Abstract
Background
Long-term health outcomes in children and young people (CYP) after COVID-19 infection are not well understood and studies with control groups exposed to other infections are lacking. This study aimed to investigate the incidence of post-COVID-19 condition (PCC) and incomplete recovery in CYP after hospital discharge and compare outcomes between different SARS-CoV-2 variants and non-SARS-CoV-2 infections.
Methods
A prospective exposure-stratified cohort study of individuals under 18 years old in Moscow, Russia. Exposed cohorts were paediatric patients admitted with laboratory-confirmed COVID-19 infection between April 2 and December 11, 2020 (Wuhan variant cohort) and between January 12 and February 19, 2022 (Omicron variant cohort). CYP admitted with respiratory and intestinal infections, but negative lateral flow rapid diagnostic test and PCR-test results for SARS-CoV-2, between January 12 and February 19, 2022, served as unexposed reference cohort. Comparison between the ‘exposed cohorts’ and ‘reference cohort’ was conducted using 1:1 matching by age and sex. Follow-up data were collected via telephone interviews with parents, utilising the long COVID paediatric protocol and survey developed by the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC). The WHO case definition was used to categorise PCC.
Results
Of 2595 CYP with confirmed COVID-19, 1707 (65.7%) participated in follow-up interviews, with 1183/1707 (69%) included in the final ‘matched’ analysis. The median follow-up time post-discharge was 6.7 months. The incidence of PCC was significantly higher in the Wuhan variant cohort (89.7 cases per 1000 person-months, 95% CI 64.3–120.3) compared to post-infection sequalae in the reference cohort (12.2 cases per 1000 person-months, 95% CI 4.9–21.9), whereas the difference with the Omicron variant cohort and reference cohort was not significant. The Wuhan cohort had higher incidence rates of dermatological, fatigue, gastrointestinal, sensory, and sleep manifestations, as well as behavioural and emotional problems than the reference cohort. The only significant difference between Omicron variant cohort and reference cohort was decreased school attendance. When comparing the Wuhan and Omicron variant cohorts, higher incidence of PCC and event rates of fatigue, decreased physical activity, and deterioration of relationships was observed. The rate of incomplete recovery was also significantly higher in the Wuhan variant cohort than in both the reference and the Omicron variant cohorts.
Conclusions
Wuhan variant exhibited a propensity for inducing a broad spectrum of physical symptoms and emotional behavioural changes, suggesting a pronounced impact on long-term health outcomes. Conversely, the Omicron variant resulted in fewer post-infection effects no different from common seasonal viral illnesses. This may mean that the Omicron variant and subsequent variants might not lead to the same level of long-term health consequences as earlier variants.
Similar content being viewed by others
Background
Multiple studies have attempted to determine the incidence and risk factors associated with SARS-CoV-2 sequelae in children and young people (CYP) [1]. However, these studies were often impeded by methodological heterogeneity, biases, and inconsistent definitions of COVID-19 consequences [2, 3]. The difficulty of appropriate reference or control group selection has subjected available studies to criticism [4].
One possible approach to obtaining a reference group is to recruit uninfected CYP whose negative status has been previously verified by PCR testing. In the CLoCk study, PCR-positive CYP were matched to test-negative CYP using the national SARS-CoV-2 testing dataset [5]. Similarly, a nationwide cohort study of CYP in Denmark included an exposed group with SARS-CoV-2 infection, verified by RT-PCR, and a reference group of randomly selected individuals who have never been test-positive for SARS-CoV-2 [6]. In a mobile app-based study, Molteni and co-authors recruited a reference group of CYP whose self-reported test results were negative [7]. In other studies, the exposed cohorts were formed from randomly selected schools based on RT-PCR test results, and reference cohorts were recruited from CYP who visited their doctor routinely, with both negative RT-PCR and antibody-based SARS-CoV-2 analysis [8, 9].
Previous efforts suffer from blending symptomatic and asymptomatic CYP in the infected groups, which does not address the possible confounding effect of severity or confounding by factors predisposing to more severe symptoms. Additionally, misdiagnosis may have occurred, as acknowledged by some authors [5]. One approach is to limit the scope of the infected group to those CYP who are symptomatic. However, the results of such studies are challenging to interpret, as previously ill CYP are compared to a generally healthy reference, and the incremental effect cannot be evaluated in the context of other previously known illnesses [10]. Previous expert statements [11, 12] as well as recent systematic review suggested that future studies would benefit from control group and adjustment of the study results for health and environmental factors, including SARS-CoV-2 variant [1].
A potential solution to this problem could be using a reference with comparably severe disease, yet without SARS-CoV-2 infection. To the best of our knowledge, a single study followed this consideration, recruiting reference cohort from both hospitalised and non-hospitalised CYP with other non-SARS-CoV-2 community-acquired infections, clinically and laboratory-confirmed, whereas cases were defined as CYP with previous acute phase of COVID-19 [13]. Given the relatively rare occurrence of highly severe SARS-CoV-2 infection [14], filling the gaps in understanding long consequences of SARS-CoV-2 on health and well-being of CYP in comparison to other known infection is needed. Additionally, there is a paucity of paediatric studies evaluating the long-term consequences of COVID-19 related to the most prevalent circulating variants of SARS-CoV-2 in the population during a specific time period [15].
Another limitation pertains to the broad outcome definition employed by most of the observational studies examining the consequences of COVID-19. Although the World Health Organization (WHO) has provided a definition for the post-COVID-19 Condition [16], a disappointingly small number of studies have chosen to incorporate this definition into their research methodology.
This prospective exposure-stratified cohort study aimed to investigate the incidence of post-COVID-19 condition among hospitalised CYP with COVID-19 infection compared with post-infection sequalae in a reference cohort of previously hospitalised CYP with non-COVID-19 infectious diseases. The study used standardised follow-up data collection protocols developed by the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) Global Paediatric COVID-19 follow-up working group. The study included assessment of post-COVID-19 condition corresponding to different waves of the pandemic in Moscow, Russia, as a proxy for infection with different SARS-CoV-2 variants.
Methods
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist for cohort studies (https://www.strobe-statement.org/) was utilised to report the present study.
Study design, setting, and participants
The present study is an exposure-stratified prospective cohort study of CYP under the age of 18 carried out in Bashlyaeva Children’s City Clinical Hospital and G.N. Speransky Children’s City Clinical Hospital No. 9. These hospitals were the primary hospitals treating COVID-19 in CYP residing in Moscow at different times of pandemic. Additional file 1: Table S1 provides a detailed description of the criteria for hospital admission according to the local clinical guidelines.
Exposed cohorts for this study included paediatric patients hospitalised to Bashlyaeva Children’s City Clinical Hospital with a laboratory-confirmed diagnosis of COVID-19 infection, spanning from April 2, 2020, to December 11, 2020 (Wuhan variant cohort), and to G.N. Speransky Children’s City Clinical Hospital No. 9 between January 12, 2022, and February 19, 2022 (Omicron variant cohort). The dates of patient hospital admission were matched with the data on variant predominance in Moscow [17] (Additional file 1: Figure S1).
CYP who were hospitalised to G.N. Speransky Children’s City Clinical Hospital No. 9 with confirmed respiratory and gastrointestinal infections in conjunction with negative lateral flow rapid diagnostic test and PCR-test results for SARS-CoV-2, between January 12, 2022, and February 19, 2022, served as the unexposed reference cohort for this study. They represent typical patients who are routinely admitted to the hospital with respiratory and gastrointestinal infections during seasonal outbreaks. Recruiting a reference cohort during the Wuhan wave proved to be a formidable challenge. The dearth of admissions of CYP with respiratory infections other than COVID-19, coupled with the high rate of false negatives in COVID-19 testing during the initial months of the pandemic and the scarcity of resources further compounded the difficulty.
Data management
Baseline data at admission consisted of information pertaining to patient demographics, symptoms, and comorbidities, documented at the time of admission. In addition, the dataset also encompassed results of clinical investigations, supportive care requirements during hospitalisation, and crucial clinical outcomes upon discharge.
Follow-up data have been collected via telephone interviews with parents conducted by research team members who had received standardised training in interview administration, REDCap data entry, and data security [18,19,20]. The interviews took place between January 31 and February 27, June 2 and August 1, 2021, and August 1 and September 15, 2022. The long COVID paediatric protocol and survey, which was developed by the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) and translated into Russian, was utilised to collect data from both exposed and the reference cohorts. The data included questions regarding symptoms and their onset and persistence at the time of the follow-up as well as the physical, psychosocial, and behavioural well-being of CYP (all proxy-reported by parents).
Data collection, storage, and management were performed using REDCap electronic data capture tools (Vanderbilt University, Nashville, TN, USA) hosted at Sechenov University and Microsoft Excel (Microsoft Corp, Redmond, WA, USA).
Definitions
The present study adopts the WHO case definition to categorise post-COVID-19 condition as the presence of any symptom that emerges no later than 3 months post-hospital discharge and persists for at least 2 months. In the absence of reliable objective medical record data pertaining to the date of first symptom appearance, symptom duration was calculated from the time of hospital discharge.
Post-COVID-19 condition/post-infection sequalae symptoms were categorised into nine manifestations, which encompassed cardiovascular, dermatological, fatigue, gastrointestinal, musculoskeletal, neurocognitive, respiratory, sensory, and sleep-related symptoms. This classification was formulated by drawing upon relevant prior literature and through ISARIC’s working group deliberations [20].
Emotional and behavioural changes, which were initially recorded using a five-point scale ranging from ‘much less’ to ‘much more’, have been converted into binary variables. We considered worsening of symptoms for excessive fatigue when parents were reporting ‘more’ and ‘much more’ with regard to this outcome during telephone interview.
Recovery was assessed using a Likert scale ranging from ‘1’ (no recovery) to ‘10’ (complete recovery). Responses were transformed into a binary variable, with a ‘1–6’ considered ‘incomplete recovery’ and ‘7–10’ complete recovery from the infection.
Patients in all the cohorts were defined as severe if required non-invasive ventilation, invasive ventilation, or intensive care unit (ICU) care during acute phase of COVID-19.
Statistical analysis
Baseline characteristics were analysed through descriptive statistics. We summarised continuous variables as medians (interquartile range, IQR), while categorical variables were presented as frequencies (percentages).
We utilised forest plots to depict the incidence and event rates associated with post-COVID-19 conditions and their varying manifestations. The incidence was calculated as the ratio of the total number of new cases to the total time at risk. In line with the World Health Organization’s definition of post-COVID-19 condition (PCC), an individual’s time at risk is capped at three months from the onset of symptoms (or from hospital admission if symptom onset is unknown). For manifestations of symptoms, we selected the shortest time at risk across all symptoms for each individual within a group. We calculated the rate of events as the ratio of the number of cases to the number of people at risk.
We conducted a comparison between the ‘exposed cohorts’ (Wuhan variant cohort and Omicron variant cohort) and ‘reference cohort’ using 1:1 matching by age (± 1 year) and sex. In a sensitivity analysis, two additional matching parameters severity and length of hospitalisation (± 2 days) were included (Additional file 1: Table S2, Figures S2 and S3). We regarded age and sex as confounders, while severity (defined as the need for non-invasive or invasive ventilation, or intensive care unit admission) and length of hospitalisation may function as proxies for true severity.
We employed bootstrap methodology (30,000 iterations) to obtain 95% confidence intervals (CIs) for the estimates of post-COVID-19 condition event rates and incidence. This involved resampling from a variety of potentially matched cohorts. We have presented the demographic characteristics and comorbidities of the matched cohorts, alongside the features of the initial sample.
We considered differences in event rates and incidence of manifestations between groups as significant if the median p-value for rate ratios, acquired from the bootstrap procedure via the exact Fisher’s test, was less than 5%.
Statistical analysis was conducted using R version 4.0.2, employing the dplyr, foreign, ggraph, and ggforce libraries.
To minimise recall bias, we limited the period from the onset date of the first symptoms (or the date of hospital admission if symptom onset was missing or inconsistent) to the follow-up date to a maximum of 8 months.
Results
Study participant characteristics
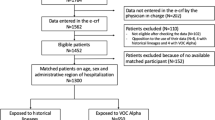
Out of the 2595 eligible CYP with laboratory-confirmed COVID-19 who were discharged between March 18, 2020, and February 20, 2022, 2520 (97.1%) had contact information available. Of these, 1707 CYP (65.7% of those discharged, 67.7% of those with contact information) participated in follow-up interviews. Upon matching, 1183 out of 1707 CYP (69%) were included in the final analysis (Fig. 1).
Table 1 presents the demographic and clinical characteristics of the study participants. The median time elapsed after hospital discharge was 6.7 months, ranging from 6.2 months for Omicron variant and control cohorts to 7.5 months in the Wuhan variant cohort. Before the matching process, the median age was 10.3 years (IQR 2.8–14.7) in the Wuhan variant cohort, 2.6 years (IQR 0.8–7.0) in the Omicron stain cohort, and 4.2 years (IQR 1.9–7.8) in the reference cohort. The share of severe patients ranged from 2.4% in the Wuhan variant cohorts to 6.2% in the Omicron cohort and 3.2% in the reference cohort.
The most common comorbidities in the pooled initial cohorts were food allergy (12.0%), intestinal (9.3%) and neurological (8.7%) problems, and atopic dermatitis/eczema (7.9%). However, in the matched sets, the prevalence of these comorbidities varied significantly. Higher prevalence of neurological problems (5.8%), food allergy (4.7%), and lower prevalence of malnutrition (4.6%) were observed in Wuhan variant cohort when compared with the reference cohort. Higher prevalence of atopic dermatitis/eczema (9.7%) and neurological problems (+ 5.4%) was found in Omicron variant cohort when compared with the reference cohort.
Post-COVID-19 condition/post-infection sequalae incidence
Figure 2 presents the incidence rates of PCC/post-infection sequalae and manifestations of symptoms in matched cohorts, while Fig. 3 depicts the well-being assessment results and incomplete recovery in matched cohorts. Detailed information is available in Table S3.
For the Wuhan variant cohort, the incidence of PCC was 89.6 cases per 1000 person-months (95% CI 64.4–120.4), compared to 11.0 cases of post-infection sequalae per 1000 person-months (95% CI 4.8–19.7) in the reference cohort (p < 0.001). Conversely, the difference between the matched Omicron variant cohort (14.1 cases per 1000 person-months, 95% CI 6.8–23.7) and the reference cohort (10.1 cases per 1000 person-months, 95% CI 3.4–18.2) was not statistically significant (p = 0.45).
When comparing the Wuhan variant cohort (87.0 cases per 1000 person-months, 95% CI 61.0–118.9) to the Omicron variant cohort (15.7 cases per 1000 person-months, 95% CI 6.5–26.7), a significant difference in the PCC event rate was noted (p < 0.001).
Post-COVID-19 condition/post-infection sequalae manifestations
The Wuhan variant cohort displayed a significantly higher incidence of dermatological, fatigue, gastrointestinal, sensory, and sleep manifestations of PCC than similar post-infection sequalae manifestations in the reference cohort. The largest difference in manifestation rates was observed for fatigue (31.4 cases per 1000 person-months, 95% CI 18.7–48.0 vs. 2.4 cases per 1000 person-months, 95% CI 0.0–6.0) and sleep problems (24.5 cases per 1000 person-months, 95% CI 13.6–38.8 vs. 3.6 cases per 1000 person-months, 95% CI 0.0–8.4).
For the Omicron variant cohort, no statistically significant differences in any symptom manifestations were found when compared with the reference cohort.
Comparing the Wuhan and Omicron variant cohorts, significant differences in incidence were observed for dermatological, fatigue, gastrointestinal, sensory and sleep manifestations. The largest differences were observed in incidence of dermatological manifestations in Wuhan vs Omicron variant cohorts (21.9 cases per 1000 person-months, 95% CI 10.7–35.8 vs. 0.0 cases per 1,000 person-months, 95% CI 0.0–3.8) and fatigue (28.9 cases per 1,000 person-months, 95% CI 16.1–45.3 vs. 2.5 cases per 1,000 person-months, 95% CI 0.0–6.5).
The rate of events for incomplete recovery was significantly higher in the Wuhan variant cohort (13.9%, 95% CI 9.6–18.7%) than in the reference cohort (3.6%, 95% CI 1.4–6.3%). For the Omicron variant cohort, this rate was not significantly different from the reference cohort, but it was significantly lower than the Wuhan variant cohort (7.0% (95% CI 3.8–10.7%) vs. 13.3% (95% CI 8.8–18.2%)) (Additional file 1: Table S3).
Post-COVID-19 condition/post-infection sequalae emotional and behavioural status
Emotional and behavioural changes also differed significantly between the Wuhan variant and reference cohorts, with higher rates observed in the Wuhan variant cohort for behavioural changes (10.4%, 95% CI 6.7–14.9 vs. 4.2%, 95% CI 1.6–7.1%), emotional problems (12.9%, 95% CI 8.7–17.5% vs. 5.8%, 95% CI 3.1–9.2%), fatigue (16.0%, 95% CI 11.4–21.1% vs. 7.1%, 95% CI 4.1–10.6%), communicating with friends personally (5.4%, 95% CI 2.2–9.4% vs 1.4%, 95% CI 0.0–3.3%), worsening relationships (5.7%, 95% CI 2.7–9.2% vs. 0.8%, 95% CI 0.0–2.5%), decline in school attendance (11.5%, 95% CI 6.9–16.8% vs. 4.5%, 95% CI 1.6–8.1%), and sleep problems (12.2%, 95% CI 8.1–16.8% vs. 5.4%, 95% CI 2.9–8.5%).
In contrast, the Omicron variant cohort only showed a significant difference from the reference cohort with regard to lower school attendance (9%, 95% CI 5.1–13.6% vs. 3.8%, 95% CI 1.4–7.2%).
When the Wuhan and Omicron variant cohorts were compared, significant differences in rates of events for emotional behavioural changes were observed for fatigue (14.9%, 95% CI 10.4–19.8% vs. 7.4%, 95% CI 4.1–11.2%), decreased physical activity (9.3%, 95% CI 5.5–13.8% vs. 2.7%, 95% CI 0.8–5.2%), and deterioration of relationships (4.9%, 95% CI 2.4–8.4% vs. 0.9%, 95% CI 0.0–2.4%).
Incidence (per 1000 person-months (95% confidence interval)) of post COVID-19 condition and different manifestations in exposure and reference groups were matched by age and sex. Statistically insignificant results are presented in white; statistically significant difference of p < 0.05 between the groups is highlighted in light green; statistically significant difference of p < 0.01 between the groups is highlighted in light yellow; statistically significant difference of p < 0.001 between the groups is highlighted in light grey.
Prevalence of incomplete recovery is presented as event rate (95% confidence interval). Statistically insignificant results are presented in white; statistically significant difference of p < 0.05 between the groups is highlighted in light green; statistically significant difference of p < 0.01 between the groups is highlighted in light yellow; statistically significant difference of p < 0.001 between the groups is highlighted in light grey.
Discussion
The importance of investigating the impact of COVID-19 on CYP has been previously emphasised, particularly in light of new variants of the virus circulating in the population [12]. However, current research on the long-term effects of COVID-19 in CYP is limited and is associated with methodological limitations, making it difficult to distinguish between the effects of the virus and the impact of social restrictions [21]. There is also a lack of studies that compare the effects of COVID-19 in CYP with a control group of individuals following other viral infections. Experts previously highlighted the importance of a control group in studies following SARS-CoV-2 infection in CYP, using standardised case definitions [4]. This study aimed to address these gaps by estimating the incidence of PCC and the impact on well-being among CYP and young people, comparing COVID-19 from different variants with a control cohort of CYP hospitalised with non-COVID-19 infections. We found that CYP hospitalised during Wuhan variant wave had a significantly higher incidence of PCC and incomplete recovery than incidence of post-infection sequalae in the controls. Emotional and behavioural changes were also observed in Wuhan cases, including behaviour changes, emotional problems, excessive fatigue, worsening of relationships, decline in school attendance, and problems with sleep. In contrast, CYP admitted to the hospital with COVID-19 during the Omicron variant wave did not differ significantly from CYP hospitalised with respiratory or gastrointestinal infections in terms of long-lasting outcomes, symptom manifestation, and recovery. However, they were shown to have distinctively more problems with school attendance.
The incidence of PCC was significantly higher in the cohort infected by the Wuhan variant compared to the post-infection sequalae incidence in reference cohort, with a disparity of 77.5 cases per 1000 person-months. Conversely, the incidence rate in the Omicron variant cohort did not show a statistically significant difference from the reference cohort. The striking difference between the Wuhan and Omicron cohorts indicates the potential difference in virulence and resultant clinical outcomes associated with the distinct viral variants. Results are somehow reassuring as Wuhan variant is very uncommon in population now, and findings allow to hypothesise that Omicron variant as well as SARS-CoV-2 circulating in the population, originating from Omicron [22], is unlikely to differ in terms of consequences compared with common seasonal viruses significantly. Such discrepancy in long-term outcomes between different variants might be attributable to the variations in the viral structure, particularly in the spike protein [23], which is known to affect the virus’s ability to bind to and enter host cells. Future studies focusing on the specific biological mechanisms behind these differences could provide more definitive answers.
When assessing symptom manifestations of PCC, the Wuhan cohort presented a markedly higher incidence of dermatological, fatigue, gastrointestinal, sensory, and sleep disturbances than the post-infection sequalae manifestations in reference cohort. Among these, fatigue and sleep problems demonstrated the largest difference in manifestation rates. Such findings corroborate the existing literature, where fatigue and sleep issues have been consistently reported as prominent manifestations of PCC, particularly in the context of the Wuhan variant. In contrast, the Omicron cohort showed no significant difference in symptom manifestations compared to the reference cohort, further highlighting the potential differential pathogenicity of the viral variants. The largest differences between the Wuhan and Omicron cohorts were found for dermatological manifestations and fatigue, again underscoring the burden of these symptoms in CYP infected with the Wuhan variant. In contrast, the Omicron cohort showed no significant difference in symptom manifestations compared to the reference cohort, further highlighting the potential differential pathogenicity of the viral variants. The largest differences between the Wuhan and Omicron cohorts were found for dermatological manifestations and fatigue, again underscoring the burden of these symptoms in CYP infected with the Wuhan variant.
Our findings also revealed that CYP infected with the Wuhan variant had significantly higher rates of incomplete recovery and emotional-behavioural changes, such as behavioural changes, emotional problems, fatigue, worsening relationships, decline in school attendance, and sleep problems, as compared to the reference cohort. These results suggest the long-lasting and pervasive impact of COVID-19 on health and well-being of CYP, especially those infected by the Wuhan variant. It is crucial for healthcare providers to recognise these long-term sequelae and to develop appropriate strategies for ongoing support and management.
The Omicron cohort showed a significant difference from the reference cohort only in terms of lower school attendance. This difference could be attributed to factors such as more conservative return-to-school policies during the Omicron wave. Additionally, parental concerns about their child’s health after infection could have contributed to lower school attendance. However, it does imply a potential impact on the children’s educational attainment and warrants further exploration.
One of the major strengths of this study is the inclusion of a control group of CYP who were admitted to the hospital with non-COVID-19 infections. This allows us to estimate the relative burden of long COVID-19 and to compare the outcomes of CYP with COVID-19 infection to those of CYP with other infections. Both cases and controls in this study were exposed to infection-related hospitalisations, which reduces the potential for bias due to differences in health-seeking behaviour. Another strength of the study is the distinction made between the early Wuhan variant and the later Omicron variant of the virus. By comparing the outcomes of CYP infected with these two variants, we are able to explore the differences in the long-term effects of the two variants of the virus on children’s health. The study utilised the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) long-term follow-up study case report forms (CRFs) for CYP. This standardised data collection method ensures that the data collected are consistent and comparable across different study sites. In addition, the study used the WHO post-COVID-19 condition definition, which provides a standardised definition of the condition that allows for more accurate and consistent identification of cases.
However, the study also has several limitations. First, all the cohorts represent hospitalised population which do not allow to extrapolate findings on all CYP. The follow-up period has been restricted to 8 months after hospital discharge. This may not be sufficient to capture the full extent of long-term effects of COVID-19 in CYP. Second, the study is limited in its ability to control for extrinsic factors and residual confounding, such as vaccinations and other viral infections, that may have affected the study outcomes. Third, the criteria for hospital admission may have changed over time, and cases across waves can have different acute severity. Fourth, the chronological association of the waves of study with COVID-19 variants was established without laboratory confirmation, and relied upon available open data sources, which may have introduced bias into the study. No patients were recruited during Delta variant wave. Fifth, the study relied on proxy-reported responses from the parents for the follow-up interviews, which may be affected by recall bias and non-blindness of respondents. Additionally, parental bias towards the health of their CYP may have influenced the accuracy of the data collected. Finally, there is a risk of potential selection bias, with those with symptoms more likely to agree to the survey and thus potentially overestimating the prevalence of post-COVID-19 condition. At the onset of the COVID-19 pandemic, when the Wuhan variant was prevalent in Russia, the only facility in Moscow equipped for the hospitalisation of infected children was the Bashlyaeva Children’s City Clinical Hospital. As the pandemic evolved and other variants, including Omicron, became dominant, the G.N. Speransky Children’s City Clinical Hospital No. 9 COVID-19 wards were set-up in response to increasingly large number of patients expected as a part of this wave. Consequently, it was not possible and feasible to gather data from just one hospital. However, given that both hospitals used identical data collection methodologies, the batch effect in the data is unlikely.
Conclusions
Overall, the findings of this study underscore the importance of continued monitoring and support for CYP who have been hospitalised with COVID-19 infection as well as for those who may be experiencing long-term effects of the virus. Future studies should aim to elucidate the underlying biological mechanisms behind the observed differences in clinical outcomes associated with different viral variants. The results offer some reassurance, given that the Wuhan variant is now quite rare in the population. These findings permit us to conjecture that the Omicron variant, as well as the SARS-CoV-2 variants currently circulating, is unlikely to diverge significantly from common seasonal viruses in terms of their consequences. Policymakers, healthcare providers, and families must work together to ensure that CYP are provided with the resources and support they need to recover fully and to continue to thrive despite the challenges posed by the COVID-19 pandemic.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, DM, upon reasonable request.
Abbreviations
- CI:
-
Confidence interval
- CLoCk:
-
Children and young people with long COVID study
- COVID-19:
-
Coronavirus disease 2019
- CRF:
-
Case report form
- CYP:
-
Children and young people
- HIV:
-
Human immunodeficiency virus
- ISARIC:
-
International Severe Acute Respiratory and Emerging Infection Consortium
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- PASC:
-
Post-acute sequelae of SARS-CoV-2 infection
- PCC:
-
Post-COVID-19 condition
- PCR:
-
Polymerase chain reaction
- REDCap:
-
Research Electronic Data Capture
- SARS CoV-2:
-
Severe acute respiratory syndrome-related coronavirus 2
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- WHO:
-
World Health Organization
References
Lopez-Leon S, Wegman-Ostrosky T, Ayuzo Del Valle NC, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A, Villapol S. Long-COVID in children and adolescents: a systematic review and meta-analyses. Sci Rep. 2022;12(1):9950.
Munblit D, O’Hara ME, Akrami A, Perego E, Olliaro P, Needham DM. Long COVID: aiming for a consensus. Lancet Respir Med. 2022;10:632–4.
Berg SK, Palm P. Playing catch with long COVID - understanding a new disease. Lancet Reg Health Eur. 2023;25:100568.
Stephenson T, Shafran R, Ladhani SN. Long COVID in children and adolescents. Curr Opin Infect Dis. 2022;35(5):461–7.
Pinto Pereira SM, Shafran R, Nugawela MD, Panagi L, Hargreaves D, Ladhani SN, Bennett SD, Chalder T, Dalrymple E, Ford T, et al. Natural course of health and well-being in non-hospitalised children and young people after testing for SARS-CoV-2: a prospective follow-up study over 12 months. Lancet Reg Health Eur. 2023;25:100554.
Borch L, Holm M, Knudsen M, Ellermann-Eriksen S, Hagstroem S. Long COVID symptoms and duration in SARS-CoV-2 positive children - a nationwide cohort study. Eur J Pediatr. 2022;181(4):1597–607.
Molteni E, Sudre CH, Canas LS, Bhopal SS, Hughes RC, Antonelli M, Murray B, Klaser K, Kerfoot E, Chen L, et al. Illness duration and symptom profile in symptomatic UK school-aged children tested for SARS-CoV-2. Lancet Child Adolesc Health. 2021;5(10):708–18.
Radtke T, Ulyte A, Puhan MA, Kriemler S. Long-term symptoms after SARS-CoV-2 infection in children and adolescents. JAMA. 2021;326(9):869–71.
Fink TT, Marques HHS, Gualano B, Lindoso L, Bain V, Astley C, Martins F, Matheus D, Matsuo OM, Suguita P, et al. Persistent symptoms and decreased health-related quality of life after symptomatic pediatric COVID-19: a prospective study in a Latin American tertiary hospital. Clinics (Sao Paulo). 2021;76:e3511.
Roessler M, Tesch F, Batram M, Jacob J, Loser F, Weidinger O, Wende D, Vivirito A, Toepfner N, Ehm F, et al. Post-COVID-19-associated morbidity in children, adolescents, and adults: a matched cohort study including more than 157,000 individuals with COVID-19 in Germany. PLoS Med. 2022;19(11):e1004122.
Munblit D, Nicholson TR, Needham DM, Seylanova N, Parr C, Chen J, Kokorina A, Sigfrid L, Buonsenso D, Bhatnagar S, et al. Studying the post-COVID-19 condition: research challenges, strategies, and importance of Core Outcome Set development. BMC Med. 2022;20(1):50.
Munblit D, Sigfrid L, Warner JO. Setting priorities to address research gaps in long-term COVID-19 outcomes in children. JAMA Pediatr. 2021;175:1095–6.
Roge I, Smane L, Kivite-Urtane A, Pucuka Z, Racko I, Klavina L, Pavare J. Comparison of persistent symptoms after COVID-19 and other non-SARS-CoV-2 infections in children. Front Pediatr. 2021;9:752385.
Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39(5):355–68.
Du M, Ma Y, Deng J, Liu M, Liu J. Comparison of long COVID-19 caused by different SARS-CoV-2 Strains: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022;19(23):16010.
Chaichana U, Man KKC, Chen A, Wong ICK, George J, Wilson P, Wei L. Definition of post-COVID-19 condition among published research studies. JAMA Netw Open. 2023;6(4):e235856.
Gushchin VA, Pochtovyi AA, Kustova DD, Ogarkova DA, Tarnovetskii IY, Belyaeva ED, Divisenko EV, Vasilchenko LA, Shidlovskaya EV, Kuznetsova NA, et al. Dynamics of SARS-CoV-2 major genetic lineages in moscow in the context of vaccine prophylaxis. Int J Mol Sci. 2022;23(23):14670.
Munblit D, Nekliudov NA, Bugaeva P, Blyuss O, Kislova M, Listovskaya E, Gamirova A, Shikhaleva A, Belyaev V, Timashev P, et al. Stop COVID cohort: an observational study of 3480 patients admitted to the Sechenov University Hospital Network in Moscow City for suspected coronavirus disease 2019 (COVID-19) infection. Clin Infect Dis. 2021;73(1):1–11.
Osmanov IM, Spiridonova E, Bobkova P, Gamirova A, Shikhaleva A, Andreeva M, Blyuss O, El-Taravi Y, DunnGalvin A, Comberiati P, Peroni DG, Apfelbacher C, Genuneit J, Mazankova L, Miroshina A, Chistyakova E, Samitova E, Borzakova S, Bondarenko E, Korsunskiy AA, Konova I, Hanson SW, Carson G, Sigfrid L, Scott JT, Greenhawt M, Whittaker EA, Garralda E, Swann OV, Buonsenso D, Nicholls DE, Simpson F, Jones C, Semple MG, Warner JO, Vos T, Olliaro P, Munblit D; and the Sechenov StopCOVID Research Team. Risk factors for post-COVID-19 condition in previously hospitalised children using the ISARIC Global follow-up protocol: a prospective cohort study. Eur Respir J. 2022;59(2):2101341. https://doi.org/10.1183/13993003.01341-2021.
Pazukhina E, Andreeva M, Spiridonova E, Bobkova P, Shikhaleva A, El-Taravi Y, Rumyantsev M, Gamirova A, Bairashevskaia A, Petrova P, et al. Prevalence and risk factors of post-COVID-19 condition in adults and children at 6 and 12 months after hospital discharge: a prospective, cohort study in Moscow (StopCOVID). BMC Med. 2022;20(1):244.
Pellegrino R, Chiappini E, Licari A, Galli L, Marseglia GL. Prevalence and clinical presentation of long COVID in children: a systematic review. Eur J Pediatr. 2022;181(12):3995–4009.
Statement on the update of WHO’s working definitions and tracking system for SARS-CoV-2 variants of concern and variants of interest https://www.who.int/news/item/16-03-2023-statement-on-the-update-of-who-s-working-definitions-and-tracking-system-for-sars-cov-2-variants-of-concern-and-variants-of-interest.
Mittal A, Khattri A, Verma V. Structural and antigenic variations in the spike protein of emerging SARS-CoV-2 variants. PLoS Pathog. 2022;18(2):e1010260.
Acknowledgements
We are very grateful to the Z.A. Bashlyaeva Children’s Municipal Clinical Hospital and G.N. Speransky Children’s City Clinical Hospital No. 9 clinical staff and to the patients, parents, carers, and families for their kindness and understanding during these difficult times of COVID-19 pandemic. We would like to express our very great appreciation to ISARIC Global COVID-19 follow-up working group for the survey development. We are very thankful to FLIP, Eat & Talk, Luch, Black Market, and Academia for providing us the workspace in time of need and their support of COVID-19 research. Finally, we would like to extend our gratitude to the Global ISARIC team, the ISARIC global adult and paediatric COVID-19 follow-up working group, and ISARIC Global support centre for their continuous support and expertise and for the development of the outbreak ready standardised protocols for the data collection.
Sechenov Stop COVID Research Team (group authors)
Khazhar Aktulaeva1, Islamudin Aldanov1, Nikol Alekseeva1, Ramina Assanova1, Asmik Avagyan1, Irina Babkova1, Lusine Baziyants1, Anna Berbenyuk1, Tatiana Bezbabicheva1, Julia Chayka1, Iuliia Cherdantseva1, Yana Chervyakova1, Tamara Chitanava1, Alexander Chubukov1, Natalia Degtiareva1, Gleb Demyanov1, Semen Demyanov1, Salima Deunezhewa1, Aleksandr Dubinin1, Anastasia Dymchishina1, Murad Dzhavadov1, Leila Edilgireeva1, Yulia Filippova1, Veronika Filippova1, Yuliia Frumkina1, Anastasia Gorina1, Cyrill Gorlenko1, Marat Gripp1, Mariia Grosheva1, Eliza Gudratova1, Elena Iakimenko1, Margarita Kalinina1, Ekaterina Kharchenko1, Anna Kholstinina1, Bogdan Kirillov1, Herman Kiseljow1, Natalya Kogut1, Polina Kondrashova1, Irina Konova2, Mariia Korgunova1, Anastasia Kotelnikova1, Alexandra Krupina1, Anna Kuznetsova1, Anastasia Kuznetsova1, Anna S. Kuznetsova1, Anastasia Laevskaya1, Veronika Laukhina1, Baina Lavginova1, Yulia Levina1, Elza Lidjieva1, Anastasia Butorina1, Juliya Lyaginskaya1, Ekaterina Lyubimova1, Shamil Magomedov1, Daria Mamchich1, Rezeda Minazetdinova1, Artemii Mingazov1, Aigun Mursalova1, Daria Nikolaeva1, Alexandra Nikolenko1, Viacheslav Novikov1, Georgiy Novoselov1, Ulyana Ovchinnikova1, Veronika Palchikova1, Kira Papko1, Mariia Pavlova1, Alexandra Pecherkina1, Sofya Permyakova1, Erika Porubayeva1, Kristina Presnyakova1, Maksim Privalov1, Alesia Prutkogliadova1, Anna Pushkareva1, Arina Redya1, Anastasia Romanenko1, Filipp Roshchin1, Diana Salakhova1, Maria Sankova1, Ilona Sarukhanyan1, Viktoriia Savina1, Ekaterina Semeniako1, Valeriia Seregina1, Anna Shapovalova1, Khivit Sharbetova1, Nataliya Shishkina1, Anastasia Shvedova1, Valeriia Stener1, Valeria Ustyan1, Yana Valieva1, Maria Varaksina1, Katerina Varaksina1, Ekaterina Varlamova1, Natalia Vlasova1, Margarita Yegiyan1, Nadezhda Ziskina1, Daniella Zolochevskaya1, Elena Zuykova1
1. Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia
2. ZA Bashlyaeva Children’s Municipal Clinical Hospital, Moscow, Russia
The names of the authors are in alphabetic order.
Funding
No external funding.
Author information
Authors and Affiliations
Consortia
Contributions
DM and AAK conceptualised the project and formulated research goals and aims. EP, MR, DBa, EB, NM, YET, PP, AE, LS, DBu, JG, AAK, and DM were responsible for the study design and methodology and participated in the overall project design discussions. ADG, PC, DGP, JG, LFR, CLHB, GC, LS, JTS, MG, MGS, JOW, PO, and DM participated in the CRF development and/or provided expert input at different stages of the project. EP implemented the computer code and supporting algorithms and tested of existing code components. DM and EP tested hypotheses and discussed statistical analyses. EP performed statistical analysis. The StopCOVID Research Team, MA, EI, PBo, MP, AT, EA, AG, YF, AB, AZ, NB, ACh, EK, AK, SG, YVI, IT, AE, and LAF, conducted a research and investigation process, specifically performed data extraction, telephone interviews, and data collection. AM, ESa, EB, SB, EB, AAK, and IMO provided study materials, access to patient data, laboratory data, and computing resources. MR, DBa, YET, MA, EI, PBo, and NN managed activities to annotate metadata and maintain research data for initial use and later reuse. EP prepared visualisation and worked under DM supervision on the data presentation. DM was responsible for the oversight and leadership for the research activity planning and execution. DM, EB, AAK, MR, DBa, EB, NM, YET, PP, AE, and EP provided management and coordination for the research activity planning and execution. SM provided invaluable views from the perspective of a person with long COVID and as a parent of children with long COVID. EP, EB, and DM wrote original draft. All the authors critically reviewed and commented on the manuscript draft at both pre-and post-submission stages. All authors read and approved the final manuscript.
Authors’ Twitter handles
Daniel Munblit: @DrMunblit; Danilo Buonsenso: @surf4children.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Moscow City Independent Ethics Committee (abbreviate 1, protocol number 74). Parental consent was sought during hospital admission, and consent for the follow-up interview was sought via verbal confirmation during telephone interview. The consent process was approved by the ethics.
Consent for publication
Not applicable.
Competing interests
DM co-leads the PC-COS project, developing Core Outcome Set for post-COVID-19 condition, outside the submitted work. LFR reports grants and personal fees from Merck and Pfizer and personal fees from GSK, outside the submitted work. LS received support by the UK Foreign, Commonwealth and Development Office and Wellcome [215091/Z/18/Z] and the Bill & Melinda Gates Foundation [OPP1209135], outside the submitted work. All other authors have no conflicts of interest relevant to this article to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Criteria for hospital admission as per local clinical guidelines. Table S2. Demographic characteristics of study participants—initial and matched cases, sensitivity analysis. Table S3. Incidence and prevalence of Post COVID-19 manifestations. Figure S1. Time of study participants hospital admission and their chronological correspondence to COVID-19 variant dominance in Moscow city. Figure S2. Incidence of post-COVID-19 condition manifestations in matched exposed and reference groups, sensitivity analysis. Figure S3. Rates of events for incomplete recovery and emotional behavioural changes in matched exposed and reference groups, sensitivity analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pazukhina, E., Rumyantsev, M., Baimukhambetova, D. et al. Event rates and incidence of post-COVID-19 condition in hospitalised SARS-CoV-2 positive children and young people and controls across different pandemic waves: exposure-stratified prospective cohort study in Moscow (StopCOVID). BMC Med 22, 48 (2024). https://doi.org/10.1186/s12916-023-03221-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-023-03221-x