Abstract
Background
Respiratory diseases contribute to global morbidity and mortality, and temperature is a significant factor. We investigated the association between ambient temperature and emergency department (ED) visits for various respiratory diseases in Seoul, South Korea.
Methods
Using data from the National Emergency Department Information System (2008–2017), we analysed 1,616,644 ED visits for respiratory diseases, categorised according to the Korean Standard Classification of Diseases 7th revision codes (J00-J99). Using a time-stratified case-crossover design and a distributed lag nonlinear model, we investigated the effect of temperature exposure on ED visits for respiratory diseases, calculating the relative risk (RR) for the maximum risk temperature (MaxRT) of both cold and hot extremes compared to the minimum risk temperature (MinRT).
Results
Cold temperatures (MaxRT: -9.0 °C) resulted in a 2.68-fold increase (RR = 2.68, 95% CI = 2.26–3.14) in ED visits for total respiratory diseases, while hot temperatures (MaxRT: 29.4 °C) led to a 1.26-fold increase (RR = 1.26, 95% CI = 1.11–1.42) compared to the MinRT (24.8 °C). Cold temperatures increased the risk of most respiratory diseases, except interstitial lung disease, whereas hot temperatures increased ED visits for acute upper respiratory infections and influenza. Cold temperatures increased ED visits for all age groups, especially those aged 18–64 (RR = 3.54, 95% CI = 2.90–4.33), while hot temperatures significantly affected those < 18 (RR = 1.45, 95% CI = 1.27–1.66). The risk levels were similar in both males and females, regardless of hot and cold temperatures.
Conclusion
Our findings underscore the significant impact of both cold and heat exposure on ED visits for respiratory diseases, with varying intensities and risk profiles across different population groups.
Similar content being viewed by others
Background
Respiratory diseases are a significant global health challenge that contribute to high morbidity and mortality rates worldwide. In 2019, chronic respiratory diseases, such as chronic obstructive pulmonary disease (COPD), asthma, and other respiratory conditions, were the third leading cause of death globally, resulting in 4.0 million deaths and affecting 454.6 million individuals [1, 2]. These diseases also impose a substantial burden on healthcare systems owing to hospitalisations, emergency department visits, and long-term care expenses [3,4,5,6]. Furthermore, respiratory infections, including upper and lower respiratory tract infections, contribute to a substantial global burden, with billions of cases and millions of deaths reported annually [7, 8].
Weather conditions, particularly temperature, significantly contribute to the development of respiratory diseases. Understanding the relationship between temperature and respiratory diseases is crucial, particularly given the increasing frequency and intensity of extreme temperature events caused by climate change [9]. Previous studies have demonstrated that both heat and cold exposure are associated with an increased risk of respiratory symptoms, exacerbation, and hospitalization [10,11,12,13,14,15,16,17,18,19,20,21,22]. However, most of these studies have focused on specific respiratory diseases in relation to either heat or cold exposure, highlighting the need for more comprehensive research examining the impact of both heat and cold on overall respiratory health. Thus, this study aimed to investigate the association between heat and cold exposure and emergency department (ED) visits for respiratory diseases in Seoul, South Korea, using a comprehensive national database. We hypothesised that both cold and heat exposure would affect respiratory diseases, with the intensity of the effects and risk groups varying across different diseases.
Methods
Study design and data extraction
We used data from the National Emergency Department Information System (NEDIS), a comprehensive database established by the National Emergency Medical Center in 2003. The NEDIS contains detailed information on patient demographics, emergency department visits, diagnoses, treatments, and outcomes from approximately 98% of all emergency medical facilities in South Korea. Our study was conducted in accordance with the Declaration of Helsinki and the study protocol was approved by the Institutional Review Board of Soonchunhyang University (202,108-SB-076-01). As the NEDIS database contains de-identified information, informed consent was not required.
Study populations and primary outcome
Our study population consisted of patients who visited the ED in Seoul between 2008 and 2017 with a primary diagnosis of respiratory disease. These diseases were classified based on the Korean Standard Classification of Diseases 7th revision codes J00–J99, a modification of the International Classification of Diseases 10th revision, to suit the specific health system in South Korea. The diseases were further categorised into specific groups: acute upper respiratory infections (AURI) (J00-J06), influenza and pneumonia (J09-J18), acute lower respiratory infection (ALRI) (J20-J22), chronic lower respiratory diseases (CLRD) (J40-J47), COPD (J42-J44 except for J43 alone), asthma (J45), acute respiratory distress syndrome (ARDS) and pulmonary edema (J80, J81), interstitial lung disease (ILD) (J84), and pneumothorax (J93). The primary outcome of interest was all ED visits with respiratory disease codes assigned as the primary diagnosis at discharge.
Exposure assessment
This study focused on assessing the exposure to daily ambient temperature in Seoul, the capital and largest city in South Korea. To estimate this parameter, we collected hourly ambient temperature data from Seoul’s weather monitoring station using the Automated Surface Observing System of the Korea Meteorological Administration. We calculated the 24-hour mean, maximum, and minimum temperatures for each day using hourly data.
Seoul is situated within a temperate zone at 37.57°N and 126.98°E. The city experiences four distinct seasons, characterised by hot summers with an average maximum temperature of 32 °C, allowing for the examination of heat exposure’s effects on respiratory health. Additionally, Seoul’s winters are cold, with an average minimum temperature of -15 °C, making it an ideal setting to study the impact of cold exposure on respiratory diseases. Seoul also experiences a rainy season in July and August, which potentially influences variations in air quality and respiratory conditions during this period. The city’s substantial population and diverse temperature range make it a suitable location for assessing the association between ambient temperature and respiratory diseases.
Statistical analysis
This time-stratified case-crossover study used conditional Poisson regression to investigate the impact of daily mean temperature on ED visits for respiratory diseases. For each patient, corresponding 3 ~ 4 control days were meticulously selected from the same year, month, and day of the week stratum, ensuring a comparable day without an ED visit. This design allowed us to effectively control for slowly varying factors such as sex, genetic predisposition, lifestyle, socioeconomic status, and comorbidities. By comparing the temperatures on case and control days, we aimed to isolate the specific impact of temperature on ED visits.
To assess both cold and hot temperature impacts, we conducted a conditional Poisson regression with a distributed lag nonlinear model (DLNM), which allowed us to construct a flexible temperature structure, capturing the potential nonlinear and lagged effects of exposure. The model was constructed using quadratic B-splines with two internal knots (33.3rd and 63.7th) for exposure-response and natural cubic B-splines with three knots at equal intervals in log-scale for lag-response, guided by the Quasi-Akaike information criteria and previous studies (Additional file 1: Table S1) [23, 24]. Using the DLNM, we obtained the minimum risk temperature (MinRT) and maximum risk temperature (MaxRT), along with the corresponding percentiles (%), providing insights into the temperature range associated with the highest and lowest risks. We calculated the relative risks (RRs) for MaxRT compared to MinRT using a lag structure of up to 21 days for the main temperature effect after adjusting for holidays, influenza epidemic, and 2-day moving averages (lag 0–1) of relative humidity and barometric pressure.
We conducted subgroup analyses based on age (< 18 years, 18–64 years, and ≥ 65 years) and sex (male vs. female). Owing to the rarity of COPD and ILD in individuals under 18 years of age, a subanalysis for this age group was not conducted. To enhance our findings’ robustness, we performed four sensitivity analyses: (1) using the minimum and maximum temperature, (2) exploring different lag periods (0–7, 0–14, and 0–28 days), (3) adjusting for ambient pollutants, such as particulate matter 10 and 2.5 micrometers or less in diameter, nitrogen dioxide, ozone, sulfur dioxide, and carbon monoxide, and (4) exploring various model specifications for the exposure-response relationship, including different combinations of internal knots and changing the spline function from quadratic to cubic [25]. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC) and R version 3.5.3 (R Core Team, 2019).
Results
Baseline characteristics
Between 2008 and 2017, 1,616,644 ED visits for respiratory diseases were recorded in Seoul, South Korea (Table 1). The average number of daily ED visits for respiratory diseases was 442.6, with AURI (253.5) being the most common diagnosis, followed by influenza and pneumonia (100.4), ALRI (28.4), and CLRD (27.4). Seoul’s average temperature during this period was 12.9 °C, with temperatures extremes ranging from − 18.0 to 36.4 °C.
The association between mean temperature and risk of ED
In our analysis, the MinRT for total respiratory diseases was 24.8 °C, corresponding to the 85.5th percentile (%). Similar MinRT values were observed for AURI (24.3 °C, 82.5%), influenza (25.0 °C, 86.5%), and ILD (26.4 °C, 92.4%) (Table 2). All other disease categories also reported MinRT values at or above the 80%, except for pneumothorax, which had a MinRT of 14.0 °C (48.8%).
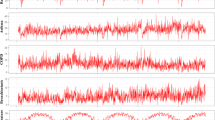
In the cold temperatures, we observed a significant 2.68-fold increase in ED visits (95% CI = 2.26–3.14) for all respiratory diseases at a MaxRT of -9.0 °C (Figs. 1 and 2). This MaxRT was consistently associated with increased ED visit risk for AURI (RR = 1.68, 95% CI = 1.68–2.39), influenza and pneumonia (RR = 11.23, 95% CI = 8.83–14.28), and COPD (RR = 1.54, 95% CI = 1.11–2.13). ARDS and pulmonary oedema (RR = 1.86, 95% CI = 1.00-3.45) and pneumothorax (RR = 1.18, 95% CI = 1.00-1.39) showed similar trends with MaxRTs of -7.9 °C and − 5.2 °C, respectively. Meanwhile, ALRI (RR = 2.01, 95% CI = 1.72–2.35), CLRD (RR = 1.53, 95% CI = 1.29–1.80), and asthma (RR = 1.88, 95% CI = 1.49–2.37) were significantly linked to ED visits at colder temperatures, specifically when MaxRT was above 10.0 °C.
Overall cumulative associations between mean ambient temperature and emergency department visits for subtypes of respiratory diseases over 0–21 lag days. Dotted vertical lines indicate MinRT, while the solid line with shaded areas represents the relative risk with 95% confidence intervals. ED, emergency department; MinRT, minimum risk temperature; AURI, acute upper respiratory infection; ALRI, acute lower respiratory infection; CLRD, chronic lower respiratory disease; COPD, chronic obstructive pulmonary disease; ARDS, acute respiratory distress syndrome; ILD, interstitial lung disease
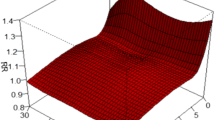
Three-dimensional curves for the RRs of emergency department visits for total respiratory diseases with mean ambient temperature over 0–21 lag days. The x-axis represents the mean ambient temperature, y-axis represents the lag days, and z-axis represents the relative risk of emergency department visits. Each curve represents a different dataset. The height and colour of the curves indicate the level of risk, with higher and darker curves representing a higher risk. RRs, relative risks
Hot temperatures (MaxRT: 29.4 °C) were significantly associated with a 1.26-fold increase (95% CI = 1.11–1.42) in ED visits for total respiratory diseases. Similar trends were observed for AURI (RR = 1.23, 95% CI = 1.08–1.40) and influenza and pneumonia (RR = 11.23, 95% CI = 8.83–14.28). However, no significant associations were observed between hot temperatures and other respiratory diseases.
Subgroup analysis stratified by age
In the age-stratified subgroup analysis, cold temperatures (MaxRT: -9.0 °C) were associated with increased ED visits for total respiratory diseases across all age groups, with the highest RR observed in the 18–64 age group (RR = 3.54, 95% CI = 2.90–4.33) compared to those aged < 18 years (RR = 2.34, 95% CI = 1.95–2.80) and ≥ 65 years (RR = 2.07, 95% CI = 1.71–2.49) (Table 3; Fig. 3). Cold temperatures were significantly associated with increased ED visits for AURI, influenza, and ALRI in all age groups. Cold temperatures were significantly associated with CLRD, asthma, and ARDS and pulmonary oedema in the group aged 18–64 and ≥ 65 years. For individuals aged ≥ 65 years, significant associations were observed between cold temperature and COPD and pneumothorax.
Overall cumulative associations between mean ambient temperature and emergency department visits for total respiratory diseases, stratified by age. (a) individuals under 18 years of age, (b) individuals between 18 and 64 years of age, (c) individuals aged 65 years and above. Dotted vertical lines indicate MinRT, while the solid line with shaded areas represents the relative risk with 95% confidence intervals. ED, emergency department; MinRT, minimum risk temperature
Hot temperatures significantly increased ED visits for total respiratory diseases in individuals < 18 years (RR = 1.45, 95% CI = 1.27–1.66) (Table 3). This association extended to all sub-respiratory diseases, except pneumothorax, which showed a significant association in patients aged ≥ 65 years. The MaxRT values for these associations, ranging from 27.9 to 29.4 °C, fell within the 96.7 to 99.0% range.
Subgroup analysis stratified by sex
In the subgroup analysis stratified by sex, both males and females demonstrated an increased RR for total respiratory disease ED visits at colder temperatures (MaxRT: − 9 °C, 1.0%), with RRs of 2.29 (95% CI = 1.95–2.70) and 3.19 (95% CI = 2.66–3.83), respectively (Table 4; Fig. 4). Similar patterns were observed for AURI, influenza, ALRI, and CLRD. However, for COPD, ARDS and pulmonary oedema, and pneumothorax, males had a higher risk at lower temperatures, whereas females had a higher risk for asthma at colder temperatures.
Overall cumulative associations between mean ambient temperature and emergency department visits for total respiratory diseases, stratified by age and sex. (a) males, and (b) females. Dotted vertical lines indicate MinRT, while the solid line with shaded areas represents the relative risk with 95% confidence intervals. ED, emergency department; MinRT, minimum risk temperature
Regarding hot temperatures, both sexes showed an increased risk for total respiratory disease ED visits at MaxRT 29.4 °C (99.0%), with males (RR = 1.27, 95% CI = 1.12–1.43) and females (RR = 1.24, 95% CI = 1.08–1.42) having similar risk levels. This trend was also observed for AURI and influenza and pneumonia. However, males exhibited a higher risk for asthma and ARDS and pulmonary oedema at hot temperatures.
Sensitivity analysis
Our sensitivity analysis, which used maximum and minimum temperatures, showed minor variations in RRs, but overall, the results supported our main findings (Additional file 1: Table S2 and Additional file 2: Fig. S1-S2). Specifically, when using maximum temperature, a significant association was found between a MaxRT of 31 °C and increased ED visits for pneumothorax (RR = 1.18, 95% CI = 1.00–1.40). In contrast, during hot weather, ARDS and pulmonary oedema were associated with increased ED visits when analysing minimum temperature (RR = 1.66, 95% CI = 1.03–2.69).
Our analysis examined the risk ratios for ED visits at various lag periods (7-day, 14-day, and 28-day) under both cold and hot conditions (Additional file 1: Table S3 and Additional file 2: Fig. S3-S5). Both heat and cold exposure demonstrated stronger effects with longer lags. Additionally, we observed that hot temperatures showed similar effects at both shorter and longer lags, whereas cold temperatures exhibited a stronger effect at longer lags compared to shorter lags. Sensitivity analyses, which included modifications to the DLNM model (Additional file 1: Table S4) and consideration of air pollution (Additional file 2: Fig. S6-S11), were consistent with our main findings.
Discussion
This is the first comprehensive analysis of the association between ambient temperature and ED visits for various respiratory diseases in Seoul, South Korea. We found that both cold and hot temperatures significantly affected the frequency of ED visits for respiratory diseases, with the intensity of the effect varying across diseases and demographic groups. Cold temperatures were associated with an increased risk of ED visits for respiratory diseases overall, whereas hot temperatures were significantly associated with increased ED visits for AURI, influenza, and pneumonia. Cold weather increased ED visits for all ages, most in 18–64 group; hot weather mainly affected those under 18.
Our findings of increased ED visits for several respiratory diseases during colder temperatures are consistent with prior studies [11, 13, 15,16,17,18]. Chen et al. revealed that in Beijing, from 2012 to 2015, extreme cold (-6.5 °C) was associated with increased asthma hospitalisations (Cumulative RR = 2.3, 95% CI = 1.57–3.42) compared to the reference temperature (22 °C) [13]. Tseng et al. found that a 5 °C decrease in mean temperature over 28 days increased the long-term risk of COPD exacerbation (odds ratio [OR] = 1.106, 95% CI = 1.063–1.152) in Taiwan [15]. Similarly, a Chinese study demonstrated that both moderate (3 °C, OR = 1.68, 95% CI = 1.18–2.39) and extreme (-7 °C, OR = 1.73, 95% CI–1.13-2.67) cold temperatures were associated with a significant increase in the risk of asthma exacerbation [16]. The increased incidence of acute exacerbations of airway diseases during the cold season can be attributed to several factors. Breathing cold air tends to heighten bronchial reactivity, making the airways more sensitive and prone to inflammation and constriction [26]. Moreover, cold temperatures, particularly during the winter, are associated with an increase in respiratory infections, including pneumonia [17, 18, 27, 28]. Impairment of mucociliary clearance function at cold temperatures facilitates the onset of these infections [29, 30]. A study in Hong Kong revealed that temperature-related pneumonia hospitalisations accounted for 10.7% of cases, with 8.7% attributed to cold temperatures and 2.0% to hot temperatures [17]. Furthermore, low air temperatures are correlated with an increased incidence of influenza [28]. Our study corroborates these findings and highlights the significant role of cold temperatures in exacerbating respiratory diseases.
Our findings showed variations in MaxRT during the cold season for different respiratory diseases. Specifically, AURI, influenza, and COPD peaked at -9.0 °C, while asthma and ALRI showed increased ED visits at temperatures above 10 °C. The association between AURI and cold air temperatures may be due to the chilling effect on the nasal and upper respiratory tracts, which can worsen symptoms by impairing respiratory defences [27]. Consequently, the subzero MaxRT for AURI, a major trigger for COPD exacerbation, may explain the increased ED visits, especially among patients with COPD [31]. Interestingly, the peak temperatures for asthma and ALRI in our study were aligned with the average temperatures during the spring and autumn transitional seasons in South Korea. This finding was consistent with the study by Sohn et al., which demonstrated that each 1 °C increase in temperature above 6 °C, up to 14 °C, was associated with an additional risk of pneumonia of 1.89 (95% CI, 1.37–2.61) [19]. This suggested that significant daily temperature fluctuations during these seasons could potentially trigger the onset of symptoms associated with these diseases [32, 33]. This is further supported by a study by Kim et al., which revealed that a 1-unit increase in day-to-day temperature change led to a 3.5% increase in asthma-related ED visits, particularly in the fall and spring [20].
Conversely, our study identified a MinRT of 14 °C for pneumothorax, with a peak at -5.2 °C. The increase in pneumothorax cases during cold weather could be associated with swift alterations in temperature, atmospheric pressure, or humidity [34, 35], which might induce a rupture, culminating in pneumothorax. However, the exact relationship between temperature and the risk of pneumothorax requires further investigation.
We observed a significant increase in ED visits for respiratory diseases among individuals aged < 18 years, particularly during extremely hot temperatures. The vulnerability of different age groups to the effects of high temperatures on respiratory diseases remains debatable [10, 12,13,14, 21, 22]. Elderly individuals are often considered more susceptible because of physiological factors, pre-existing health conditions, and economic constraints [36]. This viewpoint is supported by the findings of a Brazilian cohort study on COPD and asthma hospitalizations [21, 22]. However, these studies have reported conflicting findings. A case crossover study conducted from 2007 to 2018 in England found that summer temperature increases significantly escalated asthma-related hospital admissions in individuals aged 16–64 years, but not in those under 16 or over 65 [10]. Similarly, the age group 65–74 showed the most pronounced increase in COPD hospital admissions due to heat effects compared to other age groups [12]. However, heat exposure may be more impactful in younger populations as they tend to be more active outdoors at higher temperatures. A study conducted in the USA reported that extreme summer heat events increased asthma hospitalisations the most among youths and adults, while extreme precipitation events affected those aged 4 years or younger the most [14]. Similarly, a Chinese study demonstrated that the risk of asthma hospitalisation due to hot temperatures was higher in younger individuals (19–64 years old) than in those aged > 65 years [13]. A recent meta-analysis revealed that cold temperatures were associated with asthma exacerbations in children (< 19 years) and the elderly (≥ 65 years) but not in adults (16–64 years), while hot temperatures were associated with increased asthma exacerbations in all age groups, with the highest risk in adults [37]. Geographical, climatic, and population variations may explain these discrepancies. In addition, our study focused on ED visits rather than total hospital admissions, accounting for various influencing factors such as healthcare facility availability and accessibility and individual health-seeking behaviours.
This study had several limitations. First, ambient temperature was used as a proxy for personal exposure, which may not perfectly represent individual exposure levels. Although exposure measurement errors may have led to an underestimation of the results, the findings remain noteworthy. Second, the study relied on ED visits as the primary outcome, which may not have captured all instances of respiratory disease exacerbation. However, ED visits are critical indicators of severe disease exacerbation and remain in this context. Third, the study was conducted in Seoul, South Korea; therefore, the findings may not be generalisable to other regions with different climates, health behaviours, and healthcare systems. Finally, the study did not account for potential confounding factors such as indoor air quality, individual health behaviours, and pre-existing health conditions. Nevertheless, the case-crossover design inherently controlled for individual characteristics that did not vary over a brief period. Despite these limitations, our study stands out due to its extensive dataset, unique focus on MaxRT for various respiratory diseases, advanced statistical methods, and significant public health implications.
Conclusion
In conclusion, our study highlights the significant influence of ambient temperature on the frequency of ED visits for various respiratory diseases. This underscores the importance of considering weather patterns in developing public health strategies for managing respiratory diseases.
Data availability
The data supporting this study’s findings are available from the corresponding author upon reasonable request.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- CI:
-
Confidence interval
- ALRI:
-
Acute lower respiratory infection
- CLRD:
-
Chronic lower respiratory disease
- ED:
-
Emergency department
- AURI:
-
Acute upper respiratory infection
- ILD:
-
Interstitial lung disease
- RR:
-
Relative risk
- DLNM:
-
Distributed lag nonlinear model
- MaxRT:
-
Maximum risk temperature
- MinRT:
-
Minimum risk temperature
- NEDIS:
-
National emergency department information system
References
Global burden. Of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396:10258.
Prevalence and attributable health burden of chronic respiratory diseases. 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet Respir Med. 2020;8:6.
Duan KI, Birger M, Au DH, Spece LJ, Feemster LC, Dieleman JL. Health Care spending on respiratory diseases in the United States, 1996–2016. Am J Respir Crit Care Med. 2022;207:2.
Wang Y, Ghoshal AG, Bin Abdul Muttalif AR, Lin HC, Thanaviratananich S, Bagga S et al. Quality of Life and Economic Burden of Respiratory Disease in Asia-Pacific-Asia-Pacific Burden of Respiratory diseases Study. Value Health Reg Issues 2016;9.
Tabyshova A, Emilov B, Postma MJ, Chavannes NH, Sooronbaev T, van Boven JFM. Prevalence and economic Burden of Respiratory diseases in Central Asia and Russia: a systematic review. Int J Environ Res Public Health. 2020;17:20.
Wong AW, Koo J, Ryerson CJ, Sadatsafavi M, Chen W. A systematic review on the economic burden of interstitial lung disease and the cost-effectiveness of current therapies. BMC Pulm Med. 2022;22:1.
Estimates of the. Global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Infect Dis. 2018;18:11.
Jin X, Ren J, Li R, Gao Y, Zhang H, Li J et al. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. EClinicalMedicine 2021;37.
Parmesan C, Morecroft MD, Trisurat Y. Climate change 2022: impacts, adaptation and vulnerability. GIEC; 2022.
Konstantinoudis G, Minelli C, Lam HCY, Fuertes E, Ballester J, Davies B et al. Asthma hospitalisations and heat exposure in England: a case-crossover study during 2002–2019. Thorax 2023.
Zhang Y, Liu X, Kong D, Fu J, Liu Y, Zhao Y et al. Effects of ambient temperature on Acute exacerbations of Chronic Obstructive Pulmonary Disease: results from a time-series analysis of 143318 hospitalizations. Int J Chron Obstruct Pulmon Dis 2020;15.
Konstantinoudis G, Minelli C, Vicedo-Cabrera AM, Ballester J, Gasparrini A, Blangiardo M. Ambient heat exposure and COPD hospitalisations in England: a nationwide case-crossover study during 2007–2018. Thorax. 2022;77:11.
Chen Y, Kong D, Fu J, Zhang Y, Zhao Y, Liu Y, et al. Associations between ambient temperature and adult asthma hospitalizations in Beijing, China: a time-stratified case-crossover study. Respir Res. 2022;23:1.
Soneja S, Jiang C, Fisher J, Upperman CR, Mitchell C, Sapkota A. Exposure to extreme heat and precipitation events associated with increased risk of hospitalization for asthma in Maryland, U.S.A. Environ Health 2016;15.
Tseng C-MJ, Chen Y-T, Ou S-M, Hsiao Y-H, Li S-Y, Wang S-J et al. The Effect of Cold temperature on increased exacerbation of Chronic Obstructive Pulmonary Disease: a Nationwide Study. PLoS ONE 2013;8.
Zhu Y, Yang T, Huang S, Li H, Lei J, Xue X et al. Cold temperature and sudden temperature drop as novel risk factors of asthma exacerbation: a longitudinal study in 18 Chinese cities. Sci Total Environ 2022;814.
Qiu H, Sun S, Tang R, Chan KP, Tian L. Pneumonia hospitalization risk in the Elderly Attributable to Cold and Hot temperatures in Hong Kong, China. Am J Epidemiol. 2016;184:8.
Liu Y, Kan H, Xu J, Rogers D, Peng L, Ye X, et al. Temporal relationship between hospital admissions for pneumonia and weather conditions in Shanghai, China: a time-series analysis. BMJ Open. 2014;4:7.
Sohn S, Cho W, Kim JA, Altaluoni A, Hong K, Chun BC. Pneumonia Weather’: short-term effects of Meteorological factors on emergency room visits due to Pneumonia in Seoul, Korea. J Prev Med Public Health. 2019;52:2.
Kim J, Lim Y, Kim H. Outdoor temperature changes and emergency department visits for asthma in Seoul, Korea: a time-series study. Environ Res 2014;135.
Zhao Q, Li S, Coelho M, Saldiva PHN, Xu R, Huxley RR, et al. Ambient heat and hospitalisation for COPD in Brazil: a nationwide case-crossover study. Thorax. 2019;74:11.
Wu Y, Xu R, Wen B, Coelho M, Saldiva PH, Li S, et al. Temperature variability and asthma hospitalisation in Brazil, 2000–2015: a nationwide case-crossover study. Thorax. 2021;76:10.
Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Stat Med. 2010;29:21.
Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. The Lancet. 2015;386:9991.
Lee H, Myung W, Kim H, Lee EM, Kim H. Association between ambient temperature and injury by intentions and mechanisms: a case-crossover design with a distributed lag nonlinear model. Sci Total Environ 2020;746.
Ahmed T, Danta I. Effect of cold air exposure and exercise on nonspecific bronchial reactivity. Chest. 1988;93:6.
Eccles R, Wilkinson JE. Exposure to cold and acute upper respiratory tract infection. Rhinology. 2015;53:2.
Luan GJ, Zhou MG. [Correlation between low air temperature and influenza incidence in winter in China, 2004–2016]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:3.
Mercke U. The influence of varying air humidity on mucociliary activity. Acta Otolaryngol. 1975;79:1–2.
Mäkinen TM, Juvonen R, Jokelainen J, Harju TH, Peitso A, Bloigu A, et al. Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respir Med. 2009;103:3.
Ko FW-s, Chan KP, Hui DS-c, Goddard JR, Shaw JG, Reid DW et al. Acute exacerbation of COPD. Respirology (Carlton, Vic) : 2016;21.
Qiu H, Yu IT, Tse LA, Chan EY, Wong TW, Tian L. Greater temperature variation within a day associated with increased emergency hospital admissions for asthma. Sci Total Environ 2015;505.
Cong X, Xu X, Zhang Y, Wang Q, Xu L, Huo X. Temperature drop and the risk of asthma: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2017;24:28.
Motono N, Maeda S, Honda R, Tanaka M, Machida Y, Usuda K, et al. Atmospheric temperature and pressure influence the onset of spontaneous pneumothorax. Clin Respir J. 2018;12:2.
Vodička J, Vejvodová Š, Šmíd D, Fichtl J, Špidlen V, Kormunda S, et al. Do Weather Phenomena have any influence on the occurrence of spontaneous pneumothorax? Arch Bronconeumol. 2016;52:5.
Benmarhnia T, Deguen S, Kaufman JS, Smargiassi A. Review article: vulnerability to heat-related mortality: a systematic review, Meta-analysis, and Meta-regression analysis. Epidemiology. 2015;26:6.
Han A, Deng S, Yu J, Zhang Y, Jalaludin B, Huang C. Asthma triggered by extreme temperatures: from epidemiological evidence to biological plausibility. Environ Res 2023;216:Pt 2.
Acknowledgements
Not applicable.
Funding
This study was supported by the Soonchunhyang University Research Fund and the Young Researcher Program through the National Research Foundation of Korea, funded by the Ministry of Science and ICT [grant number NRF-2022R1C1C1010045; H Lee].
Author information
Authors and Affiliations
Contributions
H-Y.Y. was responsible for the conception and design of the study; was responsible for the content of the manuscript, including the data analysis; and performed data acquisition. H.L. performed the statistical analysis and data interpretation. H-Y.Y. and H.L. were responsible for writing the first draft of the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study was conducted in accordance with the Declaration of Helsinki and the study protocol was approved by the Institutional Review Board of Soonchunhyang University (202108-SB-076-01). As the NEDIS database contains de-identified information, informed consent was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1
. Table S1. Quasi-Akaike information criteria (QAIC) values for the association between ambient mean temperature and emergency department visits for respiratory diseases according to various distributed lag nonlinear model specifications; Table S2. Sensitivity analyses employing maximum and minimum temperature as temperature measures; Table S3. Sensitivity analyses altering lag structures for distributed lag nonlinear models; Table S4. Sensitivity analyses altering model specifications of exposure functions in distributed lag nonlinear models for results of total respiratory diseases.
Additional file 2
. Fig. S1. Sensitivity analysis conducted for the association between maximum ambient temperature and emergency department visits for various subtypes of respiratory diseases; Fig. 2. Sensitivity analysis conducted for the association between minimum ambient temperature and emergency department visits for various subtypes of respiratory diseases; Fig. S3. Sensitivity analysis of mean ambient temperature and emergency department visits for various respiratory disease subtypes over 0–7 lag days.; Fig. S4. Sensitivity analysis of mean ambient temperature and emergency department visits for various respiratory disease subtypes over 0–14 lag days; Fig. S5 Sensitivity analysis of mean ambient temperature and emergency department visits for various respiratory disease subtypes over 0–28 lag days; Fig. S6. Sensitivity analysis of the association between mean ambient temperature and emergency department visits for various subtypes of respiratory diseases, adjusted for PM10 concentration; Fig. S7. Sensitivity analysis of the association between mean ambient temperature and emergency department visits for various subtypes of respiratory diseases, adjusted for PM2.5 concentration; Fig. S8. Sensitivity analysis of the association between mean ambient temperature and emergency department visits for various subtypes of respiratory diseases, adjusted for NO2 concentration; Fig. S9. Sensitivity analysis of the association between mean ambient temperature and emergency department visits for various subtypes of respiratory diseases, adjusted for O3 concentration; Fig. S10. Sensitivity analysis of the association between mean ambient temperature and emergency department visits for various subtypes of respiratory diseases, adjusted for SO2 concentration; Fig. S11. Sensitivity analysis of the association between mean ambient temperature and emergency department visits for various subtypes of respiratory diseases, adjusted for CO concentration.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, H., Yoon, HY. Impact of ambient temperature on respiratory disease: a case-crossover study in Seoul. Respir Res 25, 73 (2024). https://doi.org/10.1186/s12931-024-02699-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-024-02699-0