Abstract
Background
Individuals with advanced Parkinson’s Disease (PD) and Parkinson-related disorders (PRD) are frequently referred for home allied therapies and nursing care, yet home healthcare professionals have limited training in PD/PRD. While recognizing the need for such care, patients and families report home healthcare professionals are unfamiliar with these conditions, which may be driven by neurophobia and may contribute to suboptimal care and early termination of services. We sought to determine the feasibility and effects of a virtual, multimodal educational intervention on PD knowledge, confidence, and empathy among home health professionals.
Methods
Home health nurses, occupational therapists, physical therapists and physical therapy assistants, and speech-language pathologists participated in a daylong, virtual symposium on advanced PD/PRD, combining focused lectures, discipline-specific breakout sessions, immersive virtual reality vignettes, and interactive panels with both patients and families, and movement disorders and home healthcare experts. Participants completed online pre- and post-symposium surveys including: demographics; PD/PRD knowledge (0–10 points possible); empathy (Interpersonal Reactivity Index); and 10-point scales of confidence with and attitudes towards individuals with PD/PRD, respectively. Pre-post intervention changes and effect sizes were evaluated with paired t-tests and Cohen’s d. We performed qualitative analyses of post-symposium free-text feedback using a grounded theory approach to identify participants’ intentions to change their practice.
Results
Participants had a mean improvement of 3.1 points on the PD/PRD knowledge test (p < 0.001, d = 1.97), and improvement in confidence managing individuals with PD/PRD (p = 0.0003, d = .36), and no change in empathy. The interactive, virtual format was rated as effective by 95%. Common themes regarding symposium-motivated practice change included: interdisciplinary collaboration; greater involvement and weighting of the patient and caregiver voice in care plans; attention to visit scheduling in relation to patient function; recognition and practical management of the causes of sudden change in PD/PRD, including infections and orthostatic hypotension.
Conclusions
A virtual, multimodal, brief educational pilot intervention improved PD/PRD-specific knowledge and confidence among home healthcare nurses and allied health professionals. Future studies are necessary to test the short- and long-term effects of this intervention more broadly and to investigate the impact of this education on patient and caregiver outcomes.
Similar content being viewed by others
Introduction
Parkinson’s Disease (PD) is the second most common neurodegenerative disease worldwide, with prevalence expected to double by 2060 [1, 2]. As PD progresses, patients have increased dependence and healthcare utilization, including both outpatient, acute or inpatient, and home care [3, 4]. Several interdisciplinary, PD-focused, educational interventions for healthcare professionals have demonstrated improvements in participants’ knowledges, attitudes, and practices in the US [5, 6], Netherlands [7], and Cameroon [8]. However, these interventions have largely attracted providers with a dedicated PD focus in their outpatient practice setting. [6, 7].
In 2015, 3.5 million US Medicare beneficiaries received 119 million home healthcare visits, of which 36% were skilled rehabilitation, including physical, occupational, or speech therapy [9] Literature supports the benefits of home-based rehabilitation on decreasing fall risk in homebound older adults [10] and improving functional recovery after hip fracture [11], and the benefits of home-based nursing in preventing rehospitalizations and improving patient outcomes [12]. To our knowledge, however, there are no interventions specifically focused on educating home nursing and rehabilitation professionals about advanced PD and related disorders such as Lewy Body Dementia (LBD), Progressive Supranuclear Palsy (PSP), Multiple System Atrophy (MSA), and Corticobasal Syndrome (CBS), hereafter referred to as Parkinson-related disorders (PRD). This is particularly important for multiple reasons: first, these healthcare professionals are the most likely to see these individuals as they become homebound, second, this population is at high risk of falls, hip fractures, hospitalization, and institutionalization, and third, as described above, home health interventions have demonstrated benefits in preventing or recovering from these outcomes in other older adult populations [13,14,15].
In pilot work conducted in New York and replicated in Chicago, our team comprised of a movement disorders specialist, nurse, and social worker, conducted over 500 interdisciplinary home visits with homebound individuals with advanced PD and PRD. Over 91% of visits culminated with allied health or specialty referrals [16,17,18]. It was not uncommon for participants to report that therapists came to the home once or twice, admitted a lack of PD or PRD knowledge, and promptly discharged the patient despite clear indications for such care. Other participants with prominent dysautonomia were inappropriately referred to the emergency department by home health professionals for asymptomatic hyper- or hypotension [17]. Despite the volume of referrals, no prior literature exists on patient or care partner satisfaction with home healthcare in PD and PRD, or the degree to which knowledge, confidence, and attitudes of the home healthcare professional effects the patient and care partner’s perception of benefit.
Beyond home visits, the lack of PD- and PRD-specific knowledge and training among nurses and allied health professionals has been identified in other contexts. The Parkinson's Disease Medication Protocol Program showed that without targeted, PD education modules, nurses may lack sufficient clinical expertise to effectively manage PD medications, specifically leading to detrimental dopaminergic medication errors and omissions [19]. More broadly, “neurophobia”, or a “fear of neural sciences and clinical neurology” [20] has long been recognized as a barrier to medical students and non-neurologist physicians, as well as dental students, occupational therapy (OT) students, and speech-language pathology (SLP) students [21, 22], with the high perceived level of difficulty of neuroanatomy inversely proportional to levels of interest in learning, understanding, and treating individuals with neurologic disorders across interdisciplinary students. To our knowledge, there have been no specific investigations of neurophobia in home healthcare professionals.
A dire need for PD- and PRD-specific home nurse and allied health professional education was identified, prompting the development of an Interactive Symposium and Educational Experience on PD for Home Health Professionals (I SEE PD Home). We aimed to determine the effect of a multimodal, interactive, virtual educational intervention on PD and PRD knowledge, confidence, and empathy among home healthcare professionals. We hypothesized that an intervention incorporating both content knowledge and experiential learning (i.e., immersive virtual reality modules) could improve knowledge of and attitudes towards individuals living with PD and PRD among home healthcare professionals [23].
Methods
Study design and setting
Here, we present a single-center, pre-post intervention study of a daylong, virtual educational symposium. Supported by a Parkinson’s Foundation (PF) Centers of Excellence Community Outreach, Research, and Engagement (CORE) grant, we partnered with our continuing education (CE) office to insure content was robust and eligible for the provision of CE credits for allied health professionals completing the full symposium. Given restrictions due to the SARS-CoV-2 pandemic, this daylong virtual symposium was broadcast via Zoom® from Rush University Medical Center in Chicago, Illinois.
Participants and recruitment
We designed the symposium specifically for licensed allied home health professionals in the following disciplines, each of whom were eligible for CE credits: registered nurse (RN), occupational therapy (OT), physical therapy (PT), physical therapy assistant (PTA), or speech-language pathology (SLP). Nursing students were invited to participate, but not eligible for CE credits. All participants met these criteria: primarily English-speaking, agreed to attend the entire day of the symposium, and had a working computer, internet connection, and email address.
Our recruitment target was 50 participants based on funding limitations, recruited from nine home healthcare agencies (HHAs). HHAs were invited to participate if the Rush Movement Disorders Clinic had referred individual patients to the agency within the past year, without significant negative feedback or concerns about the agency from referring providers. The study team contacted clinical leaders within the HHAs and asked the leaders to circulate the informational flyer to their internal teams and support participation of healthcare professionals in their respective organizations.
Intervention
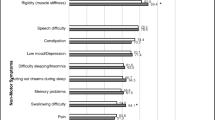
This educational intervention included four components, all focused on PD and PRD: lectures, discipline-specific breakout sessions, a patient and caregiver panel, and an immersive, virtual reality (VR) experience (Table 1). The symposium began with traditional lectures to introduce PD and PRD, including LBD, PSP, MSA, and CBS. The lectures focused on evidence-based management, including in-depth coverage of advanced motor and non-motor symptoms in later stages of PD and PRD. A second lecture focused on urgent situations detected during home healthcare visits, including falls, mental status changes, or concerns about neglect or abuse, with provision and review of critical resources in the PF Aware in Care Kit [24].
Attendees chose to attend one of three breakout sessions: 1) What Nurses Need to Know: covering the importance of medication timing and reconciliation, orthostatic hypotension, and constipation; 2) Overview for Physical and Occupational Therapists: covering fall prevention, home safety assessments, healthy exercise and movement; or 3) Overview for Speech-Language Pathologists: targeting hypophonia, dysarthria, dysphagia, and related issues, assistive devices, and other treatment options. All breakout sessions introduced practical strategies to promote healthy aging-in-place in PD/PRD and were led by a home health professional with PD/PRD expertise in each respective discipline.
After the breakout sessions, the participants were joined on Zoom by a panel of several caregivers and people living with advanced PD/PRD. Panelists introduced themselves, their experience with home health, and illustrated opportunities for benefit, change, and potential impact. Following introductions, symposium participants were able to pose questions to the panelists. Pertinent questions asked by the HHA professional participants of the patients and caregivers included: whether families felt they had sufficient education on PD/PRD when first diagnosed; cues, exercises, and devices that promoted safe aging-in-place in their own homes, and whether they had discovered these on their own or they had been recommended by healthcare professionals; communication tips for people living with PD/PRD; recommendations for scheduling home therapy sessions around motor fluctuations and non-motor symptoms such as daytime sleepiness and apathy.
Participants also completed three 10–12-min sessions of the Dima Lab (Embodied Labs, Los Angeles, CA) immersive VR experience throughout the day. While connected to the symposium’s videoconferencing software, the VR experience was livestreamed such that participants were viewing it in real-time. In the Dima Lab, the viewer inhabits the body of a Lebanese-American woman named Dima with LBD. Across the three vignettes, the viewer, as Dima, interacts with family members in her own home, and with healthcare providers in both outpatient and institutional settings, demonstrating multiple motor and non-motor symptoms along with Dima’s internal monologue. The learning objectives for the Dima Lab included: recognizing symptoms of LBD; helping people with LBD experiencing anxiety, agitation, or hallucinations; and recognizing when emotional or physical burnout, financial burden, or safety may necessitate help from professional care agencies or residential care communities.
The symposium concluded with a question and answer panel with the breakout session leaders and the movement disorders specialist, a final set of summary slides, and the online post-intervention surveys and evaluations. All symposium slides and materials are available in Additional file 2: Appendix B, and annotated facilitator guides for both the patient and caregiver panel and the final expert question and answer panel are provided in Additional file 3: Appendix C.
Measures
Survey structure
Participants completed all demographic, knowledge, and attitude measures in real-time at the beginning of the symposium (pre-intervention) and again at the end of the day (post-intervention) via a link to a secure, electronic database shared by the study team [25]. At both time points, participants were prompted to select the first initial of their first name, color of their first car, and manually enter their childhood home street name, generating a unique identifier to facilitate linkage of pre- and post-intervention assessments. To obtain CE credits, participants completed a standardized CE questionnaire via an online link emailed to them directly from the CE office.
Demographic information and experience
Sociodemographic information included: age, gender identity, race, and ethnicity. Participants reported: discipline (registered nurse, physical therapist, physical therapy assistant, occupational therapist, or speech-language pathologist); years since terminal degree; years of experience in home health care specifically; volume of individuals treated with PD/PRD in the past year (categorized as 0, 1–5, 6–10, 11–15, 16–20, or > 20), and whether the participant had any personal or family experience with PD/PRD.
PD/PRD knowledge
For this symposium, the study team developed a 10-item, multiple choice survey covering practical knowledge related to the management of individuals with PD/PRD that might reasonably be encountered by and pertinent to home healthcare professionals (Additional file 1: Appendix A). Each item was designed by a member of the study team with survey development experience [26] (JEF) based on the lecture content and following guidance on survey development in medical education, using positive language, avoiding reverse-scored items, providing an appropriate number of and appropriately labeled response options in a single column, and asking the more important items earlier in the survey [27]. A panel of independent movement disorders experts then separately reviewed and revised the prompts and response, followed by an additional round of revisions and review for any items of remaining concern, using a modified Delphi approach [28]. We hypothesized that post-intervention, participants would demonstrate a mean 10% improvement compared to their pre-intervention PD/PRD Knowledge score.
Secondary Outcomes: Empathy, confidence, attitudes, and feasibility
We assessed empathy using the Interpersonal Reactivity Index (IRI), a 28-item validated tool to measure change in empathy among nursing students and other healthcare professionals following educational interventions [29]. The IRI is scored as four domain subscales, namely, Perspective Taking, Fantasy, Empathic Concern, and Personal Distress. Each domain is made up of seven items scored on a 5-point Likert scale where higher scores indicate higher empathy. To evaluate the efficacy of the Dima Lab VR PD scenarios, we administered four proprietary questions designed by the VR manufacturer (Embodied Labs) assessing change in confidence and attitudes towards people with PD/PRD [30], where the response options for each prompt were a ten-point Likert scale ranging from strongly disagree [1] to strongly agree [10]. We assessed the feasibility of the I SEE PD Home intervention by tracking attendance in real time and awarding CE credits only once the participant had completed the post-intervention evaluation. We solicited quantitative feedback on the symposium via a standardized CE evaluation, and qualitative feedback from the participants throughout the intervention via live comments (verbal and chat) and open-ended questions in the CE evaluation.
Data analysis
All pre- and post-intervention data were entered directly into a HIPAA-compliant, secure electronic database by the participants [25]. Data was exported, cleaned, and analyzed in Stata 15 (StataCorp, 2015). Descriptive analysis of the demographics, professional experience, and baseline assessment scores included means/standard deviation or median/interquartile range, as appropriate. We used paired t-tests to assess for change in the pre- and post-intervention PD/PRD Knowledge Test (primary outcome) and in the IRI and VR questionnaires (secondary outcomes), with Cohen’s d to calculate effect size, where 0.2, 0.5, and 0.8 signified small, medium, and large effect sizes, respectively [31]. For qualitative feedback, a grounded theory approach was used to code participant free-text survey responses. Two study team members (SH, JEF) independently coded responses, met to discuss emerging themes, and reviewed coded responses in relation to the themes, highlighting illustrative quotations for each theme [32, 33]. As this was a pilot study, our target recruitment goal of 50 participants was based on feasibility and funding restrictions.
Results
Participant characteristics
A total of 52 attendees completed the full-day, I SEE PD Home virtual symposium on March 5, 2021. Of these 52 attendees, five nursing students were excluded from study participation as they were ineligible for CE credits. Forty-two of the remaining 47 participants completed the demographics information and 35 participants completed all pre- and post-intervention surveys (Table 2, middle and right columns, respectively); there were no significant differences between the groups. Most attendees were female (90.5%) and between the ages of 35–44 (26.2%) or 45–54 (38.1%). PTs represented 38% of the attendees, followed by: OTs (21.4%), RNs (16.7%), SLPs (7.1%), PTAs (4.8%), and 11.9% “other” or did not disclose their discipline.
The attendees had a mean of 16.3 years (standard deviation (SD) 10.5) in practice since training, and 7.1 years (SD 6.7) of home health care experience specifically. Nearly one quarter of participants (23.8%) had not treated any patients with PD/PRD in the past year, and another 23.8% reported treating 1–5 such individuals, combined. Eleven participants (26.2%) endorsed personal or family experience with PD/PRD. Participants cared for patients across six states: Illinois, Indiana, Kentucky, Pennsylvania, Texas, and Wisconsin.
Primary and secondary outcomes
Complete pre- and post-intervention primary outcome data (PD/PRD Knowledge score) was available for 35 individuals, and complete pre- and post-intervention secondary outcome data for 37 (IRI) and 36 (VR questionnaire), respectively. Among the 35 participants completing the PD/PRD Knowledge test pre- and post-intervention, 91.42% (n = 32) improved their post-intervention score by our a priori cut-off of at least 10% and the mean improvement was 31.14% (SD 17.62%). As shown in Table 3, home health professionals scored a mean of 4.06 out of 10.0 possible points on the PD/PRD Knowledge test at baseline pre-intervention (SD 1.53), and showed a mean 3.1-point improvement post-intervention (mean 7.17, SD 1.62, p < 0.0001), with a large effect size of 1.97.
We found no change in any of the four IRI empathy domains (p = 0.16–0.58, Cohen’s d = 0.05–0.12). In the VR questionnaire, there was a 1-point improvement (Cohen’s d = 0.39) in response to whether participants felt that “a person living with Lewy body dementia and/or Parkinson’s disease is able to spend their time meaningfully and can contribute to family and community life” (pre-intervention mean 8.50 (SD 3.00) vs. post-intervention 9.50 (SD 2.00), p = 0.01). In response to whether the participant felt “confident in my ability to help a person expressing agitation, stress, combativeness, hallucination, or sensory overload as a result of their progressing dementia and/or Parkinson’s disease”, there was a small change between pre- and post-intervention assessments (pre-intervention mean 7.00 (SD 3.00) vs. post-intervention 8.00 (2.50), p = 0.0003, d = 0.36).
Feasibility and satisfaction
Of 52 attendees, all were able to access Zoom, navigate between the main rooms, breakout rooms, and panels, and use the chat feature to submit questions. Of all attendees, 47 were eligible for CE credit and thus pre- and post-intervention evaluations, 42 initiated the pre-intervention assessment, 39 participants completed the CE evaluation, and 35 had complete data for the pre- and post-intervention assessments and the CE evaluation.
As shown in Table 4, 100% of the 39 participants completing the CE evaluation either agreed or strongly agreed with each measure of achievement. Notably, 94.9% each strongly agreed that the teaching methods were effective for learning and that the knowledge and skills acquired in the activity were directly applicable to their professional practice.
Qualitative feedback
Twenty-seven of the 39 CE evaluation respondents endorsed an intent to change their practice in response to I SEE PD Home, with a sample of their verbatim, free-text responses highlighted in Table 5. Several themes emerged from these responses, including intentions to: increase interdisciplinary collaboration and disseminate new knowledge to colleagues; solicit greater involvement of and place more weight on the voice of the patient and caregiver; pay more attention to visit scheduling in relation to the patient’s function; attend to the etiology and management of sudden changes in the patient’s condition, particularly regarding urinary tract infections and orthostatic hypotension; recognize and empathize with neuropsychiatric symptoms; and apply newfound knowledge regarding pharmacologic and non-pharmacologic treatment of various symptoms. Although the chat feature was enabled throughout the entire symposium, the majority of spontaneous qualitative feedback arose during the patient and caregiver panel. Multiple participants commented that hearing directly from caregivers and patients with PD was a novel and enriching experience for them. Many of the HHA participants recognized that each PD patient responds to different stimuli or approaches and receiving validation of this from the caregivers and patients on the panel was cited as helpful by many. One participant stated “It was very educational, informative and I loved the part with real patients. Because of their feedback we can improve our services and work together as a team to provide holistic care for their loved ones.”
Discussion
To our knowledge, this is the first medical educational intervention of its kind to specifically focus on educating home health nurses and allied health professionals about the care of people with advanced PD/PRD. Although planned prior to the SARS-CoV-2 pandemic and pivoted to a virtual format, participation in, satisfaction with, and efficacy of the virtual training were all high, in line with research on continuing education and conferences in other areas of healthcare [34, 35]. Indeed, the virtual format using Zoom® allowed for home health professionals in six different states and across different HHAs to participate and learn from each other, and the widespread availability of the platform and shared materials (in Additional file 1, 2 and 3: Appendices A-C) enhance the generalizability and ability to replicate the intervention and findings. Based on a standardized CE evaluation, all participants reported subjective improvements in knowledge and confidence regarding this patient population; objective assessments confirmed this, with a large effect on PD/PRD knowledge in particular, as demonstrated by a scale developed for this intervention. This is especially important in that it counters the likely pre-existing neurophobia in these healthcare professionals. In particular, one survey of medical, dental, OT, and SLP students found that while neuroanatomy overall was ranked the most difficult anatomic system to learn, the motor pathways and basal nuclei—the structures most involved in PD/PRD—were ranked second and fifth most difficult, respectively, out of 21 topics in the neuroanatomy curriculum [22].
While this is the first program specifically designed to educate home health professionals on PD/PRD-specific needs, similar interventions have been successful in other geriatric populations [36, 37]. Fukui and colleagues conducted a cluster randomized trial of an educational booklet and workshop on end-of-life issues for home care nurses, care managers, and care workers. Among healthcare professionals randomized to the intervention compared with control participants, active participants demonstrated improved cooperation and confidence in their ability to identify and communicate with other healthcare professionals, however there was no difference in job satisfaction between groups. Schneider and colleagues evaluated the efficacy of the Aliviado Dementia Care-Hospice Edition performance improvement program on the quality of hospice care delivered to people with dementia and their caregivers. The Aliviado program involved a two day, in-person training session for team leaders and online training for other team members. Both the team leader training and the online program demonstrated post-intervention improvements in healthcare professionals’ knowledge and confidence. However, neither of the programs above mentioned PD or PRD as part of the training despite their respective focus on end-of-life, geriatrics, and dementia, and both programs required in-person attendance. While in-person interventions are often the default, virtual models may be particularly attractive to allied health practitioners for reasons extending beyond the restrictions of the SARS-CoV-2 pandemic. Home health practitioners often reside in or near the communities they serve and may be located far from academic centers where CE and other educational programs are typically held. Access to virtual programs not only facilitates continuing education, but intra- and interdisciplinary networking opportunities [34, 35]. Particularly for home health practitioners in rural locations, they may be one of a limited number of practitioners in their area or the sole practitioner responsible for seeing a wide spectrum of patients. Providing education and resources to these more isolated providers may have disproportionate benefits for the communities they serve [38].
There were several limitations to this study. With a goal of enrolling 50 professionals in the symposium, we estimated that if each professional saw 5 PD/PRD patients per year, approximately 250 homebound PD/PRD patients could be reached with more knowledgeable, confident, and empathic providers. This was a small, uncontrolled pilot study with pre- and post-intervention data gathered within the same day, without patient-level outcome data. While longitudinal follow-up on the persistence of knowledge and attitude changes is desirable, given both the time-limited restrictions of funding and the pre-pandemic annual turnover rate of 30–65% or higher among home healthcare professionals [39, 40], we were unable to repeat participant assessments beyond the day of the symposium. This study suffers from a healthy volunteer bias, in that health professionals actively choosing to participate in I SEE PD Home may be more motivated to learn about this patient population, and both their baseline knowledge, confidence, and attitudes, along with the degree of change following the intervention, may not generalize to individuals who were offered but declined to participate in the intervention, or to the broader population of home health professionals. We anticipated that motivated participants would be more likely to participate in, gain from, and in turn serve as local champions within their respective HHAs, disseminating lessons learned to colleagues who did not choose to attend. Furthermore, to maximize recruitment within the given budgetary and time constraints, we recruited participants only from HHAs about which we had not received negative feedback from patients and families. It is plausible that home healthcare professionals in unfavorably reviewed HHAs may stand to learn and benefit the most from such an intervention, and future iterations should recruit from a broader pool of HHAs. Finally, the PD/PRD Knowledge test was created and piloted by the study team since no instrument was available to measure change in PD/PRD knowledge, with ongoing validation in a separate cohort of family caregivers.
Conclusion
A virtually-delivered, multimodal educational intervention focused on PD- and PRD-specific issues pertinent to home healthcare professionals, incorporating general and discipline-specific content, immersive virtual reality, interactive sessions with allied health experts and with patients and caregivers, was highly successful and positively received by the participants. The virtual format allowed for simultaneous participation of home healthcare professionals across multiple states and time zones and facilitated interaction with both experts and individuals affected by PD/PRD. These features may have mitigated the neurophobia commonly contributing to poor interest in and outcomes for this population. Despite the rising global prevalence and impact of neurological conditions in general and PD/PRD specifically [2, 41, 42], and despite the frequency of referrals of individuals with advanced PD/PRD to home health practitioners [43], these critical members of the health care team have previously been overlooked in educational interventions. Future directions for I SEE PD Home include replicating and systematically testing the intervention among a broader audience of home healthcare professionals, and longitudinally assessing patient- and caregiver-level outcomes among families receiving care from providers who have completed the training versus usual care. If successful and deemed valuable by the participating home healthcare professionals, I SEE PD Home could empower participants to become knowledgeable leaders within their HHAs and communities, and agents of change for this vulnerable and expanding patient population.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- CBS:
-
Corticobasal syndrome
- CE:
-
Continuing education
- CORE:
-
Community Outreach, Research, and Engagement
- HHA:
-
Home healthcare agency
- HIPAA:
-
Health Insurance Portability and Accountability Act
- IRI:
-
Interpersonal Reactivity Index
- I SEE PD Home:
-
Interactive Symposium and Education Intervention in Parkinson’s Disease Home Healthcare Professionals
- LBD:
-
Lewy Body Dementia
- MSA:
-
Multiple system atrophy
- OT:
-
Occupational therapy
- PD:
-
Parkinson’s Disease
- PF:
-
Parkinson’s Foundation
- PRD:
-
Parkinson-related disorders
- PSP:
-
Progressive supranuclear palsy
- PT:
-
Physical therapy
- PTA:
-
Physical therapy assistant
- RN:
-
Registered nurse
- SD:
-
Standard deviation
- SLP:
-
Speech-language pathology
- VR:
-
Virtual reality
References
Pringsheim T, Jette N, Frolkis A, Steeves TDL. The prevalence of Parkinson’s disease: a systematic review and meta-analysis: PD PREVALENCE. Mov Disord. 2014;29(13):1583–90.
Savica R, Grossardt BR, Rocca WA, Bower JH. Parkinson disease with and without dementia: a prevalence study and future projections. Mov Disord Off J Mov Disord Soc. 2018;33(4):537–43.
Giles S, Miyasaki J. Palliative stage Parkinson’s disease: patient and family experiences of health-care services. Palliat Med. 2009;23(2):120–5.
Hasson F, Kernohan WG, McLaughlin M, Waldron M, McLaughlin D, Chambers H, et al. An exploration into the palliative and end-of-life experiences of carers of people with Parkinson’s disease. Palliat Med. 2010;24(7):731–6.
Cohen EV, Hagestuen R, González-Ramos G, Cohen HW, Bassich C, Book E, et al. Interprofessional education increases knowledge, promotes team building, and changes practice in the care of Parkinson’s disease. Parkinsonism Relat Disord. 2016;22:21–7.
Cohen EV, Luce V, González MJ, Hagestuen R, González-Ramos G, Cohen HW. Improving team skills of health care practitioners: effects of an interprofessional education program. J Contin Educ Health Prof. 2021;41(3):185–94.
Bloem BR, Rompen L, de Vries NM, Klink A, Munneke M, Jeurissen P. ParkinsonNet: a low-cost health care innovation with a systems approach from The Netherlands. Health Aff (Millwood). 2017;36(11):1987–96.
Cubo E, Doumbe J, Njiengwe E, Onana P, Garoña R, Alcalde J, et al. A Parkinson’s disease tele-education program for health care providers in Cameroon. J Neurol Sci. 2015;357(1–2):285–7.
Collins TL, Yong KW, Marchetti MT, Miller KL, Booths B, Falvey JR. The value of home health physical therapy. Home Healthc Now. 2019;37(3):145–51.
Gallo E, Stelmach M, Frigeri F, Ahn D-H. Determining whether a dosage-specific and individualized home exercise program with consults reduces fall risk and falls in community-dwelling older adults with difficulty walking: a randomized control trial. J Geriatr Phys Ther. 2018;41(3):161–72.
Latham NK, Harris BA, Bean JF, Heeren T, Goodyear C, Zawacki S, et al. Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial. JAMA. 2014;311(7):700–8.
Whitehouse CR, Sharts-Hopko NC, Smeltzer SC, Horowitz DA. Supporting transitions in care for older adults with type 2 diabetes mellitus and obesity. Res Gerontol Nurs. 2018;11(2):71–81.
Wei Y-J, Palumbo FB, Simoni-Wastila L, Shulman LM, Stuart B, Beardsley R, et al. Relationships between antiparkinson medication nonadherence, regimen modifications, and healthcare utilization and expenditures. Parkinsonism Relat Disord. 2015;21(1):36–41.
Hassan A, Wu SS, Schmidt P, Dai Y, Simuni T, Giladi N, et al. High rates and the risk factors for emergency room visits and hospitalization in Parkinson’s disease. Park Relat Disord. 2013;19(11):949–54.
Koay L, Rose J, Abdelhafiz AH. Factors that lead to hospitalisation in patients with Parkinson disease—a systematic review. Int J Clin Pract. 2018;72(1): e13039.
Fleisher J, Barbosa W, Sweeney MM, Oyler SE, Lemen AC, Fazl A, et al. Interdisciplinary home visits for individuals with advanced parkinson’s disease and related disorders. J Am Geriatr Soc. 2018;66(6):1226–32.
Fleisher JE, Klostermann EC, Hess SP, Lee J, Myrick E, Chodosh J. Interdisciplinary palliative care for people with advanced Parkinson’s disease: a view from the home. Ann Palliat Med. 2020;9(Suppl 1):S80–9.
Fleisher JE, Hess S, Sennott BJ, Myrick E, Wallace EK, Lee J, et al. Longitudinal, interdisciplinary home visits versus usual care for homebound people with advanced Parkinson Disease: protocol for a controlled trial. JMIR Res Protoc. 2021;10(9):e31690.
Chenoweth L, Sheriff J, McAnally L, Tait F. Impact of the Parkinson’s disease medication protocol program on nurses’ knowledge and management of Parkinson’s disease medicines in acute and aged care settings. Nurse Educ Today. 2013;33(5):458–64.
Jozefowicz RF. Neurophobia: the fear of neurology among medical students. Arch Neurol. 1994;51(4):328–9.
Sandrone S, Berthaud JV, Chuquilin M, Cios J, Ghosh P, Gottlieb-Smith RJ, et al. Neurologic and neuroscience education: Mitigating neurophobia to mentor health care providers. Neurology. 2019;92(4):174–9.
Javaid MA, Chakraborty S, Cryan JF, Schellekens H, Toulouse A. Understanding neurophobia: Reasons behind impaired understanding and learning of neuroanatomy in cross-disciplinary healthcare students. Anat Sci Educ. 2018;11(1):81–93.
Gillespie GL, Farra S, Regan SL, Brammer SV. Impact of immersive virtual reality simulations for changing knowledge, attitudes, and behaviors. Nurse Educ Today. 2021;105:105025.
Foundation NP. Aware in Care Kit [Internet]. Available from: http://www.parkinson.org/find-help/aware-in-care-kit
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–81.
Fleisher JE, Dahodwala NA, Xie SX, Mayo M, Weintraub D, Chodosh J, et al. Development and Validation of the Parkinson’s Disease medication beliefs scale (PD-Rx). J Park Dis. 2016;6(2):383–92.
Gehlbach H, Artino ARJ. The survey checklist (manifesto). Acad Med. 2018;93(3):360–6.
Niederberger M, Spranger J. Delphi Technique in Health Sciences: A Map. Front Public Health. 2020;8:457.
Davis MH. A multidimensional approach to individual differences in empathy. JSAS Cat Sel Doc Psychol. 1980;10:85.
Dyer E, Swartzlander BJ, Gugliucci MR. Using virtual reality in medical education to teach empathy. J Med Libr Assoc JMLA. 2018;106(4):498–500.
Cohen J. A power primer. Psychol Bull. 1992;112(1):155–9.
Smith K, Biley F. Understanding grounded theory: principles and evaluation. Nurse Res. 1997;4(3):17–30.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Lee L, Hillier LM, Weston WW. Comparing Virtual to In-Person Delivery of Continuing Medical Education in Dementia Care: Which Is Preferred? J Am Med Dir Assoc. 2021;S1525–8610(21):00978–86.
Nelson BA, Lapen K, Schultz O, Nangachiveettil J, Braunstein SE, Fernandez C, et al. The Radiation oncology education collaborative study group 2020 spring symposium: is virtual the new reality? Int J Radiat Oncol Biol Phys. 2021;110(2):315–21.
Fukui S, Fujita J, Ikezaki S, Nakatani E, Tsujimura M. Effect of a multidisciplinary end-of-life educational intervention on health and social care professionals: A cluster randomized controlled trial. Galletta M, editor. PLoS ONE. 2019;14(8):e0219589.
Schneider CE, Bristol A, Ford A, Lin S-Y, Palmieri J, Meier MR, et al. The impact of aliviado dementia care—hospice edition training program on hospice staff’s dementia symptom knowledge. J Pain Symptom Manage. 2020;60(2):e7-13.
Berndt A, Murray CM, Kennedy K, Stanley MJ, Gilbert-Hunt S. Effectiveness of distance learning strategies for continuing professional development (CPD) for rural allied health practitioners: a systematic review. BMC Med Educ. 2017;17(1):117.
Butler SS. Exploring relationships among occupational safety, job turnover, and age among home care aides in Maine. New Solut J Environ Occup Health Policy NS. 2018;27(4):501–23.
Bergman A, Song H, David G, Spetz J, Candon M. The role of schedule volatility in home health nursing turnover. Med Care Res Rev MCRR. 2021;26:10775587211034310.
Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017 Nov;16(11):877–97.
Nichols E, Szoeke CEI, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(1):88–106.
Fleisher JE, Sweeney MM, Oyler S, Meisel T, Friede N, Rocco AD, et al. Disease severity and quality of life in homebound people with advanced Parkinson disease: A pilot study. Neurol Clin Pract. 2020;10(4):277–86.
Acknowledgements
The authors acknowledge Jennifer Comerford, MA, CHCP for her contribution to determining CE credits and helping host this program online, Emily Smith for her aid in the VR technology, and Cintra Bentley and Jacqueline Gilbert as thoughtful representatives in our caregiver panel.
Funding
This work was supported by a Parkinson’s Foundation Centers of Excellence CORE grant [PF-Core_2004]. JEF is supported by a research grant from the National Institutes of Health/National Institute of Neurological Disorders and Stroke [K23NS097615] and philanthropic support from Joyce DeMoose and George Harvey. None of the funders had any role in the design of the intervention, data collection, analysis, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
SPH and JEF conceived the intervention, secured grant funding, wrote the protocol, designed the I SEE PD Home content, and led data collection and interpretation. SPH organized the recruitment and oversight of symposium experts, coordinated the CE certification process, led communication with and dissemination of symposium materials to participant HHAs, contributed to data collection and interpretation, and drafted the manuscript. LA, KT, and PB designed the discipline-specific I SEE PD Home content. ML, FA, and KW contributed to participant recruitment, symposium organization, and data collection. BO contributed to quantitative data analysis. JEF led the qualitative analyses and interpretation, obtained ethical approvals, and drafted and revised the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This intervention was initially designed as an educational and quality improvement initiative. Following the data collection and based on participant feedback, we sought and received retrospective approval of this work, including the coded, anonymous data and waiver of informed consent, as an exempt study by the Rush University Medical Center Institutional Review Board. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Appendix A.
Parkinson’s Disease Knowledge Survey.
Additional file 2. Appendix B.
I SEE PD Home slides.
Additional file 3. Appendix C.
Facilitator guides.
Additional file 4.
I SEE PD Home Intervention Dataset combining pre- and post-intervention survey data and assessments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hess, S.P., Levin, M., Akram, F. et al. The impact and feasibility of a brief, virtual, educational intervention for home healthcare professionals on Parkinson’s Disease and Related Disorders: pilot study of I SEE PD Home. BMC Med Educ 22, 506 (2022). https://doi.org/10.1186/s12909-022-03430-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03430-7