Abstract
Background
The effects of triple therapy on gas trapping in COPD are not fully understood. We evaluated the effects of the long acting bronchodilator components of the extrafine single inhaler triple therapy beclometasone dipropionate/formoterol/glycopyrronium (BDP/F/G) pMDI on gas trapping.
Methods
This open-label, randomised, single centre, 2-way cross-over study recruited 23 COPD patients taking inhaled corticosteroid combination treatments and with residual volume (RV) > 120% predicted at screening. Inhaled BDP was taken during run-in and washout periods. Baseline lung function (spirometry, lung volumes, oscillometry) was measured over 12 h prior to randomisation to BDP/F/G or BDP/F for 5 days followed by washout and crossover. Lung function was measured prior to dosing on day 1 and for 12 h post-dose on day 5.
Results
Co-primary endpoint analysis: BDP/F/G had a greater effect than BDP/F on FEV1 area under the curve over 12 h (AUC0–12) (mean difference 104 mls, p = 0.0071) and RV AUC0–12 (mean difference − 163 mls, p = 0.0028). Oscillometry measurements showed a greater effect of BDP/F/G on the difference between resistance at 5 and 20 Hz (R5–R20) AUC0–12, which measures small airway resistance (mean difference − 0.045 kPa/L/s, p = 0.0002). Comparison of BDP/F with the baseline measurements (BDP alone) showed that F increased FEV1 AUC0–12 (mean difference 227 mls) and improved RV AUC0–12 (mean difference − 558 mls) and R5–R20 AUC0–12 (mean difference − 0.117 kPa/L/s), all p < 0.0001.
Conclusions
In COPD patients with hyperinflation, the G and F components of extrafine BDP/F/G improved FEV1, RV and small airway function. These long acting bronchodilators target small airway function, thereby improving gas trapping and airflow.
Trial registration The study was retrospectively registered at ClinicalTrials.gov on 15th February 2019 (No.: NCT03842904, https://clinicaltrials.gov/ct2/show/NCT03842904).
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) is characterised by persistent inflammation in the small airways, associated with remodelling and ultimately small airway destruction [1, 2]. These pathological changes reduce airflow and increase gas trapping [3]. Inhaled treatment with a long acting beta-agonist (LABA) and/or a long acting muscarinic antagonist (LAMA) can bronchodilate the small airways to improve airflow, reduce air trapping and thereby improve dyspnoea and exercise capacity [4,5,6,7]. Inhaled corticosteroid (ICS) treatment can target small airway inflammation to improve clinical outcomes including exacerbation rates [8].
The triple combination inhaler containing beclometasone dipropionate/formoterol/glycopyrronium (BDP/F/G) was developed as an extrafine formulation to enable efficient delivery of an ICS combined with a LABA and a LAMA to the small airways [9]. Phase 3 clinical trials have shown that this single inhaler triple therapy reduces exacerbation rates, and improves quality of life and lung function compared to double combination inhalers containing ICS/LABA or LAMA/LABA, and compared to LAMA monotherapy [10,11,12].
In order to further understand the effects of the bronchodilator components of extrafine BDP/F/G on the small airways and gas trapping, we conducted a clinical trial focusing on lung volumes and small airway physiology. To measure effects on gas trapping, we recruited patients with increased residual volume (RV) at study entry. The TRIFLOW study was a randomised, cross-over study evaluating the effects of the F and G components of BDP/F/G on lung volumes and small airway physiology (using oscillometry).
Methods
Participants
This study recruited male and female COPD patients from 40 to 75 years of age, with a post-bronchodilator forced expired volume in 1 s (FEV1) of 30–80% predicted, a FEV1/forced vital capacity (FVC) ratio of < 0.70, and a RV > 120% predicted. Eligible patients were current or ex-smokers with a smoking history of ≥ 10 pack years. All patients were required to be currently taking ICS as part of treatment with ICS/LABA or ICS/LABA/LAMA (as separate inhalers or a single inhaler). Patients were excluded using the following criteria: known respiratory disorder other than COPD; COPD exacerbation within 8 weeks or hospitalisation within 12 months due to COPD; or abnormal clinically relevant findings on physical examination, laboratory or electrocardiogram (ECG) evaluations that in the investigator`s opinion made it unsafe for the patient to participate. All patients provided written informed consent using a protocol approved by the Health & Social Care Research Ethics Committee A (18/NI/0194).
Study design
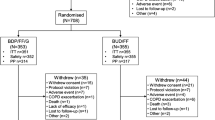
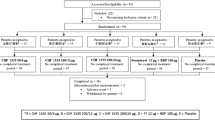
The study was a randomised, open label, 2 way cross over design (ClinicalTrials.gov registration: NCT03842904). Eligible patients commenced a 10–28 day run-in period receiving BDP (Clenil Modulite) 200 µg twice daily in place of current ICS treatment. Long acting bronchodilator treatments were withdrawn, and replaced with short acting bronchodilators for use as needed. After ≥ 10 days of run-in, a baseline visit was completed, followed by two treatment periods of 5 days each, separated by a washout period of 7–21 days during which BDP and short acting bronchodilators were used (Fig. 1). Patients were randomised (with a 1:1 ratio), to receive triple therapy (Trimbow: BDP/F/G, 100/6/10 µg pMDI, 2 puffs, twice daily) followed by dual therapy (Fostair: BDP/F, 100/6 µg pMDI, 2 puffs, twice daily) or vice-versa. BDP/F/G or BDP/F treatment was commenced on the morning of day 1 and a final dose given on the morning of day 5 (total of 9 doses).
At the baseline visit, and on day 5 of each treatment period, impulse oscillometry (IOS), spirometry, and whole body plethysmography were performed (in that order) prior to the morning dose. IOS and spirometry were then repeated 30 min and 1, 2, 4, 6, 8, 10 and 12 h post-dose. Plethysmography was repeated at 1, 2, 4, 8 and 12 h post-dose. On day 1 of each treatment period, patients performed spirometry, IOS, and whole body plethysmography prior to the first administration of BDP/F/G or BDP/F.
Lung function
IOS was performed on the IOS Masterscreen system (Erich Jaeger, Hoechberg, Germany), to European Respiratory Society (ERS) standards [13]. Acceptable tests had a coherence index of ≥ 0.7 for both 5 and 20 Hz, and the average values reported from three tests where R5, R20 and Fres values were within 10% of their respective mean values. Spirometry was performed on the NDD Easy On-PC system (NDD medical technologies, Zurich, Switzerland), to American Thoracic Society (ATS)/ERS standards [14]. Predicted values were calculated using the global lung function initiative (GLI) 2012 equations [15]. Whole body plethysmography was performed on the Vmax Encore system (CareFusion, Hoechberg, Germany), to ATS/ERS standards [16]. Thoracic gas volume (TGV) was quantified for three acceptable tests, where the associated functional residual capacity (FRC) values were within 5% of the mean value. Vital capacity (VC) manoeuvres were then performed in triplicate to ascertain residual volume (RV) and total lung capacity (TLC), where the highest two VC values agreed within 150 mls. Predicted values were calculated using the ERS 1993 equations [17]. The following measurements were collected: FEV1; forced vital capacity (FVC); mid-expiratory flow (FEF25–75%); RV; TLC; FRC; inspiratory capacity (IC); specific airway conductance (sGaw); airway resistance (Raw); peripheral respiratory resistance (R5–R20); expiratory flow limitation (∆X5); total respiratory resistance (R5); reactance (X5); resonance frequency (Fres); reactance area (AX);
Statistical methods
The co-primary objectives were to compare the effects of BDP/F/G versus BDP/F on change in FEV1 and RV on day 5 compared to day 1 pre-dose, by analysing area under the curve over 12 h (AUC0–12). The secondary objectives were to compare the effect of BDP/F/G versus BDP/F on change in all other lung function measurements for AUC0–12 and peak, while treatment differences for FEV1 and RV peak and trough (12 h post-dose) were also determined. Additionally, the differences between AUC0–12 for BDP/F/G and BDP/F at day 5 were compared to the AUC0–12 for BDP alone at baseline visit (relative to baseline visit pre-dose value). A sample size of 20 patients was required to detect a mean difference > 0.23 L (FEV1 AUC0–12) between treatments. This corresponds to a 2-sided t-test with 80% power conducted at the 5% significance level, assuming a standard deviation of 0.17 L for the paired differences between treatment groups. The primary analysis was conducted using a mixed model. The model included fixed effects for treatment and period and a random effect for patient within treatment sequence. For the primary endpoint, the AUC0–12 from the baseline visit was included as a covariate. The AUC0–12 (normalised by time), peak and trough (defined as the 12 h measurement post-dose on day 5) values were analysed as change from within-period day 1 pre-dose measurement. All were analysed without any procedures to account for multiple comparisons.
Results
Participants
Sixty-six patients were screened, with 23 randomised, as shown in Fig. 2. One patient was withdrawn due to lack of treatment compliance, leaving 22 patients analysed. Patient characteristics are shown in Table 1. The mean FEV1% predicted (post-bronchodilator) was 49%, and RV was 152% predicted.
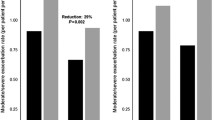
Primary endpoints
Both BDP/F/G and BDP/F caused improvements in FEV1 and RV on day 5 compared to day 1 pre-dose (Figs. 3, 4). The FEV1 AUC0–12 change with BDP/F/G was greater compared to BDP/F; mean difference 104 mls; 95% CI 37, 171 mls; p = 0.0071. RV AUC0–12 change was greater with BDP/F/G compared to BDP/F; mean difference − 163 mls; 95% CI − 263, − 64 mls; p = 0.0028.
Secondary endpoints
BDP/F/G versus BDP/F
BDP/F/G caused larger improvements than BDP/F for most of the lung function AUC0–12 parameters (Table 2). Using IOS, the change in small airway resistance, measured by R5–R20 AUC0–12, was greater with BDP/F/G compared to BDP/F (mean difference − 0.045 kPa/L/s; p = 0.0002). There were also significantly greater treatment differences in favour of BDP/F/G for Fres, AX and X5, while ∆X5 failed to reach statistical significance (p = 0.06). IC, TLC and FRC AUC0–12 measurements did not show statistically significant differences between treatments, although TLC and FRC showed numerical changes in favour of BDP/F/G. sGaw AUC0–12 change was greater with BDP/F/G (p = 0.01).
Change in peak FEV1 was greater for BDP/F/G versus BDP/F (mean difference 120 mls; p = 0.0016), while for peak RV the difference was not significant (mean difference − 79 mls; p = 0.11). Other peak lung function results are shown in the Additional File 1; R5–R20 peak change with BDP/F/G was greater compared to BDP/F (mean difference − 0.036 kPa/L/s; p = 0.0022), while there were also significant differences for Fres, AX and X5, but not ∆X5. Lung volume peak measurements did not show statistically significant differences between treatments, while sGaw changes were in favour of BDP/F/G.
Trough RV improvement was greater for BDP/F/G compared with BDP/F, (− 179 mls; p = 0.0097), while the treatment difference for trough FEV1 (65 mls; p = 0.08) did not reach statistical significance (see Additional File 1).
BDP/F/G and BDP/F change from baseline
The baseline AUC0–12 measurements were performed while patients were taking BDP alone. The differences between baseline measurements and BDP/F/G or BDP/F treatments (day 5) are shown in Table 3. The comparisons of BDP/F with the baseline measurements showed differences in FEV1 AUC0–12 (mean difference 227 mls), RV AUC0–12 (mean difference − 558 mls) and R5–R20 AUC0–12 (mean difference − 0.117 kPa/L/s), all p < 0.0001. The comparisons of BDP/F/G with the baseline measurements showed differences in FEV1 AUC0–12 (mean difference 320 mls), RV AUC0–12 (mean difference − 678 mls) and R5–R20 AUC0–12 (mean difference − 0.165 kPa/L/s), all p < 0.0001.
Safety
There were no serious AEs (adverse events) leading to withdrawal from the study or discontinuation of treatment. Further safety information is described in the Additional File 1.
Discussion
This study focused on COPD patients with evidence of gas trapping, measured by RV. For the primary endpoint analysis (AUC0–12), BDP/F/G had greater effects compared to BDP/F on FEV1 and RV (mean treatment differences; 104 mls and − 163 mls respectively). This demonstrates that the G component of extrafine BDP/F/G reduced gas trapping in COPD patients. Furthermore, the greater improvement in R5–R20 AUC0–12 for BDP/F/G compared to BDP/F demonstrates that G also reduced small airway resistance. Overall, these results indicate that G had a beneficial effect on small airway physiology leading to improvements in gas trapping.
A secondary analysis, comparing BDP/F versus BDP, showed that F improved FEV1, RV and IOS measurements including R5–R20 AUC0–12. This demonstrates benefits of F on small airway physiology which are associated with decreases in gas trapping. The effect sizes observed showed that F treatment for 5 days caused 558 mls improvement in RV AUC0–12 and a 227 mls improvement in FEV1 AUC0–12. This comparison to baseline analysis also showed the extra benefit of the addition of G for 5 days, as BDP/F/G versus BDP treatment differences were 678 mls for RV AUC0–12 and 320 mls for FEV1 AUC0–12. Overall, these results indicate a greater effect of the addition of the first bronchodilator (BDP/F versus BDP) than the addition of the second bronchodilator (BDP/F/G versus BDP/F). This smaller effect of the second bronchodilator has been observed in many previous studies [5, 18, 19], and may be due to reaching near to the maximum improvement that may be achieved with these bronchodilator drug classes.
The primary and secondary outcomes, describing improvements in different components of lung mechanics, provide insights into the physiological effects of the long acting bronchodilators within BDP/F/G. Gas trapping is associated with an increased burden of symptoms in COPD [20, 21], and pharmacological interventions to reduce gas trapping can improve exercise performance [22, 23]. The primary endpoint analysis showed that using BDP/F/G can reduce gas trapping to a greater degree compared to BDP/F. This physiological effect may be extremely useful in clinical practice, in order to optimise the reduction of gas trapping and hence associated symptoms. The short treatment duration, and limited sample size of the current study means that we could not properly assess changes in symptoms or exercise capacity. Nevertheless, the TRILOGY phase 3 study, conducted over one year, provided evidence of greater improvements at many of the time-points for symptoms and quality of life for treatment with BDP/F/G compared to BDP/F [10].
The peak lung function changes on day 5 (for the comparison of BDP/F/G versus BDP/F) followed the same pattern of results as AUC0–12, except RV showed a lower numerical difference (65 mls) that was not statistically significant (p = 0.08). This might be due to the reduction in gas trapping by the first bronchodilator (F) being relatively large at peak, leaving little room for improvement by the addition of the second bronchodilator (G). For both the AUC0–12 and peak measurements, RV had the greatest sensitivity out of all the lung volume measurements to measure differences between BDP/F/G versus BDP/F; this is likely related to the enrichment of the study population for individuals with RV > 120% predicted at screening.
Using IOS allowed measurements of airway resistance and reactance to be collected. R5–R20 is a well accepted measurement of small airway resistance, and previous papers have shown that bronchodilators improve R5–R20 in COPD patients [4, 24]. In this study, the concurrent improvements in R5–R20 and RV imply that bronchodilator related improvements in small airway function enabled reduced gas trapping. IOS reactance measurements (X5, Fres, AX) reflect lung compliance and elasticity, and here we observed consistent improvements in these parameters for the G and F components of extrafine triple therapy.
Small airway closure can prevent low frequency oscillometric signals from reaching the distal lung [7]. Small airway closure can therefore operate as regional “choke points” during expiration but not inspiration, which has been called expiratory flow limitation (EFL). This can cause marked differences in reactance measurements during tidal breathing, and is measured by ∆X5, which is an oscillometry measurement of EFL. It has been reported that EFL measurements are associated with greater airflow limitation and gas trapping, greater symptoms, more exacerbations and increased mortality [21, 25, 26]. The comparisons of BDP/F/G or BDP/F versus BDP (baseline) both showed large improvements in ∆X5, and consequently the BDP/F/G versus BDP/F comparison yielded a small treatment difference that was not statistically significant.
The design of the study, using the same inhaler device delivering extrafine formulations for all treatments, allowed the contributions of F and G on small airway function and gas trapping to be determined. We did not study a non-extrafine formulation with less peripheral lung deposition compared to BDP/F/G; this would be an interesting future study to compare changes in small airway function and gas trapping between treatments. While this was an open study, the objective nature of the endpoints (lung function measurements) restricted any bias that could be introduced by lack of treatment blinding. The main advantage of blinding is for patient reported outcomes which are more subjective. A potential limitation of the study was the relatively small sample size. However, the sample size was very similar to other crossover design studies investigating long acting bronchodilator effects on lung function [27, 28], and the enrichment for individuals with gas trapping (RV > 120% predicted) increased the homogeneity of the population thereby decreasing the potential variability in lung function data.
The mean CAT score at screening was 19.6, suggesting this was a very symptomatic population. However, 13 out of the 22 patients had mMRC scores < 2 at study entry. The majority of patients (20 out of 22) were already receiving triple therapy in real life at study entry, which likely reduced the burden of dyspnoea. The differences between CAT and mMRC scores likely reflect the broader range of disease components assessed by the former, as previously reported [29]. All patients were using ICS at study entry; these drugs should be used in patients with a history of exacerbations [30], but often are inappropriately given to patients who do not have a history of exacerbations. While some of our study population had no exacerbations in the last year, this may reflect a positive treatment response to ICS initiation [31].
Late phase studies with large sample sizes often require statistical approaches to account for multiple testing. This smaller study was more exploratory in nature, providing information on the usefulness of a broad range of lung function tests. This information can be used to select the most appropriate tests to be used in future studies comparing inhaled treatments. Multiple testing correction is often not performed in smaller clinical trials with a more exploratory nature [32]. Nevertheless, many of the p values reported were highly significant, arguing against the presence of false positives due to multiple testing.
In summary, this study focused on COPD patients with gas trapping, and demonstrated that the G and F components of extrafine BDP/F/G improved FEV1, RV and small airway function. It can be concluded that these long acting bronchodilators target small airway function, thereby improving gas trapping and airflow.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BDP:
-
Beclometasone dipropionate
- F:
-
Formoterol
- G:
-
Glycopyrronium
- COPD:
-
Chronic obstructive pulmonary disease
- ICS:
-
Inhaled corticosteroid
- LABA:
-
Long acting beta-agonist
- LAMA:
-
Long acting muscarinic antagonist
- ECG:
-
Electrocardiogram
- pMDI:
-
Pressurised metered dose inhaler
- IOS:
-
Impulse oscillometry
- CAT:
-
COPD assessment test
- mMRC:
-
Modified medical research council
- FEV1 :
-
Forced expired volume in 1 s
- AUC0–12 :
-
Area under the curve over 12 h
- FVC:
-
Forced vital capacity
- FEF25–75%:
-
Forced expiratory flow between 25 and 75% of FVC
- sGaw:
-
Specific airway conductance
- Raw:
-
Airway resistance
- RV:
-
Residual volume
- IC:
-
Inspiratory capacity
- FRC:
-
Functional residual capacity
- TLC:
-
Total lung capacity
- R5:
-
Total respiratory resistance
- R20:
-
Central respiratory resistance
- R5–R20:
-
Peripheral respiratory resistance
- X5:
-
Respiratory reactance
- ∆X5:
-
Expiratory flow limitation
- Fres :
-
Resonance frequency
- AX:
-
Reactance area
- CI:
-
Confidence interval
- AEs:
-
Adverse events
- EFL:
-
Expiratory flow limitation
References
Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu L, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(26):2645–53.
Higham A, Quinn AM, Cancado JED, Singh D. The pathology of small airways disease in COPD: historical aspects and future directions. Respir Res. 2019;20(1):49.
Singh D, Long G, Cancado JED, Higham A. Small airway disease in chronic obstructive pulmonary disease: insights and implications for the clinician. Curr Opin Pulm Med. 2020;26(2):162–8.
Borrill ZL, Houghton CM, Tal-Singer R, Vessey SR, Faiferman I, Langley SJ, et al. The use of plethysmography and oscillometry to compare long-acting bronchodilators in patients with COPD. Br J Clin Pharmacol. 2008;65(2):244–52.
Singh D. New combination bronchodilators for chronic obstructive pulmonary disease: current evidence and future perspectives. Br J Clin Pharmacol. 2015;79(5):695–708.
Tashkin DP, Celli B, Senn S, Burkhart D, Kesten S, Menjoge S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–54.
Maltais F, O’Donnell D, Galdiz Iturri JB, Kirsten AM, Singh D, Hamilton A, et al. Effect of 12 weeks of once-daily tiotropium/olodaterol on exercise endurance during constant work-rate cycling and endurance shuttle walking in chronic obstructive pulmonary disease. Ther Adv Respir Dis. 2018;12:1753465818755091.
Singh D, Corradi M, Spinola M, Petruzzelli S, Papi A. Extrafine beclometasone diproprionate/formoterol fumarate: a review of its effects in chronic obstructive pulmonary disease. NPJ Prim Care Respir Med. 2016;26:16030.
Singh D, Corradi M, Spinola M, Papi A, Usmani OS, Scuri M, et al. Triple therapy in COPD: new evidence with the extrafine fixed combination of beclomethasone dipropionate, formoterol fumarate, and glycopyrronium bromide. Int J Chron Obstruct Pulmon Dis. 2017;12:2917–28.
Singh D, Papi A, Corradi M, Pavlisova I, Montagna I, Francisco C, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting beta2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388(10048):963–73.
Papi A, Vestbo J, Fabbri L, Corradi M, Prunier H, Cohuet G, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–84.
Vestbo J, Papi A, Corradi M, Blazhko V, Montagna I, Francisco C, et al. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomised controlled trial. Lancet. 2017;389(10082):1919–29.
Oostveen E, MacLeod D, Lorino H, Farre R, Hantos Z, Desager K, et al. The forced oscillation technique in clinical practice: methodology, recommendations and future developments. Eur Respir J. 2003;22(6):1026–41.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38.
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–43.
Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–22.
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Report working party standardization of lung function tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl. 1993;16:5–40.
Bateman ED, Chapman KR, Singh D, D’Urzo AD, Molins E, Leselbaum A, et al. Aclidinium bromide and formoterol fumarate as a fixed-dose combination in COPD: pooled analysis of symptoms and exacerbations from two six-month, multicentre, randomised studies (ACLIFORM and AUGMENT). Respir Res. 2015;16:92.
Singh D, Roche N, Halpin D, Agusti A, Wedzicha JA, Martinez FJ. Current controversies in the pharmacological treatment of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2016;194(5):541–9.
Cooper CB. The connection between chronic obstructive pulmonary disease symptoms and hyperinflation and its impact on exercise and function. Am J Med. 2006;119(10 Suppl 1):21–31.
Dean J, Kolsum U, Hitchen P, Gupta V, Singh D. Clinical characteristics of COPD patients with tidal expiratory flow limitation. Int J Chron Obstruct Pulmon Dis. 2017;12:1503–6.
Beeh KM, Singh D, Di Scala L, Drollmann A. Once-daily NVA237 improves exercise tolerance from the first dose in patients with COPD: the GLOW3 trial. Int J Chron Obstruct Pulmon Dis. 2012;7:503–13.
O’Donnell DE, Fluge T, Gerken F, Hamilton A, Webb K, Aguilaniu B, et al. Effects of tiotropium on lung hyperinflation, dyspnoea and exercise tolerance in COPD. Eur Respir J. 2004;23(6):832–40.
Borrill ZL, Houghton CM, Woodcock AA, Vestbo J, Singh D. Measuring bronchodilation in COPD clinical trials. Br J Clin Pharmacol. 2005;59(4):379–84.
Aarli BB, Calverley PM, Jensen RL, Eagan TM, Bakke PS, Hardie JA. Variability of within-breath reactance in COPD patients and its association with dyspnoea. Eur Respir J. 2015;45(3):625–34.
Aarli BB, Calverley PM, Jensen RL, Dellaca R, Eagan TM, Bakke PS, et al. The association of tidal EFL with exercise performance, exacerbations, and death in COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2179–88.
Leaker BR, Barnes PJ, Jones CR, Tutuncu A, Singh D. Efficacy and safety of nebulized glycopyrrolate for administration using a high efficiency nebulizer in patients with chronic obstructive pulmonary disease. Br J Clin Pharmacol. 2015;79(3):492–500.
Singh D, Scuri M, Collarini S, Vezzoli S, Mariotti F, Muraro A, et al. Bronchodilator efficacy of extrafine glycopyrronium bromide: the Glyco 2 study. Int J Chron Obstruct Pulmon Dis. 2017;12:2001–14.
Kim S, Oh J, Kim YI, Ban HJ, Kwon YS, Oh IJ, et al. Differences in classification of COPD group using COPD assessment test (CAT) or modified Medical Research Council (mMRC) dyspnea scores: a cross-sectional analyses. BMC Pulm Med. 2013;13:35.
Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):190064.
Singh D, Barnes PJ, Stockley R, Lopez Valera MV, Vogelmeier C, Agusti A. Pharmacological treatment of COPD: the devil is always in the detail. Eur Respir J. 2018;51(4):1800263.
Singh D, Balaguer V, Astbury C, Wahlby-Hamren U, Jimenez E, Seoane B, et al. Navafenterol (AZD8871) in patients with COPD: a randomized, double-blind, phase I study evaluating safety and pharmacodynamics of single doses of this novel, inhaled, long-acting, dual-pharmacology bronchodilator. Respir Res. 2020;21(Suppl 1):102.
Acknowledgements
Statistical testing was performed by Synequanon, Diss, UK.
Funding
The study was supported by Chiesi Ltd, Manchester, UK.
Author information
Authors and Affiliations
Contributions
DS and NK were major contributors to study design. All authors contributed to the collection and analysis of the patient data. DS interpreted the patient data. JD, CP and DS were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients provided written informed consent using a protocol approved by the Health & Social Care Research Ethics Committee A (18/NI/0194).
Consent for publication
Not applicable.
Competing interests
JD; The author declares that they have no competing interests. CP; The author declares that they have no competing interests. NK; The author declares that they have no competing interests. DS has received sponsorship to attend international meetings, honoraria for lecturing or attending advisory boards and research grants from various pharmaceutical companies including AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Genentech, GlaxoSmithKline, Glenmark, Gossamerbio, Menarini, Mundipharma, Novartis, Peptinnovate, Pfizer, Pulmatrix, Therevance and Verona.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Triflow Supplement.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dean, J., Panainte, C., Khan, N. et al. The TRIFLOW study: a randomised, cross-over study evaluating the effects of extrafine beclometasone/formoterol/glycopyrronium on gas trapping in COPD. Respir Res 21, 323 (2020). https://doi.org/10.1186/s12931-020-01589-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-020-01589-5