Abstract
Background
In order to solve the problem of “expensive medical treatment and difficult medical treatment” for patients and improve the equity of medical services, China started the health-care reform in 2009, and proposed ambitious goals of providing fair and high-quality basic medical and health services to all citizens and reducing economic burden of diseases. This study was to systematically explore the association between population economic status and incidence of catastrophic health expenditures (CHE) in mainland China in the last decade since 2009 health reform.
Methods
This systematic review was reported according to the standard of preferred reporting items for systematic reviews and meta-analyses (PRISMA). We systematically searched Chinese Electronic literature Database of China Journal Full Text Database, Chinese Biomedical Journal Database, Wan fang Data Resource System, VIP Database, and English literature databases of PubMed, SCI, EMbase and Cochrane Library from January 2000 to June 2020, and references of included studies. Two reviewers independently selected all reports from 2000 to 2020 for empirical studies of CHE in mainland China, extracted data and evaluated the quality of the study. We conducted meta-analysis of the incidence of CHE and subgroup analysis according to the time of the study and the economic characteristics of residents.
Results
Four thousand eight hundred seventy-four records were retrieved and eventually 47 studies with 151,911 participants were included. The quality scores of most of studies were beyond 4 points (91.49%). The pooled incidence of CHE of Chinese residents in the last two decades was 23.3% (95% CI: 21.1 to 25.6%). The CHE incidence increased from 2000 to 2017, then decreased over time from 2017 to 2020. From 2000 to 2020, the CHE incidence in rural areas was 25.0% (95% CI: 20.9 to 29.1%) compared to urban 20.9% (95% CI: 18.3 to 23.4%); the CHE incidence in eastern, central and western China was 25.0% (95% CI: 19.2 to 30.8%), 25.4% (95% CI: 18.4 to 32.3%), and 23.1% (95% CI: 17.9 to 28.2%), respectively; the CHE incidence was 30.9% (95% CI: 22.4 to 39.5%), 20.3% (95% CI: 17.0 to 23.6%), 19.9% (95% CI: 15.6 to 24.1%), and 23.7% (95% CI: 18.0 to 29.3%) in poverty group, low-income group, middle-income group, and high-income group, respectively.
Conclusions
In the past two decade, the incidence of CHE in rural areas is higher than that of urban residents; higher in central areas than in eastern, western and other regions; in poverty households than in low-income, middle-income and high-income regions. Further measures should be taken to reduce the incidence of CHE in susceptible people.
Similar content being viewed by others
Background
In 2009, China carried out the health-care reform, proposing the near-term goal of “effectively reducing residents’ burden of medical expenses and effectively alleviating ‘difficult and expensive to see a doctor’“, and the long-term goal of “establishing a sound basic medical and health system covering urban and rural residents, and providing the people with safe, effective, convenient, and inexpensive medical and health services”. Health-care reform has undergone major social and economic reforms, from pilot to comprehensive promotion, from industry reform to Healthy China strategy, from rapid population aging to major adjustments in family planning policies, which have brought fundamental changes to peoples’ lives and the society [1].
Since the implementation of the poverty alleviation policy, China has made great achievements. The number of poor people in the country had decreased from 165.67 million in 2010 to 30.46 million in 2017. The incidence of poverty decreased from 17. 2% in 2010 to 4.5% in 2016 [2]. However, among the current remaining poor people in China, poverty due to illness and return to poverty due to illness are the most prominent causes of poverty. Among the rural poor in my country, the proportion of poverty-stricken by disease and return to poverty due to illness reached 44.1% [3]. The incidence of disease has been one of the main causes of poverty, leaving patients and their families falling into short-term or long-term poverty [4].
CHE is a general term used to describe various health care expenditures that threaten households’ financial conditions to maintain their survival needs [5]. WHO defined CHE as health expenditures being more than 40% of household’s capacity to pay (CTP) [6, 7]. In the past decade, great achievements have been made in the National Health System Reform (NHSR) with significant improvement of access, quality and equity of health services, but there are also challenges that cannot be ignored, such as the roaring health-care costs. This is especially true in western China where the per capital income is far behind eastern China [8]. On the other side of the coin, improvement of access to health services, especially hospital services, may cause households to pay a large proportion of effective earnings, pushing households into financial hardship even poverty [9, 10].
Even though China has almost built up a universal health care system, which has played an important role in reducing the economic burden of residents’ diseases, the current basic medical security system is still sub-optimal to prevent residents’ CHE and poverty due to illness. The previous payment method of health expenditure in China was fee-for-service (FFS), which is one of the main reasons for the excessively high medical and health expenditure [11] . A study showed that in 2003, 2008 and 2013, 13.6, 15.1 and 13.8% of households experienced CHE, with a impoverishment rate of 8.6% due to disease, and 64% of non-survival expenditures for households actually incurring CHE, suggesting that CHE for the population had not improved or even increased [12], being heavy financial burden on the sick households and the society, and affected the health-care affordability of the population [13]. CHE is an important indicator of the economic incidence of disease, affecting the achievement of the “Universal Health Coverage” and the equity of the health financing system, as well as on social equity. What’s more, CHE is relative to each household, and there may be a significant imbalance between the income groups in terms of the degree of health financial security, the utilization of medical resources and the tolerance of disease incidence [14].
Therefore, the objective of this study was to examine the CHE in mainland China in the last two decades and its association with socioeconomic status of residents. And this research also explored the trends of CHE in the last two decades and gaps between regions.
Methods
A systematic review was conducted according to the standard of preferred reporting items for systematic reviews and meta-analyses (PRISMA) [15].
Literature search
We systematically searched Chinese literature databases including China Journal Full Text.
Database, Chinese Biomedical Journal Database, Wan fang Data Resource System, VIP Database, and English literature databases including PubMed, SCI, Embase and Cochrane library. The search terms included “catastrophic health expenditure,” “catastrophic medical expenditure,” “poverty-causing health expenditure,” “impoverishment,” “poverty-induced poverty,” “return to poverty due to illness,” “catastrophic health spending,” “catastrophic health spending,” “health payments,” “death by diseases,” “return to poverty due to illness.” The search strategy was firstly formed in PubMed and adopted for other databases (see appendix search strategy). In addition, reference lists of included studies were scanned for more eligible studies. The search period was from January 2000 to June 2020.
Inclusion criteria
The inclusion criteria were: (1) research in mainland China; (2) quantitative studies including randomized controlled trial, non-randomized controlled trial, controlled before-after study, non-controlled before after study, cross-sectional study, cohort study or interrupted time series study; (3) the threshold for the incidence of CHE is 40%.; (4) all study populations; (5) and reported the incidence of CHE and economic status of participants. The language of literature was limited to Chinese and English, since almost all research in China were published in these two languages.
Study selection
Firstly, two reviewers (Qingqing Yuan and Yuxuan Wu) screened the titles and abstracts of the identified citations and removed those obviously not relevant to the subject. Then, according to the inclusion criteria, two reviewers (Yuxuan Wu and Furong Li) select eligible studies by reading the full text. IF there was a disagreement, the three discussed until a consensus was reached. If consensus could not be reached, a senior researcher (Kun Zou orDandi Chen) was consulted for final decision.
Data extraction and quality evaluation
Data Extraction and quality evaluation was performed by two reviewers independently (Qingqing Yuan, Yuxuan Wu). Different opinions were decided by discussion.
Data were collected using pre-designed data extraction table, including the author, year of publication, study location, study period, research design, characteristics of participants, sample size, number of CHE and economic status. If there were multiple reports on the harmonized data, priority is given to the most comprehensive publication. If two survey subjects come from the same survey data, select the literature with the most complete data to be included in the study. The quality of included studies was evaluated using the AHRQ scale [16]. The AHRQ had 11 entries, with an answer of “yes” with 1 point, and an answer of “no” or “not clear” with 0 point, with a total score of 0 to 11.
Statistical analysis
Firstly, heterogeneity between included studies was examined using I2, with I2 > 50% indicated substantial heterogeneity. The pooled incidence of CHE was estimated with 95% confidence interval (CI) using fixed effect model if there was no heterogeneity (I2 < 50%). Otherwise, random effect model was used. Subgroup analysis was conducted by study period (three-years interval from 2006 to 2020), residency (urban or rural areas), the level of socio-economic development (categorized into east, central, and western regions, if the object of the survey area has multiple cities, then divided into other. The level of social and economic development in the east is the best, in the middle is general, and in the west is poor) [17], family income levels (poverty, low-income levels, middle-income, high-income, the poverty standard is based on the poverty line or the minimum living security line stipulated by the local civil affairs department, then divide the remaining families into three equal groups according to their income) [18], to explore their relationships with CHE. We also compared the growth relationship between the incidence of CHE and total health expenditure per capita (data from the National Bureau of Statistics of China) in different time periods. Meta-regression was performed to the disease type, the secular trend, the rural and urban residency, the social development level by region and the household income level adjusted for each other. All statistical analysis was conducted used Stata 15.0 software.
Results
Study selection
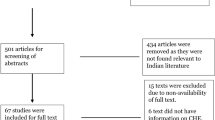
A total of 4874 citations were retrieved, 575 were likely to be relevant after viewing the titles and abstracts. Then by reading the full texts, 47 eligible studies (44 in Chinese and 3 in English) with 151,911 participants were finally included. (Fig. 1).
Characteristics of included studies
A total of 47 cross-sectional studies including 151,911 participants were included in this study. The locations of studies were across-provinces (17), Yunnan (6), Hubei (4), Shandong, (4), Shanghai (3), Sichuan (3), Hebei (3), Shaanxi (2), Gansu (2), Jiangsu (2),Chongqing (2), Shanxi (2), Guangdong (1), Heilongjiang (1), Jiangxi (1), Liaoning (1), Qinghai (1), and Xingjiang (1). The included participants were general population (40), middle-aged and elderly people (4), rural villagers (30), cancer patients (2), HBV patients (2), etc. The quality scores of most of studies were between 4 and 9 points (81.67%) (Table 1).
Pooled incidence of catastrophic health expenditure for Chinese residents
The overall incidence of CHE in the past 14 years (2006 to 2020) among Chinese residents was 23.3% (95% CI: 21.1 to 25.6%), and there was a significant heterogeneity between the studies (I2 = 99.3%, P < 0.001), so random effect model was used (Fig. 2).
1
Subgroup analysis
Secular trend
In general, with the change of time, the incidence of CHE showed an upward trend. It was 18.6% (95%CI: − 1.5 to 38.8%), 19.6% (95%CI:18.2 to 21.0%), 18.0% (95%CI:14.9 to 21.0%), 27.8% (95%CI:22.6 to 33.0%), and 25.5% (95%CI:18.8 to 32.2%) for year 2006 to 2008, 2009 to 2011, 2012 to 2014, 2017 to 2017, and 2018 to 2020 respectively (Fig. 3, Additional file 1: figure 1 for forest map).
Rural and urban residency
The incidence of CHE in rural area was 25.0% (95%CI: 20.9 to 29.1%), higher than the urban 20.9% (95%CI:18.3 to 23.4%) (Additional file 1: figure 2 for forest map).
Social development level by region
The incidence of CHE in the central was higher than in the eastern, west region. The pooled incidence of CHE was 25.4% (95%CI: 18.4 to 32.3%) in the central, 25.0% (95%CI: 19.2 to 30.8%) in eastern China, 23.1% (95%CI: 17.9 to 28.2%) in the west and 18.8% (95%CI: 16.5 to 21.2%) in the rest (Additional file 1: figure 3 for forest map).
Household income level
The incidence of CHE in poverty group is higher than that of low-income group, middle-income group and high-income group. The incidence of CHE in poverty households was 30.9% (95%CI:22.4 to 39.5%), For the low-income, middle-income and high-income households, the CHE incidence was 20.3% (95% CI: 17.0 to 23.6%), 19.9% (95% CI: 15.6 to 24.1%), and 23.7% (95% CI: 18.0 to 29.3%), respectively (Additional file 1: figure 4 for forest map).
Meta-regression of associated factors of incidence of catastrophic health expenditure
In all studies, a meta-regression analysis was conducted to explore the impact of heterogeneous sources (including disease type, secular trend, rural and urban residency, social development level by region and household income level). The results show the disease type (p > 0.05), the secular trend (p > 0.05), the rural and urban residency (p > 0.05) and the social development level by region (p > 0.05) and the household income level (p > 0.05) are non-significant regulators (Table 2).
Publication bias
There was statistically significant publication bias in included studies (p<0.001).
The funnel plot of publication bias was shown in Additional file 1: Figure 5.
Discussion
There are four main findings in this study. First, the incidence of CHE in rural areas was significantly higher than that in urban areas. Second, the incidence of CHE in central areas was higher than that in eastern and western areas, and lowest in the other areas. Third, poverty group had higher CHE incidence than that of low-income group, middle-income group and high-income group. Finally, disease type may affect the incidence of CHE.
The incidence of CHE in rural areas was significantly higher than that in urban areas. The income gap between urban and rural areas makes the proportion of rural households’ cash health expenditure higher than that of urban households, and the rural population faces greater CHE risks. Although the establishment and expansion of the New Cooperative Medical Scheme (NCMS) reduces the medical burden of poor rural residents [65], the NCMS is lower than the Urban Employee Basic Medical.
Insurance (UEBMI) in terms of fund-raising, security level and reimbursement scope. The combination of the two causes a higher risk of CHE in rural households. In addition, from 2009 to 2014, the average cost of inpatients nationwide increased from 5951.80¥ to 8290.50¥, an average annual increase of 6.86% [11]. The excessively rapid increase in medical costs partially offset the protective effect of the basic medical insurance system. The burden continues to increase.
The incidence of CHE in central areas was higher than that in eastern and western areas. The results of Li′s research found that the incidence of CHE is in the opposite direction to the regional economic level: that is, the incidence of CHE in the more economically developed areas is lower, the incidence rate in the eastern areas is the lowest, the central region is the second, and the western region is the highest [11]. This study is contrary to its results. The reason may be related to thecharacteristics of the research object, the representativeness of different literature samples is different.
The poverty group had the highest incidence of CHE, followed by the high-income group, followed by the low-income group, and the middle-income group had the lowest incidence of CHE. There are many reasons for this phenomenon. On the one hand, it may be passively over-utilized health services due to induced demand [66], that is,these families are more likely to accept more expensive drugs or over-checks provided by doctors, thereby increasing medical expenses [67]. This is a relatively common phenomenon in China; on the other hand, high-income groups may actively over-utilize health services [67], such as using higher-level nursing services or wards. This will also increase medical expenses and make families incur excessive cash health expenditures, thereby widening the overall disparity in CHE of middle-income groups. Of course, in the less developed areas of China, it may not be common for farmers to choose such special needs, but this cannot be ruled out. The poverty group will also be affected by induced demand, but due to economic reasons, its affordability for medical expenses (including the cost of induced demand) is limited.
When medical expenses exceed their ability to pay, poor families generally choose Abandon treatment [68]. It is also because of its low income that it cannot pay large amounts of health expenses, and the gap in catastrophic health expenditure may be reduced, but this also makes the use of normal health services for some poor people suppressed and its health level will be seriously affected.
Disease type may affect the incidence of CHE. Wang’s research shows that the risk of catastrophic health expenditures in families with chronically ill patients is generally higher than the average of the overall population, and there are inequalities based on income gaps [69].Wu’s research shows that there are inpatients at home, and the risk of catastrophic health expenditure is 2.5 times higher than that of the general population [70].
The overall incidence of CHE in the past 14 years (2006 to 2020) among Chinese residents was 23.3% (95% CI: 21.1 to 25.6%).Compared with other countries, the global incidence of CHE at the 10% threshold was estimated as 9.7% in 2000, 11.4% in 2005, and 11.7% in 2010. In 2010, the incidence of CHE in Asia was 3.1% [71]. In 2015, the incidence of CHE in South Korea was 2.4% [72], and in 2021, Iran’s survey results show that the incidence of CHE is 4.7% [73]. The possible reason for this situation is that this study did not distinguish patients from the general population, so it may overestimate the incidence of CHE.
Some specific measures targeting economic vulnerable groups are needed in order to reduce the incidence of CHE in China. First, policies are needed to increase the protection effects of the three types of social medical insurance, including scope and reimbursement ratio. While expanding the coverage of medical insurance in China, it needs deepen the coverage of medical insurance, such as increasing the actual compensation ratio of medical insurance;Expand the scope of medical insurance reimbursement and allow more expensive special-effect medicines and treatments to enter the medical insurance reimbursement catalog. Second, increase the scope and intensity of medical assistance and social assistance. Further strengthen the protection of the disadvantaged groups, chronic patients and other vulnerable groups, and give inclined support to the system. Establish medical assistance for severely and seriously ill patients to prevent them from becoming poor due to illness or becoming poor due to illness. Third, control the excessive growth of medical expenses.
Conclusion
Ten years after the new health reform in China, economic vulnerable groups still have higher risk of CHE than other groups. More research is needed to identify these population groups. And future health policies are warranted to contain healthcare cost, strength health financing protection and reduce the CHE in China towards universal health coverage.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Wang H. Review of the 10-year history of medical reform in China and its future prospects. Chinese Hosp Manage. 2019,39(12):1-5.
National Bureau of Statistics. China rural poverty monitoring report (2017).
Yi J, Yao T, Hongping L, et al. Evolution, current situation and improvement of China's health poverty alleviation policy. Chinese Health Serv Manage. 2019;36(09):668-71.
Wang H. Study on the economic incidence of disease and compensation effect of new rural cooperative medical system for rural residents; 2016.
Yongjian X, Jianmin, et al. Measurement and explanation of socioeconomic inequality in catastrophic health care expenditure: evidence from the rural areas of Shanxi Province. BMC Health Serv Res. 2015;15(1):256.
P. M. Public spending on health care: how are different criteria related? Health Policy. 2000;53:61–7.
Waning B, Maddix J, Tripodis Y, Laing R, Leufkens HGM, Gokhale M. Towards equitable access to medicines for the rural poor: analyses of insurance claims reveal rural pharmacy initiative triggers price competition in Kyrgyzstan. Int J Equity Health. 2009;8(1):43. https://doi.org/10.1186/1475-9276-8-43.
Chen G, Inder B, Hollingsworth B. Health investment and economic output in regional China. Contemp Econ Policy. 2014;32(2):261–74.3. https://doi.org/10.1111/coep.12022.
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–7.4. https://doi.org/10.1016/S0140-6736(03)13861-5.
Zhou Z, Gao J. Study of catastrophic health expenditure in China’s basic health insurance. HealthMED. 2011;5:1498–507.
Ye L, Wu Q, Gao L. An analysis of the institutional causes of catastrophic health expenditure of rural residents in my country. China Health Policy Res. 2012;005(011):55–9.
Ju'e Y, Nina H, Liao S, et al. Changes in catastrophic health expenditures of rural families before and after the new medical reform and their influencing factors: based on a sample survey of Meixian County, Shaanxi Province. China Health Policy Res. 2013;6(2):30–3.
Tianyi Z, Liying Z, Xiaowei M, et al. Research on catastrophic health expenditure and its influencing factors in rural households in Shaanxi Province before and after medical reform. Med Soc. 2015;26(1):1–3.
Suwan Z, Ting L. Analysis of the relationship between patients' family income and catastrophic medical expenditures. China Township Village Enter Account. 2019;03:284–5.
Alessandro Liberati D, Dsc DGA, Jennifer Tetzlaff B, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):65–94.
Hibbard J, Sofaer S. U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality.[J]. Patient Safety & Quality An Evidencebased Handbook for Nurses; 2012.
Guojie C. An analysis of the causes of the differences in the development of the east, the middle, and the west of China. Geographical Sci. 1997;01:2–8.
Wang Q. Research on the impact of catastrophic medical expenditure on rural poverty in China——based on Chinese family tracking survey. China Health Policy Res. 2016;9(02):6–10.
Lu H, Zheng J, Ying H. Analysis of the equity of the new rural cooperative medical care families in Shanxi Province. China Rural Health Serv Manage. 2006;26(11):3–6.
Xiaorong J, Xingbao C, Wenzhong Z, et al. Study on the ability of the new rural cooperative medical system in the suburbs of Shanghai to prevent poverty caused by disease. Health Econ Res. 2006;1:34–5.
Xiaojie S, Rehnberg C, et al. Study on disastrous health expenditure of urban residents in Xining and Yinchuan City. China Health Serv Manage. 2008;(01):12-15.
Ying C, Junan L, Jianli Y, et al. Analysis of catastrophic health expenditures of families with hypertension and its comorbidities in impoverished rural areas. China Primary Health Care. 2011;03:41–3.
Wan Y, Luo M, Lin Y, et al. Analysis of influencing factors of catastrophic health expenditure of rural low-income families in Sichuan. Mod Prev Med. 2011;38(23):4889–91.
Jun C, Zheng Y, Deng H, et al. Analysis on the status of catastrophic health expenditures of families with new tuberculosis patients in non-hukou population. Shanghai Prev Med. 2012;11:10–2.
Renyou C, Aitian Y, Wenjing Z, et al. Study on the influencing factors of catastrophic health expenditure of rural residents in Tengzhou City. China Health Econ. 2012;31(03):19-21.
Li Y, Wu Q, Xu L, Legge D, Hao Y, Gao L, et al. Factors affecting catastrophic health expenditure and impoverishment from medical expenses in China: policy implications of universal health insurance [J]. Bull World Health Organ. 2012;90(9):664–71. https://doi.org/10.2471/BLT.12.102178.
Wang W. Research on the status of catastrophic health expenditure in urban households and its medical security system: Hebei University of Economics and Business; 2012.
He X, Zaiyu C, Ma A. Analysis of demographic characteristics of farmers' poverty caused by disease in China. Modern Bus Ind. 2013;25(09):58–60.
Li X, Shen JJ, Lu J, et al. Household catastrophic medical expenses in eastern China: determinants and policy implications. BMC Health Serv Res. 2013;13(1):506.
Jiangmei Q, Dongsheng R, Wu N, Yanchun Z, Lifang Z, Mao L. Comparative analysis of the occurrence of catastrophic health expenditures: a health inquiry survey on typical urban residents based on comprehensive reform of community health. China Health Econ. 2013;32(09):65–8.
Baotang S. Research on the operation status of new rural cooperative medical system in Yulong County, Yunnan Province and its impact on Farmers' family medical burden: Kunming Medical University; 2013.
Fang Y, Deng A, Yao F, et al. Analysis of the incidence of poverty caused by disease in rural families with maternal deaths. China Health Econ. 2013;12:24–6.
Wenqi F, Baoyu L, Qinghua Z, et al. Analysis of disastrous health expenditure of rural households in Heilongjiang Province. China Health Econ. 2014;2:46–7.
Xiaohong L. Research on disastrous medical expenditure, Farmers' vulnerability and medical security: Nanjing Agricultural University; 2014.
Baoli S, Cong S. Research on access to health services and equity of medical burden for low-income farmers. Soft Sci Health. 2014;05:18–21.
Xu X, Jing L, Shiping F, et al. Analysis of catastrophic health expenditure status and influencing factors of stroke patients in northern Guangdong. Soft Sci Health. 2014;28(08):491-4.
Yi Y, Hui Z, Wang Y, et al. Research on the influencing factors of catastrophic health expenditure in rural households in Weishan County, Dali prefecture. Soft Sci Health. 2014;28(4):205–7.
Hui L. Research on cash health expenditure and catastrophic health expenditure of residents in a certain area of eastern Xinjiang; 2015.
Che YH, Chongsuvivatwong V, Li L, Sriplung H, Wang YY, You J, et al. Financial burden on the families of patients with hepatitis B virus-related liver diseases and the role of public health insurance in Yunnan province of China. Public Health. 2016;130:13–20. https://doi.org/10.1016/j.puhe.2015.03.015.
Gao M, Yang J, Hong Y, et al. Disastrous health expenditure of rural households in Hubei Province and its influencing factors. China Health Stat. 2016;33(06):1008-9+1013.
Xitong L. Research on disastrous health expenditure of hospitalized patients in Chongqing and its influencing factors [D]: Chongqing Medical University; 2016.
Luo H. Analysis of compensation pattern and implementation effect of rural residents' serious illness insurance based on UHC perspective: Huazhong University of Science and Technology; 2016.
Wang H. Discussion on the criteria for defining catastrophic health expenditure in rural households: a case study of Qianxi County, HebeiProvince. Economist. 2016(11):132-3.
Wang Z, Xiangjun L. Analysis of economic incidences and influencing factors of rural chronically ill families. Med Philosophy. 2016(37):55-7.
Wu X. A study on the economic burden of lung cancer patients and the impact of medical insurance policies in Nanchang City: Nanchang University; 2016.
Nanzi X. An empirical study on the economic risk of diseases of hypertension and diabetes in rural areas under the basic medical insurance system: Chongqing Medical University; 2016.
Chunguang Z. Catastrophic health expenditure measurement and influencing factors of urban and rural residents in Gansu Province: North China University of Technology; 2016.
Qi Z, Wei L, Yi L, et al. Analysis of catastrophic health expenditure status of rural residents in Shenyang and its influencing factors. China Public Health. 2016;3:306–9 4 pages in total.
Yujin Z, Yuxin T, Qun Z, et al. Research on disastrous health expenditure and its influencing factors of rural households in Zigong City, Sichuan Province before and after new rural cooperative medical care compensation. J Sichuan Univ. 2016;47:771.
Zengyi F. Analysis of disastrous health expenditure of households in a City in Western Hubei Province and its influencing factors. Med Soc. 2017;30(04):52-5.
Gao G, Ma Y, Hu X, et al. Evaluation of the effect of the new rural cooperative medical care insurance system on mitigation of catastrophic health expenditures. Soc Sec Res. 2017;(02):69-76.
Jing L. Research on disastrous health expenditure and economic incidence of disease in residents of Taiyuan City: Shanxi Medical University; 2017.
Xiangrong L, Rong T. Research on the status and influencing factors of disastrous health expenditure of rural households in Yinchuan City. China Prim Health Care. 2017;31(007):1-3.
Yuxia N. Research on the status quo and influencing factors of catastrophic health expenditures of diabetics in urban and rural residents in Shandong Province: Shandong University; 2017.
Yu J. Influencing factors and countermeasures of poverty among rural residents due to illness: Shaanxi Normal University; 2017.
Hongbo D, Wu Z. A study on the poverty of the elderly in Hebei Province——based on a field survey of 14 counties in Hebei Province. J Hebei Univ (Philosophy and Social Sciences Edition). 2018;43(1):112–9.
Jingjing H, Le C, Xiao L, Wenlong C, Wang G, Lu S. Status of diabetes incidence and disease economic incidence in rural elderly in Midu County, Yunnan Province. China Public Health. 2019;35(11):1461–4.
Shusheng H, Aitian Y. Disastrous health expenditures of rural families in Shandong Province and their influencing factors. China Public Health. 2018;34(9):1221–3.
Qing L, Le C, Wenlong C, Dingyun Y, Wang W, Yuecui L, et al. Incidence of 4 chronic diseases in rural residents in Yunnan Province and their impact on family economy. China Public Health. 2018;34(04):479–82.
Xiangjun L, Huiyong S. Study on the economic incidence of disease in the middle-aged and elderly in Jiangsu Province: Higher Vocational Medical Education and Modern Nursing; 2018.
Wang Y, Peiyuan Q, Fan T, et al. Research on the status of catastrophic health expenditure of rural families in Fushun County, Sichuan Province and its influencing factors. China Public Health. 2019;35(02):152–6.
Guoan Z, Yang P. The impact of catastrophic medical expenditure on the income gap between Chinese households——a study based on CFPS survey data [J]. Jianghan Forum. 2018;05:25–33.
Ang Zheng, Wenjuan D, Lin Z, et al. How great is current curative expenditure and catastrophic health expenditure among patients with cancer in China? A research based on “System of Health Account 2011”. Cancer Med. 2018;7(8):4036-43.
Yu Z, He L, Shuying D, Wei C, Ying C, Qiong M, et al. Analysis of catastrophic health expenditure and influencing factors of households in Zhaotong City. Health Soft Sci. 2019;33(12):31–3.
Yang H, Meng H. A study on the disparity of disastrous health expenditure between urban and rural areas and the sensitivity of distribution. China Health Policy Res. 2018;011(007):24–9.
Peng L, Wu Z. Research on the formation mechanism of over-medical problems in public hospitals in my country. Chinese Health Econ. 2014;5.
Wenqi F, Baoyu L, Qinghua Z, et al. Analysis of catastrophic health expenditures of rural households in Heilongjiang Province. China Health Econ. 2014;2:46–7.
Manxiu N, Jin L. The impact of new rural cooperative medical system on Farmers' medical burden——an empirical analysis based on the perspective of supplier induced demand. J Public Manag. 2014;3:59–69.
Wang Z, Xiangjun L. Influential factors and inequality analysis of catastrophic health expenditure of elderly chronically ill families. Popul Dev. 2014;020(003):87–95.
Wu Q, Ye L, Xu L, et al. Analysis of the effect of medical insurance system on reducing catastrophic health expenditures of residents in my country [J]. China Health Policy Res. 2012;09:66–70.
Adam W, Gabriela F, Justine H, Marc-François S, Kateryna C, Buisman Leander R, et al. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Global health. 2018;6(2):169-79.
Lee HJ, Lee DW, Choi D-W, Sarah Soyeon O, Kwon J, Park E-C. Association between changes in economic activity and catastrophic health expenditure: findings from the Korea Health Panel Survey, 2014–2016. Cost Effect Res Allocation. 2020;18(1):36.
Doshmangir L, Yousefi M, Hasanpoor E, et al. Determinants of catastrophic health expenditures in Iran: a systematic review and meta-analysis. Cost Effect Res Allocation. 2020;18(1).
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Qingqing Yuan and Yuxuan Wu contributed to study selection, data extraction and quality evaluation. Furong Li contributed to study selection and data analysis. Min Yang contributed to opinion consultation. Dandi Chen and Kun Zou contributed to opinion consultation, conceived and designed the experiments. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests in this section.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yuan, Q., Wu, Y., Li, F. et al. Economic status and catastrophic health expenditures in China in the last decade of health reform: a systematic review and meta-analysis. BMC Health Serv Res 21, 600 (2021). https://doi.org/10.1186/s12913-021-06408-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-06408-1