Abstract
Background
There are significant associations between ambient temperature and respiratory disease mortality. However, few studies have assessed the morbidity burdens of various respiratory diseases that are attributable to different temperature ranges in subtropical regions.
Methods
Daily outpatient visits, weather variables, and air pollution data were collected from January 2013 to August 2017 in a hospital in Dongguan city. A standard time series quasi-Poisson regression with a distributed lag non-linear model (DLNM) was applied to estimate the associations between daily mean temperature and morbidity for total respiratory diseases, bronchiectasis, chronic obstructive pulmonary disease (COPD), and asthma. Attributable fractions were then calculated to quantify disease burden relative to different temperature components. Finally, we conducted stratified analysis by age group.
Results
Both low and high temperatures were associated with an increased risk of morbidity secondary to respiratory diseases. Compared with the optimum temperature, the accumulated relative risk (RR) during the seven lag days was 1.13 with a 95% confidence interval (CI) of 1.01–1.26 for extreme heat and 1.02 (95% CI: 0.99–1.05) for extreme cold. Heat-related respiratory morbidity risk was higher than cold-related risk for the total population, but an opposite result was observed for the elderly. About 8.4% (95% CI: 2.8–13.3%) of respiratory morbidity was attributable to non-optimal temperatures, and moderate heat was responsible for most of the excess respiratory morbidity (7.5, 95% CI: 2.4–12.2%).
Conclusions
We found that exposure to non-optimal temperatures increased the risk of respiratory morbidity in subtropical region, and moderate heat contributed to most of the temperature-related respiratory morbidities. This indicates a need for further examination of moderate, rather than extreme, heat in subtropical region.
Similar content being viewed by others
Background
Respiratory diseases, including chronic obstructive pulmonary disease (COPD), asthma, bronchiectasis, pneumonia, etc., have been implicated in more than 354 million deaths worldwide [1]. In recent years, respiratory diseases were responsible for 11% of all deaths in China [2]. Therefore, respiratory diseases are a significant public health problem, both around the world and in China.
The associations between ambient temperatures and human health have been widely studied, and growing evidence has revealed that exposure to ambient temperatures may increase the risks of a range of respiratory diseases, cardiovascular diseases, and other diseases [3,4,5,6,7]. Although most previous studies found significant relationships between ambient temperature and morbidity or mortality [8, 9], few have assessed the disease burden attributable to ambient temperatures [10,11,12,13,14]. Compared with relative risk (RR), disease burden may provide extra public health information by calculating attributable fraction (AF) and absolute excess numbers such as the attributable number (AN). AF and AN can quantify health burden due to specific temperature range exposure for specific diseases [15]. This is critical for planning and evaluating public health interventions and controls.
Also, most previous studies explored the associations between temperature and health outcomes, with a focus on mortality rather than morbidity. There are some limitations in the analysis of associations between climate change or variations and mortality: the actual death time and the reported time may be inconsistent. Moreover, mortality only reflects the most serious health outcomes of ambient temperature exposure. Compared with mortality, morbidity includes a broader range of health events such as outpatient visits, emergency room visits, and hospitalizations, which was more suitable to examine the acute effect of temperature exposure on health. A few studies have evaluated the effect of extreme temperature on morbidity [16,17,18,19]. However, less attention has been paid to the burden of respiratory disease in relationship to different temperature ranges, such as extreme heat, moderate heat, extreme cold and moderate cold.
In the present study, we aimed to examine the associations between ambient temperature and hospital outpatient visits for total respiratory diseases, bronchiectasis, COPD, and asthma in Dongguan City, China. We further quantified the morbidity burdens attributable to different temperature ranges by computing AF and AN. The findings from our study may help to provide a better understanding of ambient temperature exposure on respiratory morbidity burden.
Methods
Data
Hospital outpatient visits data
Dongguan, located in south China, is a subtropical city. Daily data on hospital outpatient visits for respiratory illness between January 2013 and August 2017 were collected from the computerized database of the Dongguan Fifth People’s Hospital, located in southwest Dongguan City. The hospital is one of the premier hospitals in Dongguan. Most patients in this study were local residents because of medical insurance policy restrictions and convenience. The specific causes of hospital outpatient visits were coded according to the tenth revision of the International Classification of Diseases (ICD-10) and included total respiratory diseases (J00–J99), bronchiectasis (J47), COPD (J40–J44), and asthma (J45–J46).
Meteorological and air pollution data
Daily meteorological data were collected from 2013 to 2017 from the China National Weather Data Sharing System (http://cdc.cma.gov.cn/home.do), including daily mean temperature and relative humidity. Weather data were gathered by a fixed-site station located at the center of Dongguan City.
To adjust for the effect of potential confounding variables, we obtained daily concentrations of air pollutants including Particulate matter with an aerodynamic diameter ≤ 10 μm (PM10), sulfur dioxide (SO2), O3, and nitrogen dioxide (NO2) from the Dongguan Environmental Monitoring Center. These levels were measured by averaging values obtained from five fixed air monitoring stations (Additional file 1: Figure S1).
Statistical model
We used a two-stage analysis approach. During the first stage, we applied a standard time series quasi-Poisson regression with a distributed lag non-linear model (DLNM) to estimate the associations between daily mean temperature and morbidity of total and specific respiratory-related outpatient visits. Meanwhile, we conducted stratified analyses by age group to observe the potential effects of age on temperature-respiratory morbidity relationships.
The exposure-response relationship was modeled using a quadratic B-spline for temperature with three internal knots placed at equal temperature interval distributions, and the lag-response curve used a natural cubic spline with an intercept and three internal knots placed at equally spaced values along the log scale [14]. We used this stratified strategy to control for seasonality and long-term trends by the natural cubic spline of the year with 4 degrees of freedom and month with 3 degrees of freedom [20]. To control for time-varying confounders, we included relative humidity, air pollutants, dummy variables for day of the week, and public holidays in the model. We also defined three degrees of freedom for relative humidity, PM10, SO2, NO2, and O3, consistent with several previous studies. Akaike’s Information Criterion for quasi-Poisson (Q-AIC) was used to evaluate the model fits, which was subsequently applied to other studies [21,22,23]. In all the models, we used seven days as the maximum lag to adequately assess cold- and heat-related effects on hospital outpatient visits. The model was:
where t is the day of the study period; E(Yt) presents the expected daily counts for hospital outpatient visits for respiratory diseases on day t; α is the intercept; Tempt, l is the cross-basis matrix obtained by modeling the DLNM to temperature; l is the lag days. Strata refers two categorical variables of year and calendar month that were used to control for long-term trends and seasonality; ns(.) means the natural cubic spline function for nonlinear variables; df is the degrees of freedom; RH is the relative humidity; DOW is a categorical variable for controlling for the day of the week. Holiday is a binary variable. If the day t is a public holiday the value of 1 otherwise 0; β, γ, δ, ε are vectors of coefficients for corresponding terms.
The temperature of the minimum morbidity (MMT), characterized by the lowest risk of respiratory hospital outpatient visits, was derived from the lowest point of overall cumulative exposure-response curve. We referred to the value as the optimum temperature (centering value) for fitting the exposure–lag–response relationship in each model. Extreme cold and heat were defined temperatures at the 5th percentile or less (extreme cold), and at the 95th percentile or above (extreme heat). We calculated the RRs and 95% CIs of respiratory morbidity at the 5th and 95th percentile of temperature distribution, referenced to the optimum temperature for representing the effects of extreme cold and heat.
Estimation of AR
During the second stage, we used a backward perspective strategy to quantify the burden of respiratory outpatient visits due to temperature exposures. This approach examined from current risk to past exposures, and has been described in detail elsewhere [14]. Backward standpoint assumes that the risk at time t can be attributed to a series of past exposure events. The backward attributable fraction AFx,t, and number ANx,t at time t can be expressed as:
Here, nt is the number of cases at time t. The risk at time t is associated with lagged exposures at times t − l. ANx,t and AFx,t are the number of cases and the related fraction at time t attributable to past exposures to x in the period t − l0,. .., t − L.
The optimum temperature was also regarded as the reference for computing the fractions and the numbers of excess outpatient visits attributable to the temperatures. We further divided the temperature distribution into the extreme cold and heat, and the moderate cold and heat. We defined “moderate temperatures” as the ranges between the optimum temperature and the 5th and 95th percentiles (Additional file 2: Figure S2). We then calculated the health burden attributable to extreme and moderate temperatures with reference to the optimum temperature. The estimation of empirical CIs for attributable fractions and numbers were obtained through Monte Carlo simulations [24, 25], by simulating 5000 random samples. All the statistical analyses were performed using the R software (version 3.4.4) with the “dlnm” package.
Results
The characteristics of the sample
Table 1 summarizes morbidity, weather, and air pollution data in Dongguan City. During the study period, there were 75,015 hospital outpatient visits related to respiratory diseases. Of these, there were 11,068 cases of COPD, 28,059 cases of asthma, and 7991 cases of bronchiectasis. On average, there were 44 respiratory-related hospital outpatient visits. Of these, 17 were related to asthma, 7 were related to COPD, and 5 were related to bronchiectasis. The daily mean temperature was 23.2 °C (3.8–33.2 °C), and the relative humidity was 77.5% with a range of 22.0–100.0%. The daily mean concentration was 56.6 μg/m3 for PM10, 15.9 μg/m3 for SO2, 38.8 μg/m3 for NO2, and 62.0 μg/m3 for O3. Figure 1 depicts a time series plot of daily mean temperatures and hospital outpatient visits for total and specific-respiratory diseases.
Morbidity risk of temperature on respiratory diseases
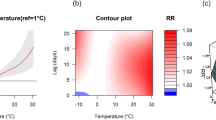
Figure 2 shows the temperature–morbidity curves for total and specific respiratory diseases. The associations between temperature and morbidity of respiratory diseases are U or inverse J-shaped. The risks of temperature on total respiratory diseases, asthma, and COPD were significantly higher at low temperatures than at high temperatures.
The cumulative associations between mean temperature and daily hospital outpatient visits for total respiratory diseases, asthma, COPD, and bronchiectasis over a lag of 0–7 days. The shaded grey is the 95% CI, and the dashed lines show the optimal temperatures of 15.20 °C, 15.50 °C, 19.60 °C, and 15.60 °C. Respiratory indicates respiratory disease; COPD means chronic obstructive pulmonary disease
The risks of extreme temperature on morbidity for total and specific respiratory diseases are displayed in Table 2. Compared with optimum temperature, the overall RRs associated with extreme heat were larger than those associated with extreme cold for total respiratory morbidity, asthma, and bronchiectasis. The effects of extreme cold or heat on outpatient visits for COPD were similar. Figure 3 further presents the temperature-respiratory morbidity relationships by age group. Among younger patients (0–64 years old), the risk of heat on total respiratory morbidity was higher than that of cold. However, a reverse J-shaped relationship was observed for the elderly; namely, the risk of cold on total respiratory morbidity was significantly higher than that of heat. Exposure-response curves for bronchiectasis and COPD followed a similar pattern as total respiratory morbidity. However, for asthma, the cold-related risk was higher than the hot-related risk.
Attributable fraction of temperature on respiratory morbidity
Table 3 shows the attributable fraction (%) of outpatient visits for respiratory diseases due to different temperature components. Overall, 8.4% (95% eCI: 2.8–13.3%) of respiratory morbidity was attributed to non-optimal temperatures, and most of these were from moderate heat (7.5, 95% eCI: 2.4–12.2%), and only 0.6% (0.0 to 1.1%) were related to extreme heat. In addition, the burden of respiratory morbidity attributable to extreme cold and mild cold were very small: 0.3% (0.0–0.6%) for extreme cold and 0.0% (0.0–0.1%) for moderate cold. Further results on the attributable number of total and specific respiratory diseases morbidity due to different temperature components are shown in Additional file 3: Table S1.
The attributable fractions (%) varied among age-groups (Table 3). For the population aged 0–64 years old, 12.6% of total respiratory, 12.5% of bronchiectasis, and 11.1% of asthma morbidity resulted from exposure to moderate heat. Nevertheless, for the elderly (≥65 years old), the temperature-related morbidity burdens for total and specific respiratory diseases were mainly caused by cold.
Discussion
In this study, we examined the association between ambient temperature and respiratory morbidity, and further quantified morbidity burden attributed to different temperature ranges in Dongguan city. Our results revealed that a significant percentage (8.4%) of respiratory outpatient visits were attributable to ambient temperatures within the study period. Most of the morbidity burden of total respiratory diseases was caused by moderate heat exposure (7.5%). In general, this finding was consistent with several previous studies [7, 26, 27]. Our results might be explained by the fact that most of days (about 82.2%) within our study time series featured moderate heat. However, our results were different from previous results that were estimated by mortality [28,29,30]. The difference may be explained mainly by that minimum morbidity temperature is much lower in our study than that minimum mortality temperature identified in previous studies.
We also observed that both cold and heat could increase the risk of respiratory outpatient visits, in agreement with previous studies [7, 20, 31]. However, the mechanisms behind this relationship are not entirely clear. Previous laboratory and clinical studies found that temperatures directly influenced respiratory morbidity by inciting vascular changes, releasing inflammatory mediators, and decreasing the effectiveness of immune responses [32,33,34,35,36]. Moreover, ambient temperatures can indirectly induce respiratory events, such as viral infections, bacterial activity, or respiratory tract infections [37,38,39].
Stratified analyses by age group showed that younger people (< 65 years) were at high risk of exposure to heat while the elderly (≥65 years) were at high risk of exposure to cold. Moreover, morbidity burdens of total and specific respiratory diseases differed by age group. For younger people, the morbidity burden of total and specific respiratory diseases was mainly attributable to moderate heat. Similar results were also reported before [40]. There are two possible reasons for the observed findings. First, attributable fractions are not only determined by relative risk, but also by temperature distributions. In subtropical cities like Dongguan, most throughout the year are hot days. Younger people tend to stay outdoors longer for work, and are more likely to be exposed to hot ambient temperatures, compared to the elderly. Second, for the younger population, the minimum morbidity temperatures are relatively low for total and specific respiratory diseases. This causes some low temperatures to be classified as hot temperature range, which leads to hot days accounting for a high proportion of our study period data. Therefore, morbidity burdens attributed to heat in the younger population may be very high.
On the contrary, we found that, for the elderly, the attributable fractions of total respiratory diseases, bronchiectasis, and asthma were caused by cold temperatures. The possible reasons are that respiratory diseases are highly prevalent among the elderly, and exposure to cold temperatures may increase the risk of developing pulmonary vascular resistance and thromboses [41, 42]. Also, airway neutrophils, macrophages, and the levels of respiratory inflammation were increased in patients residing in cold environments. Thus, bronchospasm was easily aggravated in patients with asthma, and airway obstruction was easily aggravated in COPD [43].
Our findings have important public health implications because, although extreme heat is riskier than moderate heat, days with moderate heat account for most days in a year in subtropical regions like Dongguan city. Thus, more attention should be paid to moderate heat for the young population when planning adaptation strategies and measures to reduce health risks related to ambient temperature exposures in subtropical regions. Meanwhile, we should put emphasis on the elderly in winter to prevent them from cold exposure.
There were some limitations to the current study. First, this was ecological research which lacked individual-level data pertaining to exposure and the influence of personal activity patterns, etc. Second, we did not obtain epidemiological data pertaining to influenza, which could be a confounding factor or effect moderator. Additionally, hospital visit data were gathered from one single hospital, which may limit the generalizability of our research findings.
Conclusions
Both high and low temperatures increased the morbidity risk of respiratory diseases. Moderate heat was mainly responsible for most of the morbidity burden caused by ambient temperature exposure. Younger individuals were at increased risk following exposure to hot temperatures, whereas the elderly was more susceptible to cold temperatures. These findings carry implications for planning public health interventions that protect vulnerable populations within non-optimal temperature environments.
Availability of data and materials
Please contact the author for data requests.
Abbreviations
- AF:
-
Attributable fraction
- AN:
-
Attributable number
- AR:
-
Attributable risk
- CI:
-
Confidence Interval
- CO:
-
Carbon monoxide
- COPD:
-
Chronic obstructive pulmonary disease
- DLNM:
-
Distributed lag non-linear model
- eCIs:
-
Empirical confidential intervals
- MMT:
-
Temperature of the minimum morbidity
- NO2 :
-
Nitrogen dioxide
- PM10 :
-
Particulate matter with an aerodynamic diameter ≤ 10 μm
- QAIC:
-
Akaike Information Criteria for Quasi Poisson
- RR:
-
Relative risk
- SO2 :
-
Sulfur dioxide
References
Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abera SF, et al. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1084–150.
Sun W, Zhou Y, Zhang Z, Cao L, Chen W. The trends in cardiovascular diseases and respiratory diseases mortality in urban and rural China, 1990-2015. Int J Environ Res Public Health. 2017;14(11):1391.
Analitis A, Katsouyanni K, Biggeri A, Baccini M, Forsberg B, Bisanti L, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol. 2008;168(12):1397–408.
Gasparrini A, Armstrong B, Kovats S, Wilkinson P. The effect of high temperatures on cause-specific mortality in England and Wales. Occupational & Environmental Medicine. 2011;69(1):56.
Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20(2):205.
Mäkinen TM, Juvonen R, Jokelainen J, Harju TH, Peitso A, Bloigu A, et al. Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respiratory Medicine. 2009;103(3):456–62.
Michelozzi P, Accetta G, De SM, D'Ippoliti D, Marino C, Baccini M, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med. 2009;179(5):383–9.
Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002;24(2):190–202.
Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120(1):19–28.
Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386(9991):369–75.
Baccini M, Kosatsky T, Analitis A, Anderson HR, D'Ovidio M, Menne B, et al. Impact of heat on mortality in 15 European cities: attributable deaths under different weather scenarios. J Epidemiol Community Health. 2011;65(1):64–70.
Honda Y, Kondo M, Mcgregor G, Kim H, Guo YL, Hijioka Y, et al. Heat-related mortality risk model for climate change impact projection. Environmental Health & Preventive Medicine. 2014;19(1):56.
Tian L, Qiu H, Sun S, Lin H. Emergency cardiovascular hospitalizations risk attributable to cold temperatures in Hong Kong. Circulation Cardiovascular Quality & Outcomes. 2016;9(2):135.
Gasparrini A, Leone M. Attributable risk from distributed lag models. BMC Medical Research Methodology,14,1(2014-04-23). 2014; 14(1):55.
Steenland K, Armstrong B. An overview of methods for calculating the burden of disease due to specific risk factors. Epidemiology. 2006;17(5):512–9.
Wang YC, Lin YK. Temperature effects on outpatient visits of respiratory diseases, asthma, and chronic airway obstruction in Taiwan. Int J Biometeorol. 2015;59(7):815–25.
Wang YC, Lin YK, Chuang CY, Li MH, Chou CH, Liao CH, et al. Associating emergency room visits with first and prolonged extreme temperature event in Taiwan: a population-based cohort study. Sci Total Environ. 2012;416(2):97–104.
Lin S, Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20(5):738.
Ma W, Xu X, Peng L, Kan H. Impact of extreme temperature on hospital admission in Shanghai. China Science of the Total Environment. 2011;409(19):3634–7.
Zhao Q, Zhao Y, Li S, Zhang Y, Wang Q, Zhang H, et al. Impact of ambient temperature on clinical visits for cardio-respiratory diseases in rural villages in Northwest China. Sci Total Environ. 2018;612:379–85.
Akaike H. Information theory and an extension of the maximum likelihood principle. In: International Symposium on Information Theory. 1973;1973:610–24.
Gasparrini A. Modeling exposure–lag–response associations with distributed lag non-linear models. Stat Med. 2014;33(5):881–99.
Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Stat Med. 2011;29(21):2224–34.
Greenland S. Interval estimation by simulation as an alternative to and extension of confidence intervals. Int J Epidemiol. 2004;33(6):1389–97.
Simon N. Generalized additive models : an introduction with R. Chapman & Hall/CRC. 2006.
D'Ippoliti D, Michelozzi P, Marino C, De'Donato F, Menne B, Katsouyanni K, et al. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health. 2010;9(1):37.
Green RS, Basu R, Malig B, Broadwin R, Kim JJ, Ostro B. The effect of temperature on hospital admissions in nine California counties. International Journal of Public Health. 2010;55(2):113.
Ballester F, Corella D, Pérez-Hoyos S, Sáez M, Hervás A. Mortality as a function of temperature. A study in Valencia, Spain, 1991–1993. International Journal of Epidemiology. 1997;26(3):551.
Davis RE, Knappenberger PC, Michaels PJ, Novicoff WM. Seasonality of climate-human mortality relationships in US cities and impacts of climate change. Clim Res. 2004;26(1):61–76.
Huynen MM, Martens P, Schram D, Weijenberg MP, Kunst AE. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ Health Perspect. 2001;109(5):463–70.
Su Q, Liu H, Yuan X, Xiao Y, Zhang X, Sun R, et al. The interaction effects of temperature and humidity on emergency room visits for respiratory diseases in Beijing. China Cell Biochemistry & Biophysics. 2014;70(2):1377–84.
Diesel DA, Lebel JL, Tucker A. Pulmonary particle deposition and airway mucociliary clearance in cold-exposed calves. Am J Vet Res. 1991;52(10):1665.
Gordon CJ. Role of environmental stress in the physiological response to chemical toxicants. Environ Res. 2003;92(1):1–7.
Larsson K, Tornling G, Gavhed D, Müller-Suur C, Palmberg L. Inhalation of cold air increases the number of inflammatory cells in the lungs in healthy subjects. Eur Respir J. 1998;12(4):825–30.
Togias AG, Naclerio RM, Proud D, Fish JE Jr. NFA, Kageysobotka a, et al. nasal challenge with cold, dry air results in release of inflammatory mediators. Possible mast cell involvement. J Clin Investig. 1985;76(4):1375–81.
Malik AB, Johnson A, Tahamont MV, Van dZH BFA. Role of blood components in mediating lung vascular injury after pulmonary vascular thrombosis. Chest. 1983;83(5 Suppl):21S.
Buckley JP, Richardson DB. Seasonal modification of the association between temperature and adult emergency department visits for asthma: a case-crossover study. Environ Health. 2012;11(1):55.
Danielides V, Nousia CS, Patrikakos G, Bartzokas A, Lolis CJ, Milionis HJ, et al. Effect of meteorological parameters on acute laryngitis in adults. Acta Otolaryngol. 2002;122(6):655–60.
Yu L, Yong G, Wang C, Li W, Lu J, Shen S, et al. Association between temperature change and outpatient visits for respiratory tract infections among children in Guangzhou, China. Int J Environ Res Public Health. 2015;12(1):439–54.
Zhao Q, Zhang Y, Zhang W, Li S, Chen G, Wu Y, et al. Ambient temperature and emergency department visits: time-series analysis in 12 Chinese cities. Environ Pollut. 2017;224:310–6.
Kawahara J, Sano H, Fukuzaki H, Saito K, Hirouchi H. Acute effects of exposure to cold on blood pressure, platelet function and sympathetic nervous activity in humans. Am J Hypertens. 1989;2(9):724–6.
Sprung CL. Heat stroke; modern approach to an ancient disease. Chest. 1980;77(4):461–2.
Damato G, Holgate ST, Pawankar R, Ledford DK, Cecchi L, Alahmad M, et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the world allergy organization. World Allergy Organization Journal. 2015;8(1):1–52.
Acknowledgments
We acknowledge the contributions of the staff of the Fifth People’s Hospital of Dongguan. These individuals collected data for this study.
Funding
National Key R&D Program of China supported this study (No. 2018YFA0606202) and the Guangzhou Science and Technology Program key projects (No. 201704020194).
Author information
Authors and Affiliations
Contributions
ZH, YJZ, and WJM conceived the study. ZH and JXH provided data on the outcome and performed the statistical analysis. ZH and YJZ drafted the first version of the manuscript. All authors contributed to interpretation of results and manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Figure S1.
Geographical distribution of the Dongguan in Guangdong Province, China (the left-upper panel shows the location of Guangdong Province in China). The red spots represent the location of five air monitoring stations, the blue “H” shape Icon represent the location of the Dongguan Fifth People’s Hospital.
Additional file 2: Figure S2.
The definition of temperature range.
Additional file 3: Table S1.
Attributable number of hospital outpatient visits attributable to ambient temperature exposure for respiratory diseases and subcategories by age-groups, 2013 to 2017.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhao, Y., Huang, Z., Wang, S. et al. Morbidity burden of respiratory diseases attributable to ambient temperature: a case study in a subtropical city in China. Environ Health 18, 89 (2019). https://doi.org/10.1186/s12940-019-0529-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-019-0529-8