Abstract
Objectives
Advanced cancer patients face various symptoms, which can cause physical and psychological distress. As a multidimensional construct, spiritual well-being (SWB) may be an inner resource for dealing with these problems. Our study explored the impact of different dimensions of SWB on physical and psychological symptoms in advanced cancer patients admitted to a palliative care unit.
Methods
This cross-sectional study was conducted among 108 advanced cancer patients in the Hospice Ward, Shengjing Hospital of China Medical University. Patients completed questionnaires on SWB and cancer-related symptoms (insomnia, fatigue, pain, depression and anxiety) at the time of admission. Linear regression analysis was applied to determine the relationship between SWB (meaning, peace and faith) and symptom distress.
Results
SWB accounted for an additional variance of cancer-related symptoms (17.8% to 44.4%). Meaning was negatively associated with insomnia (β = -0.516, p < 0.001) and fatigue (β = -0.563, p < 0.001). Peace and faith were related to lower psychological symptoms, while meaning represented a positive effect on anxiety (β = 0.275, p = 0.036). Higher peace was associated with lower cancer pain (β = -0.422, p < 0.001).
Conclusions
Our findings suggested that achieving peace and faith appeared to function consistently as a positive resource for advanced cancer patients on depression, anxiety and pain, while meaning may serve to facilitate or hinder positive adjustment. Future studies should focus on the potential clinical implications by identifying the distinct dimension of SWB as symptom management targets in the palliative care practice.
Similar content being viewed by others
Introduction
Advanced cancer patients suffer from avariety of physical and psychological symptoms associated with cancer diagnosis and treatment. Patients were often poly-symptomatic frequently experiencing cancer-related symptoms such as insomnia, fatigue, pain, depression, and anxiety [1, 2], which may contribute to substantial distress. Cancer-related symptoms tend to co-occur, and each of these symptoms can lead to the maintenance of the others. For instance, the positive relationship between pain, anxiety and preoperative insomnia was found in colorectal cancer patients [3], and poorly managed pain was associated with anxiety, sleep disturbance and fatigue in breast cancer survivors [4]. The pain-fatigue-depression symptom cluster was also present in prostate cancer survivors [5]. More importantly, patients with multiple symptoms were more likely to have multiplicative rather than additive distress [6]. Cancer-related symptoms can adversely influence functional activities and quality of life (QoL), decrease treatment compliance, and increase the risk for hospitalizations [1, 2, 7]. Thus, the interactions between insomnia, fatigue, pain, and depression/anxiety are complex, warranting interventions that focus not only on the routine symptom management, but also on the additional improvements in holistic cancer care.
Since spiritual well-being (SWB) is the fourth dimension of QoL in terminal patients, spiritual care has been considered as a fundamental component of palliative care (PC) [8, 9]. Spiritual care at the end of life has been proven to be important to PC patients [10]. There were notable relationships between spiritual domains and patient-centered PC outcomes [11]. However, despite its clinical significance, spiritual care often goes unrecognized and untreated in Chinese PC units. Given the immaturity of palliative medicine [12], addressing spiritual problems has not been a priority among health care professionals who carry out PC [13]. For advanced cancer patients receiving PC, their fundamental purpose is to control physical symptoms rather than to meet spiritual needs within short-term hospital stays [8, 12]. Therefore, a better understanding of the influence of SWB on cancer-related symptoms may contribute to an improved identification of spiritual care as one route to support symptom management.
SWB has been conceptualized as composed of three dimensions: meaning, peace, and faith [8, 14]. Meaning indicates the cognitive aspect of SWB and may contribute to the maintenance of stability and goals amid life challenges. Peace describes the affective domain of SWB and may be experienced when an individual has reached acceptance in the face of adversity. Faith is a sense of comfort or strength one derives from one’s spiritual beliefs as a foundation for understanding the world [8, 14]. SWB has been recognized by PC specialists as a positive coping resource to support adjustment to cancer-related symptoms [9,10,11]. Several studies demonstrated the positive influence of SWB on symptom distress, with supportive evidence that SWB was correlated with lower severity of pain, fatigue, sleep disturbance, and anxious/depressive symptoms [6,7,8]. Yet, professionals have not always found it easy to implement SWB within the holistic cancer care [15], which may be largely due to the multidimensional nature. To our knowledge, little is known about how the distinct dimensions of SWB jointly affect cancer-related symptoms. Examining only the composite score of SWB can lead PC specialists to overlook significant differences about the dimensions’ relations with symptom experience, which may result in that spiritual care remains the least developed and most neglected component of PC [10].
Meaning, peace and faith suggest different features of SWB, and they are not invariably linked with better adjustment to cancer-related experiences. A systematic review indicated that meaning and peace were related to better QoL, whereas faith was not consistently associated with health outcomes [16]. Increase in peace was related to lower depression and anxiety, while changes in meaning and faith were unrelated to psychological distress [17]. In longitudinal studies, meaning and peace were related to improved mental health and lower distress, and faith was associated with perceived growth [18]. Furthermore, the sense of faith may prompt feelings of negative emotions, such as when one experienced challenge that violated one’s views of spiritual beliefs [18]. Specially for QoL dimensions in cancer patients, meaning and peace were positively related to social/family and functional well-being, while faith had a negative effect on physical and emotional well-being [19]. The above findings lend support to the argument that the relationship of SWB dimensions with salutary outcomes may be inconsistent. Overall, despite the protective effect of SWB against maladjustment, there is limited knowledge about how meaning, peace and faith differentially influence multiple symptom experiences among advanced cancer patients in the PC unit.
Supporting SWB and its meaningful dimensions is an under-explored area which may yield future advancements in the simultaneous management of cancer-related symptoms. Moreover, there is a need to culturally reflect on differences in the dimensions of SWB [6]. The purpose of the current study was to evaluate whether specific dimensions of SWB functioned as a resource for Chinese adults experiencing cancer-related symptoms. Understanding the distinct dimension of SWB may help us address spiritual care incorporated into PC purposefully and thereby to support PC patients in dealing with physical and psychological symptoms.
Methods
Ethical approval statement
The study was approved by the Ethics committee on Human Experimentation of China Medical University (reference number: 720042321006479) and complied with the 1964 Helsinki Declaration and its later amendments. All participants provided informed written consent prior to participation.
Study design and participants
A cross-sectional study was conducted of consecutive inpatients admitted to Shengjing Hospital of China Medical University between July 2019 and October 2020. Patients were recruited at the Hospice Ward as a baseline investigation of a prospective study [8]. Eligible patients were at least 18 years of age and had a confirmed diagnosis of solid cancer. Other eligibility criteria were that patients had a life expectancy < 6 months at the time of admission and provided clear responses to questionnaires in Chinese language. Exclusion criteria were that patients had (1) concomitant psychiatric disorders, (2) intellectual and/or cognitive impairments, (3) psychotropic drug usage within 7 days before admission, (4) drug or alcohol dependence, and (5) HIV-positive.
Procedures
Eligible patients were identified through chart review and discussion with physicians. After explaining the study purpose, advanced cancer patients were asked to complete all the psychometric instruments within 24 h of admission to Hospice Ward. Demographic information and medical history were obtained through medical record review.
Measures
Demographics and clinical variables
Demographic variables including age, gender, relationship status, and education were collected at admission. Diagnosis disclosure, first or subsequent visit, and Karnofsky Performance Scale (KPS) were determined by medical chart review.
SWB
The Functional Assessment of Chronic Illness Therapy-Spiritual Well-being (FACIT-Sp) consists of 12 items measuring SWB with three empirically validated subscales of 4 items: meaning, peace, and faith [20]. Participants rated on a five-point Likert-type scale (0 = “not at all” to 4 = “very much”). Subscale scores range from 0 to 16, with higher scores reflecting higher levels of SWB dimensions. Cronbach’s alphas for FACIT-Sp and its three subscales were 0.911, 0.76 (meaning), 0.703 (peace), and 0.914 (faith), respectively.
Insomnia
Insomnia was evaluated by the Athens Insomnia Scale (AIS) [21], which comprises 8 items rated on a 4-point Likert scale, ranging from 0 (no problem at all) to 3 (a very serious problem). The total score ranges from 0 to 24, with higher scores denoting higher insomnia. The Cronbach’s alpha for AIS in this study was 0.889.
Fatigue
Fatigue was assessed using the Cancer Fatigue Scale (CFS), which is a brief, valid, and feasible measure of fatigue for use with cancer patients [22]. The scale consists of 15 items, and each item is rated on a scale of 1 (not at all) to 5 (very much). Higher scores reveal more severe fatigue. The Cronbach’s alpha for the current sample was 0.866.
Pain
Cancer pain was assessed by the Numerical Rating Scales (NRS), which is one of the frequently used tools for assessing pain severity [23]. Patients were asked to verbally rate their pain on a scale from 0 to 10, with 0 equals no pain and 10 equals worst possible pain. The 11-point NRS is easy to administer verbally among advanced cancer patients admitted to the palliative setting [8, 14].
Depression and Anxiety
The Hospital Anxiety and Depression Scale (HADS) is a 14-item measure of depressive and anxious symptoms [24]. HADS consists of two subscales, with 7 items each rated on a 4-point Likert scale (0 = “not at all” to 3 = “very much indeed”). Higher scores on both subscales indicate more severe symptoms of depression and anxiety. Cronbach’s alphas for the depression and anxiety subscales were 0.877 and 0.865, respectively.
Statistical analysis
Descriptive statistics of study variables were presented with median, mean, standard deviation (SD), 95% confidence intervals (CI), number (N), and percentage (%) as appropriate. The distributions of cancer-related symptoms in covariates were tested by independent sample t test and one-way analysis of variance (ANOVA). Pearson’s correlation was used to examine associations among the continuous variables. Hierarchical regression analysis was used to evaluate the association of SWB dimensions with symptom experience (i.e., insomnia, fatigue, pain, depression, and anxiety) after adjusting for covariates, which were related to outcomes in univariate analysis (p < 0.05). In Step 1, covariates were added. Due to the high correlations among the FACIT-Sp subscales, meaning, peace and faith were adjusted in the stepwise regression in Step 2. Data including R2, adjusted R2 (Adj. R2), R2-changes, F, standardization regression coefficients (β), and p value were provided for each step in the regression model. The Statistical Package for the Social Sciences (SPSS, version 18.0) was employed to perform the statistical analyses, with a two-tailed probability value of < 0.05 recognized to be statistically significant.
Results
Characteristics of patients
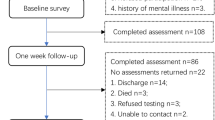
A convenience sample of 147 patients was originally recruited, and we received effective responses from 108 cancer patients (73.5%). The mean (SD) age was 65.23 ± 12.48 years. Approximately 75% of the patients were married or living with a partner, and 50.47% received middle school education. Most patients were aware of cancer diagnosis (65.71%), and were the first time to the Hospice Ward (77.78%). The mean (SD) of KPS was 47.83 ± 11.63, and 48 (45.28%) patients had a KPS score less than 50. Table 1 provided the descriptive statistics of SWB and cancer-related symptoms. The mean values were 24.12 ± 10.87 for SWB, 9.59 ± 3.74 for meaning, 7.67 ± 3.22 for peace, and 6.85 ± 4.98 for faith.
Univariate analysis
As shown in Table 2, t test indicated the significant association of depression (p = 0.018) and anxiety (p = 0.038) with diagnosis disclosure. Advanced cancer patients who knew their cancer diagnosis reported higher scores of HADS subscales. The correlations between study variables were presented in Table 3. SWB and its dimensions were negatively associated with cancer-related symptoms (r = ranged from -0.373 to -0.687; p < 0.001). Additionally, meaning, peace and faith correlated highly with each other (r = ranged from 0.706 to 0.757; p < 0.001).
Multivariate analysis
Tables 4 presented the hierarchical regression analysis of cancer-related symptoms after adjusting for covariates. The three dimensions of SWB accounted for an additional variance of cancer-related symptoms (17.8% to 44.4%) in Step 2. For insomnia-fatigue-pain symptoms, meaning or peace represented significant individual protective variables. Meaning was negatively associated with insomnia (β = -0.516, p < 0.001) and fatigue (β = -0.563, p < 0.001), and peace showed a significant association with cancer pain (β = -0.422, p < 0.001). Regarding psychological symptoms, peace and faith were negatively and significantly associated with depression and anxiety, but meaning represented a positive effect on anxiety (β = 0.275, p = 0.036). In addition, Additional file 1: Table A in the appendix also indicated the association between total score of FACIT-Sp and cancer-related symptoms, and SWB was proven to be a protective variable for these symptoms.
Discussion
The current study is the first to examine the association between the distinct dimensions of SWB and symptom experience, as referred by advanced cancer patients receiving hospital-based PC. Our central finding was that different dimensions of SWB presented the distinct value in the adjustment to cancer-related symptoms independent of sample characteristics. The present study highlights the importance of spiritual care in the integrated PC by distinguishing the dimensions of SWB among advanced cancer patients at admission.
Several researchers demonstrated Meaning/Peace as one factor associated with physical and psychological consequences in cancer patients [6, 16, 18, 25]. However, the three-factor structure of FACIT-Sp reflected the conceptual difference between meaning (cognitive dimension) and peace (affective dimension) in terminal cancer patients [26], indicating that meaning and peace may differentially correlate with cancer-related symptoms. Our findings showed that a sense of meaning can be an inner resource for advanced cancer patients when facing insomnia and fatigue. One potential explanation may be the coping strategies that patients adopted in face of advanced cancer. Positive reframing coping style was a significant predictor of the Meaning dimension [27]. Patients found a new meaning and purpose in their existence by looking at cancer-related challenges from a distinct perspective or by trying to get the best out of adversity [27]. Thus, meaning as a cognitive component of SWB may alleviate insomnia and fatigue by enabling patients to reevaluate their own symptoms experience of the PC situation.
The positive meaning-anxiety link was contrary to previous studies that Meaning/Peace component had the significant buffering effect against psychological symptoms [6, 27, 28]. The possible explanation was that providing a cognitive reframing on patients’ declining health and imminent death may be not beneficial for dealing with anxiety in response to cancer-related stress. Considered as one of emotional issues, anxious symptoms may be exacerbated from a cognitive perspective when patients strived for the meaning or purpose in their lives. However, the explanation about the negative effects of meaning is rather exploratory, and the association between meaning and anxiety deserves further investigations.
Concerning the affective domain, peace may be the dimension of SWB most closely associated with psychological symptoms. Under standardized estimate (β) sequence, peace had the strongest buffering effect against depression and anxiety, in agreement with previous studies found that there was a significant negative association between peace and psychological distress in cancer patients [17, 29, 30]. Bovero et al. demonstrated that a sense of peace contributed to relieving symptoms of depression and anxiety by adopting emotional regulation strategies (e.g., self-distraction and behavioral disengagement) [27]. According to positive emotions in positive psychology, peace and harmony are related to engaging in meaning‐in‐life behaviors [17, 31], which may reflect mechanisms underlying the adaptive value of finding peace as an affective support for advanced cancer patients.
Peace also emerged as the only dimension of SWB that was related to pain severity in our study. Cancer pain is a complex subjective experience associated with bio-psycho-spiritual factors [8, 14]. Depression and anxiety were associated with more severe pain, resulting in that cancer pain became intractable in the presence of psychological distress [32]. Sleight et al. found that meaning/peace buffered the negative effect of anxiety on physical well-being in cancer survivors. [25] We speculated that a sense of peace that can reduce depression and anxiety may further relieve pain severity, which may be a mechanism underlying the peace-pain association.
A greater faith was associated with lower psychological symptoms, which was in contrast to previous findings that meaning/peace had a greater association with improved mental health and lower psychological distress than faith in cancer patients [16,17,18]. Particularly, faith hindered the positive adjustment to cancer, such as an association between faith and adverse health outcomes [6, 19]. The mixed results when evaluating faith’s role in cancer patients may reflect cultural differences. Faith involves perceived comfort and strength derived from spiritual beliefs and practices. Faith of cancer patients who adhere to religion can be achieved by an omnipotent power or through a religious practice [7, 27]. Nevertheless, reliance on faith when one experiences events that violate one’s connection to a higher power may lead to negative religious beliefs (e.g., feeling abandoned by God and spiritual discontent), and thus may hinder favorable outcomes compared with meaning and peace [18, 29]. In opposition to a religious society, Chinese people tend to discover the meaning in life, find self-worth in the world, and explore the essence of university [19]. The search of faith may be a spiritual resource in helping Chinese cancer patients foster positive adjustment to psychological symptoms by repositioning themselves properly in the universe and establishing harmonious association with nature [19]. Therefore, a sense of faith may provide emotional regulation and greater resilience while facing depression and anxiety, making symptoms more tolerable and controllable.
Clinical implications
Our findings highlighted the distinct adaptive value of meaning, peace and faith on cancer-related symptoms, with potential clinical implications for improving symptom management. Although several interventions which are important in spiritual process have been shown to increase spirituality [8, 17], meaning, peace and faith have not been specifically distinguished and targeted in advanced cancer patients. Health care providers should explore the relevance of the distinct dimensions of SWB in the PC practice to soften symptom distress. For instance, pain is the most common and distressing symptom in advanced cancer, resulting in the particularly high priority of pain management in PC [14, 33]. Besides the pharmacological strategies, future researches should assess whether increasing peace as an intervention target in the plan of PC can decrease pain severity.
Limitations
Our findings should be interpreted within the context of study limitations. First, the study design was cross-sectional, without demonstrating a causal relationship between SWB and cancer-related symptoms. Next, the recruitment of patients was a convenience sampling in one university hospital, which limited the generalizability of our findings. Additionally, spiritual distress was not evaluated in our study while it may have clinical implications. Spiritual distress is an area worthy of future study in relation to physical and psychological symptoms [7]. Finally, our findings should be further replicated in larger studies and with chronic diseases other than cancer.
Conclusions
The present study suggested that the distinct dimensions of SWB empowered individuals to transcend cancer-related symptoms in a PC unit. Specifically, achieving peace and faith appeared to function consistently as a positive resource for advanced cancer patients on depression, anxiety and pain, while meaning may serve to facilitate (insomnia and fatigue) or hinder (anxiety) positive adjustment. Our findings have implications for incorporating spiritual care in the holistic PC and identifying the most important dimension of SWB as symptom management targets.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- PC:
-
Palliative care
- SWB:
-
Spiritual well-being
- QoL:
-
Quality of life
- NRS:
-
Numerical Rating Scales
- KPS:
-
Karnofsky Performance Scale
- FACIT-Sp:
-
Functional Assessment of Chronic Illness Therapy-Spiritual Well-being
- AIS:
-
Athens Insomnia Scale
- CFS:
-
Cancer Fatigue Scale
- NRS:
-
Numerical Rating Scales
- HADS:
-
Hospital Anxiety and Depression Scale
- SD:
-
Standard deviation
- CI:
-
Confidence intervals
- ANOVA:
-
One-way analysis of variance
References
Henson LA, Maddocks M, Evans C, et al. Palliative care and the management of common distressing symptoms in advanced cancer: pain, breathlessness, nausea and vomiting, and fatigue. J Clin Oncol. 2020;38(9):905–14.
Bail JR, Traeger L, Pirl WF, Bakitas MA. Psychological symptoms in advanced cancer. Semin Oncol Nurs. 2018;34(3):241–51.
Sun GW, Yang YL, Yang XB, et al. Preoperative insomnia and its association with psychological factors, pain and anxiety in Chinese colorectal cancer patients. Support Care Cancer. 2020;28:2911–9.
Schreier AM, Johnson LA, Vohra NA, Muzaffar M, Kyle B. Post-treatment symptoms of pain, anxiety, sleep disturbance, and fatigue in breast cancer survivors. Pain Manag Nurs. 2019;20(2):146–51.
Baden M, Lu L, Drummond FJ, Gavin A, Sharp L. Pain, fatigue and depression symptom cluster in survivors of prostate cancer. Support Care Cancer. 2020;28:4813–24.
Albusoul RM, Hasanien AA, Abdalrahim MS, Zeilani RS, Al-Maharma Y. The effect of spiritual well-being on symptom experience in patients with cancer. Support Care Cancer. 2022;30(8):6767–74.
Miller M, Kwekkeboom K, Cherwin C. The role of spirituality in symptom experiences among adults with cancer. Support Care Cancer. 2022;30:49–57.
Yang Y, Zhao X, Cui M, Wang S, Wang Y. Longitudinal changes in spiritual well-being and associations with emotional distress, pain, and optimism–pessimism: a prospective observational study of terminal cancer patients admitted to a palliative care unit. Support Care Cancer. 2021;29(12):7703–14.
Kelley AS, Morrison RS. Palliative care for the seriously ill. N Engl J Med. 2015;373(8):747–55.
Gijsberts MJHE, Liefbroer AI, Otten R, Olsman E. Spiritual care in palliative care: a systematic review of the recent European literature. Med Sci. 2019;7(2):25.
Steinhauser KE, Fitchett G, Handzo GF, et al. State of the science of spirituality and palliative care research part I: definitions, measurement, and outcomes. J Pain Symptom Manage. 2017;54(3):428–40.
Ning X. Hospice and palliative care research in mainland China: Current status and future direction. Palliat Med. 2019;33(9):1127–8.
Chung H, Harding R, Guo P. Palliative care in the greater China region: a systematic review of needs, models, and outcomes. J Pain Symptom Manage. 2021;61(3):585–612.
Yang Y, Cui M, Zhao X, et al. Association of pain management and positive expectations with psychological distress and spiritual well-being among terminally ill cancer patients admitted to a palliative care unit. BMC Nurs. 2023;22:96.
Jimenez-Fonseca P, Lorenzo-Seva U, Ferrando PJ, et al. The mediating role of spirituality (meaning, peace, faith) between psychological distress and mental adjustment in cancer patients. Support Care Cancer. 2018;26:1411–8.
Bai M, Lazenby M. A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med. 2015;18(3):286–98.
Davis LZ, Cuneo M, Thaker PH, et al. Changes in spiritual well-being and psychological outcomes in ovarian cancer survivors. Psychooncology. 2018;27(2):477–83.
Yanez B, Edmondson D, Stanton AL, et al. Facets of spirituality as predictors of adjustment to cancer: relative contributions of having faith and finding meaning. J Consult Clin Psychol. 2009;77(4):730–41.
Cheng Q, Liu X, Li X, et al. Improving spiritual well-being among cancer patients: implications for clinical care. Support Care Cancer. 2019;27:3403–9.
Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy-Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med. 2002;24(1):49–58.
Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48(6):555–60.
Okuyama T, Akechi T, Kugaya A, et al. Development and validation of the cancer fatigue scale: a brief, three-dimensional, self-rating scale for assessment of fatigue in cancer patients. J Pain Symptom Manage. 2000;19(1):5–14.
Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain. 2018;18(1):99–107.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta psychiatrica scandinavica. 1983;67(6):361–70.
Sleight AG, Boyd P, Klein WMP, Jensen RE. Spiritual peace and life meaning may buffer the effect of anxiety on physical well-being in newly diagnosed cancer survivors. Psychooncology. 2021;30(1):52–8.
Rabitti E, Cavuto S, Iani L, et al. The assessment of spiritual well-being in cancer patients with advanced disease: which are its meaningful dimensions? BMC Palliat Care. 2020;19:26.
Bovero A, Tosi C, Botto R, et al. The spirituality in end-of-life cancer patients, in relation to anxiety, depression, coping strategies and the daily spiritual experiences: a cross-sectional study. J Relig Health. 2019;58:2144–60.
McClain CS, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. Lancet. 2003;361(9369):1603–7.
Chaar EA, Hallit S, Hajj A, et al. Evaluating the impact of spirituality on the quality of life, anxiety, and depression among patients with cancer: an observational transversal study. Support Care Cancer. 2018;26(8):2581–90.
Gudenkauf LM, Clark MM, Novotny PJ, et al. Spirituality and emotional distress among lung cancer survivors. Clin Lung Cancer. 2019;20(6):e661–6.
Fredrickson BL. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. Am Psychol. 2001;56(3):218–26.
Money S, Garber B. Management of cancer pain. Curr Emerg Hosp Med Rep. 2018;6:141–6.
Zhao XX, Cui M, Geng YH, Yang YL. A systematic review and meta-analysis of randomized controlled trials of palliative care for pain among Chinese adults with cancer. BMC Palliat Care. 2019;18:69.
Acknowledgements
The authors would like to thank all the staffs who contributed to this study.
Code availability
N/A.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Project No.: 72004232).
Author information
Authors and Affiliations
Contributions
Yilong Yang: Formal analysis, Investigation, Writing-original draft, Writing-review & editing. Xinxin Zhao: Methodology, Investigation. Meng Cui: Investigation. Yumei Wang: Conceptualization, Methodology, Project administration, Supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Patients were well-informed about the purpose and contents of the present study by investigators. Written informed consent was obtained from all inpatietns included in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table A. Results of regression analyses exploring associations between spiritual well-being and cancer-related symptoms.
Additional file 2.
Raw data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, Y., Zhao, X., Cui, M. et al. Dimensions of spiritual well-being in relation to physical and psychological symptoms: a cross-sectional study of advanced cancer patients admitted to a palliative care unit. BMC Palliat Care 22, 137 (2023). https://doi.org/10.1186/s12904-023-01261-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-023-01261-x