Abstract
Background
For still unclear reasons, chronic airway infection often occurs in patients with Chronic Obstructive Pulmonary Disease (COPD), particularly in those with more severe airflow limitation. Fatty-acid binding protein 4 (FABP4) is an adipokine involved in the innate immune response against infection produced by alveolar macrophages (Mɸ). We hypothesized that airway levels of FABP4 may be altered in COPD patients with chronic airway infection.
Methods
In this prospective and controlled study we: (1) compared airway FABP4 levels (ELISA) in induced sputum, bronchoalveolar lavage fluid (BALF) and plasma samples in 52 clinically stable COPD patients (65.2 ± 7.9 years, FEV1 59 ± 16% predicted) and 29 healthy volunteers (55.0 ± 12.3 years, FEV1 97 ± 16% predicted); (2) explored their relationship with the presence of bacterial airway infection, defined by the presence of potentially pathogenic bacteria (PPB) at ≥103 colony-forming units/ml in BALF; (3) investigated their relationship with the quantity and proportion of Mɸ in BALF (flow cytometry); and, (4) studied their relationship with the severity of airflow limitation (FEV1), GOLD grade and level of symptoms (CAT questionnaire).
Results
We found that: (1) airway levels of FABP4 (but not plasma ones) were reduced in COPD patients vs. controls [219.2 (96.0–319.6) vs. 273.4 (203.1–426.7) (pg/ml)/protein, p = 0.03 in BALF]; (2) COPD patients with airway infection had lower sputum FABP4 levels [0.73 (0.35–15.3) vs. 15.6 (2.0–29.4) ng/ml, p = 0.02]; (3) in COPD patients, the number and proportion of Mɸ were positively related with FABP4 levels in BALF; (4) BALF and sputum FABP4 levels were positively related with FEV1, negatively with the CAT score, and lowest in GOLD grade D patients.
Conclusions
Airway FABP4 levels are reduced in COPD patients, especially in those with airway infection and more severe disease. The relationship observed between Mɸ and airway FABP4 levels supports a role for FABP4 in the pathogenesis of airway infection and disease severity in COPD.
Similar content being viewed by others
Introduction
Chronic Obstructive Pulmonary Disease (COPD) currently is the third leading cause of mortality worldwide [1]. Chronic airway bacterial infection often occurs in COPD patients, particularly in those with more severe airflow limitation [2, 3]. The presence of airway infection increases the economic impact of the disease and worsens clinical outcomes including increased mortality [4]. Several studies have demonstrated that innate immunity alterations favor airway infection in COPD [5, 6]. However, the underlying biological mechanisms leading to chronic airway infection in COPD have not been yet fully elucidated.
Alveolar macrophages (Mɸ) are a central component of the innate immune response against airway infection. Several alterations of Mɸ in marker expression and functions have been previously described in COPD [7, 8]. Among many other functions, Mɸ produce fatty acid-binding protein 4 (FABP4), also known as adipocyte A-FABP or aP2. FABP4 is a member of the FABP family of small-molecular weight intracellular lipid chaperones that functions as a secreted adipokine and plays a role in airway defense against infection [9, 10]. For instance, in an experimental model of Pseudomonas aeruginosa infection in mice, the presence of FABP4 protected against airway infection [11]. However, limited data on COPD and its relationship with disease severity and airway infections are available.
We hypothesized that airway FABP4 levels may be reduced in COPD patients, especially in those with the more severe disease and with potentially more dysfunctional Mɸ. Accordingly, this study sought to: (1) compare airway (and plasma) FABP4 levels in COPD and healthy volunteers and, (2) study their relationship with presence of airway infection, quantity and proportion of Mɸ and several clinical markers of disease severity, such as the severity of airflow limitation (FEV1), the GOLD classification and the level of symptoms (CAT questionnaire).
Methods
Study design and ethics
This was a prospective, multicenter, cross-sectional study that included clinically stable COPD patients and healthy volunteers with normal lung function, who served as controls. Participants were recruited from five university tertiary hospitals [Hospital de la Santa Creu i Sant Pau (Barcelona, Spain), Hospital del Mar (Barcelona, Spain), Hospital Universitari Parc Taulí (Sabadell, Spain), Hospital Germans Trias i Pujol (Barcelona, Spain) and Hospital Clínic (Barcelona Spain)]. The study protocol was approved by the local institutional review board (IIBSP-MIC-2015-57) and all subjects gave signed informed consent.
Participants
The diagnosis of COPD was established according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines [12]. The inclusion criteria were: 8 weeks of clinical stability (defined by the absence of an exacerbation that required oral corticosteroids and/or antibiotic treatment), age between 40 and 75 years, and FEV1 between 20 and 70% predicted. All patients underwent a computerized tomography scan, and those with bronchiectasis, lung cancer, pneumonia, and/or interstitial lung diseases were excluded. Other exclusion criteria were patients with active malignant disease and/or any type of immunosuppression, drug addiction or alcohol abuse. As controls, we included adult volunteers without respiratory diseases and with normal spirometry recruited in these same centers [13].
Clinical assessment
Demographic data, the number of exacerbations in the previous year, the time from last exacerbation, relevant comorbid conditions and current treatments were recorded at inclusion using standardized questionnaires. All patients underwent spirometry (Datospir-600; Sibelmed SA, Barcelona, Spain) following international recommendations. Reference values were those of Mediterranean populations [14].
Samples collection and processing
Bronchoalveolar lavage fluid (BALF), induced sputum and plasma were obtained from all participants and were processed immediately. BALF samples were recovered using 150 ml saline lavage with the bronchoscope wedged in the right middle lobe. BALF samples were centrifuged at 800 xg for 10 min to obtain the cellular pellet and the supernatant. Induced sputum was collected just before the bronchoscopy as previously described [15]. Sputum samples were disaggregated using dithiothreitol (Oxoid Ltd., Hampshire, United Kingdom) for 15 min and were centrifuged at 600 xg for 6 min to obtain the supernatant. Proteases inhibitors (Calbiochem, San Diego, CA) were added to the supernatants during thawing. Plasma samples were obtained from blood collected in ethylenediamine tetra-acetic acid (EDTA) tube and centrifuged at 850 xg for 10 min. BALF and sputum supernatants and plasma were stored immediately at − 80 °C until analysis.
Microbiological study
Samples were processed for qualitative and quantitative bacteriology, as previously described [16]. Airway infection was defined as the presence of potentially pathogenic bacteria (PPB) at ≥103 colony-forming units/ml in BALF [17] in clinically stable patients.
FABP4 measurement
FABP4 levels were measured by validated, commercially available ELISA kit (RayBiotech, Peachtree Corners, GA) according to the manufacturer’s instructions. The limit of kit detection was 38 pg/ml. The dilutions used were 1/7 for BALF supernatants, 1/5 for sputum supernatants and 1/75 for plasma. BALF FABP4 levels were adjusted to the total protein content quantified using Qubit fluorometer (Invitrogen, Carlsbad, CA).
BALF flow cytometry
In COPD patients, cellular pellet obtained from BALF samples was lysed to avoid red blood cells contamination (RBC lysing solution; BioLegend, San Diego, CA). Cells were resuspended in one ml of PBS supplemented with 2% bovine serum albumin (BSA; Roche Diagnostics GmbH, Mannheim, Germany) to quantify the number of total cells in a MACSQuant cytometer (Miltenyi Biotec, Bergisch Gladbach, Germany). Cells were adjusted to 1x106cells/ml and stained for 15 min at room temperature in dark with viability dye (Zombie NIR; BioLegend), CD45-FITC, CD14-APC (Immunotools GmbH, Friesoythe, Germany) and CD15-PE (Biolegend, San Diego, CA). Aggregated and non-viable cells were excluded from the analysis. Mɸ were gated according to CD45 positive population, CD15 negative, CD14 positive and high side scatter (SSC) parameter.
Statistical analyses
Results of continuous variables are presented as mean and standard deviation (SD) or median and interquartile range [25th – 75th percentile IQR], according to the Kolmogorov-Smirnov test of normality distribution, whereas categorical variables are presented as frequencies. Groups were compared using Student t-test, ANOVA test or their corresponding non-parametrical test when required. Correlations were analyzed using Spearman’s Rho due to the variables did not present a normal distribution. A p-value < 0.05 was considered significant. Statistical analyses were performed using SPSS version 22 and Graph Pad Prism 7 software.
Results
Characteristics of participants
Fifty-two COPD patients and 29 controls were included. Table 1 shows their demographic and clinical characteristics. COPD patients were older (65.2 ± 7.9 vs. 55.0 ± 12.3, p = 0.0002) than controls but gender (75.9 vs. 65.4% males, p = 0.6) and BMI (26.3 ± 4.7 vs. 28.7 ± 9.7, p = 0.7) were similar in both groups. Airflow limitation in patients with COPD ranged from mild to severe (FEV1 of 59 ± 15% of predicted) whereas spirometry was normal in controls by design. Twenty-four patients (46%) were classified as GOLD grade C and D, and 21 patients (40%) were frequent exacerbators, defined as those patients who suffered from 2 or more exacerbations during the previous year to the inclusion.
Twelve COPD patients (23%) had airway infection. Patients with airway infection were predominantly males (92%) and older than non-infected ones (Table 2). Haemophilus influenzae was the most common PPB isolated (n = 9, 75%), followed by Streptococcus pneumoniae (n = 2, 17%) and Moraxella catharralis (n = 1, 8%).
Airway and systemic FABP4 levels in patients and controls
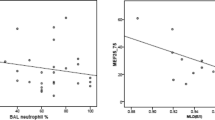
Airway FABP4 levels were lower in COPD patients than in controls, reaching statistical significant differences in BALF [219.2 (96.0–319.6) vs. 273.4 (203.1–426.7) (pg/ml)/protein, p = 0.03], but not in sputum [12.2 (0.7–27.5) vs. 14.5 (0.5–45.6) ng/ml, p = 0.4] (Fig. 1A, C). Yet, we observed a positive significant correlation between BALF and sputum FABP4 levels in the entire population (rho = 0.31, p = 0.01) and in COPD patients (rho = 0.37, p = 0.01). On the other hand, plasma FABP4 levels were similar in patients and controls [26.6 (19.3–39.5) vs. 25.2 (18.3–36.5) ng/ml, p = 0.4)] and no significant correlation was observed between systemic and airway FABP4 levels.
Airway FABP4 levels in COPD. A BALF FABP4 levels in controls and COPD patients and (B) in non-infected and infected patients. C Sputum FABP4 levels in controls and COPD patients and (D) in non-infected and infected patients. P-values were obtained by Mann-Whitney test. *p-value < 0.05. Data is represented as median with interquartile range
FABP4 levels and airway infection in COPD patients
Airway FABP4 levels were lower in COPD patients with airway infection vs. those without it, reaching statistical significant differences in sputum [0.73 (0.35–15.3) vs. 15.6 (2.0–29.4) ng/ml, p = 0.02] but not in BALF [181.5 (28.7–395.5) vs. 228.5 (106.3–319.1) (pg/ml)/protein, p = 0.7) (Fig. 1B, D). No differences in plasma FABP4 levels were observed between COPD patients with and without airway infection [29.8 (20.4–45.0) vs. 26.1 (19.3–37.9) ng/ml, p = 0.6].
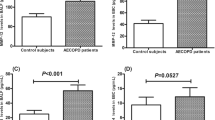
FABP4 levels and disease severity
Airway (but not plasma) FABP4 levels were related with several measures of disease severity, including GOLD stage, airway limitation and quality of life. Patient with GOLD D had the lowest values both in BALF (Fig. 2A) and sputum (Fig. 2B). In addition, a positive correlation among airway FABP4 levels and FEV1 (% predicted) (Fig. 3A, B) and a negative correlation with levels of symptoms measured in CAT questionnaire (Fig. 3C, D) were observed.
Association of airway FABP4 levels and disease severity. A BALF and (B) Sputum FABP4 levels and GOLD stages classified in mild (GOLD A), moderate (GOLD B), severe (GOLD C) and very severe (GOLD D). P-values were obtained by Mann-Whitney test. *p-value < 0.05 and **p-value < 0.01. Data is represented as median with interquartile range
No differences in airway FABP4 levels were observed regarding age and smoking status. Patients using inhaled corticosteroid (ICS) had lower values in BAL compared with those without ICS [(pg/ml)/protein, 123.6 (12.6–306.4) vs 250 (171.6–344.7), p = 0.03)].
FABP4 and alveolar Mɸ
Alveolar Mɸ represented 49.9 (26.4–76.8) % of cells in BALF of COPD patients, corresponding to an absolute number of 140 (48.9–311) Mɸ per μl. Both proportion and absolute number of alveolar Mɸ were significantly related with BALF FABP4 levels [proportion (rho = 0.54, p = 0.0003) and absolute number (rho = 0.52, p = 0.0006)] (Fig. 4). No significant differences among infected and non-infected patients and related to GOLD stage were found.
Discussion
The main results of this study show that, as hypothesized: (1) airway (but not plasma) levels of FABP4 are reduced in COPD patients, particularly in those with airway infection and more severe disease; and, (2) BALF FABP4 levels are related to the number and proportion of alveolar Mɸ. Collectively, these results suggest that reduced production of FABP4 by alveolar Mɸ is associated with the presence of airway infection in COPD.
Previous studies
FABP4 is an adipokine widely studied in metabolic and cardiovascular diseases [18]. Its role in chronic respiratory diseases is poorly understood, although it has been recognized that FABP4 is associated with airway inflammation [19]. Likewise, a dysregulation of airway FABP4 has been previously described in asthma [20] where it has been shown in experimental models that FABP4 participates in the recruitment and activation of eosinophils [21]. In patients with COPD, a dysregulation of systemic FABP4 compared with controls has been suggested [22], which is at variance with our findings here. Differences may be related to distinct inclusion criteria. Whereas Zhang et al excluded patients with metabolic and vascular comorbidities [22], known to be associated with elevated systemic FABP4 levels [23, 24], we did not because cardiovascular comorbidities are highly prevalent in patients with COPD (74% in our cohort) and we did not want to bias our study population. In any case, to our knowledge, our study is the first to investigate airway FABP4 levels, and their relationship with airway infection and disease severity in COPD.
Interpretation of novel findings
Bacterial airway infections are relevant in the natural history of COPD [3] because it worsens clinical outcomes, including mortality and costs [4]. The molecular and cellular mechanisms that favor bacterial infection in some COPD patients are, however, not yet fully elucidated. We observed that airway FABP4 levels were reduced in COPD patients, particularly in those with evidence of airway infection, and we found a relationship between BALF Mɸ (absolute number and proportion) and FABP4 levels in COPD. Given that alveolar Mɸ produce FABP4 [9], these observations support a pathogenic role for a locally defective Mɸ production of FABP4. In support of this interpretation is the fact that FABP4 facilitates the interaction between Mɸ and neutrophils through the regulation of CXCL1, a chemokine secreted by Mɸ to recruit neutrophils to the site of infection [11, 25]. Further works studying Mɸ subpopulations would help to better understand the immunological mechanism related to FABP4 production by Mɸ.
On the other hand, we found that patients with severe COPD showed the lowest airway FABP4 levels. We also found that there was a direct relationship between airway FABP4 concentration and FEV1 levels and an inverse relationship between the former and CAT score (i.e. worse health status). In keeping with these observations, some previous studies had demonstrated that patients with severe COPD have altered airway innate immunity [16, 26, 27] that leads to chronic airway inflammation and dysregulation of normal alveolar Mɸ function [28]. Yet, because our study is cross-sectional, we cannot infer what is the cause and what is the consequence, this is, what comes first.
Potential limitations
Our study has some limitations that deserve comment. First, controls were younger than COPD patients, but we did not observe any relationship between airway FABP4 levels and the age of the participants. Second, induced sputum was collected just before the bronchoscopy so we cannot discard any interaction with BALF samples, although this procedure had been applied to all the participants. Third, we did not perform flow cytometry in BALF from controls, but it is well reported in the literature that COPD alveolar Mɸ differ from healthy controls in phenotype [29] and in the ability to phagocytose bacteria and apoptotic cells [30, 31]. Forth, we have not determined FABP4 in infected patients without COPD and it would be of great interest to better understand its role in the pathogenesis or airway infection. Finally, we did not obtain follow-up samples, so we cannot infer if any therapeutic intervention (e.g., treatment with low dose azithromycin) can restore airway FABP4 levels and what clinical consequences that may have.
Conclusions
FABP4 airway levels (but not plasma ones) are reduced in COPD patients, especially in those with chronic airway infection and more severe disease, in relation to a reduced number of alveolar Mɸ. These observations may be relevant for a better understanding of the pathogenesis (and eventual prevention or treatment) of chronic airway infection in these patients.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- APC:
-
Allophycocyanin
- BALF:
-
Bronchoalveolar lavage fluid
- BSA:
-
Bovine serum albumin
- CAT:
-
COPD assessment test
- COPD:
-
Chronic obstructive pulmonary disease
- EDTA:
-
Ethylenediamine tetraacetic acid
- ELISA:
-
Enzyme-linked immunosorbent assay
- FABP4:
-
Fatty-acid binding protein 4
- FEV1 :
-
Forced expiratory volume in one second
- FITC:
-
Fluorescein isothiocyanate
- GOLD:
-
Global Initiative for chronic obstructive lung disease
- IQR:
-
Interquartile range
- PE:
-
Phycoerythrin
- PPB:
-
Potentially pathogenic bacteria
- SD:
-
Standard deviation
- SSC:
-
Side scatter
References
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (London). 2012;380(9859):2095–128.
Monsó E, Ruiz J, Rosell A, Manterola J, Fiz J, Morera J, et al. Bacterial infection in chronic obstructive pulmonary disease. A study of stable and exacerbated outpatients using the protected specimen brush. Am J Respir Crit Care Med. 1995;152(4):1316–20.
Zalacain R, Sobradillo V, Amilibia J, Barrón J, Achótegui V, Pijoan JI, et al. Predisposing factors to bacterial colonization in chronic obstructive pulmonary disease. Eur Respir J. 1999;13(2):343–8.
Patel IS, Seemungal TAR, Wilks M, Lloyd-Owen SJ, Donaldson GC, Wedzicha JA. Relationship between bacterial colonisation and the frequency, character, and severity of COPD exacerbations. Thorax. 2002;57(9):759–64.
Sethi S, Maloney J, Grove L, Wrona C, Berenson CS. Airway inflammation and bronchial bacterial colonization in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173(9):991–8.
Mizgerd JP. Acute lower respiratory tract infection. N Engl J Med. 2008;358(7):716–27.
Berenson CS, Kruzel RL, Eberhardt E, Dolnick R, Minderman H, Wallace PK, et al. Impaired innate immune alveolar macrophage response and the predilection for COPD exacerbations. Thorax. 2014;69(9):811–8.
Dewhurst JA, Lea S, Hardaker E, Dungwa JV, Ravi AK, Singh D. Characterisation of lung macrophage subpopulations in COPD patients and controls. Sci Rep. 2017;7(1):7143.
Ghelfi E, Karaaslan C, Berkelhamer S, Akar S, Kozakewich H, Cataltepe S. Fatty acid–binding proteins and Peribronchial angiogenesis in Bronchopulmonary dysplasia. Am J Respir Cell Mol Biol. 2011;45(3):550–6.
Cao H, Sekiya M, Ertunc ME, Burak MF, Mayers JR, White A, et al. Adipocyte lipid chaperone aP2 is a secreted adipokine regulating hepatic glucose production. Cell Metab. 2013;17(5):768–78.
Liang X, Gupta K, Quintero JR, Cernadas M, Kobzik L, Christou H, et al. Macrophage FABP4 is required for neutrophil recruitment and bacterial clearance in Pseudomonas aeruginosa pneumonia. FASEB J. 2018;33(3):3562–74.
Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164.
Agusti A, Calverley PMA, Celli B, Coxson HO, Edwards LD, Lomas DA, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122.
Castellsagué J, Burgos F, Sunyer J, Barberà JA, Roca J. Prediction equations for forced spirometry from European origin populations. Barcelona collaborative group on reference values for pulmonary function testing and the Spanish Group of the European Community Respiratory Health Survey. Respir Med. 1998;92(3):401–7.
Vidal S, Bellido-Casado J, Granel C, Crespo A, Plaza V, Juárez C. Flow cytometry analysis of leukocytes in induced sputum from asthmatic patients. Immunobiology. 2012;217(7):692–7.
Sibila O, Garcia-Bellmunt L, Giner J, Rodrigo-Troyano A, Suarez-Cuartin G, Torrego A, et al. Airway Mucin 2 is decreased in patients with severe chronic obstructive pulmonary disease with bacterial colonization. Ann Am Thorac Soc. 2016;13(5):636–42.
Cabello H, Torres A, Celis R, El-Ebiary M. Puig de la Bellacasa J, Xaubet a, et al. bacterial colonization of distal airways in healthy subjects and chronic lung disease: a bronchoscopic study. Eur Respir J. 1997;10(5):1137–44.
Furuhashi M. Fatty acid-binding protein 4 in cardiovascular and metabolic diseases. J Atheroscler Thromb. 2019;26(3):216–32.
Wu G, Yang L, Xu Y, Jiang X, Jiang X, Huang L, et al. FABP4 induces asthmatic airway epithelial barrier dysfunction via ROS-activated FoxM1. Biochem Biophys Res Commun. 2018;495(1):1432–9.
Shum BOV, Mackay CR, Gorgun CZ, Frost MJ, Kumar RK, Hotamisligil GS, et al. The adipocyte fatty acid-binding protein aP2 is required in allergic airway inflammation. J Clin Invest. 2006;116(8):2183–92.
Ge XN, Bastan I, Dileepan M, Greenberg Y, Ha SG, Steen KA, et al. FABP4 regulates eosinophil recruitment and activation in allergic airway inflammation. Am J Physiol Cell Mol Physiol. 2018;315(2):L227–40.
Zhang X, Li D, Wang H, Pang C, Wu Y, Wen F. Gender difference in plasma fatty-acid-binding protein 4 levels in patients with chronic obstructive pulmonary disease. Biosci Rep. 2016;36(1):e00302.
Terra X, Quintero Y, Auguet T, Porras JA, Hernández M, Sabench F, et al. FABP 4 is associated with inflammatory markers and metabolic syndrome in morbidly obese women. Eur J Endocrinol. 2011;164(4):539–47.
Kralisch S, Fasshauer M. Adipocyte fatty acid binding protein: a novel adipokine involved in the pathogenesis of metabolic and vascular disease? Diabetologia. 2013;56(1):10–21.
Makowski L, Brittingham KC, Reynolds JM, Suttles J, Hotamisligil GS. The fatty acid-binding protein, aP2, coordinates macrophage cholesterol trafficking and inflammatory activity. J Biol Chem. 2005;280(13):12888–95.
Persson LJP, Aanerud M, Hardie JA, Miodini Nilsen R, Bakke PS, Eagan TM, et al. Antimicrobial peptide levels are linked to airway inflammation, bacterial colonisation and exacerbations in chronic obstructive pulmonary disease. Eur Respir J. 2017;49(3):1601328.
Millares L, Marin A, Garcia-Aymerich J, Sauleda J, Belda J, Monsó E, et al. Specific IgA and metalloproteinase activity in bronchial secretions from stable chronic obstructive pulmonary disease patients colonized by Haemophilus influenzae. Respir Res. 2012;13:113.
Hiemstra PS. Altered macrophage function in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10(Suppl):S180–5.
Shaykhiev R, Krause A, Salit J, Strulovici-Barel Y, Harvey B-G, O’Connor TP, et al. Smoking-dependent reprogramming of alveolar macrophage polarization: implication for pathogenesis of chronic obstructive pulmonary disease. J Immunol. 2009;183(4):2867–83.
Hodge S, Hodge G, Scicchitano R, Reynolds PN, Holmes M. Alveolar macrophages from subjects with chronic obstructive pulmonary disease are deficient in their ability to phagocytose apoptotic airway epithelial cells. Immunol Cell Biol. 2003;81(4):289–96.
Berenson CS, Garlipp MA, Grove LJ, Maloney J, Sethi S. Impaired phagocytosis of Nontypeable Haemophilus influenzae by human alveolar macrophages in chronic obstructive pulmonary disease. J Infect Dis. 2006;194(10):1375–84.
Acknowledgments
Authors thank all participants in the study for the willingness to contribute to medical research, and all field workers of the different participating centers for their dedication and quality of their daily work.
Funding
This study is supported by Fundació Ramon Pla i Armengol, Instituto de Salud Carlos III, Fondos FEDER (PI15/02042, PI15/00167 and PI18/00311). RF is recipient of a MS research contract (CP16/000039). OS is supported by PERIS.
Author information
Authors and Affiliations
Contributions
Study design: OS, SV, AA, RF and EM. Patient recruitment and data collection: OS, AR, MD, JG, FS, JV, SQ, MG, AM, RF. Performed experiments and sample processing: LP, AR, EC, SV. Writing the manuscript: LP, OS, SV, AA, EM. Revising of the manuscript and approval of submission: all authors. Responsible for the overall content as guarantor: OS.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the local institutional review board (IIBSP-MIC-2015-57) and all subjects gave signed informed consent.
Consent for publication
Obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Perea, L., Rodrigo-Troyano, A., Cantó, E. et al. Reduced airway levels of fatty-acid binding protein 4 in COPD: relationship with airway infection and disease severity. Respir Res 21, 21 (2020). https://doi.org/10.1186/s12931-020-1278-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-020-1278-5