarker of dietary linoleic acid and risk for stroke: a systematic review and meta-analysis. Nutrition. 2020. https://doi.org/10.1016/j.nut.2020.110953.
Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol. 2009;8:1006–18. https://doi.org/10.1016/s1474-4422(09)70236-4.
Hankey GJ. Secondary stroke prevention. Lancet Neurol. 2014;13:178–94. https://doi.org/10.1016/s1474-4422(13)70255-2.
Kauw F, Takx RAP, de Jong H, Velthuis BK, Kappelle LJ, Dankbaar JW. Clinical and imaging predictors of recurrent ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. 2018;45:279–87. https://doi.org/10.1159/000490422.
Rujirachun P, Wattanachayakul P, Phichitnitikorn P, Charoenngam N, Kewcharoen J, Winijkul A. Association of premature ventricular complexes and risk of ischemic stroke: a systematic review and meta-analysis. Clin Cardiol. 2021;44:151–9. https://doi.org/10.1002/clc.23531.
Jiao Y, Su Y, Shen J, Hou X, Li Y, Wang J, et al. Evaluation of the long-term prognostic ability of triglyceride-glucose index for elderly acute coronary syndrome patients: a cohort study. Cardiovasc Diabetol. 2022;21:3. https://doi.org/10.1186/s12933-021-01443-y.
Sánchez-García A, Rodríguez-Gutiérrez R, Mancillas-Adame L, González-Nava V, Díaz González-Colmenero A, Solis RC, et al. Diagnostic accuracy of the triglyceride and glucose index for insulin resistance: a systematic review. Int J Endocrinol. 2020;2020:4678526. https://doi.org/10.1155/2020/4678526.
Tian X, Zuo Y, Chen S, Liu Q, Tao B, Wu S, et al. Triglyceride-glucose index is associated with the risk of myocardial infarction: an 11-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2021;20:19. https://doi.org/10.1186/s12933-020-01210-5.
Wu S, Xu L, Wu M, Chen S, Wang Y, Tian Y. Association between triglyceride-glucose index and risk of arterial stiffness: a cohort study. Cardiovasc Diabetol. 2021;20:146. https://doi.org/10.1186/s12933-021-01342-2.
Lin HY, Zhang XJ, Liu YM, Geng LY, Guan LY, Li XH. Comparison of the triglyceride glucose index and blood leukocyte indices as predictors of metabolic syndrome in healthy Chinese population. Sci Rep. 2021;11:10036. https://doi.org/10.1038/s41598-021-89494-9.
da Silva A, Caldas APS, Hermsdorff HHM, Bersch-Ferreira ÂC, Torreglosa CR, Weber B, et al. Triglyceride-glucose index is associated with symptomatic coronary artery disease in patients in secondary care. Cardiovasc Diabetol. 2019;18:89. https://doi.org/10.1186/s12933-019-0893-2.
Cui H, Liu Q, Wu Y, Cao L. Cumulative triglyceride-glucose index is a risk for CVD: a prospective cohort study. Cardiovasc Diabetol. 2022;21:22. https://doi.org/10.1186/s12933-022-01456-1.
Tian X, Zuo Y, Chen S, Meng X, Chen P, Wang Y, et al. Distinct triglyceride-glucose trajectories are associated with different risks of incident cardiovascular disease in normal-weight adults. Am Heart J. 2022;248:63–71. https://doi.org/10.1016/j.ahj.2022.02.014.
Feng X, Yao Y, Wu L, Cheng C, Tang Q, Xu S. Triglyceride-glucose index and the risk of stroke: a systematic review and dose-response meta-analysis. Horm Metab Res. 2022;54:175–86. https://doi.org/10.1055/a-1766-0202.
Wang X, Feng B, Huang Z, Cai Z, Yu X, Chen Z, et al. Relationship of cumulative exposure to the triglyceride-glucose index with ischemic stroke: a 9-year prospective study in the Kailuan cohort. Cardiovasc Diabetol. 2022;21:66. https://doi.org/10.1186/s12933-022-01510-y.
Huang Z, Ding X, Yue Q, Wang X, Chen Z, Cai Z, et al. Triglyceride-glucose index trajectory and stroke incidence in patients with hypertension: a prospective cohort study. Cardiovasc Diabetol. 2022;21:141. https://doi.org/10.1186/s12933-022-01577-7.
Zhao Q, Zhang TY, Cheng YJ, Ma Y, Xu YK, Yang JQ, et al. Triglyceride-glucose index as a surrogate marker of insulin resistance for predicting cardiovascular outcomes in nondiabetic patients with non-st-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention. J Atheroscler Thromb. 2021;28:1175–94. https://doi.org/10.5551/jat.59840.
Zhou Y, Pan Y, Yan H, Wang Y, Li Z, Zhao X, et al. Triglyceride glucose index and prognosis of patients with ischemic stroke. Front Neurol. 2020;11:456. https://doi.org/10.3389/fneur.2020.00456.
Lin SF, Hu HH, Chao HL, Ho BL, Chen CH, Chan L, et al. Triglyceride-glucose index and intravenous thrombolysis outcomes for acute ischemic stroke: a multicenter prospective-cohort study. Front Neurol. 2022;13:737441. https://doi.org/10.3389/fneur.2022.737441.
Matthew JP, Joanne EM, Patrick MB, Isabelle B, Tammy CH, Cynthia DM, The P, et al. statement an updated guideline for reporting systematic reviews. BMJ. 2020. https://doi.org/10.1136/bmj.n71.
Zhou F, Zhou J, Wang W, Zhang XJ, Ji YX, Zhang P, et al. Unexpected rapid increase in the burden of NAFLD in China from 2008 to 2018: a systematic review and meta-analysis. Hepatology. 2019;70:1119–33. https://doi.org/10.1002/hep.30702.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63. https://doi.org/10.1111/j.0006-341x.2000.00455.x.
Lee M, Kim C-h, Kim Y, Jang MU, Lim J-s, Yu K-h, et al. The effects of triglyceride-glucose (TyG) Index on leptomeningeal collateral status and outcome of reperfusion therapy in patients with acute ischemic stroke. Basel: Karger allschwilerstrasse; 2020.
Du Z, Xing L, Lin M, Sun Y. Estimate of prevalent ischemic stroke from triglyceride glucose-body mass index in the general population. BMC Cardiovasc Disord. 2020;20:483. https://doi.org/10.1186/s12872-020-01768-8.
Shi W, Xing L, Jing L, Tian Y, Yan H, Sun Q, et al. Value of triglyceride-glucose index for the estimation of ischemic stroke risk: Insights from a general population. Nutr Metab Cardiovasc Dis. 2020;30:245–53. https://doi.org/10.1016/j.numecd.2019.09.015.
Hong S, Han K, Park CY. The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic cardiovascular disease: a population-based study. BMC Med. 2020;18:361. https://doi.org/10.1186/s12916-020-01824-2.
Wang A, Wang G, Liu Q, Zuo Y, Chen S, Tao B, et al. Triglyceride-glucose index and the risk of stroke and its subtypes in the general population: an 11-year follow-up. Cardiovasc Diabetol. 2021;20:46. https://doi.org/10.1186/s12933-021-01238-1.
Zhao Y, Sun H, Zhang W, Xi Y, Shi X, Yang Y, et al. Elevated triglyceride-glucose index predicts risk of incident ischaemic stroke: The Rural Chinese cohort study. Diabetes Metab. 2021;47:101246. https://doi.org/10.1016/j.diabet.2021.101246.
Liu Q, Cui H, Ma Y, Han X, Cao Z, Wu Y. Triglyceride-glucose index associated with the risk of cardiovascular disease: the Kailuan study. Endocrine. 2022;75:392–9. https://doi.org/10.1007/s12020-021-02862-3.
Hu L, Bao H, Huang X, Zhou W, Wang T, Zhu L, et al. Relationship between the triglyceride glucose index and the risk of first stroke in elderly hypertensive patients. Int J Gen Med. 2022;15:1271–9. https://doi.org/10.2147/ijgm.S350474.
Si S, Li J, Li Y, Li W, Chen X, Yuan T, et al. Causal effect of the triglyceride-glucose index and the joint exposure of higher glucose and triglyceride with extensive cardio-cerebrovascular metabolic outcomes in the UK Biobank: a mendelian randomization study. Front Cardiovasc Med. 2020;7:583473. https://doi.org/10.3389/fcvm.2020.583473.
Zhang B, Liu L, Ruan H, Zhu Q, Yu D, Yang Y, et al. Triglyceride-glucose index linked to hospital mortality in critically Ill stroke an observational multicentre study on eICU database. Front Med. 2020;7:591036. https://doi.org/10.3389/fmed.2020.591036.
Lee M, Kim CH, Kim Y, Jang MU, Mo HJ, Lee SH, et al. High Triglyceride glucose index is associated with poor outcomes in ischemic stroke patients after reperfusion therapy. Cerebrovasc Dis. 2021;50:691–9. https://doi.org/10.1159/000516950.
Nam KW, Kang MK, Jeong HY, Kim TJ, Lee EJ, Bae J, et al. Triglyceride-glucose index is associated with early neurological deterioration in single subcortical infarction: early prognosis in single subcortical infarctions. Int J Stroke. 2021;16:944–52. https://doi.org/10.1177/1747493020984069.
Hou Z, Pan Y, Yang Y, Yang X, Xiang X, Wang Y, et al. An Analysis of the potential relationship of triglyceride glucose and body mass index with stroke prognosis. Front Neurol. 2021;12:630140. https://doi.org/10.3389/fneur.2021.630140.
Nam KW, Kwon HM, Lee YS. High triglyceride-glucose index is associated with early recurrent ischemic lesion in acute ischemic stroke. Sci Rep. 2021;11:15335. https://doi.org/10.1038/s41598-021-94631-5.
Yang X, Wang G, Jing J, Wang A, Zhang X, Jia Q, et al. Association of triglyceride-glucose index and stroke recurrence among nondiabetic patients with acute ischemic stroke. BMC Neurol. 2022;22:79. https://doi.org/10.1186/s12883-022-02588-3.
Toh EMS, Lim AYL, Ming C, Yeo LLL, Sia CH, Tan BWQ, et al. Association of triglyceride-glucose index with clinical outcomes in patients with acute ischemic stroke receiving intravenous thrombolysis. Sci Rep. 2022;12:1596. https://doi.org/10.1038/s41598-022-05467-6.
Wang F, Wang J, Han Y, Shi X, Xu X, Hou C, et al. Triglyceride-glucose index and stroke recurrence in elderly patients with ischemic stroke. Front Endocrinol. 2022;13:1005614. https://doi.org/10.3389/fendo.2022.1005614.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6:299–304. https://doi.org/10.1089/met.2008.0034.
Russell JC, Ahuja SK, Manickavel V, Rajotte RV, Amy RM. Insulin resistance and impaired glucose tolerance in the atherosclerosis-prone LA/N corpulent rat. Arteriosclerosis. 1987;7:620–6. https://doi.org/10.1161/01.atv.7.6.620.
Kitta Y, Nakamura T, Uematsu M, Sugamata W, Deyama J, Fujioka D, et al. Insulin resistance negatively affects long-term outcome in non-diabetic patients with coronary artery disease after therapies to reduce atherosclerotic risk factors. J Cardiol. 2013;62:348–53. https://doi.org/10.1016/j.jjcc.2013.05.006.
Chen W, Wang S, Lv W, Pan Y. Causal associations of insulin resistance with coronary artery disease and ischemic stroke a mendelian randomization analysis. BMJ Open Diabetes Res Care. 2020. https://doi.org/10.1136/bmjdrc-2020-001217.
Bornfeldt KE, Tabas I. Insulin resistance, hyperglycemia, and atherosclerosis. Cell Metab. 2011;14:575–85.
Oh J, Riek AE, Darwech I, Funai K, Shao J, Chin K, et al. Deletion of macrophage vitamin D receptor promotes insulin resistance and monocyte cholesterol transport to accelerate atherosclerosis in mice. Cell Rep. 2015;10:1872–86. https://doi.org/10.1016/j.celrep.2015.02.043.
Moore SF, Williams CM, Brown E, Blair TA, Harper MT, Coward RJ, et al. Loss of the insulin receptor in murine megakaryocytes/platelets causes thrombocytosis and alterations in IGF signalling. Cardiovasc Res. 2015;107:9–19. https://doi.org/10.1093/cvr/cvv132.
Suslova TE, Sitozhevskii AV, Ogurkova ON, Kravchenko ES, Kologrivova IV, Anfinogenova Y, et al. Platelet hemostasis in patients with metabolic syndrome and type 2 diabetes mellitus: cGMP- and NO-dependent mechanisms in the insulin-mediated platelet aggregation. Front Physiol. 2014;5:501. https://doi.org/10.3389/fphys.2014.00501.
Brown E, Ozawa K, Moccetti F, Vinson A, Hodovan J, Nguyen TA, et al. Arterial platelet adhesion in atherosclerosis-prone arteries of obese, insulin-resistant nonhuman primates. J Am Heart Assoc. 2021;10:e019413. https://doi.org/10.1161/jaha.120.019413.
Randriamboavonjy V, Fleming I. Insulin, insulin resistance, and platelet signaling in diabetes. Diabetes Care. 2009;32:528–30.
Guo Y, Zhao J, Zhang Y, Wu L, Yu Z, He D, et al. Triglyceride glucose index influences platelet reactivity in acute ischemic stroke patients. BMC Neurol. 2021;21:409. https://doi.org/10.1186/s12883-021-02443-x.
Li Z, Jiang H, Ding Y, Zhang D, Zhang X, Xue J, et al. Platelet Endothelial aggregation receptor 1 polymorphism is associated with functional outcome in small-artery occlusion stroke patients treated with aspirin. Front Cardiovasc Med. 2021;8:664012. https://doi.org/10.3389/fcvm.2021.664012.
Coenen DM, Heinzmann ACA, Karel MFA, Cosemans J, Koenen RR. The multifaceted contribution of platelets in the emergence and aftermath of acute cardiovascular events. Atherosclerosis. 2021;319:132–41. https://doi.org/10.1016/j.atherosclerosis.2020.12.017.
Banks WA, Rhea EM. The blood-brain barrier, oxidative stress, and insulin resistance. Antioxidants. 2021. https://doi.org/10.3390/antiox10111695.
Chen YC, Inagaki T, Fujii Y, Schwenke DO, Tsuchimochi H, Edgley AJ, et al. Chronic intermittent hypoxia accelerates coronary microcirculatory dysfunction in insulin-resistant Goto-Kakizaki rats. Am J Physiol Regul Integr Comp Physiol. 2016;311:R426–39. https://doi.org/10.1152/ajpregu.00112.2016.
Sacramento JF, Ribeiro MJ, Rodrigues T, Guarino MP, Diogo LN, Seica R, et al. Insulin resistance is associated with tissue-specific regulation of HIF-1alpha and HIF-2alpha during mild chronic intermittent hypoxia. Respir Physiol Neurobiol. 2016;228:30–8. https://doi.org/10.1016/j.resp.2016.03.007.
Fan JL, Nogueira RC, Brassard P, Rickards CA, Page M, Nasr N, et al. Integrative physiological assessment of cerebral hemodynamics and metabolism in acute ischemic stroke. J Cereb Blood Flow Metab. 2022;42:454–70. https://doi.org/10.1177/0271678x211033732.
Bas DF, Ozdemir AO, Colak E, Kebapci N. Higher Insulin resistance level is associated with worse clinical response in acute ischemic stroke patients treated with intravenous thrombolysis. Transl Stroke Res. 2016;7:167–71. https://doi.org/10.1007/s12975-016-0453-y.
Rundek T, Gardener H, Xu Q, Goldberg RB, Wright CB, Boden-Albala B, et al. Insulin resistance and risk of ischemic stroke among nondiabetic individuals from the northern Manhattan study. Arch Neurol. 2010;67:1195–200. https://doi.org/10.1001/archneurol.2010.235.
Howard G, Wagenknecht LE, Kernan WN, Cushman M, Thacker EL, Judd SE, et al. Racial differences in the association of insulin resistance with stroke risk: the REasons for geographic and racial differences in stroke (REGARDS) study. Stroke. 2014;45:2257–62. https://doi.org/10.1161/strokeaha.114.005306.
Pan Y, Jing J, Chen W, Zheng H, Jia Q, Mi D, et al. Post-glucose load measures of insulin resistance and prognosis of nondiabetic patients with ischemic stroke. J Am Heart Assoc. 2017. https://doi.org/10.1161/jaha.116.004990.
Jing J, Pan Y, Zhao X, Zheng H, Jia Q, Mi D, et al. Insulin resistance and prognosis of nondiabetic patients with ischemic stroke: The ACROSS-China study (Abnormal glucose regulation in patients with acute stroke across China). Stroke. 2017;48:887–93. https://doi.org/10.1161/strokeaha.116.015613.
Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2016;47:e98–169. https://doi.org/10.1161/STR.0000000000000098.
Stinear CM, Smith MC, Byblow WD. Prediction tools for stroke rehabilitation. Stroke. 2019;50:3314–22. https://doi.org/10.1161/strokeaha.119.025696.
Gittler M, Davis AM. Guidelines for adult stroke rehabilitation and recovery. JAMA. 2018;319:820–1. https://doi.org/10.1001/jama.2017.22036.
Wang Y, Wang Y, Zhao X, Liu L, Wang D, Wang C, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369:11–9. https://doi.org/10.1056/NEJMoa1215340.
Johnston SC, Easton JD, Farrant M, Barsan W, Conwit RA, Elm JJ, et al. Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med. 2018;379:215–25. https://doi.org/10.1056/NEJMoa1800410.
Johnston SC, Amarenco P, Denison H, Evans SR, Himmelmann A, James S, et al. Ticagrelor and aspirin or aspirin alone in acute ischemic stroke or TIA. N Engl J Med. 2020;383:207–17. https://doi.org/10.1056/NEJMoa1916870.
Wang Y, Meng X, Wang A, Xie X, Pan Y, Johnston SC, et al. Ticagrelor versus clopidogrel in CYP2C19 loss-of-function carriers with stroke or TIA. N Engl J Med. 2021;385:2520–30. https://doi.org/10.1056/NEJMoa2111749.
Toyoda K, Uchiyama S, Yamaguchi T, Easton JD, Kimura K, Hoshino H, et al. Dual antiplatelet therapy using cilostazol for secondary prevention in patients with high-risk ischaemic stroke in Japan: a multicentre, open-label, randomised controlled trial. Lancet Neurol. 2019;18:539–48. https://doi.org/10.1016/s1474-4422(19)30148-6.
González A, Moniche F, Cayuela A, García-Lozano JR, Torrecillas F, Escudero-Martínez I, et al. Effect of CYP2C19 polymorphisms on the platelet response to clopidogrel and influence on the effect of high versus standard dose clopidogrel in carotid artery stenting. Eur J Vasc Endovasc Surg. 2016;51:175–86. https://doi.org/10.1016/j.ejvs.2015.09.020.
Diener H-C, Bogousslavsky J, Brass LM, Cimminiello C, Csiba L, Kaste M, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. The Lancet. 2004;364:331–7. https://doi.org/10.1016/s0140-6736(04)16721-4.
Acknowledgements
We thank Academician Huabei Jiang (Department of Medical Engineering, University of South Florida, Tampa, FL, United States), Dr. Dan Wu and Dr. Yanting Wen (Chongqing University of Posts and Telecommunications) for their advice and assistance throughout our study.
Funding
This study was supported by grants from the Chengdu Science and Technology Bureau, Key Research and Development Support Program, No. 2021-YF09-00046-SN, Empirical research and service efficiency analysis of the health management of geriatric mental disease on computer diagnosis system. This study was also supported by Sichuan Provincial Health Commission Medical Science and Technology Project, No. 2021-21PJ150, Research on the Establishment and Application of Stroke Center Alliance Treatment System in Chengdu Area. This study was also supported by National Key R&D (or Research and Development) Program of China, No. Grant 2020YFC2008606. Noninvasive BCI for people with pathological brain aging and its application validation, NO, STI 2030-Major Projects-2022ZD0208506.
Author information
Authors and Affiliations
Contributions
YW and LC conceived and designed the study. YY, XH, Yuge Wang gathered and analyzed the original studies, extracted the data, and ensured congruence with the inclusion and exclusion criteria. They also wrote the first draft of the manuscript. LL, JX and LF conceived all the figures and tables. JW, YY and BJ participated and guided in the discussion of an overall framework of the article. SJ corrected and validated the manuscript in its entirety. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Does not involve ethical approval and consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Search Strategy
Additional file2: Table S2.
The Newcastle-Ottawa Quality Assessment Scale score for cohort studies.
Additional file 3: Table S3.
The Agency for Healthcare Research and Quality cross-sectional study evaluation criteria.
Additional file 4: Table S4.
Table S4. Univariate meta-regression analysis for the TyG index association with ischemic stroke risk.
Additional file 5: Table S5.
Subgroup analysis for the association of TyG index with prognosis among patients with ischemic stroke.
Additional file 6: Table S6.
Univariate meta-regression analysis for the TyG index association with prognosis among patients with ischemic stroke.
Additional file 7 Table S7.
The publication bias of TyG index with prognosis among patients with ischemic stroke.
Additional file 8: Fig S1.
The publication bias assessment of the TyG index association with ischemic stroke risk.
Additional file 9: Fig S2.
The sensitivity analysis for the TyG index association with ischemic stroke risk.
Additional file 10: Fig S3.
Sensitivity analysis for the association of TyG index with Mortality among patients with ischemic stroke.
Additional file 11: Fig S4.
Sensitivity analysis for the association of TyG index with Stroke recurrence among patients with ischemic stroke.
Additional file 12: Fig S5.
Sensitivity analysis for the association of TyG index with Poor functional outcome among patients with ischemic stroke.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, Y., Huang, X., Wang, Y. et al. The impact of triglyceride-glucose index on ischemic stroke: a systematic review and meta-analysis. Cardiovasc Diabetol 22, 2 (2023). https://doi.org/10.1186/s12933-022-01732-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-022-01732-0