Abstract
Background
Previous studies have implicated inherited mutations in mitochondrial DNA (mtDNA) in sensorineural hearing loss (SNHL). However, the definitive association between mitochondrial 12S rRNA (MT-RNR1) variants and hearing loss in the population has not been well established, particularly in Asia. The objective of this retrospective cohort study was to assess the association between MT-RNR1 variants and the risk of SNHL in patients in Taiwan.
Methods
The cohort included 306,068 participants from Taiwan between January 2003 and December 2020. Participants were classified based on genetic variants, particularly mitochondrial mutations (rs267606618, rs267606619, rs267606617). MT-RNR1 variant cases were matched 1:10 with non-mutant patients by age, gender, and visit year, excluding those with pre-existing hearing loss. The primary endpoint was SNHL, identified using specific ICD-TM codes with a 90% positive predictive value. Medication exposure history was determined via self-report or electronic medical records in the hospital. Cox proportional hazard regression models were used to assess the association between MT-RNR1 variants and hearing loss, adjusting for various covariates. Kaplan-Meier survival curves and log-rank tests compared hearing loss incidence between groups.
Results
The mean age of the mtDNA variants group is 32.4 years, with a standard deviation of 19.2 years. The incidence density of hearing loss for the mutation group was 36.42 per 10,000 person-years (95% Confidence Interval [CI], 27.21–47.73), which was higher than the 23.77per 10,000 person-years (95% CI, 21.32–26.42) in the wild-type group (p = 0.0036). Additionally, diabetes mellitus was associated with an increased risk of developing SNHL in individuals with MT-RNR1 variants (adjusted hazard ratio = 1.76 [95% CI, 1.00-3.09], p < 0.05).
Conclusion
This study highlights the increased risk of hearing loss in patients carrying MT-RNR1 variants, particularly those with diabetes mellitus. Future research that integrates genetic and clinical data is crucial for developing more precise interventions to monitor and treat hearing loss in this vulnerable population.
Similar content being viewed by others
Introduction
Hearing impairment is one of the most common sensory deficits in human beings. It is estimated that nearly 5% of the global population suffers from hearing loss, affecting individuals across all age groups [1]. Hearing loss is more than just a sensory deficit; it fundamentally alters the way individuals connect with their surroundings and with others. From a medical perspective, the inability to hear can induce social deprivation or culminate in secondary health implications, such as depression, dementia [2, 3]. In addition to personal health issues, hearing loss has significant socioeconomically ramifications. Those with hearing impairment, their contribution in the workforce and productivity can decline [4]. Therefore, it is crucial to thoroughly understand the causes and processes of hearing loss. Such knowledge is important to crafting some prevention or treatment strategies, benefiting both individuals and the broader community.
Multiple factors can contribute to the development of sensorineural hearing loss (SNHL), including infectious or toxic causes, metabolic abnormalities, noise exposure, aging, diseases of ear, trauma, and genetic factors [5]. Genetic factors may account for up to half of cases of hereditary hearing impairment [6]. Among genetic causes of hearing loss, 30% are syndromic, featuring associated physical issues, whereas 70% are non-syndromic. In non-syndromic cases, autosomal recessive forms predominate, comprising 75–80% of cases, autosomal dominant forms make up about 20%, and X-linked, Y-linked, and mitochondrial inheritance collectively represent the remaining 5% [7]. Among the array of genes identified for non-syndromic hearing impairment to date, GJB2, SLC26A4, and the mitochondrial 12S rRNA (MT-RNR1) gene are much more prevalent than others across different populations [8].
Moreover, inherited mutations in mitochondrial DNA (mtDNA) are predominantly inherited in a maternal manner [8, 9]. The mtDNA contains 37 genes: 13 for cellular respiration proteins, 22 for tRNAs, and 2 (MT-RNR1 and MT-RNR2) for rRNAs—MT-RNR1 codes for 12S rRNA and MT-RNR2 for 16 S rRNA [10]. The MT-RNR1 gene transcribes a specific mitochondrial-derived peptide (MDP) that has been reported to have beneficial effects on metabolic stress conditions such as obesity, insulin resistance, and type 2 diabetes [11]. Mutations in the mitochondrial 12S rRNA gene (MT-RNR1) are linked to both aminoglycoside-induced and nonsyndromic hearing loss. Particularly, the homoplasmic mutations 1555 A>G and 1494 C>T in MT-RNR1 are observed [12]. Given that cases of SNHL often involve a known history of aminoglycoside use, it is noteworthy that the m.1095 T>C mutation ranks as the third most prevalent among individuals of Chinese descent with SNHL who have been exposed to aminoglycosides [13, 14]. Despite these associations, there is considerable variability in the degree and onset of hearing loss, as well as different levels of penetrance, among families carrying these mutations [15]. The incidence of hearing impairment in patient with MT-RNR1 gene mutation remains lacking in real world data.
Considering the limited data on the penetrance of mtDNA hearing loss in Asian populations, this retrospective cohort study utilized local data to investigate the incidence of hearing impairment in patients carrying MT-RNR1 variants. These findings could have deep implications for clinical decision-making related to gene variants and healthcare practices within the local community. Hence, this study was performed to explore the association between MT-RNR1 gene mutations and the risk of hearing impairment in the Taiwanese adult patients.
Methods
Data source
In this retrospective cohort study, we analyzed data from the China Medical University Hospital (CMUH) database from January 1, 2003, to December 31, 2020. The research was approved by the Ethics Review Board of China Medical University (CMUH111-REC1-176) and adhered to the (Strengthening the Reporting of Observational Studies in Epidemiology) STROBE reporting guidelines. Data analysis was conducted between February 1 and July 31, 2023. For an investigation into the sensorineural hearing loss (SNHL) risk associated with mitochondrial gene mutations, we employed an in-house genetic database, which stands as the most extensive and representative genetic repository in Taiwan. We gathered hearing loss data from the CMUH between January 2003 and December 2020, which offers a diverse range of health data, from clinical records to genetic details. Further information on CMUH database is available in prior research [16].
Study design and participants
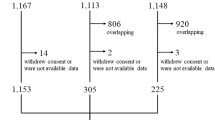
This cohort study was conducted in Taiwan, including a population of 306,068 participants from CMUH. We classified the participants based on genetic variants to evaluate their risk of hearing loss and associated health conditions. To ensure consistency in the study, we included individuals of all ages from Taiwan carrying mitochondrial gene mutations with high prevalence in Asia (rs267606618, rs267606619, and rs267606617) as variant cases. We also ensured the availability of DNA records, the presence of MT-RNR1 variants, and the provision of informed consent. MT-RNR1 variant cases and non-mutant patients were matched in a 1:10 ratio in terms of age, gender, and visit year. We also excluded individuals with pre-existing hearing loss to ensure that both groups were healthy at the time of study entry. The study addressed factors related to sensorineural hearing loss from January 2003 to December 2020. The primary endpoint was the identification of sensorineural hearing loss, determined through specific ICD-9-CM and ICD-10-CM codes with a 90% positive predictive value, supported by a requirement of three occurrences. (See supplementary Table S4, Additional file 4).
Mitochondrial 12 S rRNA variants and deletion analysis
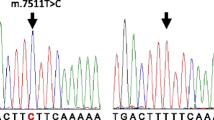
Our analysis utilized single nucleotide polymorphism (SNP) arrays from the Taiwan Precision Medicine Initiative (TPMI). The TPMv1 Array plate, based in Santa Clara, CA, USA, comprised 714,461 probesets. Genotype calling was facilitated by Affymetrix® Power Tools (APT). The first phase of the analysis involves sample quality control (QC), where we introduce a statistic called Dish-QC to assess the signal across non-polymorphic loci. We retain samples with a Dish-QC greater than 82%. In the second phase, we identify genotyped samples with a call rate (CR) lower than a default value of 97% and exclude samples that fail to meet the CR criteria. Additionally, the average CR must exceed 98.5%. For detailed information, please refer to the manufacturer’s instructions. The overall sample pass rate must be above 95%. Ultimately, we only retain probes marked as ‘Best recommended’ across all probes. For all individuals, we analyze the SNP missing rate, keeping only those individuals with a missing rate less than 10%. After quality checks, 686,432 variants and 347,954 individuals were retained. Genotypes for Affx-91,439,596 (m.1095 T>C, rs267606618), Affx-98,506,994 (m.1494 C> T, rs267606619), and Affx-89,025,706 (m.1555 A>G, rs267606617) were derived from the Axiom-TPM array.
Stratification variables
Age was used as a primary stratification variable, grouped into 10-year intervals. We also stratified based on types of MT-RNR1 variants, aminoglycosides, loop diuretics, and comorbidities to assess varying risks of hearing loss. Medication exposure history was determined either via self-report or by referencing the electronic medical records from CMUH in Taiwan. Exposure to aminoglycoside antibiotics or loop diuretics was defined as a patient having received at least one prescription (See supplementary Table S3, Additional file 3), whether oral or injectable, within the specified period. These records contained encrypted personal medical and demographic information.
Statistical analysis
We examined the baseline characteristics and the prevalence of hearing loss among comparing groups with and without MT-RNR1 variants by using the Chi-square test or Fisher’s exact test for categorical variables and the Student’s t-test or Mann-Whitney U test for continuous variables. Additionally, the normality was assessed using the Shapiro-Wilk test. Using patients’ medical histories, available in the CMUH database since 2003, we obtained information on comorbidities that may represent shared risk factors for hearing loss. Individuals with SNHL were diagnosed at least three outpatient visits or one inpatient record, and the first and last outpatient visits were at least 90 days apart. To avoid immortal time bias, the third diagnosis was designated as the index date. Comorbidities and medication usage preceding this date were identified as potential risk factors for SNHL. A comorbidity was confirmed and identified via specific ICD-9-CM and ICD-10-CM codes (See supplementary Table S4, Additional file 4). if there were at least three outpatient visits or one inpatient record with the associated code within a year. These consisted of all hospital inpatient and outpatient diagnoses of chronic kidney disease, diabetes mellitus, hypertension, otitis media, and hyperlipidemia. Secondly, we assessed the longitudinal association between MT-RNR1 variants and the incidence of hearing loss by using Cox proportional hazard regression models with covariates including sex, age, the use of aminoglycoside or loop diuretics, and comorbidities (See supplementary Tables S3-S4, Additional file 3–4). Last, the Kaplan–Meier survival curve and log-rank test were applied to compare the incidence of hearing loss among groups with and without MT-RNR1 variants. The 95% confidence intervals (CIs) of incidence of hearing loss were then calculated assuming the events followed Poisson distribution. The statistical significance level for all tests was set at a 2-sided level of 0.05. All statistical analyses were performed in Python, version 3.10 (Python Software Foundation).
Results
In this cohort study, we analyzed data from 306,068 participants in Taiwan, utilizing the CMUH database. This was linked with the catastrophic illness database to confirm that the initial study population did not have hearing loss. We identified 1,179 individuals with MT-RNR1 variants, classifying them into the mtDNA variants group. The average age of the mtDNA variants group is 32.4 years, with a standard deviation of 19.2 years. Among this group, females comprise 46.6% (550 cases). Compared to the matched group with wild-type mtDNA, there were no significant differences in age, gender, or the incidence of comorbidities (Table 1). During the 20-year follow-up period, the subjects with mtDNA variants had a higher risk of developing SNHL compared with the non-mutation comparison group, with an incidence density of 36.42 per 10,000 person-years versus 23.77 per 10,000 person-years (Table 2). The adjusted hazard ratio (aHR) of mtDNA variants was 1.54 (95% CI, 1.15–2.06, p = 0.0036). In subgroup analysis stratified by age, a higher risk of developing SNHL was observed among individuals with mtDNA variants compared to their non-mutation counterparts in the age groups of 35–44 (n = 17, aHR = 2.52, 95% CI [1.47–4.32], p = 0.001) and 45–54 (n = 12, aHR = 1.9, 95% CI [1.03–3.54], p = 0.039). Figure 1 depicts Kaplan–Meier estimates of hearing loss-free survival curves, revealing a conspicuous probability of SNHL association between individuals mtDNA variants and those without mutation (log-rank test for trend: p = 0.004).
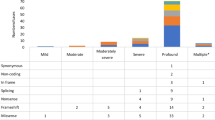
Table 3 shows the results of Cox proportional hazard regression models. Individuals with the m.1555 A>G variants exhibited a significant risk of developing SNHL (aHR = 1.97, 95% CI [1.35–2.86], p < 0.001), while no significant difference was found in those with m.1494 C>T variants (p = 0.443). Females with mtDNA variants have a higher risk of having SNHL compared to females without mutations. The aHR of mtDNA variants was 1.59 (95% CI, 1.06 − 2.38, p = 0.0262). The subjects with mtDNA variants who had diabetes mellitus had a higher risk of developing SNHL compared with the non-mutation counterparts, with an incidence density of 60.52 per 10,000 person-years versus 34.5 per 10,000 person- years. The aHR of mtDNA variants was 1.76 (95% CI, 1.00 − 3.09, p = 0.0499). No significant difference between two groups was observed in the risk of developing SNHL based on other comorbidities in our study. The association between the use of loop diuretic (p = 0.182) or aminoglycosides (p = 0.888) and risk of developing SNHL in individuals with mtDNA variants were not found to be significant.
Discussion
To our knowledge, this is the largest retrospective cohort study conducted in Asia, focusing on mtDNA allele mutations with the aim of examining the risk of hearing loss in patients with mtDNA variants. In our study, we observed that patients carrying MT-RNR1 variants exhibited a significantly lower rate of hearing preservation, particularly those with comorbidities, compared to a control group without these mutations.
Previous research has implicated inherited mtDNA mutations in both syndromic and nonsyndromic SNHL [12, 13, 15]. However, the extent to which post-lingual hearing loss and presbycusis are due to mtDNA mutations remains uncertain due to the potential for both inherent and acquired mutations [17]. In Taiwan, the common deafness-associated genes assessed, in order of prevalence included GJB2, SLC26A4, OTOF, MYO15A, and MT-RNR1 [18]. The mitochondrial m.1555 A>G mutation, has a reported prevalence of 0.1% in newborn screenings and accounts for 3.2% of Taiwanese families with idiopathic SNHL [15, 19, 20]. While mtDNA mutation is present in 5–10% of post-lingual hearing loss cases, significant ethnic variations exist [21]. The prevalence of the m.1555 A>G mutation in Taiwanese idiopathic SNHL patients is comparable to other populations [21,22,23,24], and varied penetrance of SNHL across different haplogroups suggests the mtDNA background influences disease expression [25, 26]. Moreover, modifiers such as aminoglycosides antibiotics and genetic factors can modulate the phenotypic manifestation of mtDNA mutations, underscoring the complexity of their role in hearing loss [27].
Our results support the observation that populations with mitochondrial gene variants exhibit a higher differential risk of hearing loss. This aligns with other studies, but our findings provide additional data that was still lacking for the Taiwanese Han general population [12, 18]. These findings also underscore the necessity of genetic testing for tailored hearing loss interventions, including treatment, rehabilitation, prognosis, and family planning [28]. During the 20-year follow-up period of our enrolled cases, the incidence density of hearing loss in the mtDNA variants group was 36.42 per 10,000 person-years, compared to 23.77 per 10,000 person-years in the mtDNA wild-type group. According to the results of a review article [13], m.1555 A>G, m.1095 T>C, and m.1494 C>T are the most commonly documented mutations in Chinese subjects with sporadic aminoglycoside-induced and non-syndromic hearing loss. In our study, within the mtDNA mutation group, 607 patients (51.5%) had the m.1555 A>G mutation, 573 patients (48.6%) had the m.1095 T>C mutation, and only 14 patients (1.2%) had the m.1494 C>T mutation. The second most common mutation in the MT-RNR1 in our study, m.1095 T>C, was also included in the analysis. However, based on findings from East Asian families in the current studies, it appears to lack pathogenic significance and has a low penetrance for deafness [29, 30].
We found that the presence of mtDNA pathogenic variants in the MT-RNR1 is associated with a higher risk of hearing loss, especially in the younger population (The age of 35 to 54). This could be attributed to the interplay of environmental factors (diet, radiation, etc.) with inherited nuclear DNA and mtDNA susceptibility genes on a background of accumulating mtDNA mutations, further contributing to the progressive deterioration of mitochondrial function with age [27, 31], thereby diminishing the influence of the MT-RNR1 gene [32]. So it’s possible that with increasing age, other genetic changes or pre-existing health conditions may influence the interpretation of our statistical impact of MT-RNR1 on hearing loss. From previous studies, the penetrance for hearing loss and varies widely among reports and families, but the lower penetrance was noted after aminoglycoside exposure was excluded [30,31,32,33]. It was postulated that other nuclear modifier genes or nuclear background play a role in the phenotypic manifestation of SNHL [26, 34]. The increased risk of aminoglycoside-induced hearing loss is well-documented in previous literature [34]. The Clinical Pharmacogenetics Implementation Consortium Guideline offers treatment recommendations for aminoglycoside use based on MT-RNR1 genotypes, suggesting alternatives unless the severity of infection outweighs the high risk of permanent hearing loss and no safe or effective alternatives are available [35]. However, the limited number of patients with MT-RNR1 pathogenic mutations and a history of aminoglycoside or loop diuretic exposure led to no significant correlation with increased hearing loss susceptibility in real world. This could be attributed to the rarity of patients with mitochondrial gene mutations, the infrequent diagnosis of hearing loss following the use of aminoglycosides or loop diuretics, or the possibility that patients with a history of exposure are not recorded in the database, all of which could contribute to a reverse causal relationship. Therefore, routine genetic screening before aminoglycoside therapy is somewhat challenging in our current daily clinical practice. Besides, research on early detection and prevention of related comorbidities in young individuals with mtDNA variants is notably limited clinically.
The significant impact of comorbidities on the onset of hearing loss, especially in populations with MT-RNR1 variants, is evident in our study. This impact was notably substantial in patients diagnosed with diabetes mellitus. Potential biological mechanisms of these genetic variants have been elucidated. Among these, the MT-RNR1 gene contains the sequence for mitochondrial open-reading frame of the 12 S rRNA-c (MOTS-c), one of mitochondrial-derived peptides (MDPs), reported to possess metabolic protective properties in various models of metabolic dysfunction, such as diabetes mellitus [11, 36, 37]. In vivo studies have also confirmed the role of MOTS-c in enhancing insulin sensitivity and glucose homeostasis, with implications for the folate cycle, 5-aminoimidazole-4-carboxamide ribonucleotide (AICAR), and AMP-activated protein kinase (AMPK) signaling pathways [37].
On the other hand, in most mammalian cells, reactive oxygen species (ROS), primarily produced in the mitochondria, are reactive oxygen species also known as free radicals. The accumulation of ROS and the resulting oxidative damage have been shown to cause tissue dysfunction in various parts of the auditory system [38,39,40]. Considering that mtDNA is situated near the site of oxidative phosphorylation (OXPHOS) in the inner membrane of mitochondria, it is particularly vulnerable to ROS, leading to an increased susceptibility to mtDNA mutations. Additionally, substantial evidence indicates a strong correlation between the loss of mtDNA integrity, ROS accumulation, and various health conditions, including the aging process, neurodegenerative diseases [41, 42], and diabetes mellitus, characterized by insulin resistance and hyperglycemia [43, 44].
In the context of age-related hearing loss (ARHL), a majority of studies have affirmed that the build-up of mtDNA mutations over time results in mitochondrial dysfunction and subsequent degeneration of the cochlea and central auditory pathway, culminating in ARHL [45, 46]. While the impact of the three mtDNA mutation alleles explored in this study concerning this “vicious cycle” (referred to as the mitochondrial clock theory [47]) remains uncertain, we postulate that the onset of hearing loss is strongly associated with the accumulation of oxidative damage. Even in our study, we observed a significantly different risk of developing hearing loss in the mtDNA variant group after adjusting for age. This finding supports the hypothesis that mitochondrial gene translation, including processes like the oxidative phosphorylation (OXPHOS) system mentioned previously, may play a role in hearing loss as well [37].
In previous studies [48, 49], the association between SNHL, diabetes mellitus and cardiovascular disease has been established. However, the role of dyslipidemia and renal disease in SNHL remains limited or unclear [50, 51]. Our results also demonstrated a significant relationship between SNHL and diabetes, particularly in individuals with mtDNA variants. From a clinical perspective, there is a compelling rationale for actively monitoring the hearing of patients with MT-RNR1 gene mutations, especially those with comorbid conditions like diabetes. In the era of precision medicine, it is recommended to screen individuals with mtDNA variants for hearing problem during their health exams, and multimorbidity should be considered when treating one of the comorbid condition in audiological care [52].
Establishing a causal link between MT-RNR1 mutations and aminoglycoside-induced hearing loss is challenging due to limited data. Although unable to confirm a significant association between aminoglycoside exposure and hearing loss in individuals with pathogenic variants, our findings suggest that mitochondrial sequence variants may be more common in non-syndromic hearing loss cases than clinically acknowledged. Furthermore, our study fills gaps in the interpretation guidelines for mitochondrial variants, uncovering the impact of drug exposure on phenotypes not fully recognized in these guidelines, such as comorbidities like diabetes mellitus.
Limitations and strengths
This study possesses several limitations. Firstly, defining the incidence of hearing loss events using the ICD-TM code from data could result in misclassification. However, the criteria, which requires at least three outpatient claims records with a gap exceeding 90 days between the first and last appointments for hearing impairment, should reduce the risk of such misclassification. Furthermore, given the cohort design, this misclassification likely results in a non-directional bias, potentially leading to an underestimation of the disease risk. Secondly, the diagnosis of hearing loss in our study does not differentiate between varying degrees of severity, which could potentially affect our risk assessments. Nevertheless, we posit that any auditory deficit, regardless of the degree of decibel loss, is considered hearing loss for the affected individual. Consequently, this lack of distinction may not significantly impact our study’s findings. However, it represents an area worthy of further exploration in future research, which should include a detailed analysis of the degrees of hearing loss and corresponding decibel levels. Due to constraints in accessing specific information from the database, we couldn’t account for all the environmental factors associated with hearing loss, such as noise exposure or lifestyle factors (e.g., smoking, and drinking). This may introduce residual confounding bias. Moreover, given the ethical imperative to safeguard participants, it is infeasible to conduct prospective trials determining if drug treatments might induce irreversible deafness in genetically predisposed patients. Lastly, considering causal inference and the timing of medication use, only a minority of carriers of the MT-RNR1 variant in our dataset were exposed to aminoglycosides, potentially increasing the risk of a type II error. Future research is warranted to further discuss the implications for patients with diabetes mellitus who carry this variant and are treated with aminoglycosides, in order to validate our findings.
This study offers several merits. First, our study involved a retrospective cohort design with a 20-year follow-up period, exceeding the follow-up duration of several other studies. Second, to mitigate variability in disease severity between the two groups, which could influence study outcomes, we assessed the risk of hearing loss in individuals with gene variants, using a reference group of patients without such variants for comparison. Third, we provide additional evidence regarding the risks associated with mitochondrial gene variants, specifically concentrating on the pharmacogenetic loci m.1555 A>G and m.1095 T>C, to deliver further insights. Future research is required to validate our observations.
Conclusion
In this 20-year cohort study, participants with MT-RNR1 gene mutations exhibited a risk of hearing loss approximately 1.54 times higher than those without such mutations. This risk was particularly elevated in participants with diabetes mellitus. Our study provides valuable insights into the importance of preventing hearing loss events in adults with mitochondrial gene mutations, particularly in diabetic patients. Future genetic cohort studies related to hearing loss, better integrated with clinical characteristics, will enable more precise medical interventions, including targeted treatments and monitoring for hearing loss in patients with mitochondrial gene mutations.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request. When we intend to use electronic medical record data from our hospital for research purposes, we must maintain data confidentiality. We have submitted a research proposal, obtain IRB approval, sign a data confidentiality agreement, a conflict of interest avoidance statement, and other documents. Additionally, we must obtain approval from the Hospital Medical Data Management Committee before granting permission to data users to operate the data (IRB number: CMUH111-REC1-176 in additional file). All patient data will ultimately be de-identified and unlinked to ensure confidentiality. Data users can only access the analysis results obtained after computation for publication, ensuring the confidentiality of the data.
Abbreviations
- AICAR:
-
5-aminoimidazole-4-carboxamide ribonucleotide
- aHR:
-
Adjusted hazard ratio
- AMPK:
-
AMP-activated protein kinase
- ARHL:
-
Age-related hearing loss
- CIs:
-
Confidence intervals
- CR:
-
Call rate
- CMUH:
-
China Medical University Hospital
- ID:
-
Incidence density
- mtDNA:
-
Mitochondrial DNA
- MDP:
-
Mitochondrial-derived peptide
- MT-RNR1 :
-
Mitochondrial 12 S rRNA
- MOTS-c:
-
Mitochondrial open-reading frame of the 12S rRNA-c
- OXPHOS:
-
Oxidative phosphorylation
- QC:
-
Quality control
- ROS:
-
Reactive oxygen species
- SNHL:
-
Sensorineural hearing loss
- SNP:
-
Single nucleotide polymorphism
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- TPMIL:
-
Taiwan Precision Medicine Initiative
References
Sheffield AM, Smith RJH. The epidemiology of deafness. Cold Spring Harb Perspect Med. 2019;9(9).
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–46.
Marques T, Marques FD, Migueis A. Age-related hearing loss, depression and auditory amplification: a randomized clinical trial. Eur Arch Otorhinolaryngol. 2022;279(3):1317–21.
Cunningham LL, Tucci DL. Hearing loss in adults. N Engl J Med. 2017;377(25):2465–73.
Zahnert T. The differential diagnosis of hearing loss. Dtsch Arztebl Int. 2011;108(25):433–43. quiz 44.
Birkenhager R, Aschendorff A, Schipper J, Laszig R. [Non-syndromic hereditary hearing impairment]. Laryngorhinootologie. 2007;86(4):299–309. quiz 10 – 3.
Young A, Ng M. Genetic Hearing Loss. StatPearls. Treasure Island (FL)2024.
Hilgert N, Smith RJH, Van Camp G. Forty-six genes causing nonsyndromic hearing impairment: which ones should be analyzed in DNA diagnostics? Mutat Res. 2009;681(2–3):189–96.
Shearer AE, Hildebrand MS, Schaefer AM, Smith RJH. Genetic hearing loss overview. In: Adam MP, Feldman J, Mirzaa GM, et al. editors. GeneReviews®. Seattle (WA). Volume 14. University of Washington, Seattle; 1999.
Barbarino JM, McGregor TL, Altman RB, Klein TE. PharmGKB summary: very important pharmacogene information for MT-RNR1. Pharmacogenet Genomics. 2016;26(12):558–67.
Merry TL, Chan A, Woodhead JST, Reynolds JC, Kumagai H, Kim SJ, Lee C. Mitochondrial-derived peptides in energy metabolism. Am J Physiol Endocrinol Metab. 2020;319(4):E659–66.
Guan MX. Mitochondrial 12S rRNA mutations associated with aminoglycoside ototoxicity. Mitochondrion. 2011;11(2):237–45.
Ding Y, Leng J, Fan F, Xia B, Xu P. The role of mitochondrial DNA mutations in hearing loss. Biochem Genet. 2013;51(7–8):588–602.
Nguyen T, Jeyakumar A. Genetic susceptibility to aminoglycoside ototoxicity. Int J Pediatr Otorhinolaryngol. 2019;120:15–9.
Wu CC, Chiu YH, Chen PJ, Hsu CJ. Prevalence and clinical features of the mitochondrial m.1555A > G mutation in Taiwanese patients with idiopathic sensorineural hearing loss and association of haplogroup F with low penetrance in three families. Ear Hear. 2007;28(3):332–42.
Liu TY, Hsu HY, You YS, Hsieh YW, Lin TC, Peng CW, et al. Efficacy of Warfarin Therapy guided by pharmacogenetics: a real-world investigation among Han Taiwanese. Clin Ther. 2023;45(7):662–70.
Fischel-Ghodsian N, Kopke RD, Ge X. Mitochondrial dysfunction in hearing loss. Mitochondrion. 2004;4(5–6):675–94.
Wu CC, Tsai CY, Lin YH, Chen PY, Lin PH, Cheng YF et al. Genetic epidemiology and clinical features of Hereditary hearing impairment in the Taiwanese Population. Genes (Basel). 2019;10(10).
Wu CC, Tsai CH, Hung CC, Lin YH, Lin YH, Huang FL, et al. Newborn genetic screening for hearing impairment: a population-based longitudinal study. Genet Med. 2017;19(1):6–12.
Wu CC, Hung CC, Lin SY, Hsieh WS, Tsao PN, Lee CN, et al. Newborn genetic screening for hearing impairment: a preliminary study at a tertiary center. PLoS ONE. 2011;6(7):e22314.
Kokotas H, Grigoriadou M, Korres GS, Ferekidou E, Papadopoulou E, Neou P, et al. The A1555G mitochondrial DNA mutation in Greek patients with non-syndromic, sensorineural hearing loss. Biochem Biophys Res Commun. 2009;390(3):755–7.
Jacobs HT, Hutchin TP, Kappi T, Gillies G, Minkkinen K, Walker J, et al. Mitochondrial DNA mutations in patients with postlingual, nonsyndromic hearing impairment. Eur J Hum Genet. 2005;13(1):26–33.
Bitner-Glindzicz M, Pembrey M, Duncan A, Heron J, Ring SM, Hall A, Rahman S. Prevalence of mitochondrial 1555A–>G mutation in European children. N Engl J Med. 2009;360(6):640–2.
Igumnova V, Veidemane L, Viksna A, Capligina V, Zole E, Ranka R. The prevalence of mitochondrial mutations associated with aminoglycoside-induced deafness in ethnic Latvian population: the appraisal of the evidence. J Hum Genet. 2019;64(3):199–206.
Yao GD, Li SX, Chen DL, Feng HQ, Zhao SB, Liu YJ, et al. Combination of hearing screening and genetic screening for deafness-susceptibility genes in newborns. Exp Ther Med. 2014;7(1):218–22.
Soini HK, Karjalainen MK, Hinttala R, Rautio A, Hallman M, Uusimaa J. Mitochondrial hearing loss mutations among Finnish preterm and term-born infants. Audiol Res. 2017;7(2):189.
Kokotas H, Petersen MB, Willems PJ. Mitochondrial deafness. Clin Genet. 2007;71(5):379–91.
Alde M, Cantarella G, Zanetti D, Pignataro L, La Mantia I, Maiolino L et al. Autosomal Dominant Non-syndromic hearing loss (DFNA): a Comprehensive Narrative Review. Biomedicines. 2023;11(6).
Lu J, Qian Y, Li Z, Yang A, Zhu Y, Li R, et al. Mitochondrial haplotypes may modulate the phenotypic manifestation of the deafness-associated 12S rRNA 1555A > G mutation. Mitochondrion. 2010;10(1):69–81.
Chu SY, Chiang SC, Chien YH, Hwu WL. Screening of mitochondrial DNA mutations in subjects with non-syndromic familial hearing impairment in Taiwan. Acta Paediatr Taiwan. 2002;43(6):330–3.
Young WY, Zhao L, Qian Y, Li R, Chen J, Yuan H, et al. Variants in mitochondrial tRNAGlu, tRNAArg, and tRNAThr may influence the phenotypic manifestation of deafness-associated 12S rRNA A1555G mutation in three Han Chinese families with hearing loss. Am J Med Genet A. 2006;140(20):2188–97.
Yao YG, Salas A, Bravi CM, Bandelt HJ. A reappraisal of complete mtDNA variation in east Asian families with hearing impairment. Hum Genet. 2006;119(5):505–15.
Dai P, Yuan Y, Huang D, Qian Y, Liu X, Han D, et al. Extremely low penetrance of deafness associated with the mitochondrial 12S rRNA T1095C mutation in three Chinese families. Biochem Biophys Res Commun. 2006;348(1):200–5.
Zhao H, Li R, Wang Q, Yan Q, Deng JH, Han D, et al. Maternally inherited aminoglycoside-induced and nonsyndromic deafness is associated with the novel C1494T mutation in the mitochondrial 12S rRNA gene in a large Chinese family. Am J Hum Genet. 2004;74(1):139–52.
McDermott JH, Wolf J, Hoshitsuki K, Huddart R, Caudle KE, Whirl-Carrillo M, et al. Clinical pharmacogenetics implementation Consortium Guideline for the Use of aminoglycosides based on MT-RNR1 genotype. Clin Pharmacol Ther. 2022;111(2):366–72.
Lee C, Zeng J, Drew BG, Sallam T, Martin-Montalvo A, Wan J, et al. The mitochondrial-derived peptide MOTS-c promotes metabolic homeostasis and reduces obesity and insulin resistance. Cell Metab. 2015;21(3):443–54.
Molenaars M, Daniels EG, Meurs A, Janssens GE, Houtkooper RH. Mitochondrial cross-compartmental signalling to maintain proteostasis and longevity. Philos Trans R Soc Lond B Biol Sci. 2020;375(1801):20190414.
Zhang L, Du Z, He L, Liang W, Liu K, Gong S. ROS-Induced oxidative damage and mitochondrial dysfunction mediated by inhibition of SIRT3 in cultured cochlear cells. Neural Plast. 2022;2022:5567174.
Kishimoto-Urata M, Urata S, Fujimoto C, Yamasoba T. Role of oxidative stress and antioxidants in Acquired Inner ear disorders. Antioxid (Basel). 2022;11:8.
Usami SI, Nishio SY et al. Nonsyndromic Hearing Loss and Deafness, Mitochondrial. In: Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, editors. GeneReviews((R)). Seattle (WA)1993.
Grimm A, Eckert A. Brain aging and neurodegeneration: from a mitochondrial point of view. J Neurochem. 2017;143(4):418–31.
Maynard S, Fang EF, Scheibye-Knudsen M, Croteau DL, Bohr VA. DNA damage, DNA repair, aging, and Neurodegeneration. Cold Spring Harb Perspect Med. 2015;5(10).
Victor VM, Rocha M, Herance R, Hernandez-Mijares A. Oxidative stress and mitochondrial dysfunction in type 2 diabetes. Curr Pharm Des. 2011;17(36):3947–58.
Zhang Z, Huang Q, Zhao D, Lian F, Li X, Qi W. The impact of oxidative stress-induced mitochondrial dysfunction on diabetic microvascular complications. Front Endocrinol (Lausanne). 2023;14:1112363.
Lin MT, Beal MF. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006;443(7113):787–95.
Yamasoba T, Someya S, Yamada C, Weindruch R, Prolla TA, Tanokura M. Role of mitochondrial dysfunction and mitochondrial DNA mutations in age-related hearing loss. Hear Res. 2007;226(1–2):185–93.
Tavanai E, Mohammadkhani G. Role of antioxidants in prevention of age-related hearing loss: a review of literature. Eur Arch Otorhinolaryngol. 2017;274(4):1821–34.
Stam M, Kostense PJ, Lemke U, Merkus P, Smit JH, Festen JM, Kramer SE. Comorbidity in adults with hearing difficulties: which chronic medical conditions are related to hearing impairment? Int J Audiol. 2014;53(6):392–401.
Crews JE, Campbell VA. Vision impairment and hearing loss among community-dwelling older americans: implications for health and functioning. Am J Public Health. 2004;94(5):823–9.
Deepika P, Rajeshwary A, Usha S, Goutham MK, Raghav S. Does dyslipidemia worsen the hearing level in diabetics? J Otol. 2017;12(4):198–201.
Madhan S, Bambore Suryanarayan Rao R, Parameshwarappa A, Murundi Basavaraj B, Bhadravathi Ganesh P, Shetty S, et al. Evaluation of the effects of Dyslipidemia on hearing in patients with type 2 diabetes Mellitus. Indian J Otolaryngol Head Neck Surg. 2023;75(Suppl 1):541–7.
Besser J, Stropahl M, Urry E, Launer S. Comorbidities of hearing loss and the implications of multimorbidity for audiological care. Hear Res. 2018;369:3–14.
Acknowledgements
We are grateful to Health Data Science Center, China Medical University Hospital for providing administrative and technical support. The funders had no role in the study design, data collection and analysis, the decision to publish, or preparation of the manuscript. No additional external funding was received for this study.
Funding
This study is supported in part by China Medical University Hospital (DMR 110 − 057; DMR-111-061; DMR-111-105; DMR-112-087) and the National Science and Technology Council in Taiwan(111-2302-B-039-038-MY2).
Author information
Authors and Affiliations
Contributions
Writing, review, and edting manuscript: Y-W Hsieh, H-K Chen, H-Y Hsu. Designed Research: C-D Lin, F-J Tsai, Y-W Hsieh. Performed Research: T-Y Liu, H-Y Hsu. Analyzed Data: H-Y Hsu, Y-T Zhang. H-K Chen and Y-W Hsieh have equal contributions to this article. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This research is a retrospective cohort study based on the review of electronic medical records, which does not involve subjects and falls within the scope of exemption from informed consent. Therefore, there are no ethical considerations. Furthermore, these data were inputted into the database with the informed consent of relevant subjects, ensuring that the information is used solely for academic research purposes while maintaining de-identification and privacy protection. And the research was approved by the ethics review board of the research ethics committee of China Medical University (IRB number: CMUH111-REC1-176).
Consent for publication
Not applicable.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be constructed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, HK., Hsieh, YW., Hsu, HY. et al. Increased risk of hearing loss associated with MT-RNR1 gene mutations: a real-world investigation among Han Taiwanese Population. BMC Med Genomics 17, 155 (2024). https://doi.org/10.1186/s12920-024-01921-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-024-01921-8