Abstract
Background
The need for clinical placements outside traditional teaching hospitals for medical students is growing, both due to a decrease in hospital beds and the expansion of medical students. In this survey, distributed to supervisors at university and non-university hospitals, we investigated supervisors’ self-perceived preparedness for the training assignment and searched for factors associated with self-perceived pedagogical knowledge and familiarity with the students’ learning objectives.
Methods
A pilot survey was developed using results from qualitative studies regarding clinical supervision of medical students and included questions on the supervisors’ education and preparation, if they were familiar with the students’ learning objectives, self-perceived pedagogical knowledge, and characteristics of the learning environment. The pilot survey was tested on a smaller group of supervisors. The results from the pilot survey were used to develop an e-survey that was distributed to all hospital employed physicians in Region Västra Götaland.
Results
The survey was completed by 1732 physicians (response rate 43%). Among 517 respondents at the university hospital who reported activity as supervisor, 240 (46%) had attended preparatory supervisor training, 423 (82%) perceived enough pedagogical knowledge for the teaching assignment, and 391 (76%) reported familiarity with the learning objectives. The corresponding proportions at non-university hospitals were 159/485 (33%), 363/485 (75%), and 298/485 (61%), respectively (p ≤ .007 all through, compared to the university hospital). Perceiving that goal description and written information from the course management was sufficient for being able to complete the training assignment showed strong association with both self-perceived pedagogical knowledge and familiarity with the students’ learning objectives.
Conclusions
We found consistent differences between university and non-university hospitals with respect to the supervisors’ self-perceived preparedness for the training assignment. Efforts to convey the learning objectives and support to clinical supervisors are crucial for supervision of students at non-university hospitals.
Similar content being viewed by others
Introduction
The number of hospital beds per capita is dropping globally [1]. Meanwhile, the number of medical students requiring clinical placement is stable or increasing. As an example, from 1990 to 2015, the number of hospital beds per capita in Sweden were reduced by 80% [2, 3]. At the same time, from 1997 to 2017, the number of medical students in Sweden increased by 70% [4]. More students and fewer available patients in inpatient care led all medical schools in Sweden to expand their clinical rotations to smaller hospitals, not previously involved in undergraduate medical education. Similar trends are seen in UK and USA where a growing number of smaller hospitals are involved as sites for undergraduate training of medical students [5].
A smaller hospital within a region, associated with a medical school and a university hospital and admitting medical students, can be defined as a regional clinical campus [6]. Establishing a regional clinical campus requires adaptation in several areas. First, to supply the physical environment with adequate workspace for students’ educational activities. Second, to educate and prepare colleagues and staff to participate in clinical teaching [7, 8]. Reports show large variation in supervisors clinical interaction with students, and varying quality of clinical supervision [9,10,11].
When a regional clinical campus is established, local physicians must adapt to a new role, namely as clinical supervisors to medical students. Clinical supervisors at non-university hospitals usually have less formal educational training [12]. Research regarding clinical supervision of medical students indicate that there is a need for physicians both to learn more about basic educational principles and to develop a self-image as teachers to adapt to their new role [13, 14]. Hence, university courses that address students’ clinical supervisors should aim to improve teaching skills and confidence in teaching [15].
In addition to being skilled in teaching, physicians at a clinical campus need to know what the students are expected to learn [16,17,18,19]. Constructive alignment is commonly used as a tool to devise learning activities based on the intended learning outcomes [20, 21]. In the context of clinical rotation, the learning objectives point out to both students and supervisors what knowledge, skills and attitudes students are expected to acquire, in order to pass. Typically, early stages of learning are focused on knowledge and comprehension where later stages focus on analysis and synthesis [20, 22]. It follows that clinical supervisors need to know their students learning objectives to be able to adjust to the students’ needs and facilitate learning efficiently [23,24,25,26].
To date, the literature on how physicians at regional campuses are prepared for clinical supervision of medical students is limited. In the present study, we build on previous qualitative research concerning clinical supervision of medical students, conducted at our medical school [27,28,29,30]. The results from the qualitative research formed the base for the survey used in this study, with the aim to search for (a) factors associated with clinical supervisors’ self-perceived pedagogical knowledge and (b) their familiarity with students’ learning objectives at their clinical placements. Supervisors at non-university hospital are compared with those at a university hospital.
Methods
Setting
The health care system in Sweden is publicly funded and is organized in the same way throughout the country. Sweden is divided in six larger regions served by seven tertiary care university hospitals responsible for all highly specialized care. Smaller hospitals in each region can transfer patients to their university hospital. There are seven medical schools in Sweden, each of them associated with one of the seven tertiary care university hospitals.
The study was performed in Region Västra Götaland, an area in the south-west of Sweden with 1.7 million inhabitants. Inpatient- and specialized health care is provided by Sahlgrenska University Hospital in Gothenburg and three large county hospitals and several smaller. The hospitals range in size from a small 90 bed hospital to a large 2300 bed tertiary care university hospital. All hospitals within the region are through an agreement between the Swedish state, Region Västra Götaland and University of Gothenburg affiliated with the medical school at Sahlgrenska Academy, University of Gothenburg and are through the agreement, required to assist with clinical supervision for medical students. Thus, students do clinical rotations at all hospitals and most primary care units in the region. At each hospital department, there is a physician responsible for the medical students who takes part in faculty meetings at the university. The frequency of visits from faculty to the hospital units vary between courses. There are no formal requirements or certifications for teaching medical students, and for most rotations there are no mandatory preparatory supervisor courses. However, all residents in Sweden take a mandatory course in pedagogy as part of their training. The clinical rotations are evaluated by anonymous student course evaluations.
Study design
This survey was designed by the unit for medical education and clinical learning at Sahlgrenska Academy, University of Gothenburg, Sweden. The unit consists of clinical physicians with experience from clinical supervision and senior lecturers from the medical program. The objective of the unit was to evaluate and promote clinical supervision.
Previous qualitative research at Sahlgrenska Academy regarding clinical supervision of medical students was used as a starting point. Factors with potential impact on clinical supervisors’ conditions and preparedness for supervision such as training in medical education, size of student groups and knowledge of the students’ learning objectives had been identified in interviews with clinical supervisors and from analysis of free-text questions in smaller surveys [27,28,29,30].
Using these themes, we developed a quantitative pilot survey with questions on the supervisors’ education and preparation, if they were familiar with the students’ learning objectives, self-perceived pedagogical knowledge and characteristics of the learning environment. To further investigate the perspective of the clinical supervisors, the survey ended with an open free-text question; “What can facilitate your task as a clinical supervisor?”, not reported in this study. The pilot survey was sent to all potential clinical supervisors working in internal medicine. Total number of recipients was 545 of which 265 responded (48% response rate).
The results from the pilot survey were used to finalize a larger survey. The list with courses in supervision or pedagogy was updated. As emails were described as an important way to receive information by several respondents, a question on receiving emails was added. Finally, questions using Likert scales were changed from five to six steps to enable equal dichotomization for analysis. Table 1 shows the questions and the answer alternatives of the final survey we used in this study.
Survey distribution
Email addresses to all physicians employed at the hospitals in Region Västra Götaland were obtained from the regional employee registry. Physicians working at units without clinical rotations of medical students were excluded. The survey was distributed digitally 2018-10-16, using the digital survey tool ESMAKER [31].
Two reminders were sent by e-mail and the survey was closed 2018-12-09. The Esmaker survey system works with completely anonymised recipients. This means that it is not possible to link survey responses to receiving e-mail addresses or to be able to see afterwards which of the recipients responded to the survey. The system ensures that only one response per e-mail address can be registered.
Ethics
The research was carried out in accordance with guidelines and regulations stipulated in the Declaration of Helsinki. The study protocol was reviewed by the Swedish Ethical Review Authority (Reference number 2021 − 00859). According to the assessment, formal ethical approval was deemed unnecessary according to the Swedish law in §§ 3–4 of the act concerning the Ethical Review of Research Involving Humans (SFS 2003:460). Participants received written information about the aims of the study together with the electronic survey, the information included the information that the results from the survey could be used in a scientific study. Participation was voluntary and given that the survey was completely anonymous, and no personal data was collected or analysed, the study is exempted from direct informed consent according to the Swedish law concerning personal data (PUL 1998:204 3 §).
Statistics
Responses to the questions using a six-point Likert scale were dichotomized by merging categories strongly agree / agree / slightly agree to “agree” and strongly disagree / disagree / slightly disagree to “disagree” [32, 33]. Differences between university hospital and non-university hospital supervisors’ responses in the proportion responding “agree” were tested for statistically significance using the χ2 test.
Two survey items were chosen as outcome measures indicating that the supervisor was prepared for their teaching assignment: “I feel that I have enough pedagogical knowledge to carry out my educational assignment.” and “I am familiar with the current learning objectives of the clinical placement “. All other questions were considered as potential factors associated with the outcome measures.
To investigate the association between the potential factors and the outcome measures we used logistic regression to calculate odds ratio of each potential factor for the two outcomes separately. A p-value ≤ 0.05 was considered statistically significant.
Results
The survey was distributed to 3920 physicians.1732 surveys were completed resulting in a response rate of 43%. Of those, 730 reported that they had not been active as clinical supervisors in the previous semester and were excluded. Thus, a total of 1002 respondents were included in the final analysis.
Characteristics of the clinical supervisor
The demographics of the participating physicians are described in Table 2. Of the 1002 respondents, 54% were consultants and 48% were working at non-university hospitals in the region. Most respondents were physicians engaged in the faculty courses “internal medicine” and “surgery”. There was a higher proportion of supervisors before residency in the non-university hospitals.
Preparatory supervisor training
In total, 40% of respondents reported that they had attended preparatory supervisor training. The rate was significantly higher for supervisors working at the university hospital compared to those working at non-university hospitals (Table 3). One small subgroup, 12% of respondents, reported that they had attended two or more preparatory supervisor training courses.
Knowledge of the training assignment
Familiarity with the students learning objectives was reported by 69% of respondents and 78% reported that they felt that they had enough pedagogical knowledge to supervise. Both rates were significantly higher for physicians at university hospitals compared to physicians at non-university hospitals. Receiving emails from course management was reported by 42% of respondents and 29% reported that course management had visited their workplace. Again, both rates were significantly higher for physicians at university hospitals compared to physicians at non-university hospitals (Table 3).
Supervisors’ clinical workload and support
The number of students supervised at the same time per clinical supervisor, was slightly higher in university hospital compared to non-university hospitals. Most supervisors were responsible for one to two students at the same time. A majority (74%) of respondents reported that they had no reduction in clinical workload while supervising students and a minority (38%) perceived that they had sufficient time for their task. These proportions did not differ significantly between respondents from university and non-university hospitals (Table 4). Scheduled meetings focused on teaching and learning were reported by 23% with a significantly higher frequency in the university hospital compared to the non-university hospitals (Table 3).
Factors associated with supervisors’ preparedness to teach
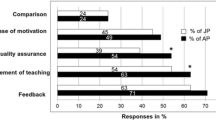
All investigated factors showed significant association with both outcomes chosen as measures for supervisors’ preparedness to teach (Figs. 1 and 2). For the outcome “I feel that I have enough pedagogical knowledge to carry out my educational assignment”, the question “I feel that goal description and written information from the course management is sufficient for me to be able to complete the training assignment” showed the highest odds ratio (OR 7.7 (95% CI 5.4–11.0), followed by “I am familiar with the current learning objectives of the clinical placement” (OR 5.8 (95% CI 4.2–8.1) (Fig. 1). For the outcome “I am familiar with the current learning objectives of the clinical placement”, the question “I have read the syllabus or other written tutor information from the course management for the current course” showed the highest odds ratio (OR 24.8 (95% CI 15.9–38.8) followed by “I feel that goal description and written information from the course management is sufficient for me to be able to complete the training assignment” (OR 13.1 (95% CI 9.4–18.2) (Fig. 2).
“I feel that I have enough pedagogical knowledge to carry out my educational assignment.” Odds ratios and 95% confidence intervals for variables with respondents reporting agree to the statement. Odds ratios with factor present (yes/agree) compared to factor not present, ranked by strength of association
Discussion
In this quantitative survey with responses from clinical supervisors at university and non-university hospitals, we found that most supervisors felt that they were prepared for their teaching assignment. However, one third of the respondents reported that they were not familiar with the learning objectives. We found consistent differences between supervisors at university and non-university hospitals with respect to preparatory supervisor training, knowledge of the training assignment and support.
We confirm findings from the same context in previous qualitative research that several facilitating factors are associated with supervisors self-perceived readiness to teach [27,28,29,30]. Especially interaction between faculty and supervisors, through visits to the workplace or emails, and local support to the supervisors showed high odds ratios both for reported knowledge of learning objectives and self-perceived pedagogical knowledge.
General findings
Although eight of ten respondents reported that they felt that they had enough pedagogical knowledge to carry out their educational assignment, only four in ten had participated in preparatory supervisor training. Consistent with previous findings from qualitative studies, we found a lower degree of participation in supervisor training for clinicians at non-university hospitals [12]. To some extent this difference can be explained by university hospitals having a significantly higher percentage of consultants compared to non-university hospitals. Concerns have been raised in previous research that supervisors without supervisor training tend to rely on various personal teaching methods and lack clear methods for evaluation [34].
Despite seven of ten respondents reporting that they were familiar with the learning objectives, less than half of respondents reported that they had read the syllabus or other written tutor information from the course management. It is possible that some of the supervisors who believe they are familiar with the learning objectives despite not having read them overestimate their understanding. Supervisors not knowing what the learning objectives are for the clinical rotation where they are supervising has been reported by students in previous research [35]. As the syllabus and learning objectives are central in how course management can influence what and how the students are taught, it is important that they are well known by the clinical supervisors [20, 21]. This finding suggests that further efforts need to be made to ensure that all supervisors are aware of the learning objectives.
Factors that support clinicians to be prepared as clinical supervisors for medical students
Our results identified a variety of factors that associated with supervisors’ preparedness to teach. Supervisors that had received visits from course management and/or emails, were more likely to agree that they had enough pedagogical knowledge to carry out their educational assignment. These supervisors also reported that they were familiar with the learning objectives. From a faculty perspective the findings suggest that interaction between faculty and supervisors is crucial. It follows that recurring visits from faculty used in some decentralized medical schools can be an effective way to support the supervisors [36]. In addition, emails sent to all supervisors each semester can be a cost-effective strategy to increase the supervisors’ knowledge of learning objectives and confidence to teach.
Taking the perspective of the hospital unit as a clinical learning environment presents another viewpoint [37, 38]. Several organizational aspects were associated with the supervisors’ preparedness to teach. Support from the person at the clinic responsible for the medical students, organized support for supervisors along with regular teacher meetings were all associated with supervisors´ reports of being prepared. This highlights the need to develop local communities of practice where education is in focus [16, 39]. Members of the faculty and individuals in the hospital setting dedicated to education, sometimes called local champions, can help bridge the gap between academy and healthcare [40, 41]. Efforts to empower and support the champions enables them in turn to support the clinical supervisors.
Preparatory supervisor training was associated both with self-assessed pedagogical knowledge and familiarity with learning objectives. However, it had a lower odds ratio than interaction with faculty through emails and visits. The finding suggests that supervisor training requires more focus in the specific context where the supervisor is involved and needs to include details on the learning objectives.
Clinical workload
Most supervisors did not get a reduced clinical workload when they were supervising students. A majority felt that they did not get enough time set aside for their educational assignment. Lack of time to teach is a returning theme in previous studies of clinical supervisors teaching experience and can potentially impact the students learning opportunities [9, 10, 28, 29, 42, 43]. Our finding highlights the constant conflict of interest where training of students often competes with a primary objective of providing healthcare to the patients. As time constraints most likely will remain a challenge to clinical supervision, time management skills are crucial for the supervisors. There are examples of scheduling patients in out-patient care in a way that allows a supervisor to manage two students without a reduction in number of patients seen [44, 45]. Pedagogical models using entrusted professional activities, where students gradually are entrusted to perform tasks in the clinical environment can also serve as a way to shift some of the clinical workload from the supervisor to the student [46,47,48]. Strategies that can facilitate integration of clinical supervision in clinical practise without a need to reduce clinical workload are crucial to establish.
Content of clinical placements
Surprisingly, less than a third of respondents reported that they felt that the clinical placement had a content that allowed students to achieve their learning goals and only four of ten reported that they found the clinical placement long enough for students to achieve their learning objectives. This result may reflect that those supervisors are not familiar with the actual learning objectives of the clinical placement. However, it may also reflect a mismatch between expectations from the faculty and the actual learning opportunities the clinical learning environment can provide. From a constructive alignment perspective, it illustrates a challenge in course design where learning objectives need to align with the students learning activities [20, 21]. The findings suggest that clinical supervisors need to understand the learning objectives and more importantly how the objectives can be achieved during the clinical rotation.
Differences between university and non-university hospitals in how clinical supervisors are prepared for their task
We found supervisors working at university hospitals generally rating slightly higher on the items investigating how they were prepared to teach. Significant differences could be seen when it came to course faculty’s interaction with the supervisors. Part of the difference may be explained by a higher fraction of supervisors being specialists in the university hospital. The findings indicate that more efforts are needed to ensure that supervisors at non-university hospitals are familiar with the learning objectives. Interestingly, at the non-university hospitals, there was a significantly higher number of supervisors who reported a reduction in clinical assignments during periods with educational assignments.
Strengths and limitations
This study was distributed to all clinical supervisors supervising medical students from a university with clinical rotation at multiple hospitals. It adds new knowledge on how clinical supervisors are prepared for their teaching assignment and allows comparison between supervisors at university and non-university hospitals teaching students from the same university. Our results are limited to the educational context of a Swedish university with regionalised medical education. However, the results conform with previous qualitative research which indicates that it can be used to better prepare clinical supervisors working under similar conditions at other universities. Our study has some further limitations. The response rate to the survey was 43%, making it difficult to say with certainty that the results apply to the whole population. There is also a need to be aware that this a cross sectional study, and associations should be interpreted with caution as we cannot make inferences with respect to causality. Finally, self-perceived preparedness is not a perfect measure of actual ability to teach and further studies investigating the supervisors’ actual abilities and knowledge of learning objectives is needed to confirm our findings.
Conclusions
In conclusion we found that supervisors’ self-perceived preparedness was associated with familiarity with the learning objectives, faculty involvement through visits to their workplace and emails as well as local organizational support. We found consistent differences between supervisors at university and non-university hospitals with respect to preparatory supervisor training, knowledge of the training assignment and support.
This implicates that when students are sent to non-university hospitals, it is crucial to ensure that the new clinical supervisors are prepared for their assignment. In this process, communicating the learning objectives is central.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author in response to reasonable requests.
References
OECD. (2021), Hospital beds (indicator). https://data.oecd.org/healtheqt/hospital-beds.htm. Accessed 22 Dec 2021.
World Bank. Hospital beds (per 1,000 people). https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?end=2011locations=SEstart=1960view=chart(http://ec.europa.eu/eurostat/tgm/table.do?tab=tableinit=1plugin=1pcode=tps00046language=en). Accessed 20 Jan 2022.
eurostat. Hospital beds Per 100 000 inhabitants. http://ec.europa.eu/eurostat/tgm/table.do?tab=table&init=1&plugin=1&pcode=tps00046&language=en. Accessed 20 Jan 2022.
Universitetskanslerämbetet. Antagna till yrkesexamenprogram. https://www.uka.se/statistik--analys/hogskolan-i-siffror/utbildning-pa-grundniva-och-avancerad-niva.html Accessed 20 Jan 2022.
Farnsworth TJ, Frantz AC, McCune RW. Community-based distributive medical education: Advantaging Society. Med Educ Online. 2012;17:1–10.
Cheifetz CE, McOwen KS, Gagne P, Wong JL. Regional Medical campuses. Acad Med. 2014. https://doi.org/10.1097/ACM.0000000000000295.
Trede F, Sheehan D, Mcewen C. Investigating what constitutes an effective workplace learning environment: a scoping review of the role physical and material elements play in student learning. J Coop Educ Internships. 2013;47.
Alsiö Å, Wennström B, Landström B, Silén C. Implementing clinical education of medical students in hospital communities: experiences of healthcare professionals. Int J Med Educ. 2019;10:54–61.
Hanlon N, Ryser L, Crain J, Halseth G, Snadden D. Establishing a distributed campus: making sense of disruptions to a doctor community. Med Educ. 2010;44:256–62.
Hägg-Martinell A, Hult H, Henriksson P, Kiessling A. Medical students’ opportunities to participate and learn from activities at an internal medicine ward: an ethnographic study. BMJ Open. 2017;7.
Cantillon P, D’Eath M, De Grave W, Dornan T. How do clinicians become teachers? A communities of practice perspective. Adv Heal Sci Educ. 2016;21:991–1008.
MacDougall J, Drummond MJ. The development of medical teachers: an enquiry into the learning histories of 10 experienced medical teachers. Med Educ. 2005;39:1213–20.
Stone S, Ellers B, Holmes D, Orgren R, Qualters D, Thompson J. Identifying oneself as a teacher: the perceptions of preceptors. Med Educ. 2002;36:180–5.
Steinert Y. Faculty development: on becoming a medical educator. Med Teach. 2012;34:74–6.
Hartford W, Nimmon L, Stenfors T. Frontline learning of medical teaching: you pick up as you go through work and practice. BMC Med Educ. 2017;17:1–10.
Page S, Birden H. Twelve tips on rural medical placements: what has worked to make them successful. Med Teach. 2008;30:592–6.
Christner JG, Dallaghan GB, Briscoe G, Casey P, Fincher RME, Manfred LM, et al. The Community Preceptor Crisis: recruiting and Retaining Community-based Faculty to teach Medical Students—A Shared Perspective from the Alliance for Clinical Education. Teach Learn Med. 2016;28:329–36.
Chatterjee D, Corral J. The Journal of Education in Perioperative Medicine how to write well-defined learning objectives. J Educ Perioper Med. 2017;XIX:1.
Mather CA, McKay A, Allen P. Clinical supervisors’ perspectives on delivering work integrated learning: a survey study. Nurse Educ Today. 2015;35:625–31.
Biggs J, Tang C. Teaching for Quality Learning at University: What the Student Does (3rd Edition). Buckingham, GBR: Open University Press; 2007.
Biggs J. What the Student does: teaching for enhanced learning. High Educ Res Dev. 1999;18:57–75.
Anderson LW. Rethinking Bloom’s taxonomy: implications for testing and assessment. Educ Resour Inf Cente. 1999;:1–25.
Kilminster S, Cottrell D, Grant J, Jolly B. AMEE Guide No. 27: effective educational and clinical supervision. Med Teach. 2007;29:2–19.
Hudak NM, Stouder A, Everett CM. A program’s analysis of communication methods with clinical preceptors. J Physician Assist Educ. 2018;29:39–42.
Morrison EH, Shapiro JF, Harthill M. Resident doctors’ understanding of their roles as clinical teachers. Med Educ. 2005;39:137–44.
Leslie K, Baker L, Egan-Lee E, Esdaile M, Reeves S. Advancing faculty development in medical education: a systematic review. Acad Med. 2013;88:1038–45.
Von Below B, Haffling AC, Brorsson A, Mattsson B, Wahlqvist M. Student-centred GP ambassadors: perceptions of experienced clinical tutors in general practice undergraduate training. Scand J Prim Health Care. 2015. https://doi.org/10.3109/02813432.2015.1041826.
von Below B, Rödjer S, Mattsson B, Hange D, Wahlqvist M. What factors motivate junior doctors to engage as clinical tutors? A qualitative study. Int J Med Educ. 2018;9:151–7.
Von Below B, Rödjer S, Wahlqvist M, Billhult A. I couldn’t do this with opposition from my colleagues: a qualitative study of physicians’ experiences as clinical tutors. BMC Med Educ. 2011. https://doi.org/10.1186/1472-6920-11-79.
Von Below B, Hellquist G, Rödjer S, Gunnarsson R, Björkelund C, Wahlqvist M. Medical students’ and facilitators’ experiences of an early professional contact course: active and motivated students, strained facilitators. BMC Med Educ. 2008. https://doi.org/10.1186/1472-6920-8-56.
Esmaker. https://entergate.se/products/esmaker/.
Rungson Chomeya. Quality of psychology test between Likert Scale 5 and 6 points. J Soc Sci. 2010;6:399–403.
Swift L, Miles S, Leinster SJ. The analysis and reporting of the Dundee Ready Education Environment Measure (DREEM): some informed guidelines for evaluators. Creat Educ. 2013;04:340–7.
Biku T, Demas T, Woldehawariat N, Getahun M, Mekonnen A. The effect of teaching without pedagogical training in st. Paul’s hospital millennium medical college, Addis Ababa, Ethiopia. Adv Med Educ Pract. 2018;9:893–904.
Sellberg M, Palmgren PJ, Möller R. Balancing acting and adapting: a qualitative study of medical students ’ experiences of early clinical placement. BMC Med Educ. 2022;:1–11.
McGrew M, Solan B, Hoff T, Skipper B. Decentralized medical education in rural communities: the circuit rider connection. Fam Med. 2008.
Laksov KB, Boman LE, Liljedahl M, Björck E. Identifying keys to success in clinical learning: a study of two interprofessional learning environments. J Interprof Care. 2015;29:156–8.
Liljedahl M, Boman LE, Fält CP, Bolander Laksov K. What students really learn: contrasting medical and nursing students’ experiences of the clinical learning environment. Adv Heal Sci Educ. 2015;20:765–79.
Waterval DGJ, Driessen EW, Scherpbier AJJA, Frambach JM. Twelve tips for crossborder curriculum partnerships in medical education. Med Teach. 2018;40:514–9.
De Villiers M, Conradie H, Snyman S, Van Heerden B, Van Schalkwyk S. Experiences in developing and implementing a community-based education strategy - a case study from South Africa. Community Based Educ Heal Prof Glob Perspect. 2014;January:176–206.
Downey LH, Wheat JR, Leeper JD, Florence JA, Boulger JG, Hunsaker ML. Undergraduate Rural Medical Education Program Development: Focus Group Consultation with the NRHA Rural Medical Educators Group. 2011;27:230–8.
GMC. Training environments 2017: Key findings from the national training surveys. 2017.
Kilty C, Wiese A, Bergin C, Flood P, Fu N, Horgan M, et al. A national stakeholder consensus study of challenges and priorities for clinical learning environments in postgraduate medical education. BMC Med Educ. 2017;17:1–9.
Nordin E. Gaffelmottagning ger mer tid till handledning och reflektion för ST-läkare. Sjukhusläkaren. 2022.
Lundin F. Gaffelmottagning - en effektiv inlärningsform för specialist- utbildning i neurologi ? Linköpings Univ. 2022.
Pinilla S, Lenouvel E, Cantisani A, Klöppel S, Strik W, Huwendiek S, et al. Working with entrustable professional activities in clinical education in undergraduate medical education: a scoping review. BMC Med Educ. 2021;21:1–10.
Chen HC, Van Den Broek WES, Ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90:431–6.
Meyer EG, Chen HC, Uijtdehaage S, Durning SJ, Maggio LA. Scoping review of Entrustable Professional activities in Undergraduate Medical Education. Acad Med. 2019;94:1040–9.
Acknowledgements
We wish to thank all clinical supervisors participating in this survey without whom this work would not have been possible.
Funding
No financial relationship to declare.
Open access funding provided by University of Gothenburg.
Author information
Authors and Affiliations
Contributions
The first author, PP (corresponding author), drafted the initial manuscript and was responsible for the data collection. The survey was developed by PP, EH and MW. PP, EH, MW, SN and KJ made equally substantial contributions to the analysis and interpretation of data and finalizing the manuscript. All authors were involved in revising the manuscript critically for important intellectual content, and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was carried out in accordance with guidelines and regulations stipulated in the Declaration of Helsinki. The study protocol was reviewed by the Swedish Ethical Review Authority (Reference number 2021 − 00859). According to the assessment, formal ethical approval was deemed unnecessary according to the Swedish law in §§ 3–4 of the act concerning the Ethical Review of Research Involving Humans (SFS 2003:460). Participants received written information about the aims of the study together with the electronic survey, the information included information about that the results from the survey could be used in a scientific study. Participation was voluntary and given that the survey was completely anonymous, and no personal data was collected or analysed the study is exempted from direct informed consent according to the Swedish law concerning personal data (PUL 1998:204 3 §).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pålsson, P., Hulegårdh, E., Wahlqvist, M. et al. Physicians’ self-perceived preparedness for clinical supervision of medical students at university and non-university hospitals -results from a Swedish survey. BMC Med Educ 23, 914 (2023). https://doi.org/10.1186/s12909-023-04908-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04908-8