Abstracts
Background
Tele-pharmacy is a subset of telemedicine in which pharmacies use telecommunication technology to provide patient care. Tele-pharmacy can improve pharmaceutical care service delivery by reducing medication errors, improving access to health professionals and facilities in remote and rural areas, and minimizing adverse drug events. However, there is limited evidence regarding future pharmacists' knowledge and perceptions of the Tele-pharmacy system in Ethiopia. As a result, this study aimed to assess tele-Pharmacy perception, knowledge and associated factors among pharmacy students in Northwest Ethiopia.
Methods
An institutional-based cross-sectional study was conducted among 376 pharmacy students in Northwest Ethiopia between July 15 and August 27, 2022. A pre-tested self-administered questionnaire was used to collect data. The data were entered using Epi info version 7.0 and analyzed using SPSS version 25. Descriptive statistics, bivariable and multivariable logistic regression analysis were used to describe pharmacy students' knowledge and perceptions of Tele-pharmacy and identify associated factors. An adjusted odds ratio (OR) and a p-value with a 95% confidence interval (CI) were calculated to declare statistical significance.
Results
From a total of 352 participants, about 32.4% with [95% CI (27%-37%)] and 48.6% with [95% CI (43%—54%)] had good knowledge and a positive perception toward Tele-pharmacy, respectively. Being age group of 26–30 (AOR = 0.35, 95% CI: 0.17–0.68), being male (AOR = 2.38, 95% CI: 1.26–4.49), Having a CPGA of > 3.5 (AOR = 2.28, 95% CI: 1.24–4.19), Taking basic computer training (AOR = 2.00, 95% CI: 1.17–3.39), Management support (AOR = 1.84, 95% CI: 1.06–3.19) were found to be significantly associated with pharmacy students' knowledge of Tele-pharmacy. Similarly, having access to electronic devices (AOR = 3.80, 95% CI: 1.81–7.97), training related to pharmacy information systems (AOR = 6.66, 95% CI: 3.34–13.29), availability of guidelines (AOR = 2.99, 95% CI: 1.62–5.50) were found to be significantly associated with pharmacy students' perceptions of Tele-pharmacy.
Conclusion
This study found that pharmacy students have limited knowledge and perceptions of the Tele-pharmacy system. A continuing Tele-pharmacy training package, incorporating pharmacy information system guidelines as part of their education, and providing managerial support could be recommended to improve pharmacy students' knowledge and perception of Tele-pharmacy.
Similar content being viewed by others
Introduction
Telemedicine refers to delivering health care and public education in rural and remote areas [1]. Telemedicine has grown steadily over the last decade as telecommunication technology has advanced and costs have decreased. Tele-pharmacy is a subset of telemedicine in which pharmacies use telecommunication technology to provide patient care [2]. Tele-pharmacy can potentially improve pharmaceutical care service delivery by reducing medication errors and adverse drug events [3]. Furthermore, Tele-pharmacy has the potential to benefit remote and rural areas with limited access to health professionals and facilities [4]. The practical and efficient use of health information technology will be of infinite importance; it will increase pharmacist accessibility, improve patient quality of life and satisfaction with healthcare services, minimize resources, and improve patient clinical outcomes [5].
Pharmacists today want to broaden their profession to provide more services to the rural community while also improving patient outcomes. As a result, Tele-pharmacy services such as medication orders, medication history reviews, dispensing drugs, remote patient consultation, therapeutic drug monitoring, and medication therapy management are becoming more common [6]. These services can be provided using eHealth tools like mobile consultation, software applications, and automated dispensing machines [7].
Pharmacists and student pharmacists should understand the application of telecommunication technology in the pharmacy field to provide the best services. Worldwide there is evidence showing that the proportion of pharmacy student knowledge of tele-pharmacy was 60.3% in the United States [8], 42% in Riyadh city of Saudi Arabia [9], and 67% in Malaysia [4]. Whereas the proportion of perception towards tele-pharmacy was 87% in the University of Tennessee [8], 70.6% in Jordan [10], 61% in Malaysia [4], and 40% in Pakistan [11]. Furthermore, evidences revealed that technological variables and socio-demographic characteristics were discovered to be the determinant factors associated to students' knowledge of and perceptions of the tele-pharmacy system [9,10,11,12].
Tele-pharmacy is one of the best options for providing community-based medication-related healthcare services, allowing pharmacists to address healthcare needs in developing countries like Ethiopia, where health professionals and healthcare facilities are scarce [13]. Furthermore, Tele-pharmacy was the best option for patients living in rural areas to reduce travel distance, save time, and access health care services, particularly for those over the age of 65 and those with disabilities [13, 14].
Ethiopian health sector transformation plan mentioned using health-related information technologies such as Tele-pharmacy as an essential transformation device to improve the quality of health care services [15]. Even though it is widely accepted that tele-pharmacy can help improve access and quality of healthcare delivery when distance is an issue, there is little evidence in Ethiopia about future pharmacists' knowledge and perceptions of tele-pharmacy.
The knowledge and perception of pharmacists students about Tele-pharmacy is a determining factor in the successful implementation of Tele-pharmacy services [16]. Since they play a vital role in the health care system and the functioning of Tele-pharmacy, investigating their knowledge and perception of tele-pharmacy is mandatory [17]. As a result, this study aimed to examine pharmacy students' knowledge and perception of tele-pharmacy.
The result of this study will provide baseline data for policymakers in solving the problem regarding the limited utilization of Tele-pharmacy and improving the knowledge and perception of pharmacy students. It will help them in planning an intervention based on the evidence generated by this study.
Methods
Study settings and design
The study was conducted among pharmacy students at the University of Gondar College of Medicine and Health Science, located in the historic town of Gondar, 726 kms northwest of Addis Abeba. The University of Gondar, formerly known as the Gondar College of Medical Sciences until 2003, is Ethiopia's oldest medical school, founded in 1954 as a Public Health College. It is located in northwest Ethiopia, 726 kms from Addis Ababa, Ethiopia's capital. According to data from the University of Gondar's college of medicine and health science school of pharmacy, 376 students were enrolled in their course. An institutional-based cross-sectional study was used to assess pharmacy students’ knowledge and perception of Tele-pharmacy and the associated factors.
Study population and eligibility criteria
The study was carried out among pharmacy students at the University of Gondar College of Medicine and Health Science. The study included all pharmacy students enrolled in their courses at the University of Gondar College of Medicine and Health Science who were available during the data collection period. However, students who were ill and unable to complete the questionnaire were excluded from this study.
Sample size determination and sampling procedure
There are currently 376 students enrolled in the pharmacy department at the University of Gondar College of Medicine and Health Sciences. The first-year students were not enrolled in the department at the time of data collection. This is because Ethiopia’s current ministry of health schedule requires all natural science students to attend a one-year common course before enrolling in their specific department. In the remaining years, students attended classes in the pharmacy department. There are 51 second-year students, 54 third-year students, 88 fourth-year students, 82 fifth-year students, and 101 post-basic and postgraduate students. Finally, all active pharmacy students in the pharmacy department at the University of Gondar College of Medicine and Health Science (n = 376) were invited to participate in this study.
Study variables
The primary outcome variable of the study was perception and knowledge of Tele-pharmacy. The tools for this study were adapted from a review of related literature [4, 11, 18]. Some independent variables include socio-demographic and technological variables related to Tele-pharmacy perception and knowledge.
Operational definitions
Knowledge of Tele-pharmacy: Ten items with "yes" or "no" responses were used to assess knowledge of Tele-pharmacy. For a total possible score of ten, each correct answer was worth one point, while each incorrect answer was worth zero points. A median of ten questions about Tele-pharmacy Knowledge was calculated. Those who scored higher than the median value were thought to have "Good knowledge about Tele-pharmacy," while those who scored a median value and lower were supposed to have "Poor knowledge about Tele-pharmacy" [4, 18].
Perception towards Tele-pharmacy was assessed using a 5-point Likert scale ranging from "strongly disagree" (score 1) to "strongly agree" (score 5). A median of 14 questions about Perception toward Tele-pharmacy was calculated. Those who scored higher than the median value were thought to have a "Good perception of Tele-pharmacy," while those who scored a median value and lower were supposed to have a "Poor perception of Tele-pharmacy” [4, 11, 18].
Data collection procedure and quality control
A structured, pre-tested, and self-administered questionnaire was used to collect data. Six health information technology professionals collected the required data, And Two health informatics professionals with master's degrees and research experience oversaw the data collection. The principal investigators provided training for data collectors and supervisors two days before the start of data collection. Supervisors strictly supervised the data collection process and provided regular onsite advice and feedback to data collectors. The principal investigators and supervisor exchanged information face-to-face daily.
Before data collection, a pre-test was conducted on 10% of the sample size among pharmacy students at Bahirdar University. The questionnaire was checked for clarity, simplicity, understandability, completeness, consistency, and coherency during the pre-testing. Appropriate corrections were taken on time for completeness and accuracy before the beginning of data collection. The pre-test results were also used to assess the internal consistency of the questionnaire. Cronbach's alpha was used to determine the internal validity of the data collection instrument, and the scores on knowledge and perception of Tele-pharmacy were 0.86 and 0.98, respectively.
Data processing and analysis
The collected data were entered into Epi info version 7.0 and transferred into SPSS version 25.0 software for further analysis. A table, graph, and text were used to present descriptive statistics. A bivariable logistic regression analysis was performed to determine each study variable's effect on the outcome variable. Variables with a p-value of 0.2 in the bivariate analysis would be entered into a multivariable logistic regression analysis to check for confounding effects on the bivariate analysis's association. The strength of the association would be determined using a 95% confidence interval odds ratio, and a p-value less than 0.05 would be considered a significant variable. The model was fitted with p = 0.34 according to homer's goodness of fit test, multi-collinearity was checked between independent variables, and all variance inflation factors were less than 3.
Results
Socio-demographic characteristics of participants
A total of 352 study subjects participated, with a response rate of 93.62%. The mean age of the study participants was 24.26 with an SD ± 3.419 years with ranges from 20 to 37 years. About 259 (73.6%) of the respondents were in the age category of 20–25. The majority, 274(77.8%) of the participants, were male, and 295 (83.8%) were single. Regarding religion, around 286 (81.3%) of the study participants were Orthodox, and 93 (26.4%) were post-basic and postgraduate students Table 1.
Technological and organizational characteristics
More than two-thirds of pharmacy students, 286 (81.3%), have access to one of the electronic devices, with the majority of respondents, 203 (57.7%), having access to smartphones. The findings show that approximately 207 (58.8%) of study participants did not receive basic computer training, and only half, 178 (50.6%) of the study participants, had sufficient skill to use computer systems, enabling them to use the Tele-pharmacy system. The majority of respondents, 298 (84.7%), said they had internet access in their learning environment, and roughly three-fourths, 210 (59.7%), said they used the internet to access health-related information.
Most of the 260 (73.9%) pharmacy students did not receive training in pharmacy information systems. Furthermore, more than two-thirds of 237 (67.3%) reported no pharmacy information system implementation guideline, and approximately 262 (74.4%) reported a lack of management support from their department to implement a Tele-pharmacy system Table 2.
Pharmacy student’s knowledge regarding Tele-pharmacy
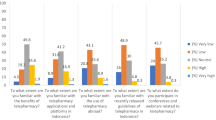
Of the study participants, 114 (32.4% CI = 27%-37%) had adequate knowledge of the Tele-pharmacy system (Fig. 1. More than three-quarters, 304(86.4%) of the participants stated that they are unaware of Tele-pharmacy systems in Ethiopia. Approximately 277 (78.7%) of participants agreed that pharmacists should know about information and communication technology to practice Tele-pharmacy.
Approximately 80% of participants believed that tele-pharmacy played a significant role in outbreaks worldwide. The majority of 283 (80.4%) of the study participants agreed that Tele-pharmacy provides better counseling in terms of privacy and length of the session, Table 3.
Pharmacy student’s perception of Tele-pharmacy
Of the total study participants, 171 (48.6% CI = 43%—54%) had a positive perception of Tele-pharmacy Fig. 1. Table 4 illustrates that about 195(55.4%) agreed that Tele-pharmacy can help patients save their money and travel time to reach healthcare facilities. The majority of 245(69.6%) of the study participants agreed that Tele-pharmacy could minimize the cost of establishing a pharmaceutical business compared to a regular pharmacy. Moreover, about 216(61.4) of the study participants agreed that pharmacy schools should provide education programs on computers, IT, and Tele-pharmacy to assist in the future utilization of Tele-pharmacy Table 4.
Factors associated with pharmacy students’ knowledge about Tele-pharmacy
Bivariate and multivariable analyses were used to investigate the factors associated with students' knowledge of Tele-pharmacy. In a bivariate analysis, the candidate variables for the multivariable logistic regression analysis were Sex, Age, Student’s grade (CPGA), Training related to pharmacy information systems, Device access, Basic computer training, computer skill, internet access, availability of pharmacy information system implementation guidelines, and management support to implement a pharmacy information system.
According to the findings of multivariable logistic regression analysis, being age group of 26–30 (AOR = 0.35, 95% CI: 0.17–0.68), being male (AOR = 2.38, 95% CI: 1.26–4.49), Having a CPGA of > 3.5 (AOR = 2.28, 95% CI: 1.24–4.19), Taking basic computer training (AOR = 2.00, 95% CI: 1.17–3.39), Management support to implement pharmacy information system (AOR = 1.84, 95% CI: 1.06–3.19) were found to be significantly associated with knowledge towards tele-pharamcy among pharmacy students Table 5.
Factors associated with pharmacy students’ perception of Tele-pharmacy
Based on the multivariable logistic regression analysis in Table 5, Having access to electronic devices (AOR = 3.80, 95% CI: 1.81–7.97), training related to pharmacy information systems (AOR = 6.66, 95% CI: 3.34–13.29), availability of pharmacy information system implementation guideline (AOR = 2.99, 95% CI: 1.62–5.50) were found to be significantly associated with perception towards Tele-pharmacy among pharmacy students Table 6.
Discussion
The finding of this study revealed that 32.4% (95% CI = 27%-37%) of pharmacy students had adequate knowledge regarding telepharmacy. The result of this study is lower as compared with studies conducted in Malaysia 67% [4], Saudi Arabia 42% [19], and the United States of America 60% [8]. The significant disparity could be attributed to the fact that developing countries use fewer eHealth applications than middle-income and developed countries [20, 21]. Because of the lower use of Tele-pharmacy in developing countries, such as Ethiopia, there is a significant knowledge gap between developed and developing countries. Another reason for the disparity could be country-specific differences in information and communication technology infrastructure and socioeconomic status [22].
In this study, 48.6% (95% CI = 43%—54%) of pharmacy students had a favorable perception of the Tele-pharmacy system. This finding is lower as compared with a study conducted in Malaysia with 61% [4], Saudi Arabia with 87% (11), Jordan 70.6% [10], and the United States 87% [8]. This could be due to technological advancement and ICT infrastructure differences between countries. Furthermore, the difference could be due to differences in educational curricula between countries; for example, in Ethiopia, pharmacy students only take fundamentals of health informatics courses. As a result, delivering an eHealth application course that includes Tele-pharmacy as part of their educational curriculum is highly recommended.
This research also found factors associated with pharmacy students' knowledge and perception of the Tele-pharmacy system.
Among the factors associated with knowledge, students in older age groups were 65% less likely to have sufficient knowledge of tele-pharmacy compared to students in younger age groups. This outcome is consistent with past research that showed younger students had a higher comprehension of health information technologies [23,24,25]. This was explained by the fact that most university students in the Ethiopian were under the age of 25, and younger students were more active in using and accessing information and communication technology [26].
This study found that male respondents were 2.38 times more likely to have adequate knowledge about Tele-pharmacy than females. Other research has also found that men understand eHealth applications better than women [27,28,29]. The digital divide could explain the difference and gender inequality in access to technology continue to be challenging in low-income countries like Ethiopia. This implied that female students would receive more attention to improve their understanding of eHealth applications. Moreover, students Having a CPGA of > 3.5 were 2.28 times more likely to have adequate knowledge of the Tele-pharmacy system. This was explained by the fact that students with higher CPGA were more likely to understand the Tele-pharmacy system than students with lower CPGA.
Pharmacy students who took training on a basic computer were 2.00 times more likely to have adequate knowledge of Tele-pharmacy than students who did not receive basic computer training. This study's findings are consistent with previous research indicating that computer training can improve understanding of the Telehealth applications [30,31,32]. This is because basic computer training is the most critical factor in improving students' knowledge of Tele-pharmacy [33]. This implies that computer training is an integral part of successful Tele-pharmacy adoption. Furthermore, those with management support were 1.84 times more likely to have good knowledge of Tele-pharmacy than those who did not have management support. This implies that health administrators should pay attention and provide ongoing support to future pharmacists to understand better and implement a Tele-pharmacy system.
Among the factors significantly associated with pharmacy students' perceptions of Tele-pharmacy, having access to electronic devices was 3.80 times more likely to have a positive perception than not having access to electronic devices. Previous research backs up this evidence that having access to electronic devices is the most critical factor in having a positive perception of the Telemedicine system [34, 35]. This implied that access to electronic devices was required to implement Ethiopia's Tele-pharmacy system successfully.
Those who received pharmacy information system training were 6.66 times more likely to have a positive perception of the Tele-pharmacy system than those who did not receive pharmacy technology training. This is because students who have received training in pharmacy technology may have a favorable opinion of the Tele-pharmacy system [10, 36]. Furthermore, the availability of pharmacy information system implementation guidelines was linked to a positive perception of the Tele-pharmacy system. Those with guidelines on pharmacy information system implementation were 2.99 times more likely to have a positive perception of Tele-pharmacy than their counterparts. This implies that health managers should prepare a user manual when planning to implement Telehealth applications in the Ethiopian healthcare system.
Conclusion and recomendation
This study found that pharmacy students have limited knowledge and perceptions of the Tele-pharmacy system. A continuing Tele-pharmacy training package, incorporating pharmacy information system guidelines as part of their education, and providing managerial support could be recommended to improve pharmacy students' knowledge and perception of Tele-pharmacy. Based on the findings, policymakers and other stakeholders can develop a plan to implement Tele-pharmacy in the health care system.
Strength and limitations of the study
This study is unique in Ethiopia because it discovered future pharmacists' knowledge and perceptions of Tele-pharmacy. However, the study has some limitations. The study's findings could be influenced by response bias. However, we attempted to reduce this bias by improving survey designs through pre-testing feedback.
Availability of data and materials
This article includes all the data generated and analyzed during this study.
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence Interval
- COR:
-
Crude odds ratio
- ADR:
-
Adverse drug reaction
- e-Health:
-
Electronic health
- ICT:
-
Information communication technology
- SPSS:
-
Statistical package for social science
References
Wootton R. Telemedicine BMJ. 2001;323(7312):557–60.
Angaran DM. Telemedicine and telepharmacy: Current status and future implications. Am J Health Syst Pharm. 1999;56(14):1405–26.
Petropoulou S, Bekakos M, Gravvanis G, editors. E-prescribing-Telepharmacy. 7th Hellenic European Conference on Computers; 2005: Citeseer.
Elnaem MH, Akkawi ME, Al-Shami AK, Elkalmi R. Telepharmacy knowledge, perceptions, and readiness among future Malaysian pharmacists amid the COVID-19 pandemic. Ind J Pharm Educ Res. 2022;56(1):09–16.
Belay TS. Utilization of Telemedicine in Tikur Anbessa Specialized Hospital, Addis Ababa. Ethiopia: Addis Ababa University; 2013.
Baldoni S, Amenta F, Ricci G. Telepharmacy services: present status and future perspectives: a review. Medicina. 2019;55(7):327.
Keeys C, Kalejaiye B, Skinner M, Eimen M, Neufer J, Sidbury G, et al. Pharmacist-managed inpatient discharge medication reconciliation: a combined onsite and telepharmacy model. Am J Health Syst Pharm. 2014;71(24):2159–66.
Patel K. Assessment of Knowledge, Attitude, Perception of Pharmacy Students Towards Telepharmacy. Applied Research Projects. 2021;75. https://doi.org/10.21007/chp.hiim.0072, https://dc.uthsc.edu/hiimappliedresearch/75.
Dat TV, Tran TD, My NT, Nguyen TTH, Quang NNA, Tra Vo Nguyen M, et al. Pharmacists’ Perspectives on the Use of Telepharmacy in Response to COVID-19 Pandemic in Ho Chi Minh City, Vietnam. J Pharm Tech. 2022;38(2):106–14.
Muflih SM, Al-Azzam S, Abuhammad S, Jaradat SK, Karasneh R, Shawaqfeh MS. Pharmacists’ experience, competence and perception of telepharmacy technology in response to COVID-19. Int J Clin Pract. 2021;75(7):e14209.
Muhammad K, Baraka MA, Shah SS, Butt MH, Wali H, Saqlain M, et al. Exploring the perception and readiness of Pharmacists towards telepharmacy implementation; a cross sectional analysis. PeerJ. 2022;10:e13296.
Umayam KAD, Rosadia ANN, Tan RNR, Salazar DJR, Masakayan RLL, Santiago GMB, et al. Knowledge, Attitudes and Perceptions on the Use of Telemedicine Among Adults Aged 18–34 in Manila, Philippines During the COVID-19 Pandemic. J Med Univ Santo Tomas. 2022;6(1):858–67.
Win AZ. Telepharmacy: Time to pick up the line. Res Social Adm Pharm: RSAP. 2017;13(4):882–3.
Poudel A, Nissen LM. Telepharmacy: a pharmacist’s perspective on the clinical benefits and challenges. Integr Pharm Res Pract. 2016;5:75.
Seboka BT, Yilma TM, Birhanu AY. Factors influencing healthcare providers’ attitude and willingness to use information technology in diabetes management. BMC Med Inform Decis Mak. 2021;21(1):1–10.
Ameri A, Salmanizadeh F, Keshvardoost S, Bahaadinbeigy K. Investigating pharmacists’ views on telepharmacy: prioritizing key relationships, barriers, and benefits. J Pharm Technol. 2020;36(5):171–8.
Ayatollahi H, Sarabi FZP, Langarizadeh M. Clinicians’ knowledge and perception of telemedicine technology. Perspect Health Inf Manag. 2015;12(Fall):1c.
Tjiptoatmadja NN, Alfian SD. Knowledge, Perception, and Willingness to Use Telepharmacy Among the General Population in Indonesia. Front Public health. 2022;10:825554.
Alanazi A, Albarrak A, Muawad R. 5PSQ-184 Knowledge and attitude assessment of pharmacists toward telepharmacy in Riyadh City. Saudi Arabia: British Medical Journal Publishing Group; 2021.
Kirigia JM, Seddoh A, Gatwiri D, Muthuri LH, Seddoh J. E-health: determinants, opportunities, challenges and the way forward for countries in the WHO African Region. BMC Public Health. 2005;5(1):1–11.
Quaglio G, Dario C, Karapiperis T, Delponte L, Mccormack S, Tomson G, et al. Information and communications technologies in low and middle-income countries: Survey results on economic development and health. Health Policy Technol. 2016;5(4):318–29.
Mekuria F, Nigussie EE, Dargie W, Edward M, Tegegne T. Information and Communication Technology for Development for Africa: First International Conference, ICT4DA 2017, Bahir Dar, Ethiopia, September 25–27, 2017, Proceedings: Springer; 2018.
Alwan K, Ayele TA, Tilahun B. Knowledge and utilization of computers among health professionals in a developing country: a cross-sectional study. JMIR Hum Factors. 2015;2(1):e4184.
Tegegne MD, Endehabtu BF, Klein J, Gullslett MK, Yilma TM. Use of social media for COVID-19-related information and associated factors among health professionals in Northwest Ethiopia: A cross-sectional study. Digital Health. 2022;8:20552076221113390.
Shiferaw KB, Mehari EA. Internet use and eHealth literacy among health-care professionals in a resource limited setting: a cross-sectional survey. Adv Med Educ Pract. 2019;10:563.
Engel A, Salvador CC, Membrive A, Badenas JO. Information and communication technologies and students’ out-of-school learning experiences. Digital Education Review. 2018;33:130–49.
Jain R, Dupare R, Bhanushali N, Kumar V. Knowledge and utilization of computer among health-care professionals in Mumbai. J Indian Assoc Public Health Dentist. 2020;18(1):97.
Kay R. Addressing gender differences in computer ability, attitudes and use: The laptop effect. J Educ Computing Res. 2006;34(2):187–211.
Shiferaw KB, Tilahun BC, Endehabtu BF. Healthcare providers’ digital competency: a cross-sectional survey in a low-income country setting. BMC Health Serv Res. 2020;20(1):1–7.
Weldegebrial TT, Berhie G. Telehealth in Ethiopia–The Barriers Vs. The Success Factors. Marshall University. 2017;2016.
Tegegne MD, Wubante SM. Identifying barriers to the adoption of information communication technology in ethiopian healthcare systems. a systematic review. Adv Med Educ Pract. 2022;13:821.
Wubante SM, Tegegne MD. Health professionals knowledge of telemedicine and its associated factors working at private hospitals in resource-limited settings. Front Digit Health. 2022;4:976566.
Aruru M, Truong H-A, Clark S. Pharmacy Emergency Preparedness and Response (PEPR): a proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res Social Adm Pharm. 2021;17(1):1967–77.
Sagaro GG, Battineni G, Amenta F. Barriers to sustainable telemedicine implementation in Ethiopia: A systematic review. Telemed Rep. 2020;1(1):8–15.
Biruk K, Abetu E. Knowledge and attitude of health professionals toward telemedicine in resource-limited settings: a cross-sectional study in North West Ethiopia. J Healthc Eng. 2018;2018:2389268.
Francis SG. Pharmacists’ Perceptions About the Effect of Work Environment Factors on Patient Safety in Large-Chain Retail Pharmacies. J Pharm Technol. 2022;38(6):376–8. https://doi.org/10.1177/87551225221116000.
Acknowledgements
First, I thank the University of Gondar for allowing us to conduct this research. My thanks also go to the pharmacy department at the University of Gondar College of Medicine and pharmacy students for devoting their time to filling out the questionnaire. Finally, I'd like to thank the data collectors and supervisors for their assistance.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
MDT contributed significantly to the conception, design, data collection supervision, data analysis, interpretation, and manuscript write-up. SMW, MSM, NDM, AF, WZ, TZ, ADW, GTL, YTT, MSA, HMA, EMG, GGT, AWD and HSD were involved in drafting the manuscript and revising it critically for important intellectual content. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We confirm that all methods were carried out following the Helsinki declarations. The study was carried out after approval from the University of Gondar, College of Medicine and Health Sciences, Institutional Review Board (IRB), and a permission letter from the University of Gondar College of Medicine and Health Sciences. Respondents provided written informed consent before administering the questionnaire, participants were assured of the confidentiality of the information, and data was collected anonymously. Participants in the study were informed that they had the option to end the question or refuse to participate at all.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tegegne, M.D., Wubante, S.M., Melaku, M.S. et al. Tele-pharmacy perception, knowledge and associated factors among pharmacy students in northwest Ethiopia: an input for implementers. BMC Med Educ 23, 130 (2023). https://doi.org/10.1186/s12909-023-04111-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04111-9