Abstract
Background
Despite many systematic reviews and meta-analyses examining the associations of pregnancy complications with risk of type 2 diabetes mellitus (T2DM) and hypertension, previous umbrella reviews have only examined a single pregnancy complication. Here we have synthesised evidence from systematic reviews and meta-analyses on the associations of a wide range of pregnancy-related complications with risk of developing T2DM and hypertension.
Methods
Medline, Embase and Cochrane Database of Systematic Reviews were searched from inception until 26 September 2022 for systematic reviews and meta-analysis examining the association between pregnancy complications and risk of T2DM and hypertension. Screening of articles, data extraction and quality appraisal (AMSTAR2) were conducted independently by two reviewers using Covidence software. Data were extracted for studies that examined the risk of T2DM and hypertension in pregnant women with the pregnancy complication compared to pregnant women without the pregnancy complication. Summary estimates of each review were presented using tables, forest plots and narrative synthesis and reported following Preferred Reporting Items for Overviews of Reviews (PRIOR) guidelines.
Results
Ten systematic reviews were included. Two pregnancy complications were identified. Gestational diabetes mellitus (GDM): One review showed GDM was associated with a 10-fold higher risk of T2DM at least 1 year after pregnancy (relative risk (RR) 9.51 (95% confidence interval (CI) 7.14 to 12.67) and although the association differed by ethnicity (white: RR 16.28 (95% CI 15.01 to 17.66), non-white: RR 10.38 (95% CI 4.61 to 23.39), mixed: RR 8.31 (95% CI 5.44 to 12.69)), the between subgroups difference were not statistically significant at 5% significance level. Another review showed GDM was associated with higher mean blood pressure at least 3 months postpartum (mean difference in systolic blood pressure: 2.57 (95% CI 1.74 to 3.40) mmHg and mean difference in diastolic blood pressure: 1.89 (95% CI 1.32 to 2.46) mmHg). Hypertensive disorders of pregnancy (HDP): Three reviews showed women with a history of HDP were 3 to 6 times more likely to develop hypertension at least 6 weeks after pregnancy compared to women without HDP (meta-analysis with largest number of studies: odds ratio (OR) 4.33 (3.51 to 5.33)) and one review reported a higher rate of T2DM after HDP (hazard ratio (HR) 2.24 (1.95 to 2.58)) at least a year after pregnancy. One of the three reviews and five other reviews reported women with a history of preeclampsia were 3 to 7 times more likely to develop hypertension at least 6 weeks postpartum (meta-analysis with the largest number of studies: OR 3.90 (3.16 to 4.82) with one of these reviews reporting the association was greatest in women from Asia (Asia: OR 7.54 (95% CI 2.49 to 22.81), Europe: OR 2.19 (95% CI 0.30 to 16.02), North and South America: OR 3.32 (95% CI 1.26 to 8.74)).
Conclusions
GDM and HDP are associated with a greater risk of developing T2DM and hypertension. Common confounders adjusted for across the included studies in the reviews were maternal age, body mass index (BMI), socioeconomic status, smoking status, pre-pregnancy and current BMI, parity, family history of T2DM or cardiovascular disease, ethnicity, and time of delivery. Further research is needed to evaluate the value of embedding these pregnancy complications as part of assessment for future risk of T2DM and chronic hypertension.
Similar content being viewed by others
Background
Pregnancy complications affect at least 30% of pregnancies and are among the leading causes of death in pregnancy [1, 2]. Physiological changes in the mother’s body during pregnancy that include increased cardiac output, a greater inflammatory response and metabolic abnormalities related to insulin resistance [3,4,5,6], can lead to some of these complications such as hypertensive disorders in pregnancy (HDP) and gestational diabetes mellitus (GDM). HDP affects between 3 and 10% of pregnancies and is the third cause of maternal mortality globally [1, 7, 8]. GDM affects around 7–10% of pregnancies globally and can lead to a higher incidence of still births and large for gestational-age babies [9].
Many of the pregnancy complications have an effect on the mother’s health and wellbeing beyond pregnancy. In a recent umbrella review, pregnancy-related complications were related to health conditions such as cardiovascular diseases [10], and results from systematic reviews have shown HDP and GDM were associated with risk of both T2DM and hypertension [11,12,13,14,15,16,17]. Although umbrella reviews that have synthesised the risk of hypertension and T2DM in women with a history of preeclampsia and GDM have been published [18,19,20], synthesis of the evidence for other pregnancy complications and a comprehensive review of the spectrum of HDP is lacking. Furthermore, there are new systematic reviews since the publication of these reviews and therefore these umbrella reviews need updating. The synthesis of this information would be beneficial to women, clinicians and other healthcare stakeholders to develop strategies to reduce the risk of future cardio-metabolic conditions in the postpartum period, a period which has been identified as a potential window of opportunity to prevent conditions associated with a history of pregnancy complications such as cardiovascular disease and diabetes [2, 21, 22].
This review aims to identify, appraise, synthesise, and consolidate evidence from systematic reviews and meta-analyses that have assessed the association between pregnancy-related complications and risk of post-partum hypertension and T2DM.
Methods
The umbrella review was reported following Preferred Reporting Items for Overviews of Reviews (PRIOR) guidelines [23]. We also registered the protocol prior to the review in PROSPERO (registration No. CRD42022323718) and the protocol has undergone peer review [24].
Exposures, comparator, and outcomes
Table 1 shows the pregnancy complications (exposures) we identified through discussion within the MuM-PreDiCT consortium [25] experts.
The comparator group was women who did not have the pregnancy complication of interest. The outcomes were T2DM and hypertension, diagnosed any time after pregnancy.
Inclusion criteria
We included systematic reviews with or without meta-analysis investigating the association between any of the exposures defined previously and any of the outcomes defined previously in women with a history of pregnancy. We excluded narrative reviews, literature reviews, commentaries, conference abstracts, genetic studies and reviews looking at association between the exposures and T2DM and hypertension which were diagnosed during pregnancy.
Search strategy
We searched Ovid Medline, Embase and Cochrane Database of Systematic Reviews from inception until 26 September 2022. There was no language restriction. We developed the search strategy around the key terms presented in Table 1.
We also limited the search to systematic reviews and meta-analyses using appropriate search filters and terms [26]. In addition, we searched the references of identified systematic reviews for further studies. The detailed search strategy for Ovid Medline database is provided in Additional file 1: Table S1. The search strategy was adapted for searches conducted in Embase and Cochrane databases.
Study selection and data extraction
Two reviewers (SW and MS) independently reviewed all titles and abstracts identified by the search using Endnote and Covidence. Articles were included for full-text review if they met the inclusion criteria defined previously. In the case where there were any disagreements, these were resolved through discussion and where necessary with consultation with a third reviewer (FC). Data was extracted by the two reviewers independently using a data extraction form developed for this umbrella review. Table 1 presents information extracted from systematic reviews:
The form used for the data extraction was adapted from the Joanna Briggs Institute and is provided in Additional file 1: Table S2.
Quality assessment
Methodological quality was assessed independently by two reviewers (SW and MS) using the AMSTAR 2 (A Measurement Tool to Assess Systematic Reviews) checklist [27]. In the case where there were any disagreements, these were resolved through discussion and where necessary through discussion with a third reviewer (FC). Seven of the sixteen items in the checklist are considered critical in determining the validity of a review [3]. The seven critical items are as follows: whether the review registered the protocol; whether the literature search was comprehensive; reasons for excluding individual studies were provided; risk of bias for individual studies was assessed (using recommended tools such as the Risk Of Bias In Non-randomized Studies of Interventions I (ROBINS-I) tool [28], Quality In Prognosis Studies (QUIPS) tool [29] or The Newcastle–Ottawa Scale (NOS) [30]); appropriate meta-analytical methods were used; whether the interpretation of results considered risk of bias in individual studies; and whether publication bias was assessed. We rated the reviews using gradings that are recommended by the AMSTAR 2 checklist authors: critically low, where more than one of the critical items was not satisfied with or without non-critical items being satisfied; low, where one critical item was not satisfied with or without non-critical items unsatisfied; moderate, where all critical items were satisfied and more than one non-critical items were not met; high, where all critical items were satisfied with no more than one non-critical item not met.
Overlapping and outdated reviews
Two or more reviews that evaluated the same exposure(s) and outcome(s) were considered to be potentially overlapping if they included the same sets of primary studies [31, 32]. The degree of overlap was quantified by generating a citation matrix with systematic reviews as the columns and primary studies as the rows for each exposure-outcome combination of interest [32, 33]. A measure of overlap, the corrected covered area (CCA) was then calculated using the formula below,
where N represents the number of publications included in evidence synthesis, r is the number of rows, and c is the number of columns. Overlap was considered very high if CCA was greater than 15%, high if between 11 and 15%, moderate if between 6 and 10% and slight if between 0 and 5% [32]. We used the following criteria to manage overlap between reviews [34,35,36]: (1) where the overlap occurred between Cochrane and non-Cochrane reviews, the Cochrane review was selected as previous studies have shown the evidence from Cochrane reviews is of higher quality [35]; (2) where CCA was more than 11%, and neither of the reviews was a Cochrane review, preference was given to the review that met the following criteria: (i) had highest AMSTAR 2 rating and the rating was moderate or higher; (ii) was most recent; had conducted a meta-analysis or provided pooled summary estimates; and (iii) had the greatest sample size (including both the number of studies and participants); (3) where CCA was less than 10%, all reviews were retained and the findings compared.
Data synthesis
For associations that were reported in only one review, we used the effect size reported in the original meta-analysis (i.e. hazard ratio (HR), relative risk (RR), odds ratio (OR), or mean difference (MD)). For associations that were reported in more than one included review, we estimated ORs for each review using the reported data (i.e. number of controls, exposed and events in the included studies) to enable comparison across reviews [37]. Additionally, we performed a meta-analysis of primary studies included in the reviews after excluding duplicate studies across the reviews to obtain a summary estimate. We extracted information on the variables adjusted for in primary studies included in each systematic review. We extracted the definitions of exposures and outcomes provided in the corresponding systematic review or meta-analysis and reported them in a table. We also extracted data on the follow-up time of assessment of outcomes reported in each review and the confounders adjusted for in the primary studies included in each systematic review.
For each meta-analysis of the primary studies, summary effect size estimate and 95% confidence intervals (CI) were estimated using the inverse variance random-effects model using the DerSimonian and Laird method [38, 39]. Heterogeneity among included studies in each meta-analysis was assessed using the Cochrane Q test and reported using tau2 and inconsistency in the estimates was reported using I2 [40]. The 95% prediction interval (95% PI) for each meta-analysis was also estimated to evaluate the expected uncertainty in the effect estimates for a study evaluating the same association [41, 42]. Egger’s test was used to quantify small-study effects bias if more than 10 studies were included in the meta-analysis [43]. For studies where there were no outcomes in the exposed or control group, a continuity correction using 0.5 was applied to avoid any division by zero [44].
All statistical analyses were conducted using R [45], RStudio [46] and the meta package [47].
Deviations from protocol
There were no deviations from the protocol.
Patient and public involvement
Patients and the public involvement representatives of the MuM-PreDiCT consortium [25] were involved in selecting the pregnancy complications. We plan to engage patient and public representatives, local policy makers in public health, and local charities (e.g. British Heart Foundation) to disseminate the results of the review in conferences and on social media.
Results
Literature search
The literature search yielded 6743 articles. After removing duplicates and screening titles and abstracts, 79 full-text articles were selected for further review. Fifty-nine articles were excluded after full-text screening, leaving 20 reviews included for evaluation. The list of excluded articles with reasons is provided in Additional file 1: Table S3 [13, 18,19,20, 48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110].
Methodological quality
Using the AMSTAR 2 rating criteria, 8 of the 20 reviews were rated high quality [14, 15, 105, 111,112,113,114,115], 4 were moderate quality [16, 17, 116, 117], 5 were rated low quality [13, 102, 104, 106] and 3 were rated as critically low quality [99, 108, 110]. Assessment of the quality of the systematic reviews is presented in Additional file 1: Table S4. The three reviews of critically low quality were excluded from further evaluation, resulting in 17 reviews being taken forward for further evaluation.
Overlapping and non-overlapping reviews
Ten of the 17 remaining reviews included similar sets of primary studies [13, 102, 104,105,106,107, 111]. These included the associations of two pregnancy complications (GDM and HDP) with risk of T2DM at any time after pregnancy. Among the overlapping reviews, the review selected was of moderate or high quality, was the latest and had the highest number of included primary studies, as described in the methods section.
Using the criteria for handling overlapping reviews, two of the 10 reviews with overlapping sets of primary studies were selected (one review for the association between GDM and T2DM and the second for the association between HDP and T2DM) [114, 115] and the other eight were considered for exclusion. The review selected for the association between GDM, and T2DM had the most primary studies among the overlapping reviews with at least moderate quality [114]. The second review for the association between HDP and T2DM was the latest, of high quality and had the most primary studies [115]. Additional file 1: Tables S5a to S5g show the citation matrices with the degree of overlap between reviews for the association between the two pregnancy complications and T2DM. Further, Additional file 1: Table S6 shows the general characteristics of reviews with overlapping primary studies and the calculated CCA with accompanying reasons for including or excluding them. Out of the eight reviews considered for exclusion, one review evaluated both T2DM and hypertension and was eligible for inclusion for the association between preeclampsia and hypertension and was therefore retained [117]. Therefore, in total seven reviews were excluded resulting in ten reviews remaining for further analysis. The list of the excluded reviews due to the overlap is provided in Additional file 1: Table S7 [102,103,104,105,106,107, 111].
Study characteristics of reviews with non-overlapping studies
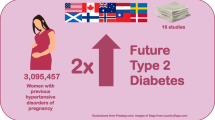
In total, there were 10 systematic reviews included in this umbrella review. The flow diagram of these studies is shown in Fig. 1 below, and the general characteristics of the included reviews are provided in Table 2 below. The systematic reviews assessed two pregnancy complications. These were GDM and hypertensive disorders of pregnancy (including chronic hypertension, gestational hypertension, preeclampsia, eclampsia and HELLP syndrome). Additional file 1: Table S8 [14,15,16,17, 112,113,114,115,116,117] includes the definitions of the exposures and the extent of other confounders adjusted for in the reviews included. The number of women included in the systematic reviews ranged between 1,332,373 and 3,095,457 for studies relating to postpartum T2DM while for hypertension it was between 8041 and 2,711,443 (Table 2).
Summary findings
Overall and subgroup estimates alongside 95% CI for the associations of each pregnancy complication with T2DM and hypertension from the meta-analyses are shown in Table 3 below and the findings from narrative synthesis are shown in Additional file 1: Table S9 [15, 115]. A forest plot of the overall estimates is also provided in Fig. 2. Further estimates from subgroup analysis and publication bias measures are presented in Additional file 1: Table S10 [14,15,16,17, 112,113,114,115,116,117].
Forest plot of overall adjusted and unadjusted estimates of meta-analyses from systematic reviews that investigated the association between pregnancy complications and risk of future T2DM and hypertension. § Estimate from studies that adjusted for potential confounders. First vertical line is the reference point (zero) for the mean difference estimates. The second vertical line is the reference line (one) for the relative risk, odds ratio and hazard ratio estimates. Hazard ratios should be interpreted as an increase in the rate of the outcome while odds ratios should be interpreted as increase in the odds of the outcome and relative risk as an increase in the risk of the outcome in exposed compared to controls. For the association between hypertensive disorders of pregnancy (HDP) and hypertension, there were three reviews with non-overlapping associations and the estimates for each review are presented [14, 112, 113]. Similarly, five estimates from five reviews with non-overlapping associations between preeclampsia and hypertension are provided [16, 17, 112, 116, 117]. aHDP included gestational hypertension and preeclampsia, including HELLP (haemolysis, elevated liver enzymes, lowered platelets) syndrome and eclampsia, and excluded pre-existing chronic hypertension. bHDP included gestational hypertension and preeclampsia and excluded pre-existing chronic hypertension. Common adjustment factors across the studies were maternal age, body mass index, socioeconomic status, smoking status, pre-pregnancy and current BMI, parity, ethnicity and time of delivery Abbreviations: GDM gestational diabetes mellitus, NA not applicable, 95% PI 95% prediction interval, Egger’s p Egger test p value
Pregnancy complications associated with T2DM
GDM
In a review of 20 primary studies including 1,332,373 women, the risk of T2DM at least 12 months after delivery was almost 10-fold greater in women with a history of GDM compared to healthy controls (RR 9.51, 95% CI 7.14 to 12.67, tau2 = 0.23) [114]. The summary estimate is based on unadjusted estimates (Table 3 and Fig. 2). Common confounders adjusted for by primary studies included in the review were maternal age, body mass index (BMI), family history of T2DM, parity, ethnicity, and socioeconomic status. All confounders adjusted for are presented in Additional file 1: Table S8, Tables S8a-S8f and Fig.S1.
Subgroup and sensitivity analysis
Analyses showed the association of GDM with risk of T2DM compared to those without GDM for women in subgroups defined by ethnicity remained elevated with the highest relative risk in women of white ethnicity and lowest in women of mixed ethnicity (white: RR 16.28, 95% CI 15.01 to 17.66, studies = 6, tau2 = 0); non-white: RR 10.38, 95% CI 4.61 to 23.39, studies = 4, tau2 = 0.46; mixed populations: RR 8.31, 95% CI 5.44 to 12.69, studies = 10, tau2 = 0.34). There were no statistically significant differences between the subgroups (white ethnicity vs mixed ethnicity, p-value = 0.26 and white ethnicity vs non-white ethnicity, p-value = 0.54). The association between GDM with risk of T2DM was attenuated over a longer period of follow-up (1 to 5 years: RR 17.06, 95% CI 8.95 to 32.55, studies = 6, tau2 = 0; more than 5 years and up to 10 years: RR 10.42, 95% CI 5.68 to 19.11, studies = 7, tau2 = 0.52; more than 10 years: RR 8.09, 95% CI 4.34 to 15.08, studies = 7, tau2 = 0.52). There were no statistically significant differences between the subgroups (1–5 years vs > 5–10 years, p-value = 0.63; 1–5 years vs > 10 years, p-value = 0.38). Subgroup estimates are provided in Table 3.
HDP
In the selected review, prior HDP (defined as gestational hypertension and preeclampsia, including HELLP (haemolysis, elevated liver enzymes, lowered platelets) syndrome and eclampsia) was associated with a higher rate of developing T2DM at least 1 year after delivery compared to those without those conditions (HR 2.24, 95% CI 1.95 to 2.58, studies = 15, tau2 = 0.10) (Table 3 and Fig. 2) [115]. The summary estimate is based on adjusted estimates.” The meta-analysis included a total of 3,095,457 women. Common factors adjusted for in the included primary studies include maternal age, BMI, socioeconomic status, smoking status, parity, ethnicity and time of delivery. All confounders adjusted for are presented in Additional file 1: Table S8, Table S8a-S8f and Fig.S1. A narrative review also reported that women with prior HDP developed T2DM at earlier ages than women without the pregnancy complication [115, 118] (Additional file 1: Table S9 [115]).
Subgroup and sensitivity analysis
Studies with shorter follow-up duration showed a higher rate of T2DM (less than 20 years of follow-up: HR 2.64, 95% CI 2.23 to 3.12, studies = 7; greater or equal to 20 years of follow-up: HR 1.34, 95% CI 1.20 to 1.50, studies = 2).
There was a dose–response relationship between HDP severity and future risk of T2DM (gestational hypertension: HR 2.19, 95% CI 1.69 to 2.84, studies = 7, tau2 = 0.07; preeclampsia: HR 2.56, 95% CI 2.02 to 3.24, studies = 11, tau2 = 0.23; preterm preeclampsia (preeclampsia that resulted in preterm birth < 37 weeks): HR 3.05, 95% CI 2.05 to 4.56, studies = 3, tau2 = 0.09). Subgroup estimates are provided in Table 3.
Pregnancy complications associated with hypertension
GDM
The included review showed that women with previous GDM have higher mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) any time after delivery compared to women without previous GDM (SBP: mean difference 2.47 mmHg, 95% CI 1.74 to 3.4, studies = 48, tau2 = 5.56); DBP: mean difference 1.89 mmHg, 95% CI 1.32 to 2.46, studies = 48, tau2 = 2.18). The summary estimates are based on unadjusted estimates (Table 3 and Fig. 2) [15]. BMI, parity, age, history of diabetes and other pregnancy complications were most adjusted for in included primary studies in the review. In the narrative synthesis of 12 primary studies, six reported higher mean DBP in women with previous GDM compared to the control group, with three studies showing statistical significance, and eight studies reported higher mean SBP with five studies showing statistical significance [15] Additional file 1: Table 9 [15].
Subgroup analysis
Further analysis by follow-up duration shows higher mean blood pressure in women with a history of GDM across different periods of follow-up, with the highest mean blood pressure observed for the period 5 to 10 years postpartum (DBP: < 1 year mean difference 2.48 mmHg, 95% CI 0.58 to 4.37; 1–5 years mean difference 1.37 mmHg, 95% CI 0.20 to 2.54; 5–10 years mean difference 7.17 mmHg, 95% CI 1.69 to 16.03; > 10 years mean difference 1.23 mmHg, 95% CI 1.03 to 1.96, SBP: < 1 year mean difference 3.47 mmHg, 95% CI 1.26 to 5.68; 1–5 years mean difference 2.26 mmHg, 95% CI 0.27 to 4.25; 5–10 years mean difference 3.96 mmHg, 95% CI 2.36 to 5.56; > 10 years mean difference 2.58 mmHg, 95% CI 1.05 to 4.11). Subgroup estimates are provided in Table 3.
HDP
Three reviews reported higher odds (3- to 6-fold higher) of hypertension in women with a history of HDP compared to women without a history of HDP [14, 112, 113]. Two of the three reviews defined HDP to include gestational hypertension and preeclampsia, excluding chronic hypertension [112, 113] while the third study defined HDP to include gestational hypertension, preeclampsia, eclampsia and HELLP syndrome (providing estimates with and without including chronic hypertension) [14].
In the two reviews, the odds of hypertension were significantly higher in the HDP group (OR 3.61, 95% CI 2.18 to 6.00, studies = 11, tau2 = 0.54, time = at least 1 year postpartum) and (OR 4.33, 95% CI 3.51 to 5.33, studies = 37, tau2 = 0.27, time = at least 6 weeks postpartum) and in the third review the reported risk remained higher between 6 weeks and 2 years postpartum both before excluding pre-existing chronic hypertension in the analysis (OR 6.28, 95% CI 4.18 to 9.43, studies = 15, tau2 = 0.24) and after excluding pre-existing chronic hypertension (OR 5.75, 95% CI 3.92 to 8.44, studies = 14, tau2 = 0.18) The summary estimate is based on unadjusted estimates (Table 3 and Fig. 2) [14]. Common confounders adjusted for in the primary studies included in the three reviews included age, ethnicity, socioeconomic status, BMI, family history of cardiovascular diseases, parity, history of diabetes mellitus and smoking status. The odds remained elevated after meta-analysing the primary studies that excluded chronic hypertension from the three systematic reviews (OR 4.26, 95% CI 3.54 to 5.12, studies = 53, tau2 = 0.29) (Additional file 1: Fig.S2).
On the specific types of HDP, six reviews reported between 3 and 10-fold higher in the odds of hypertension in women with a history of preeclampsia (OR 6.20, 95% CI 3.74 to 10.28, studies = 13, tau2 = 0.50; OR 3.90, 95% CI 3.16 to 4.82, studies = 30, tau2 = 0.13; OR 3.74, 95% CI 2.87 to 4.94, studies = 15, tau2 = 0.23; OR 3.19, 95% CI 1.52 to 6.70, studies = 13, tau2 = 1.35; OR 6.83, 95% CI 4.25 to 10.96, studies = 12, tau2 = 0.26; OR 3.76, 95% CI 2.87 to 4.94, studies = 12, tau2 = 0.03) (Table 3 and Fig. 2) [14, 16, 17, 112, 116, 117]. Mean blood pressure was higher in women with a history of preeclampsia compared to women without a history of the pregnancy complication (SBP: mean difference 8.28 mmHg, 95% CI 6.85 to 9.71, studies = 38, tau2 = 12.37; DBP: mean difference 6.79 mmHg, 95% CI 5.62 to 7.96, studies = 37, tau2 = 9.10) (Table 3 and Fig. 2) [16].
Subgroup and sensitivity analysis
Two reviews showed the risk of hypertension after HDP remained elevated but attenuated by follow-up; (first 6 months: OR 13.39, 95% CI 1.27 to 141.04, studies = 3, tau2 = 3.05; 6 to 12 months: OR 4.13, 95% CI 2.82 to 6.07, studies = 3, tau2 = 0.06; 1 to 2 years: OR 8.73, 95% CI 4.66 to 16.35, studies = 8, tau2 = 0.18) [14], and (less or equal to 5 years: OR 6.05, 95% CI 3.55 to 10.30, studies = 7, tau2 = 0.35; 6 to 10 years: OR 5.95, 95% CI 4.69 to 7.54, studies = 6, tau2 = 0.05; 11 to 15 years: OR 4.22, 95% CI 2.44 to 7.32, studies = 7, tau2 = 0.41; greater than 15 years: OR 2.44, 95% CI 1.93 to 3.08, studies = 2, tau2 = 0.02; Duration unspecified: OR 3.74, 95% CI 2.50 to 5.58, studies = 15, tau2 = 0.40) [113].
Further subgroup analysis in one of the reviews showed the odds of post-partum hypertension in women with a history of HDP compared to healthy controls differed in different continents with the lowest odds in North and South America (OR 2.11, 95% CI 1.42 to 3.14, studies = 5, tau2 = 0.12), highest in Europe (OR 5.52, 95% CI 3.01 to 10.14, studies = 3, tau2 = 0.17) and similar to the overall estimate in Asia (OR 4.26, 95% CI 1.05 to 17.21, studies = 3, tau2 = 1.30) [112]. The differences among the continents were statistically significant (p-value = 0.03).
On the specific types of HDP, two reviews reported differences in odds of postpartum hypertension after preeclampsia by follow-up periods; first review: (first 6 months: OR 43.95, 95% CI 5.72 to 338.04, studies = 2, tau2 = 0; 6–12 months: OR 4.46, 95% CI 2.76 to 7.21, studies = 3, tau2 = 0.10; 1–2 years: OR 8.91, 95% CI 4.33 to 18.33, studies = 7, tau2 = 0.28) [14], second review: (up to 60 months: OR 19.03, 95% CI 2.47 to 146.49, studies = 2, tau2 = 0; up to 60.1 to 180 months: OR 4.13, 95% CI 2.47 to 6.90, studies = 6, tau2 = 0.09; above 180 months: OR 3.41, 95% CI 2.41 to 4.82, studies = 4, tau2 = 0.01) [16]. The odds of postpartum hypertension after preeclampsia was greater in women from Asia (OR 7.54, 95% CI 2.49 to 22.81, studies = 3, tau2 = 0.45) compared to women in North and South America (OR 3.32, 95% CI 1.26 to 8.74, studies = 6, tau2 = 1.07) and Europe (OR 2.19, 95% CI 0.30 to 16.02, studies = 4, tau2 = 3.57). There is however a lot of uncertainty in the estimates as the confidence intervals were quite wide and comparisons were made across studies rather than within. The subgroup estimates are provided in Table 3.
Discussion
Findings
In summary, results from this umbrella review showed the risk of T2DM at least 12 months after delivery was nearly 10-fold greater in women with previous GDM compared to women without GDM. Furthermore, mean blood pressure was higher in women with a history of GDM. HDP were associated with a higher rate of T2DM, and the risk of developing hypertension was 3- to 4-fold higher in women with a history of HDP or preeclampsia. It is noteworthy that the risk of hypertension was greater in women who had severe hypertensive disorders of pregnancy (e.g. severe preeclampsia and a preterm birth).
Analysis by follow-up based on one systematic review showed the risk of T2DM and hypertension after HDP and GDM was greatest in studies with shorter follow-up periods compared to those with longer periods of follow-up. The risk of T2DM in women with a history of GDM was highest in women of white ethnicity and lowest in women of mixed ethnicity, while the risk of hypertension in women with a history of HDP was highest in Europe and lowest in North and South America. However, for preeclampsia the risk of hypertension was highest in women from Asia compared to women in the Americas and Europe.
Strengths and limitations
The umbrella review has the following strengths: registration of a protocol for the umbrella review prior to the start of the umbrella review; a comprehensive search of reviews in multiple databases; evaluation of the quality of the reviews using the recommended AMSTAR 2 checklist and including the quality of the reviews in the decision to include or exclude reviews in the evidence synthesis; assessment of overlap in reviews that included the same primary studies and reporting of relevant subgroup and sensitivity analyses.
The following limitations in the review could be considered in the interpretation of the results. Firstly, the number of participants, measures of heterogeneity and publication bias were not reported in some reviews. Secondly, some factors associated with the outcomes (e.g. ethnicity, lifestyle (diet, physical activity, smoking), family history of cardiovascular diseases etc.) were rarely included in the adjusted analyses. Thirdly, the strongest association between HDP and risk of hypertension was observed in the immediate post-partum period (< 6 months) in one systematic review. This may be an overestimate of risk and should be interpreted with caution because HDP may take up to 12 months to resolve [14, 119, 120]. Fourthly, although we obtained risk estimates for certain intervals of time in the postpartum period, it was difficult to obtain risk estimates at particular time points. Lastly, reviews on some pregnancy factors including miscarriage, pre-term birth and postnatal depression were not identified in the literature and hence not incorporated in this review.
Methodological issues
There is potential for significant heterogeneity attributable to various study characteristics (e.g. study design and quality) as well as residual confounding inherent in observational studies. There is potential for recall bias for some of the results where primary studies included self-reported data and also misclassification of cases due to differences in diagnostic criteria by included primary studies, for instance, there is a possibility of misclassification of hypertension as pre-eclampsia or gestational hypertension, leading to overestimation of the effect sizes. Estimates from subgroup analyses with fewer than four studies should be interpreted with caution as the precision of the estimates might be affected where the number of studies included in a meta-analysis is small and heterogeneity is high [121, 122], and may be biased by confounding from other study-level characteristics. A more informative way to examine differences in subgroups is by conducting an individual participant meta-analysis [123].
Comparison with other studies
Results from this review are consistent with previous research and guidelines showing that both HDP and GDM are associated with a higher risk of T2DM and hypertension. In 2018, a multiple exposure umbrella review for T2DM found one systematic review showing GDM was associated with almost 8-fold risk of T2DM [18], and in 2016, an umbrella review evaluating risk factors for vascular disease and mortality found two systematic reviews showing that both preeclampsia and gestational hypertension were associated with an elevated risk of hypertension [20]. A recent umbrella review which evaluated the relationship between preeclampsia and long-term maternal outcomes showed that preeclampsia was associated with a greater risk of developing both hypertension and diabetes mellitus [19].
Potential mechanisms of association
Shared genetic factors between GDM and T2DM have also been hypothesised to be the link between the two conditions. Meta-analyses on the relationship between common T2DM genetic variants and GDM found nine variants shared between the two conditions on genes that may be related to β-cell function, insulin resistance and glycolysis [66, 124].
The mechanism through which HDP increases T2DM and hypertension is not well understood [115, 116] but may be mediated through insulin resistance [4, 125]. HDP may be an early manifestation of underlying insulin resistance as a result of increased metabolic demands during pregnancy, similar to GDM. Besides insulin resistance, other shared risk factors of HDP with cardiovascular diseases such as obesity, hypertension, hyperlipidaemia, and renal dysfunction may explain the link between HDP and T2DM [106, 126].
Implications for practice, public health and future research
The findings of this review might help to increase awareness of the risk of these conditions to women and hence enable attendance at regular screening for hypertension and T2DM. Previous research has demonstrated risk factors for vascular conditions such as systolic blood pressure and total cholesterol reduced significantly for those who attended screening programmes for cardiovascular diseases [127].
Guidelines to prevent or mitigate the risk of future vascular conditions such as T2DM and hypertension recommend healthcare professionals to obtain detailed pregnancy history in women with a history of pregnancy complications to enable effective determination of the risk of future health conditions. The National Institute for Health and Care Excellence (NICE) guidelines recommend healthcare professionals to advise women with a history of HDP about their greater risk of hypertension and cardiovascular disease and encourage them to discuss with their GPs on ways to reduce the risk [128]. Avoiding smoking, maintaining a healthy lifestyle and a healthy weight are recommended in the guideline as potential interventions to reduce the risk of future hypertension. NICE guidelines also recommend risk assessment for T2DM in women with a history of GDM and no specific guidelines on risk assessment for women with a history of HDP [129].
Risk prediction models for diabetes (e.g. QDiabetes) and hypertension (e.g. Framingham score) in the general population have also been developed to calculate the risk of developing these conditions. However, QDiabetes does not include HDP and the Framingham score does not include both HDP and GDM in the risk equations [130, 131]. Further research is needed to quantify the prognostic value of adding a history of these pregnancy complications as predictors to these risk prediction models specifically in the postpartum period in the low-risk population of women of reproductive age who have a history of pregnancy.
Conclusions
In summary, evidence from this umbrella review of systematic reviews showed strong and consistent evidence that women with previous GDM have a much greater risk of developing T2DM and higher blood pressure, and women with HDP had a greater risk of developing hypertension and T2DM. Further research is required to explain the underlying mechanisms of these associations and to evaluate whether adding these pregnancy complications to current risk prediction models improves the prediction of T2DM and hypertension in women with a history of pregnancy.
Availability of data and materials
All data are included in this manuscript and its supplementary information files.
Abbreviations
- AMSTAR2:
-
A MeaSurement Tool to Assess systematic Reviews 2
- BMI:
-
Body mass index
- CCA:
-
Corrected covered area
- CI:
-
Confidence intervals
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- GDM:
-
Gestational diabetes mellitus
- GP:
-
General practitioner
- HDP:
-
Hypertensive disorders of pregnancy
- HELLP:
-
Hemolysis, elevatated liver enzymes, and low platelets
- HR:
-
Hazard ratio
- MD:
-
Mean difference
- MuM-PreDiCT:
-
Multimorbidity in Pregnancy: Determinants, clusters, Consequences and Trajectories
- NHMRC:
-
National Health and Medical Research Council
- NHS:
-
National Health Service
- NICE:
-
The National Institute for Health and Care Excellence
- NOS:
-
The Newcastle–Ottawa Scale
- OR:
-
Odds ratio
- PRIOR:
-
Preferred Reporting Items for Overviews of Reviews
- QUIPS:
-
Quality In Prognosis Studies
- ROBINS-I:
-
Risk Of Bias In Non-randomized Studies of Interventions I
- RR:
-
Relative risk
- SBP:
-
Systolic blood pressure
- T2DM:
-
Type 2 diabetes mellitus
References
Fraser A, Nelson SM, Macdonald-Wallis C, Cherry L, Butler E, Sattar N, et al. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the avon longitudinal study of parents and children. Circulation. 2012;125(11):1367–80.
Rich-Edwards JW, Fraser A, Lawlor DA, Catov JM. Pregnancy characteristics and women’s future cardiovascular health: an underused opportunity to improve women’s health? Epidemiol Rev. 2014;36(1):57–70.
Sattar N, Greer IA. Pregnancy complications and maternal cardiovascular risk: opportunities for intervention and screening? BMJ. 2002;325(7356):157–60.
Seely EW, Solomon CG. Insulin resistance and its potential role in pregnancy-induced hypertension. J Clin Endocrinol Metab. 2003;88(6):2393–8.
Bosio PM, McKenna PJ, Conroy R, O’Herlihy C. Maternal central hemodynamics in hypertensive disorders of pregnancy. Obstet Gynecol. 1999;94(6):978–84.
Redman CW, Sacks GP, Sargent IL. Preeclampsia: an excessive maternal inflammatory response to pregnancy. Am J Obstet Gynecol. 1999;180(2):499–506.
Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertens Res. 2017;40(3):213–20.
Obstetricians ACo, Gynecologists. Gestational hypertension and preeclampsia: ACOG Practice Bulletin, number 222. Obstet Gynecol. 2020;135(6):e237–60.
Behboudi-Gandevani S, Amiri M, Bidhendi Yarandi R, Ramezani TF. The impact of diagnostic criteria for gestational diabetes on its prevalence: a systematic review and meta-analysis. Diabetol Metab Syndr. 2019;11(1):1–18.
Okoth K, Chandan JS, Marshall T, Thangaratinam S, Thomas GN, Nirantharakumar K, et al. Association between the reproductive health of young women and cardiovascular disease in later life: umbrella review. BMJ (Clinical research ed). 2020;371:m3502.
Wilkins-Haug L, Celi A, Thomas A, Frolkis J, Seely EW. Recognition by women’s health care providers of long-term cardiovascular disease risk after preeclampsia. Obstet Gynecol. 2015;125(6):1287–92.
Young B, Hacker MR, Rana S. Physicians’ knowledge of future vascular disease in women with preeclampsia. Hypertens Pregnancy. 2012;31(1):50–8.
Bellamy L, Casas J-P, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet (London, England). 2009;373(9677):1773–9.
Giorgione V, Ridder A, Kalafat E, Khalil A, Thilaganathan B. Incidence of postpartum hypertension within 2 years of a pregnancy complicated by pre-eclampsia: a systematic review and meta-analysis. BJOG. 2021;128(3):495–503.
Pathirana MM, Lassi Z, Ali A, Arstall M, Roberts CT, Andraweera PH. Cardiovascular risk factors in women with previous gestational diabetes mellitus: a systematic review and meta-analysis. Rev Endocr Metab Disord. 2021;22(4):729–61.
Alonso-Ventura V, Li Y, Pasupuleti V, Roman YM, Hernandez AV, Perez-Lopez FR. Effects of preeclampsia and eclampsia on maternal metabolic and biochemical outcomes in later life: a systematic review and meta-analysis. Metabolism. 2020;102:154012.
Bellamy L, Casas J-P, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS One. 2018;13(3):e0194127.
Pittara T, Vyrides A, Lamnisos D, Giannakou K. Pre-eclampsia and long-term health outcomes for mother and infant: an umbrella review. BJOG. 2021;128(9):1421–30.
Leslie MS, Briggs LA. Preeclampsia and the risk of future vascular disease and mortality: a review. J Midwifery Womens Health. 2016;61(3):315–24.
Haas DM, Ehrenthal DB, Koch MA, Catov JM, Barnes SE, Facco F, et al. Pregnancy as a window to future cardiovascular health: design and implementation of the nuMoM2b heart health study. Am J Epidemiol. 2016;183(6):519–30.
Adam S, McIntyre HD, Tsoi KY, Kapur A, Ma RC, Dias S, et al. Pregnancy as an opportunity to prevent type 2 diabetes mellitus: FIGO Best Practice Advice. Int J Gynecol Obstet. 2023;160:56–67.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Singh M, Crowe F, Thangaratinam S, Abel KM, Black M, Okoth K, et al. Association of pregnancy complications/risk factors with the development of future long-term health conditions in women: overarching protocol for umbrella reviews. BMJ Open. 2022;12(12):e066476.
MuM-PreDiCT Group. Multimorbidity in pregnancy: determinants, clusters, consequences and trajectories. Available from: https://mumpredict.org. Accessed 20 Feb 2023.
Lee E, Dobbins M, DeCorby K, McRae L, Tirilis D, Husson H. An optimal search filter for retrieving systematic reviews and meta-analyses. BMC Med Res Methodol. 2012;12(1):1–11.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute; 2000. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):1–6.
Pieper D, Antoine S-L, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich A-B. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. 2018;93:9–24.
Okoth K, Chandan JS, Marshall T, Thangaratinam S, Thomas GN, Nirantharakumar K, et al. Association between the reproductive health of young women and cardiovascular disease in later life: umbrella review. BMJ. 2020;371:m3502.
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):1–8.
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):1–14.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. BMJ Ment Health. 2018;21(3):95–100.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127(9):820–6.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549.
Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc A Stat Soc. 2009;172(1):137–59.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Chichester: Wiley; 2019.
R Core Team. R: a language and environment for statistical computing; 2022. Available from: https://www.R-project.org/.
RStudio Team. RStudio: integrated development environment for R; 2022. Available from: http://www.rstudio.com/.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. BMJ Ment Health. 2019;22(4):153–60.
Bundhun PK, Soogund MZS, Huang F. Impact of systemic lupus erythematosus on maternal and fetal outcomes following pregnancy: a meta-analysis of studies published between years 2001–2016. J Autoimmun. 2017;79:17–27.
Di Cianni G, Ghio A, Resi V, Volpe L. Gestational diabetes mellitus: an opportunity to prevent type 2 diabetes and cardiovascular disease in young women. Womens Health. 2010;6(1):97–105.
Edstedt Bonamy AK, Parikh NI. Predicting women’s future cardiovascular health from pregnancy complications. Curr Cardiovasc Risk Rep. 2013;7(3):173–82.
Gortner L. Intrauterine growth restriction and risk for arterial hypertension: a causal relationship? J Perinat Med. 2007;35(5):361–5.
Guo J, Chen J-L, Whittemore R, Whitaker E. Postpartum lifestyle interventions to prevent type 2 diabetes among women with history of gestational diabetes: a systematic review of randomized clinical trials. J Womens Health (2002). 2016;25(1):38–49.
Hutchesson M, Campbell L, Leonard A, Vincze L, Shrewsbury V, Collins C, et al. Do modifiable risk factors for cardiovascular disease post-pregnancy influence the association between hypertensive disorders of pregnancy and cardiovascular health outcomes? A systematic review of observational studies. Pregnancy Hypertens. 2022;27:138–47.
Jenabi E, Afshari M, Khazaei S. The association between preeclampsia and the risk of metabolic syndrome after delivery: a meta-analysis. J Matern Fetal Neonatal Med. 2021;34(19):3253–8.
Kramer CK, Campbell S, Retnakaran R. Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Diabetologia. 2019;62(6):905–14.
Lao TT. The mother - the long-term implications on metabolic and cardiovascular complications. Best Pract Res Clin Obstet Gynaecol. 2015;29(2):244–55.
Lassi ZS, Bhutta ZA. Risk factors and interventions related to maternal and pre-pregnancy obesity, pre-diabetes and diabetes for maternal, fetal and neonatal outcomes: a systematic review. Expert Rev Obstet Gynecol. 2013;8(6):639–60.
Leya M, Armstrong LL, Scheftner DA, Lowe WL, Hayes MG, Lowe LP, et al. Association of plasma glucose and type 2 diabetes susceptibility genes with gestational diabetes. Diabetes. 2013;62(SUPPL. 1):A431.
Li M, Rawal S, Hinkle S, Liu S, Tekolaayele F, Zhang C. Sex hormone-binding globulin, cardiometabolic biomarkers, and gestational diabetes-a longitudinal pregnancy cohort study and a meta-analysis. Diabetes. 2018;67(Supplement 1):A384–5.
Li P, Shan Z, Zhou L, Xie M, Bao W, Zhang Y, et al. Parity and risk of type 2 diabetes: a systematic review and dose-response meta-analysis. Eur J Endocrinol. 2016;175(5):R231–45.
Li S, Xi B. Preterm birth is associated with risk of essential hypertension in later life. Int J Cardiol. 2014;172(2):e361–3.
Li W, Ruan W, Lu Z, Wang D. Parity and risk of maternal cardiovascular disease: a dose-response meta-analysis of cohort studies. Eur J Prev Cardiol. 2019;26(6):592–602.
Liao L, Deng Y, Zhao D. Association of low birth weight and premature birth with the risk of metabolic syndrome: a meta-analysis. Front Pediatr. 2020;8:405.
Lin Z, Wang Y, Zhang B, Jin Z. Association of type 2 diabetes susceptible genes GCKR, SLC30A8, and FTO polymorphisms with gestational diabetes mellitus risk: a meta-analysis. Endocrine. 2018;62(1):34–45.
Liu J, Song G, Zhao G, Meng T. Lack of association between IGF2BP2 rs4402960 polymorphism and gestational diabetes mellitus: a case-control study, meta-analysis and trial sequential analysis. Biosci Rep. 2020;40(7):BSR20200990.
Mao H, Li Q, Gao S. Meta-analysis of the relationship between common type 2 diabetes risk gene variants with gestational diabetes mellitus. PLoS One. 2012;7(9):e45882.
McIntyre HD, Kapur A, Divakar H, Hod M. Gestational diabetes mellitus-innovative approach to prediction, diagnosis, management, and prevention of future NCD-mother and offspring. Front Endocrinol. 2020;11:614533.
Minhas AS, Ying W, Ogunwole SM, Miller M, Zakaria S, Vaught AJ, et al. The association of adverse pregnancy outcomes and cardiovascular disease: current knowledge and future directions. Curr Treat Options Cardiovasc Med. 2020;22(12):61.
Moore LE, Voaklander B, Savu A, Yeung RO, Ryan E, Chojecki D, et al. Association between the antepartum oral glucose tolerance test and the risk of future diabetes mellitus among women with gestational diabetes: a systematic review and meta-analysis. J Diabetes Complications. 2021;35(4):107804.
Morton S, Kirkwood S, Thangaratinam S. Interventions to modify the progression to type 2 diabetes mellitus in women with gestational diabetes: a systematic review of literature. Curr Opin Obstet Gynecol. 2014;26(6):476–86.
Neiger R. Long-term effects of pregnancy complications on maternal health: a review. J Clin Med. 2017;6(8):76.
Noctor E. Risk associated with development of type 2 DM in gestational diabetes. Clin Chem Lab Med. 2019;57(8):eA105.
Park K, Minissian MB, Wei J, Saade GR, Smith GN. Contemporary clinical updates on the prevention of future cardiovascular disease in women who experience adverse pregnancy outcomes. Clin Cardiol. 2020;43(6):553–9.
Peacock AS, Bogossian F, McIntyre HD, Wilkinson S. A review of interventions to prevent type 2 diabetes after gestational diabetes. Women Birth. 2014;27(4):e7–15.
Pedersen ALW, Terkildsen Maindal H, Juul L. How to prevent type 2 diabetes in women with previous gestational diabetes? A systematic review of behavioural interventions. Prim Care Diabetes. 2017;11(5):403–13.
Pons MB, Badia OA. A systematic review with meta analysis of women with gestational diabetes indicate that they are at risk to suffer diabetes seven times more than normoglycemic women: commentary. FMC Form Med Contin Atencion Prim. 2010;17(3):200.
Reddy M, Palmer K, Rolnik D, Mol B, Wallace E, Costa F. Preeclampsia and long-term cardiovascular function - a systematic review and meta-analysis. J Paediatr Child Health. 2019;55(Supplement 1):96.
Sangtani A, Alrahmani L, Parikh P. Effect of hypertensive disorders of pregnancy on clinical outcomes in peripartum cardiomyopathy. Obstet Gynecol. 2019;133(SUPPL 1):105S.
Steinthorsdottir V, McGinnis R, Williams NO, Stefansdottir L, Thorleifsson G, Shooter S, et al. Genetic predisposition to hypertension is associated with preeclampsia in European and Central Asian women. Nat Commun. 2020;11(1):5976.
Tranidou A, Dagklis T, Tsakiridis I, Siargkas A, Apostolopoulou A, Mamopoulos A, et al. Prevalence of metabolic syndrome after pregnancies complicated by gestational diabetes mellitus - a systematic review and meta-analysis. Clin Nutr ESPEN. 2020;40:539–40.
Tranidou A, Dagklis T, Tsakiridis I, Siargkas A, Apostolopoulou A, Mamopoulos A, et al. Risk of developing metabolic syndrome after gestational diabetes mellitus - a systematic review and meta-analysis. J Endocrinol Invest. 2021;44(6):1139–49.
Varner MW, Rice MM, Landon MB, Casey BM, Reddy UM, Wapner RJ, et al. Pregnancies after the diagnosis of mild gestational diabetes mellitus and risk of cardiometabolic disorders. Obstet Gynecol. 2017;129(2):273–80.
Visser S, Hermes W, Ket JCF, Otten RHJ, van Pampus MG, Bloemenkamp KWM, et al. Systematic review and metaanalysis on nonclassic cardiovascular biomarkers after hypertensive pregnancy disorders. Am J Obstet Gynecol. 2014;211(4):373.e1-9.
Wang Z, Kanguru L, Hussein J, Fitzmaurice A, Ritchie K. Incidence of adverse outcomes associated with gestational diabetes mellitus in low- and middle-income countries. Int J Gynecol Obstet. 2013;121(1):14–9.
Lo CCW, Lo ACQ, Leow SH, Fisher G, Corker B, Batho O, et al. Future cardiovascular disease risk for women with gestational hypertension: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9(13):e013991.
Xu Y, Shen S, Sun L, Yang H, Jin B, Cao X. Metabolic syndrome risk after gestational diabetes: a systematic review and meta-analysis. PLoS One. 2014;9(1):e87863.
Zhao G, Bhatia D, Jung F, Lipscombe L. 47 - risk of type 2 diabetes mellitus after hypertensive disorders of pregnancy: a systematic review and meta-analysis. Can J Diabetes. 2020;44(7 Supplement):S21.
Baptiste-Roberts K, Barone BB, Gary TL, Golden SH, Wilson LM, Bass EB, et al. Risk factors for type 2 diabetes among women with gestational diabetes: a systematic review. Am J Med. 2009;122(3):207-14.e4.
Ben-Haroush A, Yogev Y, Hod M. Epidemiology of gestational diabetes mellitus and its association with type 2 diabetes. Diabet Med. 2004;21(2):103–13.
Burger RJ, Delagrange H, van Valkengoed IGM, de Groot CJM, van den Born BJH, Gordijn SJ, et al. Hypertensive disorders of pregnancy and cardiovascular disease risk across races and ethnicities: a review. Front Cardiovasc Med. 2022;9:933822.
Cao S, Li N, Zhang C, Liu J, Wang H, Leng J, et al. Adverse pregnancy outcomes are associated with an increased risk of postpartum prediabetes and diabetes in Chinese women with gestational diabetes. Diabetes Res Clin Pract. 2022;186:109817.
Craici IM, Wagner SJ, Hayman SR, Garovic VD. Pre-eclamptic pregnancies: an opportunity to identify women at risk for future cardiovascular disease. Womens Health (Lond). 2008;4(2):133–5.
Farahvar S, Walfisch A, Sheiner E. Gestational diabetes risk factors and long-term consequences for both mother and offspring: a literature review. Expert Rev Endocrinol Metab. 2019;14(1):63–74.
Groenhof TKJ, van Rijn BB, Franx A, Roeters van Lennep JE, Bots ML, Lely AT. Preventing cardiovascular disease after hypertensive disorders of pregnancy: Searching for the how and when. Eur J Prev Cardiol. 2017;24(16):1735–45.
Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25(10):1862–8.
Krome S. Gestational diabetes: individual risk assessment for type 2 diabetes. Diabetol Stoffwechsel. 2016;11(4):248–50.
Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Diabetologia. 2016;59(7):1403–11.
Ganesh A, Sarna N, Mehta R, Smith E. Hypertensive disorders in pregnancy and future risk of stroke: a systematic review (P2. 114). Minneapolis: AAN Enterprises; 2014.
Veiga ECDA, Rocha PRH, Caviola LL, Cardoso VC, Costa FDS, Saraiva MDCP, et al. Previous preeclampsia and its association with the future development of cardiovascular diseases: a systematic review and meta-analysis. Clinics. 2021;76:e1999.
Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017;10(2):e003497.
Brouwers L, van der Meiden-van Roest AJ, Savelkoul C, Vogelvang TE, Lely AT, Franx A, et al. Recurrence of pre-eclampsia and the risk of future hypertension and cardiovascular disease: a systematic review and meta-analysis. BJOG. 2018;125(13):1642–54.
Dennison RA, Chen ES, Green ME, Legard C, Kotecha D, Farmer G, et al. The absolute and relative risk of type 2 diabetes after gestational diabetes: a systematic review and meta-analysis of 129 studies. Diabetes Res Clin Pract. 2021;171:108625.
Li Z, Cheng Y, Wang D, Chen H, Chen H, Ming W-K, et al. Incidence rate of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review and meta-analysis of 170,139 women. J Diabetes Res. 2020;2020:3076463.
Song C, Lyu Y, Li C, Liu P, Li J, Ma RC, et al. Long-term risk of diabetes in women at varying durations after gestational diabetes: a systematic review and meta-analysis with more than 2 million women. Obes Rev. 2018;19(3):421–9.
Wang Z, Wang Z, Wang L, Qiu M, Wang Y, Hou X, et al. Hypertensive disorders during pregnancy and risk of type 2 diabetes in later life: a systematic review and meta-analysis. Endocrine. 2017;55(3):809–21.
Wu P, Kwok CS, Haththotuwa R, Kotronias RA, Babu A, Fryer AA, et al. Pre-eclampsia is associated with a twofold increase in diabetes: a systematic review and meta-analysis. Diabetologia. 2016;59(12):2518–26.
You H, Hu J, Liu Y, Luo B, Lei A. Risk of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review & meta-analysis. Indian J Med Res. 2021;154(1):62–77.
Hopmans TEJP, Van Houten CB, Kasius A, Kouznetsova OI, Nguyen AL, Rooijmans SV, et al. Increased risk of type 2 diabetes mellitus and cardiovascular disease after diabetes gravidarum. Ned Tijdschr Geneeskd. 2015;159(24):A8043.
Cavalli R, Veiga E, Rocha P, Cardoso V, Bettiol H. P-099. Previous preeclampsia and its association with future cardiovascular diseases: a systematic review and meta-analysis. Pregnancy Hypertens. 2021;25(1):e61.
Wu R, Wang T, Gu R, Xing D, Ye C, Chen Y, et al. Hypertensive disorders of pregnancy and risk of cardiovascular disease-related morbidity and mortality: a systematic review and meta-analysis. Cardiology. 2020;145(10):633–47.
Gadve SS, Chavanda S, Mukherjee AD, Aziz S, Joshi A, Patwardhan M. Risk of developing type 2 diabetes mellitus in south asian women with history of gestational diabetes mellitus: a systematic review and meta-analysis. Indian J Endocrinol Metab. 2021;25(3):176–81.
Xu J, Li T, Wang Y, Xue L, Miao Z, Long W, et al. The association between hypertensive disorders in pregnancy and the risk of developing chronic hypertension. Front Cardiovasc Med. 2022;9:897771.
Sukmanee J, Liabsuetrakul T. Risk of future cardiovascular diseases in different years postpartum after hypertensive disorders of pregnancy: a systematic review and meta-analysis. Medicine. 2022;101(30):e29646.
Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361.
Zhao G, Bhatia D, Jung F, Lipscombe L. Risk of type 2 diabetes mellitus in women with prior hypertensive disorders of pregnancy: a systematic review and meta-analysis. Diabetologia. 2021;64(3):491–503.
Brown MC, Best KE, Pearce MS, Waugh J, Robson SC, Bell R. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28(1):1–19.
Dall’Asta A, D’Antonio F, Saccone G, Buca D, Mastantuoni E, Liberati M, et al. Cardiovascular events following pregnancy complicated by pre-eclampsia with emphasis on comparison between early- and late-onset forms: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2021;57(5):698–709.
Groenhof TKJ, Zoet GA, Franx A, Gansevoort RT, Bots ML, Groen H, et al. Trajectory of cardiovascular risk factors after hypertensive disorders of pregnancy: an argument for follow-up. Hypertension. 2019;73(1):171–8.
Berks D, Steegers EA, Molas M, Visser W. Resolution of hypertension and proteinuria after preeclampsia. Obstet Gynecol. 2009;114(6):1307–14.
Sibai BM. Etiology and management of postpartum hypertension-preeclampsia. Am J Obstet Gynecol. 2012;206(6):470–5.
Cornell JE, Mulrow CD, Localio R, Stack CB, Meibohm AR, Guallar E, et al. Random-effects meta-analysis of inconsistent effects: a time for change. Ann Intern Med. 2014;160(4):267–70.
Bender R, Friede T, Koch A, Kuss O, Schlattmann P, Schwarzer G, et al. Methods for evidence synthesis in the case of very few studies. Res Synth Methods. 2018;9(3):382–92.
Riley RD, Debray TP, Fisher D, Hattle M, Marlin N, Hoogland J, et al. Individual participant data meta-analysis to examine interactions between treatment effect and participant-level covariates: statistical recommendations for conduct and planning. Stat Med. 2020;39(15):2115–37.
Zhang C, Bao W, Rong Y, Yang H, Bowers K, Yeung E, et al. Genetic variants and the risk of gestational diabetes mellitus: a systematic review. Hum Reprod Update. 2013;19(4):376–90.
Semenkovich CF. Insulin resistance and atherosclerosis. J Clin Investig. 2006;116(7):1813–22.
Ruksasakul R, Tharavanij T, Sritipsukho P. Metabolic syndrome in thai women previously diagnosed with gestational diabetes. J Med Assoc Thailand. 2016;99:S195-202.
Alageel S, Wright AJ, Gulliford MC. Changes in cardiovascular disease risk and behavioural risk factors before the introduction of a health check programme in England. Prev Med. 2016;91:158–63.
The National Institute for Health and Care Excellence (NICE). Hypertension in pregnancy: diagnosis and management; 2019. (NICE guideline [NG133]).
The National Institute for Health and Care Excellence (NICE). Type 2 diabetes: prevention in people at high risk; 2017.
Hippisley-Cox J, Coupland C. Development and validation of QDiabetes-2018 risk prediction algorithm to estimate future risk of type 2 diabetes: cohort study. BMJ. 2017;359:j5019.
Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, et al. A risk score for predicting near-term incidence of hypertension: the Framingham Heart Study. Ann Intern Med. 2008;148(2):102–10.
Acknowledgements
We would like to thank the MuM-PreDiCT consortium team members for their involvement in this study.
Funding
This work is funded by the Strategic Priority Fund “Tackling multimorbidity at scale” programme (grant number MR/W014432/1) delivered by the Medical Research Council and the National Institute for Health Research in partnership with the Economic and Social Research Council and in collaboration with the Engineering and Physical Sciences Research Council. SW PhD studentship is funded by the British Heart Foundation (BHF) Data Science Centre (BHF grant number SP/19/3/34678, awarded to Health Data Research (HDR)). His PhD is also supported through the HDR-UK-Turing Wellcome PhD Programme. RR, KS, KN and FC are supported by funding from the NIHR Birmingham Biomedical Research Centre at the University Hospitals Birmingham NHS Foundation Trust and the University of Birmingham. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
SW was responsible for the study conceptualization and design and drafted the initial manuscript. MS, KO, KS, RR, CY, ST, KN and FC were responsible for the study conceptualization and design and revised the manuscript critically for important intellectual content. KS, RR, CY, ST, KN and FC were responsible for supervision of the study. All authors read and approved the final manuscript.
Authors’ Twitter handles
Twitter handles: Mr. Steven Wambua, @StevenWambua; Dr. Megha Singh, @meghasingh_16; Dr. Kelvin Okoth, @KelvinOkoth_; Dr. Kym I E Snell, @Kym_Snell; Prof. Richard Riley, @Richard_D_Riley; Prof. Christopher Yau, @cwcyau; Prof. Shakila Thangaratinam, @thangaratinam; Prof. Krishnarajah Nirantharakumar, @Nirantharakumar; Dr. Francesca L Crowe, @francescacrowe
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Tables S1-11 and Figures S1-S2. Table S1 -
Search Strategy for systematic review, Table S2 - Data extraction form, Table S3 - List of excluded reviews, Table S4 - AMSTAR 2 quality appraisal scores, Table S5 - Citation matrices for reviews with overlapping associations, Table S6 - General characteristics of reviews with overlapping associations, Table S7 - List of reviews with overlapping associations excluded from analysis, Table S8 - Exposure definitions and extend of risk factors adjustment in systematic reviews included in the umbrella review, Table S9 - Tabular presentation of findings: Narrative syntheses, Table S10 - Tabular presentation of original estimates: Meta-analysis, Table S11 - PRIOR Checklist, FigS1 - Word cloud of confounders adjustment reported by reviews, FigS2 - meta-analysis of primary studies that excluded chronic hypertension.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wambua, S., Singh, M., Okoth, K. et al. Association between pregnancy-related complications and development of type 2 diabetes and hypertension in women: an umbrella review. BMC Med 22, 66 (2024). https://doi.org/10.1186/s12916-024-03284-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-024-03284-4