Abstract
Background
Medical schools are called to be socially accountable by medical education and healthcare system stakeholders. Social accountability is a feature of excellent medical education. Medical students are essential to the development of socially accountable medical schools. Therefore, understanding the perceptions and experiences of medical students regarding social accountability is critical for efforts to improve social accountability practices and outcomes.
Methods
This cross-sectional online questionnaire-based survey used Google Forms and involved medical students in their fourth and fifth years of study at the Makerere University School of Medicine. The survey was conducted between September 2022 and October 2023. We used a study questionnaire and a validated toolkit designed by students as part of The Training for Health Equity Collaborative to gauge a school’s progress towards social accountability in medical schools to collect data on demographics, perceptions and experiences and evaluate social accountability.
Results
Out of 555 eligible medical students, 426 responded to the online questionnaire. The response rate was 77%. The mean age of the students was 25.24 ± 4.4 years. Almost three fourths of the students were male (71.3%), and slightly less than two thirds were in their fourth year of study (65%). Almost half of the students (48.1%%) evaluated the school as doing well with regard to social accountability. The evaluation items referring to community-based research and positive impact on the community had the highest mean scores. Only 6 (3.6%) students who reported hearing of social accountability had a clear understanding of social accountability. Students receiving career guidance in secondary school was associated with evaluating social accountability in the medical school as strong (p-0.003).
Conclusions
Medical students evaluated the medical school favorably forsocial accountability despite lacking a clear understanding of social accountability. Receiving career guidance in secondary school was significantly associated with a positive evaluation of social accountability.
Similar content being viewed by others
Background
Medical students are essential to the development of a socially accountable medical school [1, 2]. Social accountability for medical schools is defined as the obligation of the medical school to direct education, research, and service activities toward the most important needs of the community served by the medical school and its graduates [3]. While medical students are expected to learn about social accountability and become socially accountable practitioners, little has been documented about their perceptions and experiences of social accountability.
Medical students have distinct and unique experiences during training, which may influence their future practice and choices following graduation [4, 5]. It is important to understand these experiences to improve the teaching and learning of social accountability. Previous studies have shown that medical students have a limited understanding of social accountability [5,6,7]. The partnership pentagram identifies five key stakeholders for social accountability in health professions education including policymakers, health administrators, health professionals, academics and community members [2, 8]. A survey of Deans in Korea reported that interactions between partners had the greatest influence on social accountability in medical education [9]. Medical students are the future of the healthcare system; therefore, understanding their perceptions and experiences could be a starting point for improving their learning and adoption of social accountability [1, 4].
The Students’ Toolkit on Social Accountability of Medical Schools was developed through a collaboration between the International Federation of Medical Students Associations (IFMSA) and the Training for Health Equity Network (THEnet) [1, 4, 10]. The toolkit aims to provide a brief introduction to social accountability for medical students and empower them to make a difference in their schools in the area of social accountability. The toolkit is an evaluation tool for students to assess the progress made by their medical school in terms of social accountability and to create action plans to improve social accountability at the medical school [1]. This kit has been applied in various settings most often in high-income countries [4, 11].
The perceptions and experiences of medical students regarding social accountability are unique because of contextual differences that may influence their learning and adoption of social accountability [12, 13]. There is a dearth of published literature about these perceptions and experiences, particularly from sub-Saharan Africa. The purpose of this study is to determine the perceptions and experiences of medical students regarding social accountability at the Makerere University School of Medicine.
Methods
Study design and questionnaire
We conducted a cross-sectional online questionnaire-based survey between September 2022 and October 2023 using Google Forms. This study collected responses from medical students from the Makerere University School of Medicine. The validated Students’ Toolkit on Social Accountability in Medical Schools, which has been applied widely to study perceptions of social accountability, was used for this study, with some modifications [1]. The final study questionnaire had three sections: demographic information, perceptions, and experiences related to social accountability; and the evaluation section from the toolkit. The questionnaire was pretested on eight undergraduate medical students in their fourth or fifth year of study. The link to the questionnaire on Google Forms was sent to each student’s email. Each link was unique to each email address to avoid reuse and double enrollment.
Study setting
We conducted this study at the Makerere University School of Medicine in Uganda. Makerere University is a government-owned university, and the Makerere University School of Medicine is the oldest medical school in East Africa. The Bachelor of Medicine and Bachelor of Surgery (MBCHB) program spans five years. In their third and fourth year of study, medical students spend time in the community for Community Based Education, Research and Service (COBERS). Before COBERS, students undergo preparatory sessions at the university and are assigned site and university supervisors to follow their progress. During COBERS, students identify a community problem, develop and implement interventions. Thereafter, the students evaluate the impact of the intervention [14].
Characteristics of participants
We invited all students in their fourth or fifth year of medical school to participate in the study through trained research assistants. A total of 555 students were eligible to participate in the study. We selected fourth- and fifth-year students because they were more likely to have had experiences related to social accountability in medical school. We identified twelve research assistants from among the fourth- and fifth-year students and trained them in the study procedures. The research assistants obtained written informed consent from the participants and registered their email addresses. We sent links to the electronic survey to the registered email addresses. The research assistants provided weekly phone call or in-person reminders to students who had not responded to the survey. We collected responses over two academic years therefore two sets of fourth year students were enrolled. However, the fifth years in the second academic year of the study had already been enrolled as fourth year students.
Statistical analysis
We collected the data using Google Forms. We exported the data to Microsoft Excel, checked for completeness and missing data. We then cleaned the data. The data were analyzed with R statistical software. The descriptive statistics are reported. The total score for the students’ toolkit 12 social accountability evaluation items was computed, and the means and standard deviations for the individual items are presented. The total scores were categorized according to the key provided in the student toolkit. The categories included 0–8, weak foundation; 9–17, some evidence of social accountability; 18–26, doing well (identify areas of improvement); and 27–36, strong foundation. For the regression analysis to determine the factors associated, the categories defined in the toolkit were classified in two groups (1) Limited social accountability (weak and some social accountability) and (2) Strong social accountability (looking for areas of improvement and strong social accountability). The chi-square test and Fisher’s exact test were used. A p value < 0.05 indicated statistical significance.
Results
There were 555 eligible medical students at the Makerere University School of Medicine during the study period. This study involved 426 medical students therefore the response rate was 77%. The mean age of the students was 25.24 ± 4.4 years. Most of the participants were in their fourth year of study, as the link was available over two academic years. The characteristics of the study participants are summarized in Table 1.
Student perceptions and experiences of social accountability
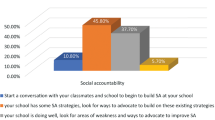
When asked if they had ever heard about social accountability, 165 (38.73%) students responded ‘yes’. To build on this previous question, participants were asked ‘What do you understand by the term social accountability?’. Only 6 (3.6%) of those who reported having heard about social accountability clearly defined the term capturing the active and multidimensional nature of social accountability. Of the 165 (39%) participants who reported hearing about social accountability before, 91 (55%) encountered the term in personal reading. The average time spent in community-based education research and service was 6.8 weeks, and most (40.1%) of the students reported feeling moderately prepared for their last COBERS experience. (Fig. 1)
Students’ evaluation of social accountability at medical schools
Using the Students’ Toolkit for Social Accountability in Medical Schools, 48.1% of the medical students evaluated the medical school as doing well in social accountability, with a total score between 18 and 26. In contrast, 1.4% of the students felt that the medical school had a weak foundation for social accountability. (Fig. 2)
Of the twelve items used to assess social accountability, seven items (1, 2, 3, 7, 8, 11 and 12) were related to perceptions, while five items (4, 5, 6, 9 and 10) were related to experiences. Item 10 (Does your school have community-based research? ) 2.57 ± 0.62 and Item 12 (Does your school have a positive impact on the community? ) 2.434 ± 0.67 had the highest mean scores. Item 4 (Do you learn about other cultures? ) 1.37 ± 0.93 and Item 8 (Do your teachers reflect the sociodemographic characteristics of the reference population? ) 1.60 ± 0.92 had the lowest mean scores. (Table 2)
The only factor that was significantly associated with evaluation of social accountability in medical school as strong was receiving career guidance in secondary school (p 0.003). (Table 3)
Discussion
We evaluated the perceptions and experiences of medical students at the Makerere University School of Medicine regarding social accountability. Medical students are central to the adoption and practice of social accountability efforts in medical schools. The perceptions and experiences of the medical students in this study reflect exposure to the concept and practice of social accountability. Learning social accountability requires deliberate and meaningful efforts in which medical students are considered partners. Our study findings suggest that medical students at the Makerere University School of Medicine have varied perceptions and experiences of social accountability; most of the students evaluated the medical school favorably, and receiving career guidance in secondary school was associated with a positive evaluation of social accountability. Most medical students felt that the medical school was doing well in social accountability and needed to look at areas of weakness and ways to advocate for improving social accountability. The recommended actions for students to take concerning each scoring category of social accountability in the student toolkit reflect the continuous quality improvement approach that is vital for social accountability [1]. The highest mean scores for items in the students’ toolkit for social accountability in medical schools were for community-based research and for the positive impact of the medical school on the community. The least favorable assessment items include learning about other cultures and teachers reflecting the reference population. Medical students come from varied backgrounds and have different experiences during medical education; therefore, it is not surprising that the perceptions, experiences and evaluations of the medical school were diverse. While career guidance in secondary school was associated with a good evaluation of social accountability at the medical school, we cannot confirm a causal relationship between the two. This relationship may be an area for further evaluation. This study helps us to characterise medical students’ views regarding social accountability and the factors that may influence these views. These findings provide a starting point for improving student experiences of social accountability in medical education.
The high percentage of students who gave a good evaluation of social accountability at medical school reflects efforts by the medical school to achieve this goal. These efforts include community-based education, research and services and adopting a competency-based medical education curriculum to better meet the community’s needs [15, 16]. Our findings are comparable to those of a study conducted at a Saudi Arabian government-funded medical school where most students felt that the medical school was performing well in terms of social accountability [4].
There have been gains in pursuing social accountability goals, and more needs to be done to enable students to understand the concept and demonstrate its values. Our findings concur with a previous study that showed a poor understanding of social accountability among stakeholders. This previous study also provided evidence of social accountability in medical school activities [6]. Similarly, a qualitative study in the United Kingdom also showed that students did not understand the concept of social accountability or feel that it has implications for their medical education or future practice [5].
The major strength of this study lies in the relatively large sample size, as we tried to enroll all eligible participants. The limitation of this study is that it was conducted at one study site, which may limit the generalizability of the findings. However, the presence of similar findings in other settings supports the generalizability of our findings. Recall bias was minimized by enrolling students who were still in medical school.
Conclusions
Medical students at the Makerere University School of Medicine have varied perceptions and experiences of social accountability. However, the students lack a clear understanding of social accountability. Most students felt moderately prepared for COBERS and evaluated the medical school positively for social accountability. Regarding individual items in the student toolkit, the presence of community-based research and the school having a positive impact on the community had higher mean evaluation scores. Receiving career guidance in secondary school was associated with a positive evaluation of the medical school.
Recommendations
The medical school should provide students with more opportunities to learn about social accountability and routinely evaluate the perceptions and experiences of medical students regarding social accountability. In addition, the medical school should effectively prepare students for Community-Based Education Research and Service.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- COBERS:
-
Community Based Education Research and Service
References
Dijk S, Pálsdóttir B, Ross SJ, Bhiri M, Ramalho R, Glasner J. Students’ Toolkit on Social Accountability in Medical Schools. Amst IFMSA. 2017.
Rourke J. Social accountability in theory and practice. Ann Fam Med. 2006;4(Suppl 1):S45–8. discussion S58.
Boelen C, Heck JE, World Health Organization. Defining and measuring the social accountability of medical schools. World Health Organization; 1995.
Masud N, Alenezi S, Alsayari O, Alghaith D, Alshehri R, Albarrak D et al. Social accountability in Medical Education: students’ perspective. In Frontiers; 2022. p. 868245.
McCrea ML, Murdoch-Eaton D. How do undergraduate medical students perceive social accountability? Med Teach. 2014;36(10):867–75.
Galukande M, Nakasujja N, Sewankambo NK. Social accountability: a survey of perceptions and evidence of its expression at a sub saharan African university. BMC Med Educ. 2012;12:1–6.
Clithero-Eridon A, Ross A, Albright D. Conceptualising social accountability as an attribute of medical education. Afr J Prim Health Care Fam Med. 2020;12(1):1–8.
Boelen C. Towards unity for health: challenges and opportunities for partnership in health development [Internet]. Geneva: World Health Organization; 2000 [cited 2023 Jul 1] p. 84 p. Report No.: WHO/EIP/OSD/2000.9. https://apps.who.int/iris/handle/10665/66566.
Lee ST, Yang EB. Factors affecting social accountability of medical schools in the Korean context: exploratory factor and multiple regression analyses. Med Educ Online. 2022;27(1):2054049.
Swed S, Alibrahim H, Bohsas H, Nasif MN, Abouainain Y, Jabban YKE, et al. Assessing social accountability perspectives among Syrian medical students: a cross-sectional study. BMC Med Educ. 2023;23(1):980.
Coşkun Ö, Timurçin U, Kıyak YS, Budakoğlu Iİ. Validation of IFMSA social accountability assessment tool: exploratory and confirmatory factor analysis. BMC Med Educ. 2023;23(1):138.
Mohammadi M, Bagheri M, Jafari P, Bazrafkan L. Motivating medical students for social accountability in medical schools. J Adv Med Educ Prof. 2020;8(2):90.
Boelen C, Woollard R. Social accountability: the extra leap to excellence for educational institutions. Med Teach. 2011;33(8):614–9.
Kizito S, Baingana R, Mugagga K, Akera P, Sewankambo NK. Influence of community-based education on undergraduate health professions students’ decision to work in underserved areas in Uganda. BMC Res Notes. 2017;10(1):726.
McKenzie-White J, Mubuuke AG, Westergaard S, Munabi IG, Bollinger RC, Opoka R, et al. Evaluation of a competency based medical curriculum in a sub-saharan African medical school. BMC Med Educ. 2022;22(1):724.
Nakanjako D, Omaswa F. A century of health professions’ education, training, academic research and service at Makerere University, Kampala, Uganda. Afr Health Sci. 2022;22(2):i–v.
Acknowledgements
Not applicable.
Funding
The research reported in this publication was supported by the Fogarty International Center of the National Institutes of Health, U.S. Department of State’s Office of the U.S. Global AIDS Coordinator and Health Diplomacy (S/GAC) and the President’s Emergency Plan for AIDS Relief (PEPFAR) under Award Number 1R25TW011213. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
LO conception of the study, acquisition and analysis of data, drafting the paper and writing the final version. IGM, SK and AGM- refined the study concept, reviewed the results, drafted the paper and approved its final version.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Ethical approval for the study was obtained from the Makerere University School of Medicine Institutional Review Board (Mak-SOMREC-2021-77) and the Uganda National Council for Science and Technology. Written informed consent was obtained from the study participants.
Consent for publication
Not applicable.
Competing interests
AGM is a member of the BMC Medical Education editorial board. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Oriokot, L., Munabi, I.G., Kiguli, S. et al. Perceptions and experiences of undergraduate medical students regarding social accountability: a cross-sectional study at a Subsaharan African medical school. BMC Med Educ 24, 409 (2024). https://doi.org/10.1186/s12909-024-05412-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05412-3