Abstract
Background
Infective endocarditis (IE) is a disease with high in-hospital mortality. The objective of the present investigation was to develop and validate a nomogram that precisely anticipates in-hospital mortality in ICU individuals diagnosed with infective endocarditis.
Methods
Retrospectively collected clinical data of patients with IE admitted to the ICU in the MIMIC IV database were analyzed using the Least Absolute Shrinkage and Selection Operator (LASSO) regression to identify potential hazards. A logistic regression model incorporating multiple factors was established, and a dynamic nomogram was generated to facilitate predictions. To assess the classification performance of the model, an ROC curve was generated, and the AUC value was computed as an indicator of its diagnostic accuracy. The model was subjected to calibration curve analysis and the Hosmer–Lemeshow (HL) test to assess its goodness of fit. To evaluate the clinical relevance of the model, decision-curve analysis (DCA) was conducted.
Results
The research involved a total of 676 patients, who were divided into two cohorts: a training cohort comprising 473 patients and a validation cohort comprising 203 patients. The allocation ratio between the two cohorts was 7:3. Based on the independent predictors identified through LASSO regression, the final selection for constructing the prediction model included five variables: lactate, bicarbonate, white blood cell count (WBC), platelet count, and prothrombin time (PT). The nomogram model demonstrated a robust diagnostic ability in both the cohorts used for training and validation. This is supported by the respective area under the curve (AUC) values of 0.843 and 0.891. The results of the calibration curves and HL tests exhibited acceptable conformity between observed and predicted outcomes. According to the DCA analysis, the nomogram model demonstrated a notable overall clinical advantage compared to the APSIII and SAPSII scoring systems.
Conclusions
The nomogram developed during the study proved to be highly accurate in forecasting the mortality of patients with IE during hospitalization in the ICU. As a result, it may be useful for clinicians in decision-making and treatment.
Similar content being viewed by others
Background
Infective endocarditis (IE) is a disease in which pathogenic microorganisms such as bacteria or fungi attach to the endocardial tissue of the heart, causing inflammation and damage to the endocardium or valve tissue. The incidence of IE is 3–10 per 100,000 people, with an increasing trend in some places [1, 2]. In spite of various diagnostic tools and therapeutic measures such as antibiotics and surgery being developed, the in-hospital mortality rate due to IE remains at approximately 20% [3,4,5]. Individual patient characteristics, along with cardiac and non-cardiac comorbidities, the infecting microbial species and the echocardiographic disease status are the primary factors contributing to the poor prognosis of IE [6]. Early diagnosis is now recognized as critical to improving patient outcomes and reducing mortality associated with IE [7].
Due to the complex and unpredictable clinical characteristics and disease progression of IE, timely and accurate diagnosis is imperative to ensure that patients receive appropriate treatment during critical stages of the disease. However, there is currently limited evidence regarding the effective intensive care management of IE, including specific clinical features that are indicative of a poor prognosis, as well as predictive tools that are effective in identifying high-risk patients [8].
A nomogram is a common statistical tool used in medicine to predict the probability or risk of a certain outcome based on multiple patient factors. This tool is especially useful in clinical predictive modeling, as it visualizes the impact of each predictor on the outcome event. Clinicians can use this tool to make prognostic predictions more accurately [9, 10]. The objective of this study was to construct a nomogram utilizing data sourced from the public database MIMIC-IV, subsequently assessing its prognostic value in predicting the risk of in-hospital mortality among patients with IE who were admitted to the ICU.
Data and method
Data source
The information utilized in this research endeavor was sourced from MIMIC-IV 2.0, a publicly available archival system for extensive care medicinal data, which was established by the Massachusetts Institute of Technology (Cambridge, MA). The database containing hospitalization data for patients treated at Beth Israel Deaconess Medical Center (Boston, MA) between 2008 and 2019 exists as a comprehensive collection of patient information, and includes vital signs, laboratory test results, organ failure score, disease severity score, comorbidities, diagnosis, treatment, length of hospital stay, survival data and demographic information. The database contains patient information that has been de-identified, and informed consent from patients is not necessary. The authors of this study have completed the requisite training and certification to access the database.
Study population
From the MIMIC-IV database, a cohort of 925 patients diagnosed with IE and admitted to the Intensive Care Unit (ICU) was identified. Among them, 237 cases with repeated ICU admissions in a single hospitalization were excluded from the analysis. Patients over 90 years of age, those without basic laboratory test results, and individuals with hospitalization times exceeding 100 days were also excluded from the study. The final analysis consisted of 676 patients deemed eligible according to the pre-determined criteria (Fig. 1).
Clinical variables
The raw data of the 676 selected patients was extracted using Structured Query Language (SQL) and PostgreSQL tools (version 9.6) through Navicat Premium software, based on their unique HADM_ID and ICUSTAY_ID. The extracted raw data comprised demographic characteristics (age, gender, race and weight), vital signs (heart rate, blood pressure, and temperature), blood gas analysis (lactate, SpO2, SpCO2 and anions gap), laboratory tests (e.g., white blood cells [WBC] and red blood cells [RBC] counts, hemoglobin, prothrombin time [PT], calcium, bicarbonate, glucose, lymphocytes), comorbidities (e.g., atrial fibrillation, myocardial infarction, chronic lung disease, heart valve disease, cerebrovascular disease), score systems (Acute Physiology Score III [APSIII], Simplified Acute Physiology Score II [SAPSII] and Sequential Organ Failure Score [SOFA]), clinical risk factors associated with IE (continuous renal replacement therapy [CRRT], blood culture results, the presence of embolism, history of prior cardiac surgery).
Statistical analysis
Indexes with a missing degree above 20% were excluded from this study, and remaining missing data were imputed using R packages “lattice (0.21-8)” and “mice (3.16.0)” for multiple imputation. A random allocation of participants into the training and validation cohorts was accomplished in a ratio of 7:3. More specifically, 70% of the study’s subjects were assigned to the training cohort, and the remaining 30% were allocated to the validation cohort to test the data. The median and interquartile range were used to express continuous variables, and the Wilcoxon rank-sum test was employed to compare two groups. Proportions were utilized to represent categorical variables, and the comparison between groups was analyzed by either the Chi-square test or Fisher’s exact test, depending on the context of the comparison. The methodology employed adheres to academic standards in statistical analysis. The variables in the training cohort were screened for mortality predictors using the Least Absolute Shrinkage and Selection Operator (LASSO) approach. The variable set for the logistic regression models was determined through the selection of lambda.1se using cross-validation [11, 12]. Subsequently, utilizing the selected set of variables, we constructed multiple logistic regression models, and nomograms were created using the ‘regplot (1.1)’ R package. The nomogram was validated using data from the validation cohort. The evaluation of the model’s performance was conducted by computing the area under the receiver operating characteristic (ROC) curve, commonly referred to as AUC. Additionally, we compared the AUC of our model with the APSIII and SAPSII scoring systems to evaluate its efficacy.
The utilization of the calibration curve aimed to evaluate discrepancies between the expected outcomes of the model and the factual observed measurements. The assessment was conducted to ensure the accuracy of the model’s predictions in an empirical manner. The Hosmer-Lemeshow goodness-of-fit test (HL test) was employed to determine whether the model’s estimation of the observed probability was consistent with the actual probability. The Integrated Discrimination Improvement (IDI) method was utilized to evaluate the overall improvement in the accuracy of predictions. Furthermore, to establish the clinical validity of the model, a Decision Curve Analysis (DCA) approach was employed. The statistical analyses were performed utilizing the R language (4.3.0), while the level of significance was established at a p-value of less than 0.05.
Results
Patient characteristics
The eligibility criteria were met by a cohort of 676 patients diagnosed with IE, who were subsequently divided into two cohorts, namely the training cohort (n = 473) and the validation cohort (n = 203), through a random sampling process. Table 1 provides a comprehensive overview of the demographic and clinical features of the respective cohorts. In the training cohort, the median age was 58 years (43, 68), and the sample consisted of 310 (65.54%) male and 163 (34.46%) female patients. The validation cohort had a median age of 57 years (40, 66), with 132 (65.02%) male and 71 (34.98%) female participants. The majority of patients in both groups were white (> 67%). In the training cohort, the median weight of the patients was 77.3 kg (67.5,92.0). While in the validation cohort, the patients had a median weight of 77.9 kg (66.2, 94.2). Apart from the prevalence of liver disease (p = 0.044) (Supplementary materials), baseline clinicopathological data did not significantly differ between the cohorts (p = 0.077-1).
Variable analysis and selection
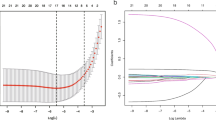
During the cross-validation process of the LASSO regression, we used the mean square error (MSE) as the evaluation index to successfully screen seven significant independent variables from the initial pool of 54. We selected Lambda.1se and found that the coefficients of these variables were not equal to zero, indicating their significant contribution to the model’s prediction results (Fig. 2). In the multivariate logistic regression analysis, seven variables were incorporated and evaluated: lactate (OR: 1.182; 95% CI 1.084–1.297), bicarbonate (OR: 0.913; 95% CI 0.847–0.984), white blood cells (OR: 1.213; 95% CI 1.126–1.317), platelet (OR: 0.996; 95% CI 0.993–0.997), PT (OR: 1.074; 95%CI 1.009–1.163), APSIII score (OR: 1.014; 95%CI 1–1.029), and SAPSII score (OR: 1.020; 95% CI 0.994–1.048) (Fig. 3).
Development of the nomogram
To mitigate the potential impact of multicollinearity on model accuracy, a new nomogram model was constructed by selecting the remaining five variables (Fig. 4), as the APSIII score and SAPSII score overlapped with other variables among the independent variables obtained through LASSO regression. Each factor in the nomogram was assigned an individual score based on its value, and the total score was calculated by summing these scores. The cumulative score derived from the aforementioned parameters was employed in forecasting the mortality of patients with IE during hospitalization in the ICU.
Nomogram for predicting the in-hospital mortality rate of patients with infective endocarditis. Each variable is represented by a vertical line drawn to its corresponding score. The scores for each variable are summed to obtain a total score, which corresponds to the predicted probability of in-hospital mortality rate at the bottom of the nomogram. WBC white blood cell; PT prothrombin time; *** means p < 0.001; * means p < 0.05
Evaluation of nomogram performance
Our nomogram model generated an AUC value of 0.843 (95% CI: 0.792–0.893) under the ROC curve for the training cohort, which is higher than both APSIII (0.764; 95% CI: 0.711–0.817) and SAPSII (0.764; 95% CI: 0.712–0.816). In the validation cohort, the AUC value is also 0.891(95% CI: 0.837–0.946), which is higher than APSIII (0.782; 95% CI: 0.698–0.867) and SAPSII (0.706; 95% CI: 0.617–0.796) (Fig. 5). With a Delong’s test, we have proven that the difference in AUC between our nomogram model and the APSIII and SAPSII scoring systems is statistically significant (Table 2). And calculating the IDI value demonstrates that our model outperforms the two scoring systems, indicating that our nomogram’s graphical model exhibits superior classification accuracy compared to the commonly used APSIII and SAPSII scores (Table 3). In the training and validation sets, the calibration curve closely approximates the ideal curve (45-degree diagonal line). This indicates a strong correlation between the predicted and observed values, signifying a robust fit (Fig. 6). The HL test (subgroups = 10) yielded a χ2 of 13.97 (p = 0.12) for the training cohort and 3.68 (p = 0.93) for the validation cohort. Finally, the DCA curve indicates that our model has good clinical validity in predicting mortality, as it represents a net benefit (Fig. 7). The DCA curve for the validation cohort indicated a net clinical gain of 8.37% when the prediction probability threshold was set to 20%. These results suggest that our model is more successful in predicting in-hospital mortality caused by IE.
Calibration curves of the training cohort (A) and validation cohort (B) for the nomogram. The x-axis represents the nomogram-predicted probability, and the y-axis represents the actual probability of the nomogram. The diagonal line represents the perfect prediction of the ideal model. The dashed line represents the nonparametric calibration curve, the solid line represents the calibration curve of logistic regression
Discussion
The outcome of patients with IE is generally unfavorable, with a high mortality rate [13]. Thus, there is a pressing need for accurate prediction models to identify high-risk patients at an early stage. In this study, we successfully developed a nomogram model for the prediction of in-hospital mortality in IE patients admitted to the ICU, and assessed its effectiveness. Through the utilization of LASSO regression analysis on the data of MIMIC IV database, we identified several significant indicators, namely lactate, bicarbonate, white blood cell count (WBC), platelet count, prothrombin time (PT), APSIII score, and SAPSII score, that were associated with adverse outcomes in this particular patient cohort.
The APS score is a component of the Acute Physiology and Chronic Health Evaluation (APACHE) score. Within APS III, there are 17 physiological variables assessed, including temperature, mean arterial pressure, heart rate, respiratory rate, PaO2 or A-aDO2, pH or HCO3, Na+, K+, Cr, hematocrit, WBC, blood urea nitrogen, urine output, serum albumin, bilirubin, glucose, and Glasgow Coma Scale (GCS) score [14]. On the other hand, the SAPS II is a tool that incorporates age, admission type (planned surgery, unplanned surgery, or medical), underlying disease variables (acquired immune deficiency syndrome, metastatic cancer, and hematological malignancy), and 12 physiological variables (such as heart rate, systolic blood pressure) into its scoring system [15]. Both APS III and SAPS II scores are commonly used in assessing the risk of mortality in patients [16, 17]. However, due to the overlap of these scoring systems and other variables in this study, the APS III and SAPS II scores were excluded to maintain model accuracy.
Based on these findings, a nomogram prediction model was developed with the aim of providing clinicians with a practical tool to predict in-hospital mortality in patients with IE who are receiving intensive care. By employing this nomogram, physicians can gain a comprehensive understanding of the patient’s condition and identify individuals at high risk during the early stages, enabling the formulation of more personalized treatment plans. Additionally, nomograms can serve as initial assessment tools for patient admission, establish baseline data for patients, and provide references for subsequent treatment and care. To facilitate clinical use, we developed a dynamic nomogram based on this model and made it available on the website, enhancing the user-friendliness of the nomogram prediction model.
Our study found a correlation between lactate elevation and patient mortality. Elevated levels of lactate serve as a crucial prognostic indicator in the evaluation of patients [18], hyperlactatemia strongly associated with poorer prognosis [19]. The mechanisms by which hyperlactatemia occurs have been debated, but irrespective of these mechanisms, numerous studies have demonstrated lactate as a marker for disease severity [20], and there exists a positive correlation between lactate concentration, disease severity and mortality [21, 22]. Bicarbonate serves as a vital regulator of body fluids and acid-base homeostasis, supporting essential physiological processes. However, metabolic acidosis is often observed in patients admitted to Intensive Care Units (ICUs), leading to reduced levels of bicarbonate [23, 24]. Such alteration in bicarbonate levels has been linked to a higher incidence of adverse patient outcomes, including increased morbidity and mortality rates [25].
Coagulation is at the core of IE, with inflammation capable of disrupting the proper balance between the coagulation and immune systems [26]. This disruption leads to the generation of thrombin, which activates platelets and generates fibrin. Fibrin seals infected tissue to prevent further spread of bacteria [27], while platelets with immunoglobulin receptors and pattern receptors can also kill bacteria [28]. Research has revealed that the depletion of platelets can worsen outcomes in animal models of IE [29,30,31]. Additionally, thrombocytopenia, which is the reduction of platelet counts, is correlated with longer hospital stays, an increased incidence of major bleeding events, and higher in-hospital mortality rate among individuals with septic shock [32]. While platelets could contribute to bacterial adhesion to heart valves that result in vegetation, their involvement in clearing bacteria at a later stage may be more beneficial. The inflammatory response that accompanies IE can cause activated endothelial cells and leukocytes to release several tissue-active factors, which can activate the extrinsic coagulation pathway and prolong PT [26]. Patients with severe infections commonly exhibit elevated white blood cell counts (WBC), and the severity of their illness correlates with the degree of elevation of their WBC counts [33].
The study analyzed several known risk factors that could affect the prognosis of IE patients, such as CRRT, blood culture results, embolism symptoms and prior history of cardiac surgery [34], but none of these variables were incorporated into the model. This situation can be attributed to the requirement of producing a practical and reliable model. Therefore, Lambda.1se was utilized as the cut-off point for variable selection during LASSO regression to avoid overfitting the model with too many selected variables.
In clinical practice, several scoring systems, including ANCLA, PALSUSE, DeFeo, RISK-E and EndoSCORE have been employed to evaluate the prognosis of patients with IE [35,36,37,38,39], these scoring systems mainly focus on the postoperative prognosis of IE surgery patients. This approach is inadequate, as only approximately 51% of IE patients undergo surgical intervention, as shown in EURO-ENDO 2019 registry data [40]. Our study exhibits a significant advantage due to the comprehensive inclusion of data pertaining to all patients diagnosed with IE who were admitted to the ICU, as opposed to solely concentrating on those necessitating surgical intervention. In addition, the variables present in our model comprise of objective indicators widely utilized in routine clinical practice, hence facilitating the process of data acquisition.
Our study also has several limitations. First, echocardiographic findings could not be included in the analysis as the MIMIC IV 2.0 database did not have such imaging data. Second, the data was gathered solely from a single medical center, which may hinder the generalizability of the findings to a broader population. Moreover, we only performed internal validation of the model, indicating the need for further research involving external validation to consider other factors and improve the model’s validation.
Conclusions
We developed a practical nomogram model based on laboratory results, primarily comprising lactate, bicarbonate, WBC, platelet, PT. Our model demonstrates a precise estimation of in-hospital mortality among patients with IE within the ICU setting. The objective of the model is to assist physicians in making reasonable assessments and treatments, resulting in an improved survival rate of patients while hospitalized.
Data availability
The data were available on the MIMIC-IV website at https://mimic.physionet.org/, https://doi.org/10.13026/a3wn-hq05.
Abbreviations
- AF:
-
Atrial fibrillation
- AG:
-
Anion gap
- ALT:
-
Alanine transaminase
- APSIII:
-
Acute physiology score III
- AUC:
-
Area under the curve
- CRRT:
-
Continuous renal replacement therapy
- DBP:
-
Diastolic blood pressure
- HR:
-
Heart rate
- IDI:
-
Integrated Discrimination Improvement
- LASSO:
-
Least Absolute Shrinkage and Selection Operator
- LD:
-
Lactic dehydrogenase
- MBP:
-
Mean blood pressure
- MCH:
-
Mean corpuscular hemoglobin
- MIMIC IV:
-
Medical Information Mart for Intensive Care IV
- PT:
-
Prothrombin time
- PTT:
-
Partial thromboplastin time
- RBC:
-
Red blood cell
- SAPSII:
-
Simplified acute physiology score
- SBP:
-
Systolic blood pressure
- SOFA:
-
Sequential organ failure assessment
- WBC:
-
White blood cell
References
Cahill TJ, Prendergast BD. Infective endocarditis. Lancet. 2016;387(10021):882–93.
Chen H, Zhan Y, Zhang K, Gao Y, Chen L, Zhan J, Chen Z, Zeng Z. The global, regional, and national burden and trends of infective endocarditis from 1990 to 2019: results from the global burden of disease study 2019. Front Med (Lausanne). 2022;9:774224.
Duval X, Delahaye F, Alla F, Tattevin P, Obadia JF, Le Moing V, Doco-Lecompte T, Celard M, Poyart C, Strady C, et al. Temporal trends in infective endocarditis in the context of prophylaxis guideline modifications: three successive population-based surveys. J Am Coll Cardiol. 2012;59(22):1968–76.
Krajinovic V, Ivancic S, Gezman P, Barsic B. Association between cardiac surgery and mortality among patients with infective endocarditis complicated by sepsis and septic shock. Shock. 2018;49(5):536–42.
Habib G, Erba PA, Iung B, Donal E, Cosyns B, Laroche C, Popescu BA, Prendergast B, Tornos P, Sadeghpour A, et al. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J. 2019;40(39):3222–32.
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, et al. 2015 ESC guidelines for the management of infective endocarditis: the task force for the management of infective endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-thoracic surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075–128.
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Munoz D, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739–91.
Yang E, Frazee BW. Infective endocarditis. Emerg Med Clin North Am. 2018;36(4):645–63.
Park SY. Nomogram: an analogue tool to deliver digital knowledge. J Thorac Cardiov Sur. 2018;155(4).
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):E173–80.
Zhou J, Liu Y, Zhang Y, Li Q, Cao Y. Modeling tumor evolutionary dynamics to predict clinical outcomes for patients with metastatic colorectal cancer: a retrospective analysis. Cancer Res. 2020;80(3):591–601.
Wang S, Tu J. Nomogram to predict multidrug-resistant tuberculosis. Ann Clin Microbiol Antimicrob. 2020;19(1):27.
Pettersson GB, Coselli JS, Hussain ST, Griffin B, Blackstone EH, Gordon SM, LeMaire SA, Woc-Colburn LE, Infective AST, Comm W. 2016 the American Association for Thoracic Surgery (AATS) consensus guidelines: surgical treatment of infective endocarditis: executive summary. J Thorac Cardiov Sur. 2017;153(6):1241–U1581.
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–36.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
Glance LG, Osler TM, Dick AW. Identifying quality outliers in a large, multiple-institution database by using customized versions of the simplified acute physiology score II and the mortality probability model II. Crit Care Med. 2002;30(9):1995–2002.
Jentzer JC, van Diepen S, Murphree DH, Ismail AS, Keegan MT, Morrow DA, Barsness GW, Anavekar NS. Admission diagnosis and mortality risk prediction in a contemporary cardiac intensive care unit population. Am Heart J. 2020;224:57–64.
Hernandez G, Castro R, Romero C, de la Hoz C, Angulo D, Aranguiz I, Larrondo J, Bujes A, Bruhn A. Persistent sepsis-induced hypotension without hyperlactatemia: is it really septic shock? J Crit Care. 2011;26(4).
Jansen TC, van Bommel J, Mulder PG, Lima AP, van der Hoven B, Rommes JH, Snellen FTF, Bakker J. Prognostic value of blood lactate levels: does the clinical diagnosis at admission matter? J Trauma. 2009;66(2):377–85.
Hernandez G, Bellomo R, Bakker J. The ten pitfalls of lactate clearance in sepsis. Intensive Care Med. 2019;45(1):82–5.
Nichol A, Bailey M, Egi M, Pettila V, French C, Stachowski E, Reade MC, Cooper DJ, Bellomo R. Dynamic lactate indices as predictors of outcome in critically ill patients. Crit Care. 2011;15(5).
Haas SA, Lange T, Saugel B, Petzoldt M, Fuhrmann V, Metschke M, Kluge S. Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensive Care Med. 2016;42(2):202–10.
Kraut JA, Madias NE. Metabolic acidosis: pathophysiology, diagnosis and management. Nat Rev Nephrol. 2010;6(5):274–85.
Ellis MF. Use of bicarbonate in patients with metabolic acidosis. Crit Care Nurse. 2015;35(5):73–5.
Kraut JA, Madias NE. Treatment of acute metabolic acidosis: a pathophysiologic approach. Nat Rev Nephrol. 2012;8(10):589–601.
Liesenborghs L, Meyers S, Vanassche T, Verhamme P. Coagulation: at the heart of infective endocarditis. J Thromb Haemost. 2020;18(5):995–1008.
Papareddy P, Rydengard V, Pasupuleti M, Walse B, Morgelin M, Chalupka A, Malmsten M, Schmidtchen A. Proteolysis of human thrombin generates novel host defense peptides. PLoS Pathog. 2010;6(4):e1000857.
Liesenborghs L, Verhamme P, Vanassche T. Staphylococcus aureus, master manipulator of the human hemostatic system. J Thromb Haemost. 2018;16(3):441–54.
Sullam PM, Frank U, Yeaman MR, Tauber MG, Bayer AS, Chambers HF. Effect of thrombocytopenia on the early course of streptococcal endocarditis. J Infect Dis. 1993;168(4):910–4.
Dall L, Miller T, Herndon B, Diez I, Dew M. Platelet depletion and severity of streptococcal endocarditis. Can J Infect Dis. 1998;9(6):359–66.
Wuescher LM, Takashima A, Worth RG. A novel conditional platelet depletion mouse model reveals the importance of platelets in protection against staphylococcus aureus bacteremia. J Thromb Haemost. 2015;13(2):303–13.
Menard CE, Kumar A, Houston DS, Turgeon AF, Rimmer E, Houston BL, Doucette S, Zarychanski R. Evolution and impact of thrombocytopenia in septic shock: a retrospective cohort study. Crit Care Med. 2019;47(4):558–65.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr., Tleyjeh IM, Rybak MJ, Barsic B, Lockhart PB, Gewitz MH, Levison ME, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435–86.
Martinez-Selles M, Munoz P, Arnaiz A, Moreno M, Galvez J, Rodriguez-Roda J, de Alarcon A, Garcia Cabrera E, Farinas MC, Miro JM, et al. Valve surgery in active infective endocarditis: a simple score to predict in-hospital prognosis. Int J Cardiol. 2014;175(1):133–7.
De Feo M, Cotrufo M, Carozza A, De Santo LS, Amendolara F, Giordano S, Della Ratta EE, Nappi G, Della Corte A. The need for a specific risk prediction system in native valve infective endocarditis surgery. ScientificWorldJournal. 2012;2012:307571.
Olmos C, Vilacosta I, Habib G, Maroto L, Fernandez C, Lopez J, Sarria C, Salaun E, Di Stefano S, Carnero M, et al. Risk score for cardiac surgery in active left-sided infective endocarditis. Heart. 2017;103(18):1435–42.
Gatti G, Perrotti A, Obadia JF, Duval X, Iung B, Alla F, Chirouze C, Selton-Suty C, Hoen B, Sinagra G et al. Simple scoring system to predict in-hospital mortality after surgery for infective endocarditis. J Am Heart Assoc. 2017;6(7).
Gatti G, Benussi B, Gripshi F, Della Mattia A, Proclemer A, Cannata A, Dreas L, Luzzati R, Sinagra G, Pappalardo A. A risk factor analysis for in-hospital mortality after surgery for infective endocarditis and a proposal of a new predictive scoring system. Infection. 2017;45(4):413–23.
Habib G, Erba PA, Iung B, Donal E, Cosyns B, Laroche C, Popescu BA, Prendergast B, Tornos P, Sadeghpour A, et al. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J. 2019;40(39):3222–+.
Funding
This work was supported by the Fundamental Research Funds for Central Universities of Jinan University (No. 21622413).
Author information
Authors and Affiliations
Contributions
DC analyzed the data and wrote the paper; JH collected the data; JZ checked the integrity of the data; XZ and JL designed the study and revised the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The institutional review boards (IRB) of Beth Israel Deaconess Medical Center (BIDMC) and Massachusetts Institute of Technology (MIT) approved the project and consent was obtained for the original data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
The webpage prediction tool corresponding to the column chart we are studying is located at (https://cdyhaa.shinyapps.io/IENomapp/).
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Che, D., Hu, J., Zhu, J. et al. Development and validation of a nomogram for predicting in-hospital mortality in ICU patients with infective endocarditis. BMC Med Inform Decis Mak 24, 84 (2024). https://doi.org/10.1186/s12911-024-02482-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12911-024-02482-7