Abstract
Background
Mutations in ABHD12 (OMIM: 613,599) are associated with polyneuropathy, hearing loss, ataxia, retinitis pigmentosa, and cataract (PHARC) syndrome (OMIM: 612674), which is a rare autosomal recessive neurodegenerative disease. PHARC syndrome is easily misdiagnosed as other neurologic disorders, such as retinitis pigmentosa, Charcot-Marie-Tooth disease, and Refsum disease, due to phenotype variability and slow progression. This paper presents a novel mutation in ABHD12 in two affected siblings with PHARC syndrome phenotypes. In addition, we summarize genotype-phenotype information of the previously reported patients with ABHD12 mutation.
Methods
Following a thorough medical evaluation, whole-exome sequencing was done on the proband to look for potential genetic causes. This was followed by confirmation of identified variant in the proband and segregation analysis in the family by Sanger sequencing. The variants were interpreted based on the American College of Medical Genetics and Genomics (ACMG) guidelines.
Results
A novel pathogenic homozygous frameshift variant, NM_001042472.3:c.601dup, p.(Val201GlyfsTer4), was identified in exon 6 of ABHD12 (ACMG criteria: PVS1 and PM2, PM1, PM4, PP3, and PP4). Through Sanger sequencing, we showed that this variant is co-segregated with the disease in the family. Further medical evaluations confirmed the compatibility of the patients’ phenotype with PHARC syndrome.
Conclusions
Our findings expand the spectrum of mutations in the ABHD12 and emphasize the significance of multidisciplinary diagnostic collaboration among clinicians and geneticists to solve the differential diagnosis of related disorders. Moreover, a summary based on mutations found so far in the ABHD12 gene did not suggest a clear genotype-phenotype correlation for PHARC syndrome.
Similar content being viewed by others
Introduction
Concurrent impairments of the essential senses of hearing and vision greatly influence affected individuals’ quality of life and often result in morbidity and mortality [1,2,3,4]. This accompaniment accounts for nearly 0.015% of the general population, with patients under 18 years of age making up 5.7% of this group [5]. Among diverse etiological reasons for these impairments, heritable factors are estimated to be responsible for 27% of cases [5]. Usher syndrome has the highest frequency among such impairments [5, 6]; other syndromes include PHARC (polyneuropathy, hearing loss, ataxia, retinitis pigmentosa, and cataract) syndrome (OMIM: 612674), Heimler syndrome 1 (OMIM: 234580), Alstrom syndrome (OMIM: 203800), Bardet-Biedel syndrome (OMIM: 209900), and Cone-rod dystrophy and hearing loss 1 (OMIM: 617236).
PHARC syndrome is an autosomal recessive neurodegenerative disease influencing the peripheral and central nervous systems. Its name is taken from its significant features, including polyneuropathy, hearing loss, ataxia, retinitis pigmentosa (RP), and cataract [7], although not all of these features necessarily manifest at the initial presentation [7, 8]. Some patients show only some of these symptoms for years so affected individuals are usually misdiagnosed with other neurodegenerative diseases like Usher syndrome, RP, Refsum, Charcot-Marie-Tooth, and mitochondrial diseases [8, 9]. Genetic testing can lead to a definitive diagnosis by differentiating between these similar syndromes.
Loss of function mutations in the ABDH12 gene (OMIM: 613599) cause PHARC syndrome. This gene contains 13 coding exons on chromosome 20 and translates to an α/βhydrolase domain-containing 12 (ABHD12) protein. The ABHD12 protein is a kind of enzyme that participates in lipid metabolism by catalyzing 2-arachidonoyl glycerol (2-AG) [7]. 2-AG, as the main endocannabinoid lipid transmitter, acts in neuroinflammation and synaptic plasticity. The endocannabinoid system participates in different biological processes, for instance, neurotransmission, inflammation, mood, appetite, pain appreciation, and addiction behavior [10]. ABHD12 is expressed in different mouse tissues, but the highest expression has been observed in microglia and macrophages, especially in the brain [7]. Since a single functional copy of ABHD12 makes sufficient enzyme activity therefore, heterozygous carriers do not present any clinical features [11, 12].
The current challenge of diagnosing PHARC syndrome makes it essential to investigate its clinical and genetic features. Increasing data in these areas can expand the current knowledge about its onset, the existence of genotype-phenotype correlations, and the natural history of PHARC syndrome; it may also help introduce new potential treatment strategies.
This report presents the clinical manifestation of two affected individuals from a consanguineous Iranian family with mild sensory symptoms, progressive hearing impairment, cataract, and RP. Whole-exome sequencing (WES), followed by segregation analysis, confirmed a novel biallelic mutation in ABHD12. We also compared the clinical presentation and molecular findings of these patients with the previous reports of PHARC syndrome to gain a better realization of the genotype-phenotype correlations of ABHD12.
Methods
Study participants and clinical evaluations
In this study, two Iranian consanguineous siblings with mild sensory symptoms, progressive hearing impairment, RP, and cataract were enlisted (Fig. 1a). The proband (IV.1) was a 25-year-old male; his 18-year-old sister (IV.2) had the same manifestation but with milder symptoms. Clinical examinations, involving family history and physical exams, were conducted in Hazrat Rasoul Akram Hospital, Tehran, Iran. The patients (IV.1 and IV.2) were examined by otologists, ophthalmologists, and neurologists.
Pedigree information and hearing level in family. (A) Pedigree of the family indicates a pattern autosomal recessive inheritance. The pedigree shows co-segregation of ABHD12 variant ((+) = NM_001042472.3:c.601dup; p.(Val201GlyfsTer4). In this image, the arrow presents proband, black symbols implicate affected; white symbols represent unaffected; circles are females; squares are men; and parallel lines indicate consanguineous marriage. (B) Pure tone audiograms of an unaffected father. (C) Pure tone audiograms of an unaffected mother (D) Audioprofile indicates progressive hearing loss in patient IV.1 in 8-year, 11-year, 18-year, 24-year and 25-year, respectively. (E) Audioprofile indicates progressive hearing loss in patient IV.2 in 7-year, 11-year, 16-year and 18-year, respectively. The frequency is shown in hertz (Hz) and the hearing threshold is shown in decibels (dB). The blue ‘×’ and red ‘o’ show results from an air conduction test of the left and right ear, respectively
Standard conventional audiometry, including air- and bone-conduction testing, was carried out for IV.1, IV.2, III.1, and III.2 [13]. Additionally, a complete ophthalmologic examination of the afflicted individuals (IV.1 and IV.2) included assessments of best-corrected visual acuity (BCVA), slit lamp bio microscopy, electroretinography (ERG), and optic coherence tomography (OCT). Neurological evaluations include electromyographic recordings, nerve conduction studies comprising measurements of motor and sensory nerves of the upper and lower extremities, and magnetic resonance brain imaging (MRI). Routine laboratory testing was conducted, including tests for liver transaminases, glomerular filtration rate, complete blood count, and electrolytes. Genomic DNA was extracted from blood samples (5 mL) of patients and healthy parents as described before [14].
Whole-exome sequencing and bioinformatics analysis
WES was done based on the previous works [15, 16]. Briefly, the exomes were captured by the SureSelect Human All Exon V7 Kit (Agilent, Santa Clara, CA, USA). Sequencing was done on an Illumina Hiseq2000 system (Illumina, San Diego, USA) with a mean coverage of 100X. The GRCh38/hg38 genome assembly was used to align reads.
To reach the disease-causing variants, firstly, the variants with minor allele frequency above 1% in databases like bSNP [17], gnomAD [18], and Iranome [19] were removed from the WES data of the patient. Secondly, synonymous changes and all non-coding areas other than the 20 bp flanking regions were eliminated. Bioinformatics techniques such as SIFT [20], Polyphen2 [21], MutationTaster [22], PROVEAN [23], and Combined Annotation Dependent Depletion [24] were used to predict the outcomes of the variants. According to patients’ clinical manifestations (e.g., sensorimotor neuropathy, hearing impairment, and abnormal eye physiology), the remaining variations were prioritized using ClinVar [25], Human Gene Mutation Database (HGMD) [26], human phenotype ontology [27], and Deafness Variation Database (DVD) [28]. Variant interpretation followed the ACMG/AMP (American College of Genetics and Genomics/Association for Molecular Pathology) recommendations [2].
Family segregation study and protein analysis
Direct Sanger sequencing was used to verify the identified variants in affected members, and co-segregation analysis of the causative homozygous variant was done on all family members. The primers for the area of interest were designed using Primer3 software [29]. The forward primer: 5′-GTCTTTGTCAGGACCCAGGA-3′ and the reverse primer: 5′-AGTCAGGCAGCATGTCACAG-3′ were used to amplify the identified variant in ABHD12. PCR was done in standard conditions [15]. The PCR products were used for direct Sanger sequencing and the data were analyzed using Codon code aligner V.5.1.5.
To study the effect of identified mutation on the ABHD12 functional domains ConSurf server (https://consurf.tau.ac.il/) and UniProt [30] were used. Swiss-Model software (https://swissmodel.expasy.org/interactive) was used to design the 3D structure of the protein. I-Mutant3.0 was used to predict protein stability (http://gpcr2.biocomp.unibo.it/cgi/predictors/I-Mutant3.0/I-Mutant3.0.cgi), and MetaDome [31] was used to recognize the intolerant areas in the ABHD12 protein.
Literature review
In November 2022, a thorough search was conducted in Google Scholar and PubMed using the terms ABHD12 and PHARC syndrome. All original English full-text articles and case reports with clinical and genetic information were added. Available phenotype and genotype were included.
Results
Clinical findings
The patients were born to a first-cousin marriage (Fig. 1a). Both patients presented bilateral pes cavus. Audiology evaluations showed a progressive sensorineural hearing impairment in patients (IV.1 and IV.2) that was first distinguished at the age of 11. The audio profiles of patients at different ages are shown in (Fig. 1d, e), and air conduction audiograms of their healthy parents are presented in (Fig. 1b,c).
A physical examination of IV.1 indicated mild symptoms of stance ataxia with positive Romberg and tandem gait signs, while IV.2 was normal. Heel-to-shin and finger-to-nose tests were normal in both patients, and sensory deficits in the sensation of temperature, vibration, and touch could not be found. Furthermore, both patients’ tendon reflexes in the upper and lower extremities were normal, and muscular atrophy and weakness were absent. Routine laboratory tests were normal in both patients.
Electrophysiology
Both patients’ nerve conduction studies revealed a chronic demyelinating sensorimotor neuropathy with uniform conduction, showing that nerve conduction velocities were well below 40 m/s in both the upper and lower extremities.
Electromyographic recordings in both patients displayed a regular pattern of the motor unit. Pathologic spontaneous activity could not be found.
Ophthalmologic examination and brain imaging
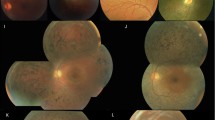
An ophthalmologic examination revealed that BCVA was 2/10 and 2/10 for IV.1 and 9/10 and 8/10 for IV.2 for the right and left eyes, respectively. Patient IV.1 showed a bilateral moderate posterior subcapsular cataract, while his younger sister (IV.2) showed a bilateral mild posterior subcapsular cataract. Both patients showed signs of RP in fundus autofluorescence (FAF), OCT, and ERG (Fig. 2and Fig. 3). The MRI of the brain of patient IV.1 revealed cerebellar atrophy (Fig. 4), while it was normal in patient IV.2.
Fundus autofluorescence (FAF), optical coherence tomography (OCT) images, and electroretinography (ERG) in patient IV.1 with ABHD12 variants. (A) The eyes of a 25-year-old man with Snellen best-corrected visual acuity (BCVA) of 2/10. Fundus autofluorescence imaging showed typical ring-shaped macular alterations. (B) OCT showed preservation of the outer retinal layers in the fovea with outer retinal atrophy outside fovea. (C) ERG revealed a significant reduction in the amplitude of the scotopic and photopic recordings
Fundus autofluorescence (FAF), optical coherence tomography (OCT) images, and electroretinography (ERG) in patient IV.2 with ABHD12 variants. (A) The eyes of an 18-year-old woman with Snellen BCVA of 9/10 and 8/10 for the right and left eye, respectively. FAF imaging was preserved in this case. (B) On OCT, loss of the ellipsoid zone was observed in the extrafoveal area. (C) ERG showed a significant reduction in the amplitude of the scotopic and photopic recordings
Molecular findings
Four family members were evaluated in total (Fig. 1a). Firstly, based on the ACMG guidelines for screening for genes associated with hearing loss [2], the absence of mutation in GJB2 was investigated in both patients (IV.1 and IV.2) [32, 33]. After the analysis of the exome sequencing data on IV.1 (Fig. 5b), a novel frameshift duplication in exon six of the ABHD12 gene—NM_001042472.3: c.601 dup; p.(Val201GlyfsTer4)— that co-segregated with the phenotype was identified (Figs. 1a and 5a). The variant was not reported in ClinVar, DVD, HGMD, dbSNP v.154, and gnomAD. The allele frequency for this variant was zero in Iranome (local database).
Chromatogram, multiple amino acid alignment, and 3D protein structure. (A) The chromatogram for the c.601dup found in the family in exon 6 of ABHD12 is highlighted in blue. Patient individuals are homozygous (IV.1, IV.2), and their parents are heterozygous (III.1, III.2). (B) Schematic representation of filtering strategies used in this study (C) The wild-type model structure of ABHD12 protein (left side) and p.Val 201GlyfsTer4 protein (right side). Sequencing analysis showed a novel frameshift variant resulting in premature stop codon of ABHD12 (bottom side)
This variant is located in the αβ-hydrolase domain of the ABHD12 protein (Fig. 6a). We further confirmed this finding by using I-Mutant3.0, which exhibited that this variant can bring the protein close to an unstable (Free Energy change value < − 3.03) and predict its effect on human health (Disease RI: 5). Actually, the I-mutant server calculates the free energy of mutant protein and negative value of free energy change shows a decrease in protein stability. The MetaDome (a server for analysis the mutation tolerance at each position in a human protein) results indicated that this variant was situated in the intolerant regions of the ABHD12 protein (Fig. 6b).
Gene and protein structure. (A) Intron-exon structure of ABHD12 and location of all mutations found up to now. Twenty-nine mutations in ABHD12 associated with PHARC syndrome have been found. The new frameshift variant, c.601dup, is indicated by the purple color in ab hydrolase domain which is indicated by brown color. Black rectangles and black lines represent exons and introns, respectively. ABHD12 has 13 exons. The only difference between the two isoforms is in their last exon, which is indicated by two stop codons in the picture (black frame, isoform 1, and orange frame, isoform 2). Gray rectangles indicate 3′UTR and 5′UTR rejoin. The blue rectangle shows GINS1 gene next to ABHD12 gene. In the 59Kb deletion removes the exon 1 of ABHD12 and exons 1–4 of GINS1 and both promoters. The gray arrows on the top of the image indicate the orientation of the genes. The figure is redrawn from ref [38] (B) MetaDome [31] was used to recognize the intolerant regions in the ABHD12 protein
We classified the novel frameshift based on ACMG/AMP guidelines (Criteria: PVS1 and PM2, PM1, PM4, PP3, and PP4) as “pathogenic” variant [2].
Literature review
A comprehensive analysis of ABHD12 variants was carried out. Data from this research were compared with 14 previously published articles [7,8,9, 11, 12, 34,35,36,37,38,39,40,41,42]. In summary, 58 patients from 38 families were included. 29 distinct ABHD12 mutations have been identified in these published articles. Their phenotype, genotype, age, and sex are summarized in (Table 1), while all variants are illustrated in Fig. 6. It has been documented that ABHD12 exhibits a broad range of clinical heterogeneity in terms of age of onset, spectrum of phenotypes, severity, and progression. Cataract and hearing impairment were the most common conditions reported in ABHD12 patients.
Most mutations reported in ABHD12 were frameshift mutations (Table 1). The c.337-338delGAinsTTT is the most common variant. only seven of these variants (c.193 C > T, c.316 + 2T > A, c.337-338delGAinsTTT, c.784 C > T, c.846-852dupTAAGAGC, c.1054 C > T, and c.1063 C > T) have been reported in more than one family.
Discussion
In this study, we detected a novel frameshift variant in the ABHD12 gene in two affected Iranian siblings with PHARC syndrome from a first-cousin marriage (Fig. 1a). The identified variant, c.601dup; p.(Val201GlyfsTer4), leads to a premature stop codon (Fig. 5c), which can result in a loss of function, and was determined as a pathogenic variant in agreement with ACMG guidelines [2].
PHARC syndrome is distinguished by hearing impairment, polyneuropathy, RP, ataxia, and early-onset cataract. The variety of clinical symptoms showed that ABHD12 play crucial roles in the in the central and peripheral nervous systems, as well as the eye, which is confirmed by its expression patterns [7]. ABHD12 is expressed ubiquitously and is extremely expressed in the brain, especially in microglia, macrophages, and in the retina [7, 43].
ABHD12 was detected on chromosome 20 (20p11.21) for the first time in 2010. 29 mutations in 58 patients (38 families) from 14 previously published articles related to the PHARC syndrome around the world have been introduced (Table 1; Fig. 6a). These patients exhibited clinical variability concerning the spectrum of phenotypes, disease onset, severity, and progression [7, 8], and this variability was observed both within the same family and between patients with the same variant from different families (Table 1) [8, 37]. In addition, there is no correlation between the location and type of mutation and the severity of phenotypes in patients. For example, in a comparison between two nonsense mutations (p.Arg352* and p.Arg65*), the patients with the first mutation in early adulthood showed complete phenotypes of PHARC syndrome, while the patients with the second mutation did not experience neuropathy until the fifth decade of their lives (Table 1) [41]. The current evidence does not indicate any genotype-phenotype correlation in patients with mutations in the ABHD12 gene. However, the limited number of reported cases, the multisystemic nature of the PHARC syndrome (which leads to misdiagnosis or delayed diagnosis), delayed referral for evaluation of related phenotypes, or failure to record all phenotypes at the same time in different studies can be effective.
This study’s proband (IV.1) manifested a typical PHARC phenotype, the onset of which dates to the patient’s early teenage years. It had a progressive nature, eventually revealing hearing impairment, bilateral posterior subcapsular cataract, ataxia, demyelinating polyneuropathy, and RP. The clinical picture was completely compatible with PHARC syndrome when the patient was 24 years old. The progression of the disease in the second affected family member was the same, though the symptoms were milder.
In line with most previous studies, sensorineural hearing impairment was the first manifestation in both patients (Table 1). Figure 1 indicates the progress of hearing impairment in both patients. Both patients developed posterior subcapsular cataract during childhood, corroborating previous reports showing that posterior subcapsular cataract frequently occurs in RP patients at a young age [44]. Similar to previous studies, our patients’ definitive diagnosis of PHARC syndrome after a long follow-up period was possible only using WES [7, 8, 35]. The multisystemic nature and slow progression of PHARC syndrome is the main reason for its misdiagnosis. Performing genetic testing next to clinical findings could lead to early diagnosis, timely referrals, and better management of future symptoms.
The ABHD12 gene encodes a 398-amino acid protein product that participates in endocannabinoid metabolism and synaptic plasticity. This product is called the ABHD12 protein, which is a member of the serine hydrolase family and inactivates the endocannabinoid neurotransmitter 2-AG [35, 38]. Furthermore, previous in vivo studies indicated the lysophosphatidylserine (LPS) lipase activity of Abhd12 in the mouse brain and the accumulation of LPS in the mouse model. This accumulation increases phagocytosis activity and microglial activation, which causes neuroinflammation and atrophy in the cerebellum. This neuroinflammation is the presumed cause of motor and auditory defects over time [45,46,47].
ABHD12 is a single-pass integral membrane protein with a transmembrane helix in the N-terminal region and an extracellular active site domain in the C-terminal region [48]. The αβ-hydrolase domain of ABHD12 consists of a lipase motif and catalytic triad (predicted amino acid residues S246-D333-H372), which serves as a fully conserved structure in both humans and rodents [49]. This domain expands between residues 165–351 of ABHD12 (Fig. 6) [36]. The p.(Val201GlyfsTer4) variant occurs within the conserved αβ-hydrolase domain and causes a premature stop codon, which may result in nonsense-mediated decay and, consequently, a lack of the protein product. Navia-Paldanius et al. have shown that site-directed mutagenesis of residues of the catalytic triad of the αβ-hydrolase domain abolished the enzymatic activity of ABHD12 [49]. The research group of Tingaud-Sequeira et al. with functional studies on p.R352* mutation that produces a truncated protein have proved the loss of enzyme activity [38]. Moreover, the variants in this domain are likely to disturb interactions with other molecules or other parts of the protein and affect protein function [38].
ABHD12 is a critical protein in the signaling, metabolism, and regulation of lipids, especially in immune and neurological processes [8, 38, 45, 47].
However, further research is required to fully understand the cellular, molecular, and biochemical mechanisms through which ABHD12 contributes to the PHARC syndrome. Such research could lead to earlier diagnosis, appropriate referrals, effective prognosis for future rehabilitations, improved medical management of disease progression, better genetic counseling, and prevention strategies, and a higher increasing quality of life for patients and their relatives.
A significant limitation in this research pertains to the inability to perform a functional analysis that would elucidate the specific contribution of the newly identified variant to PHARC syndrome.
Conclusion
We elucidated the role of a novel pathogenic mutation in the ABHD12 as a genetic reason of PHARC syndrome in an Iranian family. Additionally, we demonstrated the value of using WES for the early diagnosis of this syndrome. Our findings extend the mutation spectrum of ABHD12 by introducing a novel mutation. We also summarized previously reported mutations in the ABHD12 gene throughout the world and compared them to the new mutation investigated in the present study. We believe these results can help practitioners identify disease pathology and manage the phenotypes in a multidisciplinary setting.
Data Availability
The datasets produced during this manuscript are available from the corresponding author upon reasonable request. The novel variant and phenotypes were submitted in ClinVar database (accession number: VCV001727244.1) and available at (https://www.ncbi.nlm.nih.gov/clinvar/variation/1727244/).
Abbreviations
- PHARC:
-
polyneuropathy hearing loss ataxia retinitis pigmentosa cataracts
- RP:
-
Retinitis pigmentosa
- ABHD12:
-
α/βhydrolase domain-containing 12
- 2-AG:
-
2-arachidonoyl glycerol
- WES:
-
whole-exome sequencing
- BCVA:
-
best-corrected visual acuity
- ERG:
-
electroretinography
- OCT:
-
optic coherence tomography
- MRI:
-
magnetic resonance brain imaging
- Val:
-
valine
- Gly:
-
glycine
- ACMG/AMP:
-
American College of Medical Genetics/Association for Molecular Pathology
References
Lam BL, Lee DJ, Gómez-Marín O, Zheng DD, Caban AJ. Concurrent visual and hearing impairment and risk of mortality: the National Health interview survey. Archives of Ophthalmology (Chicago Ill: 1960). 2006;124(1):95–101.
Oza AM, DiStefano MT, Hemphill SE, Cushman BJ, Grant AR, Siegert RK, et al. Expert specification of the ACMG/AMP variant interpretation guidelines for genetic hearing loss. Hum Mutat. 2018;39(11):1593–613.
Chia E-M, Mitchell P, Rochtchina E, Foran S, Golding M, Wang JJJA. Association between vision and hearing impairments and their combined effects on quality of life. 2006;124(10):1465–70.
Liljas AE, Wannamethee SG, Whincup PH, Papacosta O, Walters K, Iliffe S et al. Socio-demographic characteristics, lifestyle factors and burden of morbidity associated with self-reported hearing and vision impairments in older british community-dwelling men: a cross-sectional study. 2016;38(2):e21–e8.
Wittich W, Watanabe DH, Gagné JP. Sensory and demographic characteristics of deafblindness rehabilitation clients in Montréal. Can Ophthalmic Physiological Optics: J Br Coll Ophthalmic Opticians (Optometrists). 2012;32(3):242–51.
Kimberling WJ, Hildebrand MS, Shearer AE, Jensen ML, Halder JA, Trzupek K, et al. Frequency of Usher syndrome in two pediatric populations: implications for genetic screening of deaf and hard of hearing children. Genet Medicine: Official J Am Coll Med Genet. 2010;12(8):512–6.
Fiskerstrand T, H’Mida-Ben Brahim D, Johansson S, M’Zahem A, Haukanes BI, Drouot N, et al. Mutations in ABHD12 cause the neurodegenerative disease PHARC: an inborn error of endocannabinoid metabolism. Am J Hum Genet. 2010;87(3):410–7.
Nguyen XT, Almushattat H, Strubbe I, Georgiou M, Li CHZ, van Schooneveld MJ et al. The phenotypic spectrum of patients with PHARC Syndrome due to Variants in ABHD12: an Ophthalmic Perspective. Genes. 2021;12(9).
Dias Bastos PA, Mendonça M, Lampreia T, Magriço M, Oliveira J, Barbosa R. PHARC Syndrome, a Rare Genetic disorder-case report. Mov Disorders Clin Pract. 2021;8(6):977–9.
Pacher P, Bátkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58(3):389–462.
Chen DH, Naydenov A, Blankman JL, Mefford HC, Davis M, Sul Y, et al. Two novel mutations in ABHD12: expansion of the mutation spectrum in PHARC and assessment of their functional effects. Hum Mutat. 2013;34(12):1672–8.
Lerat J, Cintas P, Beauvais-Dzugan H, Magdelaine C, Sturtz F, Lia AS. A complex homozygous mutation in ABHD12 responsible for PHARC syndrome discovered with NGS and review of the literature. J Peripheral Nerv System: JPNS. 2017;22(2):77–84.
Falah M, Farhadi M, Kamrava SK, Mahmoudian S, Daneshi A, Balali M, et al. Association of genetic variations in the mitochondrial DNA control region with presbycusis. Clin Interv Aging. 2017;12:459–65.
Falah M, Houshmand M, Mahmoudian S, Emamdjomeh H, Ghavami Y, Farhadi M. The anticipation and inheritance pattern of c.487A > G mutation in the GJB2 gene. Arch Iran Med. 2012;15(1):49–51.
Rayat S, Farhadi M, Emamdjomeh H, Morovvati S, Falah M. Analysis of TMIE gene mutations including the first large deletion of exon 1 with autosomal recessive non-syndromic deafness. BMC Med Genom. 2022;15(1):133.
Vafaee-Shahi M, Farhadi M, Razmara E, Morovvati S, Ghasemi S, Abedini SS et al. Novel phenotype and genotype spectrum of NARS2 and literature review of previous mutations. Ir J Med Sci. 2021.
Smigielski EM, Sirotkin K, Ward M, Sherry ST. dbSNP: a database of single nucleotide polymorphisms. Nucleic Acids Res. 2000;28(1):352–5.
Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alföldi J, Wang Q, et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581(7809):434–43.
Fattahi Z, Beheshtian M, Mohseni M, Poustchi H, Sellars E, Nezhadi SH, et al. Iranome: a catalog of genomic variations in the iranian population. Hum Mutat. 2019;40(11):1968–84.
Sim NL, Kumar P, Hu J, Henikoff S, Schneider G, Ng PC. SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic Acids Res. 2012;40(Web Server issue):W452–7.
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7(4):248–9.
Schwarz JM, Cooper DN, Schuelke M, Seelow D. MutationTaster2: mutation prediction for the deep-sequencing age. Nat Methods. 2014;11(4):361–2.
Choi Y, Chan AP. PROVEAN web server: a tool to predict the functional effect of amino acid substitutions and indels. Bioinf (Oxford England). 2015;31(16):2745–7.
Rentzsch P, Witten D, Cooper GM, Shendure J, Kircher M. CADD: predicting the deleteriousness of variants throughout the human genome. Nucleic Acids Res. 2019;47(D1):D886–d94.
Landrum MJ, Chitipiralla S, Brown GR, Chen C, Gu B, Hart J, et al. ClinVar: improvements to accessing data. Nucleic Acids Res. 2020;48(D1):D835–d44.
Stenson PD, Ball EV, Mort M, Phillips AD, Shaw K, Cooper DN. The human gene mutation database (HGMD) and its exploitation in the fields of personalized genomics and molecular evolution. Curr Protocols Bioinf. 2012;Chap. 1:Unit1.13.
Köhler S, Vasilevsky NA, Engelstad M, Foster E, McMurry J, Aymé S, et al. The human phenotype ontology in 2017. Nucleic Acids Res. 2017;45(D1):D865–d76.
Azaiez H, Booth KT, Ephraim SS, Crone B, Black-Ziegelbein EA, Marini RJ, et al. Genomic Landscape and Mutational Signatures of Deafness-Associated genes. Am J Hum Genet. 2018;103(4):484–97.
Kõressaar T, Lepamets M, Kaplinski L, Raime K, Andreson R, Remm M. Primer3_masker: integrating masking of template sequence with primer design software. Bioinf (Oxford England). 2018;34(11):1937–8.
UniProt. The Universal protein knowledgebase in 2023. Nucleic Acids Res. 2023;51(D1):D523–d31.
Wiel L, Baakman C, Gilissen D, Veltman JA, Vriend G, Gilissen C, MetaDome. Pathogenicity analysis of genetic variants through aggregation of homologous human protein domains. Hum Mutat. 2019;40(8):1030–8.
Falah M, Houshmand M, Akbaroghli S, Mahmodian S, Ghavami Y, Farhadi M. Profile of iranian GJB2 mutations in young population with novel mutation. J Iran J Basic Med Sci. 2011;14(3):213–8.
Falah M, Houshmand M, Balali M, Asghari A, Bagher Z, Alizadeh R, et al. Role of GJB2 and GJB6 in iranian nonsyndromic hearing impairment: from Molecular Analysis to Literature Reviews. Fetal Pediatr Pathol. 2020;39(1):1–12.
Igelman AD, Ku C, da Palma MM, Georgiou M, Schiff ER, Lam BL, et al. Expanding the clinical phenotype in patients with disease causing variants associated with atypical Usher syndrome. Ophthalmic Genet. 2021;42(6):664–73.
Thimm A, Rahal A, Schoen U, Abicht A, Klebe S, Kleinschnitz C, et al. Genotype-phenotype correlation in a novel ABHD12 mutation underlying PHARC syndrome. J Peripheral Nerv System: JPNS. 2020;25(2):112–6.
Li T, Feng Y, Liu Y, He C, Liu J, Chen H, et al. A novel ABHD12 nonsense variant in Usher syndrome type 3 family with genotype-phenotype spectrum review. Gene. 2019;704:113–20.
Frasquet M, Lupo V, Chumillas MJ, Vázquez-Costa JF, Espinós C, Sevilla T. Phenotypical features of two patients diagnosed with PHARC syndrome and carriers of a new homozygous mutation in the ABHD12 gene. J Neurol Sci. 2018;387:134–8.
Tingaud-Sequeira A, Raldúa D, Lavie J, Mathieu G, Bordier M, Knoll-Gellida A, et al. Functional validation of ABHD12 mutations in the neurodegenerative disease PHARC. Neurobiol Dis. 2017;98:36–51.
Yoshimura H, Hashimoto T, Murata T, Fukushima K, Sugaya A, Nishio SY et al. Novel ABHD12 mutations in PHARC patients: the differential diagnosis of deaf-blindness. The Annals of otology, rhinology, and laryngology. 2015;124 Suppl 1:77s-83s.
Nishiguchi KM, Avila-Fernandez A, van Huet RA, Corton M, Pérez-Carro R, Martín-Garrido E, et al. Exome sequencing extends the phenotypic spectrum for ABHD12 mutations: from syndromic to nonsyndromic retinal degeneration. Ophthalmology. 2014;121(8):1620–7.
Eisenberger T, Slim R, Mansour A, Nauck M, Nürnberg G, Nürnberg P, et al. Targeted next-generation sequencing identifies a homozygous nonsense mutation in ABHD12, the gene underlying PHARC, in a family clinically diagnosed with Usher syndrome type 3. Orphanet J Rare Dis. 2012;7:59.
Corriols-Noval P, López Simón EC, Cadiñanos J, Diñeiro M, Capín R, González Aguado R et al. Clinical Impact of Genetic Diagnosis of Sensorineural Hearing Loss in Adults. Otology & neurotology: official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2022;43(10):1125-36.
Uhlén M, Fagerberg L, Hallström BM, Lindskog C, Oksvold P, Mardinoglu A, et al. Proteomics. Tissue-based map of the human proteome. Volume 347. New York, NY: Science; 2015. p. 1260419. 6220.
Chatterjee S, Agrawal D, Agrawal D, Parchand SM, Sahu A. Cataract surgery in retinitis pigmentosa. Indian J Ophthalmol. 2021;69(7):1753–7.
Blankman JL, Long JZ, Trauger SA, Siuzdak G, Cravatt BF. ABHD12 controls brain lysophosphatidylserine pathways that are deregulated in a murine model of the neurodegenerative disease PHARC. Proc Natl Acad Sci USA. 2013;110(4):1500–5.
Ogasawara D, Ichu TA, Vartabedian VF, Benthuysen J, Jing H, Reed A, et al. Selective blockade of the lyso-PS lipase ABHD12 stimulates immune responses in vivo. Nat Chem Biol. 2018;14(12):1099–108.
Singh S, Kamat SS. The loss of enzymatic activity of the PHARC-associated lipase ABHD12 results in increased phagocytosis that causes neuroinflammation. Eur J Neurosci. 2021;54(10):7442–57.
Savinainen JR, Saario SM, Laitinen JT. The serine hydrolases MAGL, ABHD6 and ABHD12 as guardians of 2-arachidonoylglycerol signalling through cannabinoid receptors. Acta Physiologica (Oxford England). 2012;204(2):267–76.
Navia-Paldanius D, Savinainen JR, Laitinen JT. Biochemical and pharmacological characterization of human α/β-hydrolase domain containing 6 (ABHD6) and 12 (ABHD12). J Lipid Res. 2012;53(11):2413–24.
Acknowledgements
We are so grateful to the family members for their collaboration in this study.
Funding
This work was supported by Iran University of Medical Sciences, Tehran, Iran (Grant Number: 1400-2-22-21218). The funding bodies played no role in the study design, data collection and analysis, decision to publish and writing of the manuscript.
Author information
Authors and Affiliations
Contributions
AD, enrolled the patient and contributed to clinical diagnoses and report writing, proved manuscript final version; MG, Study design, enrolled the patient and contributed to clinical diagnoses and report writing, data analysis and interpretation, revising the manuscript; MF, enrolled the patient and contributed to clinical diagnoses and report writing, proved manuscript final version; KGF, enrolled the patient and contributed to clinical diagnoses and report writing, revising the manuscript, proved manuscript final version; MV, enrolled the patient and contributed to clinical diagnoses and report writing, revising the manuscript, proved manuscript final version; NA, enrolled the patient and contributed to clinical diagnoses and report writing, proved manuscript final version; MZ, performed experiments, manuscript preparation; MAGH, data analysis and interpretation, proved manuscript final version; MF, Study design, enrolled the patient and contributed to clinical diagnoses, data analysis and interpretation, manuscript preparation, proved manuscript final version. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance to the guidelines of the Declaration of Helsinki, and approved by the ethics committee of Iran University of Medical Sciences (Tehran, Iran). (Approval number: IR.IUMS.REC.1400.862). Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
Written informed consent for publication of clinical details and clinical images was obtained from the legal guardians.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Daneshi, A., Garshasbi, M., Farhadi, M. et al. Genetic insights into PHARC syndrome: identification of a novel frameshift mutation in ABHD12. BMC Med Genomics 16, 235 (2023). https://doi.org/10.1186/s12920-023-01682-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12920-023-01682-w