Abstract
Background
Patient care ownership (PCO) among medical students is a growing area in the field of medical education. While PCO has received increasing attention, there are no instruments to assess PCO in the context of Japanese undergraduate medical education. This study aimed to translate, culturally adapt, and validate the PCO Scale – Medical students (PCOS-S) in the Japanese context.
Methods
We collected survey data from fifth- and sixth-grade medical students from five different universities varying in location and type. Structural validity, convergent validity, and internal consistency reliability were examined.
Results
Data from 122 respondents were analyzed. Factor analysis of the Japanese PCOS-S revealed three factors with Cronbach’s alpha values exceeding the satisfactory criterion (0.70). A positive correlation was observed between the total Japanese PCOS-S scores and the global rating scores for the clinical department as a learning environment (Pearson’s correlation coefficient = 0.61).
Conclusions
We conducted the translation of the PCOS-S into Japanese and assessed its psychometric properties. The Japanese version has good reliability and validity. This instrument has potential value in assessing the development of medical students’ PCO.
Similar content being viewed by others
Background
Medical professionalism is an important competency for physicians and the cornerstone that underpins the quality medical education and clinical practice [1]. It articulates the core values of physicians and establishes the rules and norms that guide physicians’ behavior [2]. There is a consensus that national and international professional associations have recognized the importance of medical professionalism and defined a framework for its core elements [3, 4]. Therefore, it remains a powerful force in the medical education community.
Patient care ownership (PCO), affective-cognitive state in which physicians use emotional and intellectual skills to make decisions in clinical practice, is an essential component of medical professionalism [5]. PCO was previously described as “the philosophy that one knows everything about one’s patients and does everything for them [6].” More recently, the concept has gradually changed against the backdrop of international working hour regulations for physicians and the promotion of interprofessional work and team-based patient care. For example, a qualitative study in the U.S. revealed that PCO was composed of the following components: advocacy for the patient, communication and care coordination, decision-making, follow-up in completing tasks of patient care, knowledge, leadership, attitudes of doing more than the minimum required, responsibility, serving as primary or main care provider, demonstrating initiative, and providing the best care [7]. Another qualitative study identified three key components of PCO in the night float system of a Canadian internal medicine residency program: continuous personal concern for patients, autonomous decision-making, and knowledge of patients’ problems [8]. While PCO is an important element that should be mastered during residency [9], it should also be cultivated during medical school, when medical students begin to form professional identities [10, 11].
There have been many studies on PCO, most of which focused on medical residents [12]. Most of these studies employ qualitative research design. In addition to the aforementioned studies investigating the components of PCO, Robinson et al. investigated the relationship between PCO and pediatric residents’ decision-making opportunities [13]. The PCO Scale (PCOS) was developed for U.S. medical residents by Djulbegovic et al. in 2019 [14, 15] and its Japanese translation by Fujikawa et al. in 2021 [16]. Since then, quantitative studies on PCO among medical residents have gradually been conducted. For example, a study conducted in Japan explored the association between PCO and personal or environmental factors among medical residents using the Japanese medical residents’ version of the PCOS [17].
Conversely, few studies have focused on PCO among medical students because there were no instruments to measure PCO among medical students. Recently, a version of the PCOS for medical students (PCOS-S) was developed and validated by Wyatt et al. in 2023 [12]. Medical undergraduates are expected to take patient ownership appropriate to their level of training; since Djulbegovic’s scale is too advanced for medical undergraduates, Wyatt et al. created a scale adapted for them, PCOS-S. There is no corresponding tool in Japan. Developing such a tool would be useful to conduct future international studies and to track the development of medical students in important aspects of becoming a physician. Therefore, the aim of this study was to construct the Japanese version of the PCOS-S by translating, adapting and validating the scale for use in Japan.
Methods
Study design and participants
This multicenter cross-sectional study was conducted at five universities in Japan between June and July 2023. The participating universities varied in location and type to ensure the diversity of the student population. Eligible participants were all fifth- and sixth-grade medical students (i.e., clinical-year medical students) at the five universities. Anonymous online questionnaires, using a weblink created by SurveyMonkey (www.surveymonkey.com), were distributed to all the eligible participants by the director of undergraduate medical education at each university. Since the questionnaire was designed to be applicable only to inpatient care at the time of survey response, we decided to include only students who were in charge of inpatients at the time of the study.
Curriculum of medical undergraduates in Japan
Herein, we briefly describe the curriculum of medical students in Japan to aid understanding the study context. The Japanese undergraduate medical education is six years long [18, 19]. It typically consists of four years of preclinical education and two years of clinical education. A shift in clinical clerkship from the traditional “observation” model to the “participation” model has been continually advocated since the 2000s. In reality, however, the shift has made little progress [20]. In addition, although the Model Core Curriculum for Medical Education, developed by the Ministry of Education, Culture, Sports, Science and Technology, serves as the guideline for curricula of all medical schools [21], actual medical education varies from university to university and department to department.
Measures
The questionnaire consisted of three parts:1) informed consent, 2) demographic questions, and 3) questions PCO.
1) Informed consent.
Informed consentwas obtained from all the participants. We asked the participants to tick a consent box to indicate their agreement to take part in the survey.
2) Demographic questions.
In the second part of the questionnaire, we collected data on participants’ demographic information, including gender, name of the university, grade, and clinical department to which they were assigned to at the time of the survey. We also asked them whether the participants were in charge of inpatients in the clinical clerkship at the time of the study because the questionnaire was only used in inpatient care settings. In addition, we asked the participants to what extent the department was educational (as described in detail hereafter).
3) Questions regarding PCO.
The third part of the questionnaire asked the participants about their experiences with PCO. The PCOS-S used in this study includes 19 items [12]. Each item is answered on a six-point Likert scale (from 1 = strongly disagree to 6 = strongly agree). Scale scores are calculated by simple summation of the items, with higher scores indicating higher PCO. Factor analysis supported a four-factor structure: Factor 1 (seven items, team inclusion), Factor 2 (five items, accountability), Factor 3 (four items, territoriality), and Factor 4 (three items, self-confidence) [12].
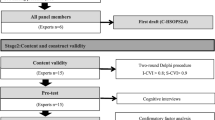
The Japanese version of the scale was developed using an established translation process [22] as follows: We obtained permission from the original author for the translation of the scale into Japanese. Second, three translators (HF, DS, and KK) performed forward translations from English to Japanese. They had experience translating survey instruments [16, 23, 24], including medical residents’ version of the PCOS [16]. Third, the three translations were reviewed and synthesized by three translators (Version 1). Fourth, Version 1 was back translated from Japanese into English by professional bilingual translators who were not involved in the study. Three translators compared the above two versions, the back-translated version with the original, and revised them to create Version 2. Fifth, FH emailed the original author, asked for a review, and the author confirmed that there was no need for correction of the translation. Sixth, a medical education expert (MH) reviewed Version 2 and found no particular problems with the translation. Seventh, we conducted a pilot survey with three medical students to check if there were any difficulties in understanding the content and completing the questionnaire. Pilot tests revealed no major problematic items. Finally, all authors confirmed the instrument’s face and content validity. Therefore, Version 2 was considered acceptable for use in collecting data.
Statistical analysis
The following four steps were taken to validate the Japanese version of the PCOS-S:
First, we performed an exploratory factor analysis (EFA) to test the structural validity of the scale. After checking the Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy and Bartlett’s sphericity test, we conducted an EFA. The recommended criteria for reliable EFA are as follows: a KMO value of 0.60 or greater and a significant Bartlett’s test of sphericity [25]. We used promax rotation in conjunction with the maximum likelihood estimation. A parallel analysis was conducted for factor extraction [26]. Items with factor loading below 0.40 were excluded.
Second, convergent validity was assessed through hypothesis testing. A previous study showed a link between PCO and the level of the clinical department as a learning environment among medical residents [17]. In this study, the association between the Japanese version of the PCOS-S and global rating scores of the clinical department as a learning environment was assessed using Pearson’s correlation coefficients. Consistent with a previous study [17], the question asking to rate the clinical department as a learning environment was as follows: “Using any number from 0 to 10, where 0 is the worst possible and 10 is the best possible, what number would you use to rate your current department as a learning environment?” Pearson correlation coefficients above 0.30 were considered meaningful [27].
Third, the internal consistency reliability was assessed using Cronbach’s alpha. Previous studies suggest that a value of 0.70 or higher is the satisfactory criterion [28].
Fourth, descriptive statistics were calculated on the scale scores, including the mean, standard deviation, and observed range. We also conducted an independent t-test to investigate the possible influence of participant’s year group on the PCOS-S scores. We chose a complete case analysis. R version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria; www.R-project.org) was used for the data analysis. To conduct the EFA, we used psych version 2.3.6 and GPArotation version 2023.8-1 [29, 30].
Ethical considerations
The participants were enrolled in a drawing for one of five ¥5,000 vouchers. Ethical approval was obtained from the Institutional Review Board of the University of Tokyo (2022066NI).
Results
A flowchart of the participants is shown in Fig. 1. Of the total 1236 eligible participants, 227 responded to the online questionnaire. Of these, 86 students who were responsible for outpatient care only and 19 students who were responsible for inpatient care but had missing data were excluded. Therefore, 122 students’ responses were included in the final analysis. The characteristics of those participants are presented in Table 1. Responses to each item on the scale are shown in Table 2.
1) Structural validity.
The KMO value was 0.80, exceeding the required 0.60, and the result of Bartlett’s test of sphericity was χ2 = 1170.557 (df = 171, p < 0.001). As these results indicated that the items of the scale were suitable for EFA, we decided to conduct it.
After several iterations, the EFA suggested that 6 of the 19 items should be deleted because of low factor loadings (< 0.37). The authors reviewed six items and concluded that they should be deleted because they did not appear to fit the Japanese context. The final results of the EFA are listed in Table 3. The results suggest a three-factor structure, and all factor loadings presented good values (> 0.40).
Through discussions among the authors, the following three factors were identified: Factor 1 (7 items), team engagement; Factor 2 (3 items), self-confidence; and Factor 3 (3 items), territoriality.
2) Convergent validity.
We examined the Pearson correlation coefficient between the Japanese PCOS-S scores and the global rating scores of the clinical department as a learning environment. The value was 0.61, which exceeded the required 0.30 (p < 0.001).
3) Internal consistency reliability and descriptive statistics.
Table 4 shows the internal consistency reliability and descriptive statistics of our scale. The overall Cronbach’s alpha for the scale was 0.81. The Cronbach’s alpha values of all the factors exceeded the satisfactory criterion of 0.70. Table 5 shows the result of the independent t-test to examine the influence of participants’ year group on the PCOS-S scores. 6th-year students had significantly higher PCO than 5th-year students. Thus, the final version of the Japanese PCOS-S was developed.
Discussion
We developed a 13-item Japanese version of the PCOS-S to assess PCO in medical students and examined its psychometric properties. PCO assessment plays a vital role in medical education. The instrument developed in this study can improve the quality of undergraduate medical education and PCO research.
In the internal consistency reliability analysis, Cronbach’s alpha for all subscales met the satisfactory criterion. This finding was consistent with that of the original study. The original scale had four subscales with Cronbach’s alpha coefficients of 0.78 or higher. Thus, the scales appeared to have adequate internal consistency and reliability.
In the present study, the factor analysis showed a three-factor structure, whereas the original scale of the English version has a four-factor structure. Comparing the Japanese and English versions, most items in the accountability dimension were excluded from the former. There may be two possible reasons. First, differences in the content of medical education between Japan and the U.S. may have an impact on the results. As we described in the Methods, the clinical clerkship in Japan is often conducted in an “observation” model [20]. Accordingly, Japanese medical students may have few experiences of accountability in each clinical clerkship. Second, it is possible that this discrepancy may be a reflection of the unique characteristics of Japanese culture. It is often said that Japanese society is traditionally ill-suited to the concept of accountability [31]. In Japan, the Western notion of “accountability” was first introduced in the mid-1990s [32]. It was a difficult concept to understand in Japanese society and is currently often translated as “setsumei sekinin,” which literally means “duty to explain” [32]. However, it has been pointed out that by translating the term accountability into “setsumei sekinin,” the original broad meaning of accountability has been lost in Japan. For example, “setsumei sekinin” does not include responsibility for results, responsibility to have other people explained, or the ability to explain and gain acceptance [31]. Behind this is a part of the Japanese culture that favors stillness and silence. In Japan, silence is important because of Zen Buddhism [33,34,35]. The discourse on silence has been found not only in traditional literature but also in modern Zen practices, in which silence is understood as an expressive form of understanding [34]. In other words, the culture values refraining from speaking up and questioning in public and avoiding people who do so [31]. This long-standing attitudinal difference could explain why most items in the accountability dimension disappeared in our Japanese version, resulting in a three-factor structure. There would be a need for future research to confirm the factor structure.
Our scale is the first validated instrument to assess PCO in a Japanese undergraduate medical education setting. Factor analysis appears to have succeeded in creating a scale that is commensurate with the current state of clinical clerkship for Japanese medical students, as described earlier. In addition, in our sample, 6th graders had significantly higher PCO than 5th graders, suggesting that educational intervention may nurture PCO. We suggest that medical educators in Japan use our scale to assess the PCO of medical students, which we believe will be an effective tool to guide to quality improvements in undergraduate medical education. It would be useful to observe how the PCO of medical students changes over time during their clerkships. We also recommend that researchers use our instrument to examine the association between the PCO of medical students and their clinical outcomes (e.g., patient experience), which has not yet been explored. Moreover, developing a PCOS-S in languages other than English and Japanese would facilitate international research and enrich medical students’ PCO knowledge.
We should note a couple of potential limitations. First, the response rate and sample size were relatively low. Including more medical students in future studies would strengthen our argument for using this scale. Second, we cannot exclude the possibility of selection bias. It is possible that only medical students with high PCO responded to the questionnaire. Third, as the questionnaire was for a particular clinical department inpatient clerkship at the time of response, the educational curriculum of the department would influence the result. Fourth, we did not carry out confirmatory factor analysis to verify the factor structure resulting from the EFA. Future studies should test the three-factor structure using confirmatory factor analysis. Fifth, validity other than structural and convergent validity (e.g., discriminant validity) and reliability other than internal consistency reliability (e.g., test-retest reliability) were not evaluated. Further research is required to assess these psychometric properties. Sixth, because this was a scale validation study, the association between PCOS-S overall and subscale scores and other concepts is unknown. Future research would deepen our knowledge of PCOS-S, for example, by investigating the relationship between PCOS-S scores and academic performance.
Conclusions
We translated the PCOS-S into Japanese, and tested and verified its structural validity, convergent validity, and internal consistency reliability. The Japanese PCOS-S has good reliability and validity. Three factors were extracted from the factor analysis. This instrument could be useful for quality improvement and research on bridging undergraduate medical education for PCO to clinical settings and practices. Further studies are required to confirm the robustness of this scale.
Data availability
The datasets generated and analyzed in this study can be made available by the corresponding author upon reasonable request.
Abbreviations
- EFA:
-
Exploratory factor analysis
- KMO:
-
Kaiser–Meyer–Olkin
- PCO:
-
Patient care ownership
- PCOS:
-
Patient care ownership scale
- PCOS-S:
-
Patient care ownership scale – Medical students version
References
Parthiban N, Boland F, Fadil Azim DH, Pawlikowska T, O’Shea MT, Jaafar MH, et al. Asian medical students’ attitudes towards professionalism. Med Educ Online. 2021;26(1):1927466.
Monrouxe L, Rees C. What is healthcare professionalism? Healthcare professionalism: improving practice through reflections on workplace dilemmas. Chichester, UK: Wiley; 2017.
Medical Professionalism Project. Medical professionalism in the new millennium: a physicians’ charter. Lancet. 2002;359(9305):520–2.
ABIM (American Board of Internal Medicine Foundation), ACP-ASIM. (American College of Physicians-American Society of Internal Medicine) Foundation, European Federation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med. 2002;136(3):243–6.
Dubov A, Fraenkel L, Seng E. The importance of fostering ownership during medical training. Am J Bioeth. 2016;16(9):3–12.
Van Eaton EG, Horvath KD, Pellegrini CA. Professionalism and the shift mentality: how to reconcile patient ownership with limited work hours. Arch Surg. 2005;140(3):230–5.
Cowley DS, Markman JD, Best JA, Greenberg EL, Grodesky MJ, Murray SB, et al. Understanding ownership of patient care: a dual-site qualitative study of faculty and residents from medicine and psychiatry. Perspect Med Educ. 2017;6(6):405–12.
Masson V, Snell L, Dolmans D, Sun NZ. Exploring the evolving concept of ‘patient ownership’ in the era of resident duty hour regulations-experience of residents and faculty in an internal medicine night float system. Perspect Med Educ. 2019;8(6):353–9.
McLaren K, Lord J, Murray SB, Levy M, Ciechanowski P, Markman J, et al. Ownership of patient care: a behavioural definition and stepwise approach to diagnosing problems in trainees. Perspect Med Educ. 2013;2(2):72–86.
Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. Reframing medical education to support professional identity formation. Acad Med. 2014;89(11):1446–51.
Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185–91.
Wyatt TR, Wood EA, Waller JL, Egan SC, Stepleman LM. Patient care ownership in medical students: a validation study. BMC Med Educ. 2023;23(1):127.
Robinson M, Bowen J, Aylor M, van Schaik M. Finding (and keeping) a voice: pediatric residents’ perceptions of autonomy and patient care ownership. Acad Med. 2021;96(11S):S213–4.
Djulbegovic M, Beckstead JW, Fraenkel L. The patient care ownership scale: development of an instrument to measure patient care ownership among internal medicine trainees. J Gen Intern Med. 2019;34(8):1530–7.
Djulbegovic M, Kulkarni SA, Chen KL, Canavan M, White MA, McGuire WC, et al. The patient care ownership scale: external validation of an instrument that measures patient care ownership among internal medicine trainees-a multi-institutional study. J Gen Intern Med. 2021;36(12):3680–8.
Fujikawa H, Son D, Kondo K, Djulbegovic M, Takemura Y, Eto M. Translating and validating a Japanese version of the Patient Care Ownership Scale: a multicenter cross-sectional study. BMC Med Educ. 2021;21(1):415.
Fujikawa H, Son D, Aoki T, Eto M. Association between patient care ownership and personal or environmental factors among medical trainees: a multicenter cross-sectional study. BMC Med Educ. 2022;22(1):666.
Fujikawa H, Son D, Eto M. Are residents learners or workers? A historical perspective in Japan. TAPS. 2021;6(1):122–4.
Fukushima O. History of medical education in Japan. Med Educ (Japan). 2018;49:421–8.
Ministry of Health, Labour and Welfare. Research on medical practices that can be carried out in clinical practices in undergraduate medical education 2018 [cited 2024 June 1]. https://www.mhlw.go.jp/content/10803000/000341168.pdf.
Medical Education Model Core Curriculum Expert Research Committee. Model Core Curriculum for Medical Education in Japan. AY 2022 Revision 2023 [cited 2024 June 1]. https://www.mext.go.jp/content/20230323-mxt_igaku-000028108_00003.pdf].
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–91.
Fujikawa H, Son D, Aoki T, Kondo K, Takemura Y, Saito M, et al. Translating and validating a Japanese version of the instrument for patient assessment of medical professionalism (J-IPAMP): a cross-sectional survey. BMC Med Educ. 2022;22(1):641.
Fujikawa H, Son D, Hayashi M, Kondo K, Eto M. Translation, adaptation, and validation of the Tolerance of Ambiguity in Medical students and doctors (TAMSAD) scale for use in Japan. BMC Med Educ. 2023;23(1):405.
Tabachnick BG, Fidell LS. Using multivariate statistics. 7th ed. New York: Pearson; 2019.
Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. 8th ed. Andover: Cengage Learning EMEA; 2019.
Cohen J. Statistical power analysis. Curr Dir Psychol Sci. 1992;1(3):98–101.
Nunnally J, Bernstein I. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
The Comprehensive R. Archive Network. Package ‘psych’: The Comprehensive R Archive Network; 2023 [ https://cran.r-project.org/web/packages/psych/psych.pdf.
The Comprehensive R. Archive Network. Package ‘GPArotation’: The Comprehensive R Archive Network; 2023 [ https://cran.r-project.org/web/packages/GPArotation/GPArotation.pdf.
Yamaya K. Accountability and assessment — once again. Situation Reflect Kaikeityosakenkyu. 2020;62(1):5–10.
Kadomatsu N. Accountability of administration in Japan after the mid-1990s. J Japanese Law. 2011;16:5–20.
John B, Sueki F, Yamada S, Beyond Zen. D. T. Suzuki and the Modern Transformation of Buddhism. 1st ed. Hawaii: University of Hawaii; 2022.
Davis BW. Zen pathways: an introduction to the philosophy and practice of Zen Buddhism. New York: Oxford University Press; 2021.
Jones S. Speech is silver, silence is golden: the cultural importance of silence in Japan. ANU Undergrad Res J. 2011;3:17–27.
Acknowledgements
The authors would like to thank Dr. Tasha R. Wyatt for her advice on the writing of this paper. We would also like to thank all the participants.
Funding
This work was partly supported by JSPS KAKENHI Grant Number JP23K19809.
Author information
Authors and Affiliations
Contributions
HF, MH, DS, KK, and ME designed the study. HF analyzed the data and drafted the manuscript. All authors rigorously reviewed the manuscript and collectively approved its final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
At the beginning of the questionnaire, each participant ticked the consent box to indicate that they agreed to participate in the study. The procedures passed the Institutional Review Board of the University of Tokyo (2022066NI) and kept with the Declaration of Helsinki’s ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fujikawa, H., Hayashi, M., Son, D. et al. Translating, adapting, and validating the medical student version of the patient care ownership scale for use in Japan. BMC Med Educ 24, 706 (2024). https://doi.org/10.1186/s12909-024-05704-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05704-8