Abstract
Background
The use of telemedicine technology has significantly increased in recent years, particularly during the Covid-19 pandemic. This study aimed to investigate the use of telemedicine technology for cancer patients during the Covid-19 pandemic.
Methods
This was a scoping review conducted in 2023. Various databases including PubMed, Web of Science, Scopus, Cochrane Library, Ovid, IEEE Xplore, ProQuest, Embase, and Google Scholar search engine were searched. All quantitative, qualitative, and mixed-method studies published in English between 2020 and 2022 were included. Finally, the needed data were extracted, and the results were synthesized and reported narratively.
Results
A total of 29 articles were included in this review. The results showed that teleconsultation, televisit, and telerehabilitation were common telemedicine services, and video conferencing and telephone were common technologies used in these studies. In most cases, patients and healthcare providers preferred these services compared to the face-to-face consultations due to their convenience and advantages. Furthermore, the findings revealed that in terms of clinical outcomes, telemedicine could effectively reduce anxiety, pain, sleep disorders, and hospital admission rates.
Conclusion
The findings provided valuable insights into the various telemedicine technologies, services, users’ perspectives, and clinical outcomes in cancer patients during the Covid-19 pandemic. Overall, the positive outcomes and users’ satisfaction showed that the use of telemedicine technology can be expanded, particularly in cancer care. Future research needs to investigate both clinical and non-clinical effectiveness of using various telemedicine services and technologies for improving cancer care delivery, which can help to develop more successful strategies for implementing this technology.
Similar content being viewed by others
Background
Cancer is a widespread public health concern, with more than 19 million new cancer cases and about 10 million cancer-related deaths reported worldwide in 2020 [1, 2]. The International Agency for Research on Cancer (IARC) reported that globally, one out of five people is susceptible to develop cancer during their lifetime, and one out of every eight men and one out of every 11 women may die from cancer. It seems that an increase in the global population, diseases, and economic factors are the main risk factors for increasing the prevalence of cancer [3].
Recent studies have shown that cancer patients face an increased possibility of being diagnosed with Covid-19 and they experience more severe clinical manifestations [4]. Moreover, the mortality of cancer patients due to Covid-19 is higher compared to the people without cancer [5]. Cancer patients are more affected by the side effects of Covid-19, and the lack of adequate and timely care for these patients may lead to an increase in their mortality rate [4].
There are a number of risk factors that cause cancer patients being affected by Corona virus transmission. These risk factors include the progression of the disease, the suppressive nature of the immune system, frequent visits to hospitals for active chemotherapy, radiotherapy, immunotherapy, targeted therapy and immunosuppressant for bone marrow transplantation [6, 7]. As a result, telemedicine tools have been recommended to reduce disease transmission rates while continuing medical care provision remotely, particularly during the pandemic [8, 9].
Although telemedicine technology is not a novel method for providing cancer patients with a variety of healthcare services, such as diagnosis, consultation, treatment, and home care [10], the use of this technology has increased during the Covid-19 pandemic, mainly due to the high workload on the healthcare system and the provision of global strategies such as social distancing and quarantine requirements. These reasons encouraged cancer patients to use telemedicine technologies instead of receiving an in-person visit in medical centers [11, 12]. The use of telemedicine has a number of advantages. For example, it can help to reduce the waiting times compared to the traditional in-person visits at healthcare centers [13]. However, despite the advantages and positive users’ attitudes, there are still concerns over the lack of face-to-face communication and the inability to conduct physical examinations [14].
So far, several review studies have been conducted; however, a few of them discussed the use of telemedicine technology by cancer patients during the Covid-19 pandemic [15,16,17]. The review studies in this area were also scarce and their objectives were different [15, 17, 18]. Therefore, in the current study, we aimed to conduct a scoping review to systematically investigate and consolidate the evidence related to the application of telemedicine technology for cancer patients during the Covid-19 pandemic. By adopting a scoping review methodology, we could provide a comprehensive understanding of different types of technology, services, users’ perspectives, and clinical outcomes of using telemedicine technology within the context of cancer care during the pandemic. The results can be useful for future research, further technology development, and response to the unique needs of cancer patients especially during the pandemic.
Methods
This scoping review was conducted in 2023 and different types of research, in which telemedicine intervention was used for cancer patients during the Covid-19 pandemic and its outcome was evaluated, were reviewed. Unlike systematic reviews, which typically focus on a narrow research question and employ a rigorous method to assess the risk of bias and quality, scoping reviews provide a broad overview of the available literature without a formal assessment of these factors [19]. To achieve this goal, Arksey and O’Malley’s framework [19] was used. Before conducting this research, ethics approval (IR.IUMS.REC.1401.392) was obtained from the National Ethics Committee of Biomedical Research.
Stage 1: identifying the research question
Before developing a search strategy for review studies, the research question should be explained clearly. The initial literature review suggested that the literature about the use of telemedicine technology for cancer patients during the Covid-19 pandemic was scarce; therefore, we generated research questions as follows:
-
How was telemedicine technology used for cancer patients during the Covid-19 pandemic?
-
What was the outcome of telemedicine technology used for cancer patients compared to in-person visits?
Stage 2: identifying relevant studies
To identify relevant studies, eight databases including PubMed, Web of Science, Scopus, Cochrane Library, Ovid, IEEE Xplorer, ProQuest, and Embase as well as the Google Scholar search engine were searched. The search timeframe was between 1st January 2020 and 31th December 2022 to access all relevant studies published during the pandemic. The search strategy consisted of three main terms: “Covid-19”, “Telemedicine” and “Cancer,” along with their corresponding synonyms and MeSH terms. All of them were combined using AND OR logical operators to create search strategies for different databases (Table 1). The reference list of the selected studies and their citations were also searched to ensure that all relevant studies were included.
Stage 3: study selection
The current study utilized specific criteria for including and excluding articles during the selection process. The inclusion criteria consisted of original articles published in English in which quantitative, qualitative, or mixed methods approaches were used to evaluate telemedicine interventions for cancer patients during the Covid-19 pandemic, and their results were compared with the in-person visits.
The exclusion criteria encompassed review articles, letters to the editor, protocols, and studies that did not involve the evaluation of telemedicine technology by cancer patients or their care providers. Furthermore, studies that were not published in the English language, those that focused on cancer survivors instead of individuals currently undergoing treatment, those that did not report clinical outcomes or did not gather users’ perspectives (patients or care providers), abstract-only documents, and full-texts that were not accessible were all excluded from this review study.
Stage 4: charting the data
To perform a complete search on the subject, all related keywords and MeSH terms were identified and combined. The retrieved studies were organized using EndNote software, and after removing duplicates, the remaining articles were screened in terms of the title and abstract relevancy to the aim of the study. The full text of eligible studies was then retrieved and reviewed. Both authors contributed to screen the articles independently and any disagreements between them were resolved via discussion.
The required data were extracted using a data extraction form and included the author(s) name, country of the study, year of publication, study objective, type of telemedicine technology, type of cancer, type of services (such as diagnosis, treatment, consultation, screening or home care), users’ (patients’ and healthcare providers’) perspectives regarding the use of telemedicine technology for cancer patients during the Covid-19 pandemic, and clinical outcomes.
Stage 5: collating, summarizing, and reporting the results
The extracted data were tabulated, summarized, and reported narratively. Results were reported by categorizing studies according to the type of services, type of technology, patients’ and providers’ opinions, and clinical outcomes.
Results
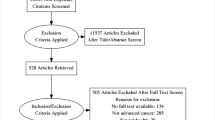
Initially, 3501 articles were retrieved and after completing the screening process based on the PRISMA-ScR statement and applying the inclusion and exclusion criteria, 29 studies [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48] were identified for the final review. Figure 1 shows the process of selecting articles.
Characteristics of the selected studies
The results showed that most studies (n = 19) were conducted in the United States [20, 22,23,24,25, 28, 30,31,32,33,34,35,36, 39,40,41, 43, 44, 47]. Other studies were completed in the United Kingdom (n = 3) [27, 37, 42], Italy (n = 2) [26, 48], Australia (n = 2) [29, 45]. Saudi Arabia (46), China (21), and Canada (38) each contributed to publish one relevant study. Most of the article (n = 17) were published in 2022 [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. Table 2 shows a summary of the articles included in the study.
Types of telemedicine technology
Video conferencing [20,21,22,23,24,25, 30, 32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48], telephone [22, 23, 26,27,28,29, 33, 36,37,38,39,40,41,42,43,44,45, 47] and messenger applications such as WeChat [21] were the most commonly used technologies. The platforms used for video conferencing were Zoom [23, 30, 31, 33, 34, 41], Jeff Connect [25, 35], Microsoft Teams [38, 48], WeChat [21], and MyChart [20]. Additionally, the results showed that using video conferencing helped with discussing various treatment plans [20, 22, 23, 31, 32, 34, 39, 41, 45, 46, 48] and patients’ symptoms [20, 21, 23, 24, 36, 37, 42, 46, 47], as well as receiving advice and self-care recommendations from the physicians [20,21,22,23, 25, 30, 33, 35, 36, 43, 45, 47, 48].
Similarly, telephone-based telemedicine services helped with receiving advice about the clinical symptoms of cancer patients [23, 29, 36, 42, 47], scheduling the next appointments [27, 28, 39], and receiving regular consultation services [22, 23, 26,27,28,29, 33, 36,37,38,39,40,41,42,43,44,45, 47]. In addition, for cancer patients who were in the initial stages of the disease, telephone consultation was an effective way to receive continuous care and support [45]. In Chen et al.‘s study, the results showed that the messenger applications facilitated message exchange for the rehabilitation of cancer patients during the Covid-19 pandemic [21].
Types of telemedicine services
Teleconsultation (n = 13) [20, 22, 23, 30,31,32,33,34, 39, 41, 45, 47, 48], televisit (n = 13) [24,25,26,27,28,29, 35, 36, 40, 42,43,44, 46], telerehabilitation (n = 3) [21, 37, 38] and telemonitoring (n = 1) [21] were the main types of telemedicine services provided to the cancer patients. Teleconsultation and televisit were the most common types of services that allowed cancer patients to communicate with healthcare providers without having to leave their homes and helped to eliminate the need to visit health centers and minimize the risk of virus exposure [20, 22, 23, 30,31,32,33,34, 39, 41, 45, 47, 48]. Televisit was used to provide ongoing care through symptom management and drug prescription for cancer patients [24,25,26,27,28,29, 35, 36, 40, 42,43,44, 46].
Telerehabilitation was another telemedicine service which was used to provide physiotherapy [21, 38] and occupational therapy [37] for cancer patients during the Covid-19 pandemic Telemonitoring was used to continuously track vital signs and provided feedback regarding the progress of patient rehabilitation, which could be useful in motivating and improving the effectiveness of telerehabilitation in the era of Covid-19 [21].
Patients’ and healthcare providers’ perspectives
According to the results, in some studies, patients were highly satisfied with telemedicine services [20, 30, 39, 44, 45, 48]. Patient satisfaction was specifically related to the audio/video quality [30, 39], ease of communication [30, 38], technology ease of use [30, 38, 39], comfort, appropriate length of visit, and overall experience of using telemedicine technology compared to the in-person visits [44]. In some studies, physicians were also highly satisfied with the use of telemedicine technology in the field of cancer care [20, 30, 45]. For example, Aghdo et al. showed that physicians were satisfied with the teamwork, increased communication, and quality of care which were resulted from using telemedicine technology [30].
The findings also showed that most patients were willing to use telemedicine technology compared to the in-person consultations [20, 22, 25, 27, 28, 31, 32, 35, 39, 47]. Their main reasons included reducing the number of in-person visits [32, 43], feeling more comfortable [31, 35], improving the follow-up services [25, 35], and increasing the number of successful appointments [28, 47] compared to the in-person visits.
The main benefits of telemedicine for patients included eliminating unnecessary travels [24, 25, 33, 34, 37, 42], saving time [29, 33, 37, 38, 42] and cost [21,22,23, 27, 29, 34, 37, 38], better and easier access to medical services [24, 25, 27], facilitating family members engagement [34], more flexibility in making appointments [29, 37], increasing the duration of visits [24, 29], improving adherence to medical advice [41] and reducing the risk of exposing to Covid-19 [24, 25, 27, 33, 34, 48]. Healthcare providers could also benefit from reducing the workload [33] and collaborating with other caregivers and specialists inside and outside the hospital [41].
There were also some challenges to the use of telemedicine technology by patients and their care providers [20, 24, 25, 27, 29, 33,34,35, 37,38,39, 41, 42, 44]. For instance, inability to conduct physical examinations and monitor the clinical symptoms of patients [20, 24, 25, 29, 34, 35, 38, 41, 44], limited physician-patient interactions [20, 24, 25, 27, 29, 35, 44], concerns over data privacy and security [24, 25, 35, 37], and issues with Internet connectivity and IT support [33, 34, 37, 39, 41] were some of these challenges.
Patients were concerned about the lack of access to communication tools and appropriate equipment (such as the Internet and personal computers) [38], low technical skills and e-literacy [24, 33, 34, 37, 38, 41], medical responsibility [20], and care quality through telemedicine [20, 37, 39]. Similarly, healthcare providers were concerned with the compatibility of technology with their common workflows [33, 35, 41], limited access to patient information and medical records [20, 33, 41], and reimbursement difficulties [20, 33, 41] as challenges hindering them from using telemedicine effectively. The results of some studies also showed that telephone consultations may cause several challenges, such as delay in diagnosis [27] and limiting physician-patient interactions [27]. In addition, it can be challenging for patients with language or hearing impairments to use this technology effectively [42].
Clinical outcomes
In addition to the non-clinical benefits of telemedicine technology, several studies have demonstrated that patients who received care through this technology experienced positive clinical outcomes, such as reduction in anxiety [24, 27, 29, 38], pain [21, 23], sleep disorders [21, 23], fatigue [23], and uncontrolled appetite [21, 23] compared to those who had in-person visits. For instance, Chen et al. found that telerehabilitation was associated with reduced difficulty swallowing saliva, asphyxia, and cough among patients with head and neck cancers [21]. Other positive clinical outcomes of telemedicine over in-person consultations included reducing hospitalization and emergency care visits [33, 36, 46], reducing mortality rates [29], and improving treatment outcomes [42] for patients undergoing systemic anti-cancer treatments. Additionally, telemedicine can lead to faster biopsy consultation and diagnosis processes compared to the in-person visits [47].
Synthesis
Overall, the synthesis of the results showed that telemedicine was widely used for cancer patents during the Covid-19 pandemic. Like other chronic diseases, teleconsultation and televisit were the most common methods for delivering healthcare services. Although patients and healthcare providers were generally satisfied with this technology, a number of technical and non-technical challenges are still remaining which need further attention.
Discussion
During the Covid-19 pandemic, telemedicine was identified as a valuable intervention to facilitate the provision of care services for cancer patients [17]. This study aimed to investigate the use of telemedicine technology for cancer patients during the Covid-19 pandemic. The results revealed that video conferencing, telephone consultation, messaging applications, such as WeChat, and telemonitoring were commonly used technologies. Popular platforms included Zoom, Jeff Connect, Microsoft Teams, WeChat, and My Chart. Teleconsultation, televisit, and telerehabilitation were among the most frequently offered services. Overall, both healthcare providers and patients were highly satisfied with the telemedicine technology. The benefits of telemedicine included eliminating unnecessary travel time and costs, facilitating access to medical services, and reducing the risk of exposure to Covid-19. However, potential challenges such as limited access to, or proficiency with the communication tools or equipment, lack of technical skills, low level of e-literacy, and concerns over quality assurance are still remaining. Additionally, the findings suggested that using telemedicine helped to reduce anxiety levels, pain, sleep disorders, fatigue, and uncontrolled appetite while decreasing emergency care needs in many cases.
Several studies have demonstrated that video conferencing is an effective method for delivering virtual face-to-face consultations to the cancer patients during the Covid-19 pandemic [17, 49]. This technology has been used to facilitate screening, counseling, rehabilitation, mental health support [16], while improving clinical outcomes [50]. Additionally, video conferencing can help to reduce travel time and costs. However, some potential challenges, such as poor Internet connectivity, concerns over privacy and security, and limitations in conducting physical examinations or remote diagnostic tests still need further attentions [51]. Fortunately, the use of popular platforms such as WhatsApp, Zoom, and Skype has helped with conducting video conferencing sessions between healthcare providers and patients [52].
Several studies have indicated that telephone counseling can be an effective tool in providing palliative care for cancer patients [53] and can assist with providing mental health support to manage their anxiety and stress associated with the treatments [54]. Furthermore, with the increasing use of smartphones, messaging applications like WhatsApp, Viber, and WeChat [55] have been used to provide palliative support and rehabilitation services to cancer patients, leading to better management of clinical symptoms [56]. In addition, the use of these platforms has increased awareness among cancer patients regarding the treatment options during Covid-19 [56], and improved their functional capacity, psychological well-being, and overall quality of life [57].
Our study findings are consistent with other studies in which teleconsultation has been identified as one of the most commonly used telemedicine services for cancer patients during the Covid-19 pandemic [17]. Teleconsultation has proven to be an efficient and effective tool for receiving medical care, and timely palliative and emotional counseling outside of the hospital settings [58]. Similarly, televisit services have been used to maintain ongoing care delivery and support cancer patients during the pandemic. These virtual visits offered a valuable alternative for urgent medical care needs when in-person consultations were not feasible due to the social restrictions [59, 60] In addition, telerehabilitation services have demonstrated benefits in improving muscle strength, functional ability, pain relief, and reducing sleep disorders among cancer patients undergoing surgery or chemotherapy during the pandemic [61, 62]. Telemonitoring was also found to be effective in tracking the vital signs of cancer patients and providing feedback on rehabilitation progress during the pandemic [21, 63]. This finding is supported by Steimer et al.‘s study which showed that telemonitoring improved clinical outcomes and vital signs, and reduced hospitalization rates compared to the in-person visits among cancer patients [64].
Our research findings demonstrated that telemedicine services have also increased patients’ and healthcare providers’ satisfaction mainly due to maintaining quality of care and positive clinical outcomes compared to the in-person visits [60, 65, 66]. This positive feedback can help to accelerate development and implementation of telemedicine technology for cancer patients [67]. Although the effectiveness of telemedicine may vary depending on various factors, such as patient characteristics, type of cancer and its stage [14, 68], patients still use this type of services for various reasons, including reduced waiting times/costs [69], ease of accessibility/use, reduction in physician visits, improved treatment follow-up, and increased comfort levels [70]. Apart from their positive feedback, their concerns need to be addressed, too. It is crucially important to address infrastructure deficiencies and resolve technical issues, and reimbursement challenges for encouraging continuous use of telemedicine services [71, 72].
Implications for practice
This research provided an insight into the use telemedicine for cancer care during the Covid-19 pandemic. According to the findings, it is essential to customize telemedicine platforms to address users’ concerns regarding the quality of audio and video materials, as well as the ease of communication. Adapting services to meet the specific needs of patients at various stages of cancer care improves their overall satisfaction. Moreover, it is crucial to address technical obstacles, such as the Internet connectivity issues, in order to achieve a smooth telemedicine experience. Promoting patient engagement through effective communications, improving patient-physician interactions, and paying more attention to the positive clinical outcomes, such as decreased anxiety and pain, are necessary to encourage patients and their healthcare providers to use telemedicine services more effectively, despite ongoing challenges posed by the pandemic.
The experiences obtained during the Covid-19 pandemic can also contribute to plan for the future and better use of the telemedicine technology. In fact, by leveraging the recent literature, evidence-based findings, and best practices in telemedicine implementation, this technology can be adopted more effectively and broadly in cancer care in the post-Covid era, as its weaknesses have been previously identified and now, they need to be addressed properly. Furthermore, as patients and healthcare providers are relatively ready to accept the technology, team working and establishing interdisciplinary collaborations among oncologists, information technology experts, and policymakers can help to develop new implementation strategies tailored to the specific needs of cancer patients to promote the adoption of telemedicine technology.
Strengths and limitations of the study
This scoping review enhanced our understanding about using telemedicine for cancer care during the Covid-19 pandemic through a thorough examination of different technologies, their applications, and outcomes. Presenting users’ perspectives and experiences with telemedicine technology, challenges and clinical outcomes compared with the results of the in-person visits were other strengths of this study which can make a substantial contribution to the ongoing endeavors aimed at enhancing and promoting the consistent utilization of telemedicine services in cancer treatment.
However, this study had some limitations, including the restriction of articles to the English language. In fact, due to time and resource constraints, publications in other languages were not included. Moreover, this research solely focused on the interventional studies that analyzed the outcome of telemedicine technology and compared the results with the in-person visits. Therefore, other types of the research studies were excluded from the current study. Future studies can broaden their scope by incorporating various types of studies and objectives into their design to gain an in-depth understanding of the use of telemedicine for different groups of patients and healthcare providers.
In contrast to systematic reviews, the scoping review did not formally evaluate the methodological quality or risk of bias of the included studies. This constraint directly results from the fundamental nature of scoping reviews, which primarily focus on mapping the existing evidence rather than critically evaluating individual studies. Nevertheless, future studies could incorporate quality assessment methods to enhance the credibility of the results by conducting systematic reviews.
Conclusion
This study aimed to investigate the use of telemedicine technology for cancer patients during the Covid-19 pandemic. The research findings provided a valuable insight into the use of various telemedicine technologies, services, and users’ opinions about, and clinical outcomes of these services. The results showed that in most studies positive outcomes in terms of patients’ and providers’ satisfaction and clinical aspects were reported after using telemedicine interventions. This shows that overall, the context is ready to accept the technology and there are a number of opportunities for expanding the use of telemedicine technology, particularly for cancer patients. Therefore, future research should focus on identifying optimal strategies for implementing telemedicine for cancer care while taking into account both the clinical and non-clinical effectiveness of various services and technologies.
Data availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- IARC:
-
International Agency for Research on Cancer
- PRISMA ScR:
-
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews
References
Fidler MM, Bray F, Soerjomataram I. The global cancer burden and human development: a review. Scand J Public Health. 2018;46(1):27–36.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Albert T. Latest global cancer data: Cancer burden rises to 18.1 million new cases and 9.6 million cancer deaths. International Agency for Research on Cancer; 2018 Sep. p. 3.
Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–7.
Giannakoulis VG, Papoutsi E, Siempos II. Effect of cancer on clinical outcomes of patients with Covid-19: a meta-analysis of patient data. JCO Glob Oncol. 2020;6(2020):799–808.
Hennessy MA, Linehan A, Cowzer D, Coyne ZL, Fitzpatrick O, Barrett F, et al. Chemotherapy in the Covid-19 era: the patient’s perception. Ir J Med Sci. 2021;190(4):1303–8.
Karacin C, Acar R, Bal O, Eren T, Sendur MAN, Acikgoz Y, et al. Swords and Shields against Covid-19 for patients with cancer at clean and pandemic hospitals: are we ready for the second wave? Support Care Cancer. 2021;29(8):4587–93.
Baig AHB, Jenkins P, Lamarre E, McCarthy B. The Covid-19 recovery will be digital: A plan for the first 90 days.[Internet] 2020 [cited 02 June 2023]. https://www.mckinsey.com/capabilities/mckinsey-digital/our-insights/the-Covid-19-recovery-will-be-digital-a-plan-for-the-first-90-days.
Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–81.
Sirintrapun SJ, Lopez AM. Telemedicine in cancer care. Am Soc Clin Oncol Educ Book. 2018;38:540–5.
Bakouny Z, Hawley JE, Choueiri TK, Peters S, Rini BI, Warner JL, et al. Covid-19 and cancer: current challenges and perspectives. Cancer Cell. 2020;38(5):629–46.
Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (Covid-19) pandemic: an international collaborative group. Oncologist. 2020;25(6):e936–45.
Jiang CY, El-Kouri NT, Elliot D, Shields J, Caram MEV, Frankel TL, et al. Telehealth for cancer care in veterans: opportunities and challenges revealed by Covid. JCO Oncol Pract. 2020;17(1):22–9.
Shirke MM, Shaikh SA, Harky A. Implications of telemedicine in oncology during the Covid-19 pandemic. Acta Biomed. 2020;91(3):e2020022.
Bitar H, Alismail S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during Covid-19 pandemic: a rapid systematic review. Digit Health. 2021;7:20552076211009396.
McGrowder DA, Miller FG, Vaz K, Anderson Cross M, Anderson-Jackson L, Bryan S, et al. The utilization and benefits of telehealth services by health care professionals managing breast cancer patients during the Covid-19 pandemic. Healthcare. 2021;9(10):1401.
Garfan S, Alamoodi AH, Zaidan BB, Al-Zobbi M, Hamid RA, Alwan JK, et al. Telehealth utilization during the Covid-19 pandemic: a systematic review. Comput Biol Med. 2021;138:104878.
Doraiswamy S, Abraham A, Mamtani R, Cheema S. Use of Telehealth during the Covid-19 pandemic: scoping review. J Med Internet Res. 2020;22(12):e24087.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Darcourt JG, Aparicio K, Dorsey PM, Ensor JE, Zsigmond EM, Wong ST, et al. Analysis of the implementation of telehealth visits for care of patients with cancer in Houston during the Covid-19 pandemic. JCO Oncol Pract. 2021;17(1):e36–43.
Chen K, Yao F, Chen X, Lin Y, Kang M. Effectiveness of telerehabilitation on short-term quality of life of patients after esophageal cancer surgery during Covid-19: a single-center, randomized, controlled study. J Gastrointest Oncol. 2021;12(4):1255–64.
Shaverdian N, Gillespie EF, Cha E, Kim SY, Benvengo S, Chino F, et al. Impact of telemedicine on patient satisfaction and perceptions of care quality in radiation oncology. J Natl Compr Canc Netw. 2021;19(10):1174–80.
Narayanan S, Lopez G, Powers-James C, Fellman BM, Chunduru A, Li Y, et al. Integrative oncology consultations delivered via telehealth in 2020 and in-person in 2019: paradigm shift during the Covid-19 world pandemic. Integr Cancer Ther. 2021;20:1–8.
Granberg RE, Heyer A, Rising KL, Handley NR, Gentsch AT, Binder AF. Medical oncology patient perceptions of telehealth video visits. JCO Oncol Pract. 2021;17(9):e1333–43.
Heyer A, Granberg RE, Rising KL, Binder AF, Gentsch AT, Handley NR. Medical oncology professionals’ perceptions of telehealth video visits. JAMA Netw Open. 2021;4(1):e2033967.
Picardo E, Bau MG, Anatrone C, Mondino A, Surace A, Gallo F, et al. Oncophone20 study: patients’ perception of telemedicine in the Covid-19 pandemic during follow-up visits for gynecological and breast cancers. Int J Gynaecol Obstet. 2021;155(3):398–403.
Zhu Y, Chen Z, Ding A, Walter H, Easto R, Wilde A. Patient satisfaction with the head and neck cancer telephone triage service during the Covid-19 pandemic. Cureus. 2021;13(9):e18375.
Kotsen C, Dilip D, Carter-Harris L, O’Brien M, Whitlock CW, de Leon-Sanchez S, et al. Rapid scaling up of telehealth treatment for tobacco-dependent cancer patients during the Covid-19 outbreak in New York City. Telemed J E Health. 2021;27(1):20–9.
Watson N, Cox A, Sanmugarajah J, Dzienis M, Hughes I. Safety and efficacy of telephone clinics during the Covid-19 pandemic in the provision of care for patients with cancer. Intern Med J. 2021;51(9):1414–9.
Aghedo BO, Svoboda S, Holmes L, Man L, Wu Y, Linder J, et al. Telehealth adaptation for multidisciplinary colorectal cancer clinic during the Covid-19 pandemic. Cureus. 2021;13(9):e17848.
Fassas S, Cummings E, Sykes KJ, Bur AM, Shnayder Y, Kakarala K. Telemedicine for head and neck cancer surveillance in the Covid-19 era: promise and pitfalls. Head Neck. 2021;43(6):1872–80.
Uppal A, Kothari AN, Scally CP, Roland CL, Bednarski BK, Katz MHG, et al. Adoption of telemedicine for postoperative follow-up after inpatient cancer-related surgery. JCO Oncol Pract. 2022;18(7):e1091–9.
Mackwood M, Butcher R, Vaclavik D, Alford-Teaster JA, Curtis KM, Lowry M, et al. Adoption of telemedicine in a rural us cancer center amid the Covid-19 pandemic: qualitative study. JMIR Cancer. 2022;8(3):e33768.
Alpert JM, Taylor G, Hampton CN, Paige S, Markham MJ, Bylund CL. Clinicians’ perceptions of the benefits and challenges of teleoncology as experienced through the Covid-19 pandemic: qualitative study. JMIR Cancer. 2022;8(1):e34895.
Handley NR, Heyer A, Granberg RE, Binder AF, Gentsch AT, Csik VP, et al. Covid-19 pandemic influence on medical oncology provider perceptions of telehealth video visits. JCO Oncol Pract. 2022;18(4):e610–9.
Waseem N, Boulanger M, Yanek LR, Feliciano JL. Disparities in telemedicine success and their association with adverse outcomes in patients with thoracic cancer during the Covid-19 pandemic. JAMA Netw Open. 2022;5(7):e2220543.
Brady G, Ashforth K, Cowan-Dickie S, Dewhurst S, Harris N, Monteiro A, et al. An evaluation of the provision of oncology rehabilitation services via telemedicine using a participatory design approach. Support Care Cancer. 2022;30(2):1655–62.
Khan MM, Manduchi B, Rodriguez V, Fitch MI, Barbon CEA, McMillan H, et al. Exploring patient experiences with a telehealth approach for the PRO-ACTIVE trial intervention in head and neck cancer patients. Supporti Care Cancer. 2022;30(S1):1–207.
Breen KE, Tuman M, Bertelsen CE, Sheehan M, Wylie D, Fleischut MH, et al. Factors influencing patient preferences for telehealth cancer genetic counseling during the Covid-19 pandemic. JCO Oncol Pract. 2022;18(4):e462–71.
Mackwood MB, Tosteson TD, Alford-Teaster JA, Curtis KM, Lowry ML, Snide JA, et al. Factors influencing telemedicine use at a northern New England cancer center during the Covid-19 pandemic. JCO Oncol Pract. 2022;18(7):e1141–53.
Turner K, Bobonis Babilonia M, Naso C, Nguyen O, Gonzalez BD, Oswald LB, et al. Health care providers’ and professionals’ experiences with telehealth oncology implementation during the Covid-19 pandemic: a qualitative study. J Med Internet Res. 2022;24(1):e29635.
Grant M, Hockings H, Lapuente M, Adeniran P, Saud RA, Sivajothi A, et al. Learning from crisis: a multicentre study of oncology telemedicine clinics introduced during Covid-19. J Cancer Educ. 2022;37(6):1861–9.
Ackroyd SA, Walls M, Kim JS, Lee NK. Lessons learned: Telemedicine patterns and clinical application in patients with gynecologic cancers during Covid-19. Gynecol Oncol Rep. 2022;41:100986.
Mojdehbakhsh RP, Mora Hurtado AC, Uppal S, Milakovich H, Spencer RJ. The long game: Telemedicine patient satisfaction metrics and methods of recurrence detection for gynecologic cancer patients throughout the initial year of the Covid-19 pandemic. Gynecol Oncol Rep. 2022;42:101037.
Collins A, McLachlan SA, Pasanen L, Wawryk O, Philip J. Perceptions of telehealth in real-world oncological care: an exploration of matched patient- and clinician-reported acceptability data from an Australian cancer centre. Cancer Med. 2022;11(17):3342–51.
Almouaalamy NA, Jafari AA, Althubaiti AM. Tele-clinics in palliative care during the Covid-19 outbreak: tertiary care cancer center experience. Saudi Med J. 2022;43(4):394–400.
Tang A, Neeman E, Kuehner GE, Savitz AC, Mentakis M, Vuong B, et al. Telehealth for preoperative evaluation of patients with breast cancer during the Covid-19 pandemic. Perm J. 2022;26(2):54–63.
Pardolesi A, Gherzi L, Pastorino U. Telemedicine for management of patients with lung cancer during Covid-19 in an Italian cancer institute: SmartDoc Project. Tumori. 2022;108(4):357–63.
ElKefi S, Asan O. How technology impacts communication between cancer patients and their health care providers: a systematic literature review. Int J Med Inf. 2021;149:104430.
Paleri V, Hardman J, Tikka T, Bradley P, Pracy P, Kerawala C. Rapid implementation of an evidence-based remote triaging system for assessment of suspected referrals and patients with head and neck cancer on follow-up after treatment during the Covid-19 pandemic: Model for international collaboration. Head Neck. 2020;42(7):1674–80.
Lidia SH, Pieter UD, van der Sjoukje W, Kees A, Jan LNR. Benefits and drawbacks of videoconferencing for collaborating multidisciplinary teams in regional oncology networks: a scoping review. BMJ Open. 2021;11(12):e050139.
Eslami Jahromi M, Ayatollahi H. Utilization of telehealth to manage the Covid-19 pandemic in low- and middle-income countries: a scoping review. J Am Med Inf Assoc. 2022;30(4):738–51.
Grewal US, Terauchi S, Beg MS. Telehealth and palliative care for patients with cancer: implications of the Covid-19 pandemic. JMIR Cancer. 2020;6(2):e20288.
Rainwater L, Lichiello S, Duckworth K, Tolbert A, Moskop R, McQuellon R. Psychosocial oncology care during a pandemic: Effect of offering telemental health in an academic medical center. Psychooncology. 2021;30(S1):181.
Ganapathy S, de Korne DF, Chong NK, Car J. The role of text messaging and telehealth messaging apps. Pediatr Clin. 2020;67(4):613–21.
Biswas S, Adhikari SD, Gupta N, Garg R, Bharti SJ, Kumar V, et al. Smartphone-based telemedicine service at palliative care unit during nationwide lockdown: our initial experience at a tertiary care cancer hospital. Indian J Palliat Care. 2020;26(Suppl 1):S31–5.
Omidi Z, Kheirkhah M, Abolghasemi J, Haghighat S. Effect of lymphedema self-management group-based education compared with social network-based education on quality of life and fear of cancer recurrence in women with breast cancer: a randomized controlled clinical trial. Qual Life Res. 2020;29(7):1789–800.
Marzorati C, Renzi C, Russell-Edu SW, Pravettoni G. Telemedicine use among caregivers of cancer patients: systematic review. J Med Internet Res. 2018;20(6):e223.
Choi Y, Parrillo E, Wenzel J, Grabinski VF, Kabani A, Peairs KS. Optimizing cancer survivorship in primary care: patient experiences from the Johns Hopkins primary care for cancer survivors clinic. J Cancer Surviv. 2022;13:1–9.
Read Paul L, Salmon C, Sinnarajah A, Spice R. Web-based videoconferencing for rural palliative care consultation with elderly patients at home. Support Care Cancer. 2019;27(9):3321–30.
Munce S, Andreoli A, Bayley M, Guo M, Inness EL, Kua A, et al. Clinicians’ experiences of implementing a telerehabilitation toolkit during the Covid-19 pandemic: qualitative descriptive study. JMIR Rehabil Assist Technol. 2023;10:e44591.
Ogourtsova T, Boychuck Z, O’Donnell M, Ahmed S, Osman G, Majnemer A. Telerehabilitation for children and youth with developmental disabilities and their families: a systematic review. Phys Occup Ther Pediatr. 2023;43(2):129–75.
Coats V, Moffet H, Vincent C, Simard S, Tremblay L, Maltais F, et al. Feasibility of an eight-week telerehabilitation intervention for patients with unresectable thoracic neoplasia receiving chemotherapy: a pilot study. Can J Respir Crit Care Sleep Med. 2020;4(1):14–24.
Steimer M, Leabo J, Wang H, Heyer D, Addison N, Bowles N, et al. Remote home monitoring of patients with cancer during the Covid pandemic: a pilot study. JCO Oncol Pract. 2021;17(9):e1286–92.
Smith SJ, Smith AB, Kennett W, Vinod SK. Exploring cancer patients’, caregivers’, and clinicians’ utilisation and experiences of telehealth services during Covid-19: a qualitative study. Patient Educ Couns. 2022;105(10):3134–42.
Gondal H, Abbas T, Choquette H, Le D, Chalchal HI, Iqbal N, et al. Patient and pysician satisfaction with telemedicine in cancer care in saskatchewan: a cross-sectional study. Curr Oncol. 2022;29(6):3870–80.
Maroongroge S, Smith B, Bloom ES, Ning MS, Wang C, Das P, et al. Telemedicine for radiation oncology in a post-covid world. Int J Radiat Oncol Biol Phys. 2020;108(2):407–10.
Morrison KS, Paterson C, Toohey K. The feasibility of exercise interventions delivered via telehealth for people affected by cancer: a rapid review of the literature. Semin Oncol Nurs. 2020;36(6):151092.
Paterson C, Bacon R, Dwyer R, Morrison KS, Toohey K, O’Dea A, et al. The role of telehealth during the Covid-19 pandemic across the interdisciplinary cancer team: implications for practice. Semin Oncol Nurs. 2020;36(6):151090.
Pogorzelska K, Chlabicz S. Patient satisfaction with telemedicine during the Covid-19 pandemic:a systematic review. Int J Environ Res Public Health. 2022;19(10):6113.
Ftouni R, AlJardali B, Hamdanieh M, Ftouni L, Salem N. Challenges of telemedicine during the Covid-19 pandemic: a systematic review. BMC Med Inf Decis Mak. 2022;22(1):207.
Tang M, Reddy A. Telemedicine and its past, present, and future roles in providing palliative care to advanced cancer patients. Cancers (Basel). 2022;14(8):1884.
Acknowledgements
This research was supported by the Health Management and Economics Research Center, Health Management Research Institute, Iran University of Medical Sciences, Tehran, Iran.
Funding
This research was funded by the Health Management and Economics Research Center, Health Management Research Institute, Iran University of Medical Sciences, Tehran, Iran (1401-1-113-23183). The funding body played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
ET designed and conducted the study. He also prepared the first draft and revisions of the manuscript. HA helped with conceptualizing the research, conducting the study, and finalizing the manuscript. Both authors approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations in the Declaration of Helsinki. Also, this study was reviewed and approved by the National Ethics Committee of Biomedical Research (IR.IUMS.REC.1401.392). No human participant was involved in this research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Toni, E., Ayatollahi, H. An insight into the use of telemedicine technology for cancer patients during the Covid-19 pandemic: a scoping review. BMC Med Inform Decis Mak 24, 104 (2024). https://doi.org/10.1186/s12911-024-02507-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-024-02507-1