Abstract
Background
Conducting on-site, hands-on training during the Coronavirus disease 2019 (COVID-19) pandemic has been challenging. We conducted a before and after interventional study to estimate the efficacy of a new remote hands-on training model for improving the trainees’ tracheal intubation competency using optical stylets.
Methods
Residents or physicians in anesthesiology apartment who have not received the nominated training in tracheal intubation using optical stylets were enrolled. The 4-week training course contains theoretical knowledge along with preclinical and clinical training of optical stylets techniques. Competency of intubation using optical stylets on patients with normal airways was evaluated according to an assessment tool with a maximum score of 29 points based on video recording pre-post training performance. Pre-post questionnaires measured theoretical knowledge and self-efficacy.
Results
Twenty-two participants were included (8 females, 14 men, mean age of 33.5 years). The total score of intubation competency was significantly improved after training from 14.6±3.7 to 25.3±2.6 (P < 0.0001). The scores of three subitems (anatomical identification, hand-eye coordination, and optimized intubation condition) were all significantly increased after training (P < 0.0001). The total percentage of correct answers in the multiple-choice questionnaire increased from 58.2%±8.2% before training to 85.2%±7.2% shortly after training (P < 0.0001). In addition, the self-efficacy score was significantly increased from 2.5±1.2 to 4.4±0.6 (P < 0.0001).
Conclusions
The new remote and progressively advanced hands-on training model improved the competency of intubation using optical stylets under the COVID-19 pandemic.
Similar content being viewed by others
Background
Airway management training is an integral part of an anaesthesiologist’s professional career [1], as delayed or unsuccessful tracheal intubation could cause trauma to the brain or even death [2]. Rigid and semi-rigid optical stylets have gained utmost popularity in airway management in patients with limited neck extension, mouth opening, epiglottic cysts, thyroid tumors, and so on [3,4,5,6,7]. Thus, in the residency period and continued medical education, it is essential to induct training in optical stylets intubation technique awareness.
However, due to the pandemic of Coronavirus disease 2019 (COVID-19; severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]), traditional highly structured on-site skills training courses, such as hands-on workshops and simulation training, weren’t feasible to conduct offline [8]. It is imperative to develop new technical skills training models in medical education, which were less influenced by the pandemic of COVID-19.
With the improved development of interactive online education platforms and advanced electronic gears [9], it is possible to perform a real-time, remote demonstration of the required protocols. It is also convenient to record and share videos due to the popularity of video recording systems and the development of network technologies. The increased number of online training and webinars positively affected acquiring theoretical knowledge. In contrast, the feasibility and effectiveness of implementing online skills training (for example, training in tracheal intubation using optical stylets) remain to be explored.
It was proposed that a highly structured, proficiency-based training model helped improve clinical operating skills [10, 11]. A remote difficult airway management skills training project, named ‘All-in-one airway remote training program,’ was established in the Airway Management Training Center of Fudan University at the end of 2019 (www.linaatp.com). This study aims to evaluate the effect of launching a new remote hands-on training course regarding the intubation technique using an optical stylet.
Methods
Study design
This study was conducted as a before and after interventional study at Shanghai Eye & ENT Hospital of Fudan University. Ethical approval for this study (Ethical committee No. 2021008) was provided by the Ethical Committee of Shanghai Eye & ENT Hospital of Fudan University on January 15, 2021. All methods were performed following the 1975/1983 Helsinki declaration. Each participant provided written informed consent.
From February 2021 to October 2021, anesthesiologists were trained in a group of 10 to 12 participants. The competency of optical stylets intubation was evaluated by video recordings pre- and posttraining. Theoretical knowledge was examined by a pre-post multiple-choice questionnaire (MCQ) 3 days before and after training. Participants’ self-efficacy was assessed by using a self-reported pre-post questionnaire.
Inclusion and exclusion criteria
Eligible residents and physicians met the following inclusion criteria: voluntarily participated in the training, had at least 1 year of practical experience in the department of anesthesiology, and had performed at least one-time tracheal intubation using optical stylets on the patient. Exclusion criteria included declining to submit the video recordings of intubation using optical stylets.
Education and training of optical stylets intubation competency
Competency-based optical stylets training program focused on three critical skills: anatomical identification, hand-eye coordination, and optimized intubation condition (Fig. 1). The curriculum contents were splitted into three steps: theoretical knowledge, preclinical training, and clinical training through online and remote offline learning (Figs. 2 and 3). From Step 2, we gave feedback on trainees’ performance using the assessment scale as the essential educational tool during online coaching.
Step 1 consisted of fundamental theoretical knowledge, including concept and classification, indication and complication of optical stylets use, and airway anatomy. Theoretical knowledge and case-based discussion were communicated through a low-cost, commercial online live broadcasting application, ‘Tencent Meeting’ (Tencent, Shenzhen, China), in a live broadcasting room in the trainers’ center. By watching the interactive live broadcast, the trainees could communicate with the lecturers from any place without locational obligation, mimicking the face-to-face teaching environments.
Step 2 consisted of hands-on preclinical training with a box trainer and video-based feedback. A novel portable training simulator created of acrylic material was designed for personal training (Fig. 4A) and shipped to every participant before training. The training simulator consists of a hand-made box with three hollow pipes on one side and English letters from A to K on the other side (Fig. 4B). It was designed to practice the essential operation of optical stylets, including forwarding and backward rotation direction and specific positioning. The operation demonstration was transmitted through the Tencent Meeting application. The trainees needed to practice using the optical stylets simulator for at least 1 hour and completed the designed procedures within 60 seconds before moving to the next training step.
Step 3 consisted of supervised clinical training and video-based feedback. Given that the novice practitioners needed about 20 cases to excel in the skill of optical stylets through the video-monitoring method, physicians were required to submit their 10th and 20th clinical cases. All procedures were performed on patients with normal airways and supervised by senior consultants to ensure patients’ safety. Each video consisted of a 20-minute one-on-one coaching session conducted by the supervisor, scheduled 0 to 5 days after intubation. All video-based feedback based on our assessment tool consisted of constructive guidance, identification of weaknesses and flaws, and positive reinforcement of the participants’ practice. The individual tutorials were realized through online live broadcasting software, a closed live chat function platform ‘WeChat’ (Tencent, Shenzhen, China), and cellular tools without requiring an in-person meeting.
Competency assessment, knowledge testing, and self-efficacy evaluation
Competency assessment was carried out by video recordings of individual intubations using optical stylets on patients. The video recordings were taken in the participants’ hospitals. All patients with the Scale of American Society of Anesthesiologists grade > II and with difficult airway risks like the known history of difficult intubation, upper airway abnormalities, airway inflammation, tumors, abscesses, foreign bodies, known cervical spine injury; a small mouth (< 3 cm when open), a Mallampati score of ≥3, a body mass index of > 30 were excluded. An assessment tool (minimum score 0; maximum score 29) focused on anatomical identification, hand-eye coordination, and optimized intubation condition was designed to evaluate the skills based on the video recordings. The details are deeply briefed in the nominated table [see STable 1 in Additional file 1]. A higher intubation score indicates a better intubation performance. The validity and reliability of this assessment tool were resolute in our study, shown in Additional file 1. All videos were randomly numbered. Two raters (including the experienced consultants) blinded to the participant’s identity scored the videos and recorded the intubation time. Then the results were calculated on the averages and interrater reliability assessment.
Academical knowledge testing was performed using a MCQ exam of 20 questions focusing on indications, intubation techniques, and complications of optical stylets use. The MCQ exam was designed based on currently available best practice literature and validated by four senior anesthesiologists by a modified Delphi technique. Senior anesthesiologists rated each item, which was retained if the consensus was reached with at least 80% of the clinical experts’ voting [12]. At the end of the process, the final tool consisted of 20 items with a maximum acquiring score of 100 points. Then the questions were trialed with four anesthesiologists to ensure that the MCQ exam was understandable and consistent with the training content.
A questionnaire performed self-efficacy evaluation, an individual’s confidence in the ability to complete a specific task [13]. Self-efficacy was also helpful in mediating the reduction of the knowledge-behavior gap among health care workers [14]. Questions were asked about participants’ ability to use optical stylets on a 5-item scale which ranged from 1 (strongly disagree) to 5 (strongly agree). Responses of “not applicable” for any item were excluded. The self-efficacy was also designed based on the previous study [13], and the final tool consisted of 7 items.
Outcomes
The primary study outcome was competency measured by the assessment tool according to pre-post video recordings. The time to successful intubation was recorded (from insertion to removal of the stylet). The intubation quality score (score per minute) was also calculated based on a previous study [15]. The secondary outcomes were the scores of the pre-post MCQ exam and self-efficacy evaluated by the pre-post questionnaire.
Sample size calculation
In the educational field, an adequate sample size of above 1.0 SD is considered relevant and significant for an educational intervention reported in the previous study [16]. Thus, assuming such an effect size of 1.0 SD, a sample of 15 participants was sufficient to achieve a discriminating power of 80% with a 2-sided alpha level of 5%. Considering airway management skill is essential for anesthesiologists’ continuing education, we decided to include all eligible participants during the recruitment period. This also would allow us to ensure a sufficient sample size despite the likelihood of participants dropping out.
Statistical analysis
Statistical analyses were performed using SPSS 19.0 (Chicago, IL, USA). The normal distribution of the outcome variables was analyzed using the Shapiro–Wilk test. Interrater reliability was assessed using Pearson product-moment correlation coefficient. The scores of intubation performance and self-efficacy were expressed as mean ± SD using a paired t-test. The MCQs questionnaire was presented as median [IQR] and was compared using the Wilcoxon signed-rank test. The characteristics of participants were expressed as numbers and percentages. P < 0.05 was considered statistically significant.
This manuscript was prepared according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [17].
Results
Baseline participant characteristics
From February to October 2021, among 45 anesthesiologists who were invited to the study, 22 remained as demonstrated in Fig. 5 (8 females, 14 men, mean age of 33.5 years). Overview of participants regarding gender, age, professional level, grade of the hospital, working years, and the type of optical stylets are shown in Table 1.
The outcome of training and scores of intubation skills
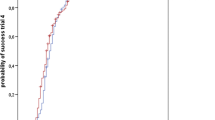
A total of 44 videos were reviewed and scored. The intubation performance was assessed by a designed assessment tool (STable 1). The Pearson product-moment correlation coefficient of the interrater reliability is 0.94 (Fig. 6). The construct and content validity of the assessment tool has been conducted, and the results were shown in STable 2 and STable 3.
The interrater reliability of the assessment tool for intubation using optical stylets. The interrater reliability concerning the total scores based on 44 video recordings was good, Pearson’s r = 0.94. Reliability was highest for optimized intubation condition, Pearson’s r = 0.90, and the anatomical identification, Pearson’s r = 0.84, somewhat lower concerning hand-eye coordination, Pearson’s r = 0.79
The average score of overall intubation performance was significantly improved posttraining compared to the pretraining period (25.3 ± 2.6 vs. 14.6 ± 3.7, P < 0.0001). The average score for anatomical identification, hand-eye coordination, and the optimized intubation condition increased significantly (P < 0.0001, Table 2).
Interestingly, the scores in hand-eye coordination and optimized intubation condition domain improved to a similar degree between the less (performed 1-50 optical stylets) and more experienced trainees (performed > 50 optical stylets). However, the degree of improvement of anatomical identification scores was lower in the more experienced trainees than that in the less ones (P = 0.016, Table 3).
The correct answers for MCQs increased from 58.2 ± 8.2% before training to 85.2 ± 7.2% shortly after training (P < 0.0001). Forty-four questionnaires were returned and analyzed. There were significant improvements in self-efficacy scores for all seven subitems compared with pretraining (all P < 0.0001, except one P = 0.0003, Table 4), with the sum of all items increasing from 2.5 ± 1.2 pretraining to 4.4 ± 0.6 posttraining (P < 0.0001, Table 4).
Discussion
Our study has shown that the competency of optical stylets on patients with normal airways significantly increased after remote training. Among these, three critical skills were improved considerably, including anatomical identification, hand-eye coordination, and optimized intubation conditions. In addition, participants’ knowledge and self-efficacy in using optical stylets were also significantly improved. Overall, this remote training model is an effective teaching technique for optical stylets intubation training.
Optical stylets not only offer effective airway management aid [3,4,5,6,7], but also can reduce intubation complications such as hoarseness and sore throat compared with laryngoscope [18]. Skillful usage of optical stylets is essential for the anesthesiologist. However, the lack of experienced faculty, inconsistent availability of equipment, and intubation methods differing from video laryngoscopy can be obstacles. To our knowledge, this is a novel study investigating the efficiency of a remote airway management project to improve optical stylets intubation competency.
It is challenging to implement airway management technique training during the COVID-19 pandemic. In this study, we guaranteed the training effectiveness through several strategies. One one hand, we have adopted a good curriculum structure from simple to complex ideas in remote training, from basic theoretical to preclinical and clinical training. On the other hand, participants acquired hands-on skill proficiency through deliberate practice with video-based feedback instead of face-to-face guidance. Furthermore, we ensured patients’ safety by enrolling experienced participants, supervised operations on patients with normal airways, and provided instant feedback using ‘WeChat’. Considering that not all trainees had access to airway manikins, and all participants had at least 1 year of anesthesiology experience with basic upper airway anatomy knowledge, airway manikins’ performance was not mandatory. This flexible skill training model could be extended to other airway management skills training under the pandemic.
We designed the training curricula based on the learning curve of optical stylets intubation and our center’s training experience. The expertise criterion was defined as the intubation experience of > 100 optical stylets, according to a previous study regarding rigid bronchoscopies [19]. The three critical techniques as an expert are recognizing the anatomical landmark, to be hand-eye coordination and optimizing intubation conditions. Instead of speeding up the intubation time, we encouraged the participants to slow the intubating speed and put their awareness on avoiding contact with surrounding mucosal tissue. With the video monitor during the intubating procedure, the “avoiding contact” technique highly reduces the incidence of injury, bleeding, and mass rupture caused by blind approach [20].
In recent years, many studies have presented and assessed the effectiveness of remote medical education. Among which, only several studies reported remote learning regarding hands-on clinical skills, focusing on training effect in preclinical settings instead of real clinical ones [21,22,23]. However, the skills’ evaluation, including navigational skills, decision-making, team cooperation, and anatomical identification, could hardly be assessed based on the remote simulator [23]. In this study, our training program focused on improving the optical stylets intubation skill and tested the effectiveness in clinical settings.
In this remote training circumstance, we used video recordings for performance evaluation and improvement instead of direct observations in the operation room. Beneficially, video recording is an emerging approach to evaluate health workers’ performance, such as neonatal resuscitation [24,25,26] and surgery skills [27, 28], thus ultimately enlightening patient safety. The video-recorded clinical performance is cost-effective and noninvasive to the performed procedure. The researchers would be able to secure highly observational and essential data of real-time happenings [29], and directs it towards individualized goal-directed learning [30]. The results of our study were consistent with previous studies [24,25,26].
The assessment tool was designed specifically for this study with assurance of its validity and reliability because no previously validated tools were available. Our assessment tool can aid in recognizing the most experienced subject compared to novices, making it a progressive tool.
Our study has some limitations. First, the number of participants is limited. We minimized the number of tutor participants in the ‘classroom’ and allowed more interaction for the trainees with peers and instructors. Introducing a larger scale, remote training needs to be carefully planned and organized [31]. Second, technical skills may decline noticeably after three to six months [32, 33], and skill retention should be tested in the sustainability phase. Third, our study was a before and after research, not a parallel randomized controlled trial of two groups. A randomized controlled trial should be designed to prove the effectiveness of remote hands-on airway management skills training.
Conclusion
In conclusion, this study confirms the value of an advanced hands-on technical skill remote training model for anesthesiologists to learn optical stylets intubation technique. Furthermore, this training model may be feasible for other airway management skills training under the COVID-19 pandemic.
Availability of data and materials
All data and additional file are available upon request from the corresponding author.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- MCQ:
-
Multiple-choice questionnaire
References
Bessmann EL, Østergaard HT, Nielsen BU, Russell L, Paltved C, Østergaard D, et al. Consensus on technical procedures for simulation-based training in anaesthesiology: a Delphi-based general needs assessment. Acta Anaesthesiol Scand. 2019;63(6):720–9.
Cook T, Morgan P, Hersch P. Equal and opposite expert opinion. Airway obstruction caused by a retrosternal thyroid mass: management and prospective international expert opinion. Anaesthesia. 2011;66(9):828–36.
Kim JK, Kim JA, Kim CS, Ahn HJ, Yang MK, Choi SJ. Comparison of tracheal intubation with the airway scope or Clarus video system in patients with cervical collars. Anaesthesia. 2011;66(8):694–8.
Xu M, Li XX, Guo XY, Wang J. Shikani optical stylet versus Macintosh laryngoscope for intubation in patients undergoing surgery for cervical spondylosis: a randomized controlled trial. Chin Med J. 2017;130(3):297–302.
Seo H, Lee G, Ha SI, Song JG. An awake double lumen endotracheal tube intubation using the Clarus video system in a patient with an epiglottic cyst: a case report. Korean J Anesthesiol. 2014;66(2):157–9.
Liu L, Yue H, Li J. Comparison of three tracheal intubation techniques in thyroid tumor patients with a difficult airway: a randomized controlled trial. Med Principles Pract. 2014;23(5):448–52.
Phua DS, Mah CL, Wang CF. The Shikani optical stylet as an alternative to the GlideScope® videolaryngoscope in simulated difficult intubations--a randomised controlled trial. Anaesthesia. 2012;67(4):402–6.
Sneyd JR, Mathoulin SE, O'Sullivan EP, So VC, Roberts FR, Paul AA, et al. Impact of the COVID-19 pandemic on anaesthesia trainees and their training. Br J Anaesth. 2020;125(4):450–5.
Chen T, Peng L, Yin X, Rong J, Yang J, Cong G. Analysis of user satisfaction with online education platforms in China during the COVID-19 pandemic. Healthcare (Basel). 2020;8(3):200. https://doi.org/10.3390/healthcare8030200.
Hogg ME, Tam V, Zenati M, Novak S, Miller J, Zureikat AH, et al. Mastery-based virtual reality robotic simulation curriculum: the first step toward operative robotic proficiency. J Surg Educ. 2017;74(3):477–85.
Mehdipour-Rabori R, Bagherian B, Nematollahi M. Simulation-based mastery improves nursing skills in BSc nursing students: a quasi-experimental study. BMC Nurs. 2021;20(1):10.
Gogovor A, Zomahoun HTV, Ben Charif A, McLean RKD, Moher D, Milat A, et al. Essential items for reporting of scaling studies of health interventions (SUCCEED): protocol for a systematic review and Delphi process. Syst Rev. 2020;9(1):11.
Zhao QJ, Rozenberg D, Nourouzpour S, Orchanian-Cheff A, Flannery J, Kaul R, et al. Positive impact of a telemedicine education program on practicing health care workers during the COVID-19 pandemic in Ontario, Canada: a mixed methods study of an extension for community healthcare outcomes (ECHO) program. J Telemed Telecare. 2021. https://doi.org/10.1177/1357633x211059688:1357633X211059688.
Rimal RN. Closing the knowledge-behavior gap in health promotion: the mediating role of self-efficacy. Health Commun. 2000;12(3):219–37.
Konge L, Larsen KR, Clementsen P, Arendrup H, von Buchwald C, Ringsted C. Reliable and valid assessment of clinical bronchoscopy performance. Respiration. 2012;83(1):53–60.
Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic press; 1977. p. 24–7.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Lee JY, Hur HJ, Park HY, Jung WS, Kim J, Kwak HJ. Comparison between video-lighted stylet (Intular scope™) and direct laryngoscope for endotracheal intubation in patients with normal airway. J Int Med Res. 2020;48(11):300060520969532.
Mahmood K, Wahidi MM, Osann KE, Coles K, Shofer SL, Volker EE, et al. Development of a tool to assess basic competency in the performance of rigid bronchoscopy. Ann Am Thorac Soc. 2016;13(4):502–11.
Hung KC, Tan PH, Lin VC, Wang HK, Chen HS. A comparison of the Trachway intubating stylet and the Macintosh laryngoscope in tracheal intubation: a manikin study. J Anesth. 2013;27(2):205–10.
Ohshima T, Koiwai M, Matsuo N, Miyachi S. A novel remote hands-on training for neuroendovascular-based treatment in the era of the COVID-19 pandemic. Interv Neuroradiol. 2022. https://doi.org/10.1177/15910199211068666:15910199211068666.
Takahashi K, Tanaka C, Numaguchi R, Kuroda Y, Nemoto H, Yoshino K, et al. Remote simulator training of coronary artery bypass grafting during the coronavirus disease 2019 pandemic. JTCVS Open. 2021;8:524–33.
Elrod J, Boettcher J, Vincent D, Schwarz D, Trautmann T, Reinshagen K, et al. Telementoring of open and laparoscopic knot tying and suturing is possible: a randomized controlled study. Eur J Pediatr Surg. 2022. https://doi.org/10.1055/s-0041-1741542.
den Boer MC, Houtlosser M, Foglia EE, Tan R, Engberts DP, Te Pas AB. Benefits of recording and reviewing neonatal resuscitation: the providers' perspective. Arch Dis Child Fetal Neonatal Ed. 2019;104(5):F528–f34.
Shivananda S, Twiss J, El-Gouhary E, El-Helou S, Williams C, Murthy P, et al. Video recording of neonatal resuscitation: a feasibility study to inform widespread adoption. World J Clin Pediatr. 2017;6(1):69–80.
Holm-Hansen CC, Poulsen A, Skytte TB, Stensgaard CN, Bech CM, Lopes MN, et al. Video recording as an objective assessment tool of health worker performance in neonatal resuscitation at a district hospital in Pemba, Tanzania: a feasibility study. BMJ Open. 2022;12(5):e060642.
Saun TJ, Zuo KJ, Grantcharov TP. Video Technologies for Recording Open Surgery: a systematic review. Surg Innov. 2019;26(5):599–612.
Alameddine MB, Englesbe MJ, Waits SA. A video-based coaching intervention to improve surgical skill in fourth-year medical students. J Surg Educ. 2018;75(6):1475–9.
Gelbart B, Hiscock R, Barfield C. Assessment of neonatal resuscitation performance using video recording in a perinatal Centre. J Paediatr Child Health. 2010;46(7-8):378–83.
Greenberg CC, Dombrowski J, Dimick JB. Video-based surgical coaching: an emerging approach to performance improvement. JAMA Surg. 2016;151(3):282–3.
Sánchez-Mendiola M, Martínez-Franco AI, Rosales-Vega A, Villamar-Chulin J, Gatica-Lara F, García-Durán R, et al. Development and implementation of a biomedical informatics course for medical students: challenges of a large-scale blended-learning program. J Am Med Inform Assoc. 2013;20(2):381–7.
Moulton CA, Dubrowski A, Macrae H, Graham B, Grober E, Reznick R. Teaching surgical skills: what kind of practice makes perfect?: a randomized, controlled trial. Ann Surg. 2006;244(3):400–9.
Stefanidis D, Korndorffer JR Jr, Markley S, Sierra R, Scott DJ. Proficiency maintenance: impact of ongoing simulator training on laparoscopic skill retention. J Am Coll Surg. 2006;202(4):599–603.
Acknowledgements
The authors acknowledge the participants from different hospitals in this study for assistance with the study.
Funding
This study was supported in part by the Natural Science Foundation of Shanghai (21ZR1411300) and Shenkang Clinical Study Foundation of Shanghai (SHDC2020CR4061) to Dr. Han, the Shanghai Municipal Health and Family Planning Commission Research Project (2019SY015) to Dr. Wenxian Li and the Shanghai Municipal Health commission (20214Y0067) Ms. Fu. The sponsors have no involvements in study design, data collection and interpretation, writing of the manuscript, and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Author Wenxian Li and author Yuan Han have contributed substantially to the conception or design of the manuscript, and author Danyun Fu, and author Weixing Li to the acquisition, analysis, and interpretation of the data. All authors have participated to drafting the manuscript, author Yuan Han revised it critically. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study (Ethical committee No. 2021008) was provided by the Ethical Committee of Shanghai Eye & ENT Hospital of Fudan University on January 15, 2021. All methods were performed in accordance with the 1975/1983 Helsinki declaration. Written informed consent was provided by each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fu, D., Li, W., Li, W. et al. Improved skill for tracheal intubation using optical stylets through remote training model: a before and after interventional study. BMC Med Educ 22, 668 (2022). https://doi.org/10.1186/s12909-022-03715-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03715-x