Abstract
Background
The end of life represents a therapeutic context that acutely raises cultural and linguistic specificities, yet there is very little evidence illustrating the importance of such dynamics in shaping choices, trajectories and care practices. Culture and language interplay to offer considerable potential challenges to both patient and provider, with further work needed to explore patient and caregiver perspectives across cultures and linguistic groups, and provider perspectives. The objective of this study was to develop a critical, evidence-based understanding of the experiences of people from Culturally and Linguistically Diverse (CALD) backgrounds, and their caregivers, in a palliative care setting.
Methods
A qualitative study, using semi-structured interviews to explore key experiences and perspectives of CALD patients and caregivers currently undergoing treatment under oncology or palliative care specialists in two Australian hospitals. Interviews were digitally audio recorded and transcribed in full. A thematic analysis was conducted utilising the framework approach.
Results
Sixteen patients and fourteen caregivers from a range of CALD backgrounds participated in semi-structured interviews. The research identified four prevalent themes among participants: (1) Terminology in the transition to palliative care; (2) Communication, culture and pain management; (3) (Not) Talking about death and dying; and, (4) Religious faith as a coping strategy: challenging the terminal diagnosis.
Conclusions
CALD patients and caregivers’ experiences are multifaceted, particularly in negotiating linguistic difficulties, beliefs about treatment, and issues related to death and dying. Greater attention is needed to develop effective communication skills, recognise CALD patients’ particular cultural, linguistic and spiritual values and needs, and acknowledge the unique nature of each doctor-patient interaction.
Similar content being viewed by others
Background
The transition to palliative care is challenging for patients and their loved ones [1, 2]. Culturally and linguistically diverse (CALD) populations may need extra support [3], as their experience of transition may entail additional complications around language and cultural values, including barriers to communication and isolation from the broader community. While doctor-patient-caregiver communication around transitions to palliative care has been shown to be complex and prone to interpersonal difficulties [1, 4, 5], cultural and linguistic diversity further complicates doctor-patient communication and treatment options, and the decision to cease potentially life-prolonging treatment [4, 6,7,8,9]. In the transition to palliative care, and cultural expectations around death and dying more broadly, CALD patients and families must navigate a range of challenges across the domains of formal and informal care. This study aimed to explore the experiences and perspectives of both CALD patients and family caregivers, revealing various implications for practice for oncologists and palliative care specialists treating CALD patients in the Australian hospital system. Specifically, we focus on the transition to palliative care.Footnote 1 to explore attitudes towards, and understandings and experiences of, end-of-life care among CALD patients and their caregivers.
Cultural and linguistic diversity when approaching the end of life
Australia is culturally and linguistically diverse, with a range of cultural values and beliefs shaping illness experiences, access to care and interactions with healthcare providers [10]. CALD populations face particular challenges when it comes to accessing healthcare in Australia and in most western nations, including issues related to language and communication, cultural preferences, and isolation [10,11,12]. In relation to end of life care, patients and caregivers from CALD backgrounds have varying preferences regarding the disclosure of diagnosis and prognosis and the management decision-making in health/care [13, 14]. Internationally, there have been some attempts to understand the particular needs of diverse populations in end-of-life care [15, 16], yet further in-depth, patient-focused work still remains necessary [17, 18].
Cultural expectations, decision-making and care
Although full disclosure of diagnosis and prognosis is not uniformly practiced in all cultures, it is central to the Western biomedical system [19]. In Australia, doctors are trained in breaking ‘bad news’ to patients and families, particularly when transitioning patients to palliative care [20, 21]. This system is based on the principles of medical ethics, with the notion of ‘patient autonomy’ at its centre [22, 23]. As such, the right of the patient to know their health status and make decisions about treatment options is considered a key facet of medical care. However, some CALD patients and caregivers – particularly those who are older or less ‘acculturated’ to western biomedical contexts – may prioritise a family decision-making model when it comes to treatment decisions [22, 24], or indeed, may defer decisions to their doctors who may be afforded significant cultural authority [7, 25, 26]. As such, Western biomedical notions of patient-centred care may not resonate with patients and caregivers from different cultural backgrounds who have considerably different expectations of medical systems [26,27,28].
Communication, culture and palliative care
Doctor-patient communication around diagnosis/prognosis and treatment decision-making is informed by a range of lay and expert interpretations of illness and mortality. Lay interpretations in particular are highly culturally variable and can pose particular challenges for CALD patients and caregivers. For example, the words ‘cancer’ or ‘palliative’ are avoided across a number of cultural contexts because of their direct association with death [25, 29]. There are several explanations for this, including: persistent taboos around cancer and mortality, the idea that speaking of cancer will hasten death, and the idea that the timing of death can be known only by god [25]. Diagnostic/prognostic disclosure is thus a culturally-laden form of communication with considerable implications for palliative care. Furthermore, in the palliative care context, communication necessarily extends beyond doctor-patient relations to include the family, which is often viewed as the appropriate ‘unit of care’. Yet in CALD contexts, family caregivers may be called upon to perform multiple types of caring roles: It is not unusual, for instance, for family caregivers to take on the role of interpreting during medical examinations [30]. Despite the greater accuracy of professional interpreters in conveying information to patients [31], many patients prefer the familiarity of family caregivers [7]. However, the use of family members as interpreters can also be fraught, with tensions around who controls the actual consultation process, and the information conveyed between doctor and patient as mediated by the interpreting caregiver [25, 30, 32]. As we discuss below, such multifarious and complex factors may result in additional confusion, misunderstandings and frustrations in the transition to palliative care for CALD patients and caregivers.
Methods
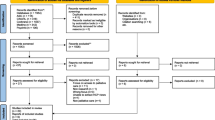
This study, while discrete, was part of a broader program of research exploring the lived experience of the end of life. We used qualitative semi-structured interviews to explore the experiences of CALD patients’ and caregivers’ transition to palliative care. Following local and national ethics approval [HREC approval: HREC/14/MHS/22], potential participants were approached by the clinical members of the research team during routine clinic appointments or during inpatient stays at two metropolitan hospitals in south-east Queensland, Australia. When appropriate, potential participants were approached with the aid of an accredited professional interpreter.Footnote 2 Each patient and/or caregiver was given ample opportunity to discuss the study and the context of the interview. Participants who were interested in taking part in the study were then contacted to schedule a convenient time and location for the interview to take place. Eligible participants were people over the age of 18 from CALD communities, defined as those from non-Indigenous ethnic/language groups other than the English-speaking majority in Australia. Patients were approached based on their CALD status as noted in hospital records, who were currently undergoing treatment under oncology or palliative care specialists within the two hospitals. While we did not limit recruitment to specific diagnoses or stage of disease, eligible patients were those who were no longer undergoing potentially curative treatment, and were being transitioned to palliative care. Caregivers were approached based on their provision of care for patients from CALD communities, or based on their own CALD status.
A purposive sampling strategy was used, and coordinated through whole research team meetings, including the clinical members of the research team who approached participants. The process was iterative, and regularly reviewed to update the strategy and facilitate discussion around which patients and carers to approach in order to include participants from a range of backgrounds, including spread across age, sex, languages spoken, inpatient/outpatient status, and public/private care settings. All interviews, conducted during 2014, were digitally audio-recorded and transcribed in full in English.Footnote 3 During the interviews we focused on the following domains: experiences and understandings of palliative care; communication, needs and values in the context of hospital care; experiences of being cared for/caring at a time of serious illness; and, experiences and perspectives on formal/institutional support/care for patients and caregivers with CALD backgrounds. The COREQ qualitative research reporting checklist was used to ensure comprehensive reporting [33].
Analysis
Data analysis took place concurrently with the qualitative fieldwork over a period of 7 months. In line with sociological interpretive traditions, our approach to analysis focused on reaching a nuanced understanding of the range of perspectives, within systems of beliefs and life experiences more broadly [34]. We employed the framework approach of qualitative data analysis using NVivo 10 software to systematically analyze the transcripts. We employed the following steps: (1) Familiarization: the researchers reviewed the manuscripts. (2) Identification of framework: key themes were identified around which the data were organized. (3) Indexing: application of themes to text. This stage involved using NVivo 10 to label and arrange each excerpt of text, use of a word or term, or research note related to each participant and transcript. This produced several (complicated and overlapping) lists including data and notes from several participants according to each theme. (4) Charting: use of headings and sub-headings to build up a picture of the data as a whole. Each thematic ‘index’ was discussed by three research team members, with Author A leading the development of summaries or ‘charts’ for each thematic area: one ‘overall’ summary, along with one summary of patient participants and one for caregiver participants. (5) Mapping and interpretation: in which associations were clarified and explanations developed. This involved finding associations between and within themes, moving towards and developing explanations for the findings in line with our research aims [35]. The three research team members participated in all stages of the analysis and independently coded the data, and these separate analyses were then cross-checked to uncover related and/or deviant cases/themes, and to develop an overall interpretation of the data. Once a theme was identified in the transcripts, interviews were searched for related comments using constant comparison in order to further develop themes [36]. In this way the richness of the data was retained, while interrelated associations were uncovered. Analytical rigor was augmented by constant comparison and searching for negative cases during code and theme development [35,36,37]. Following ongoing concurrent analysis of the interviews, informed by the concept of saturation in qualitative research [38]. the researchers agreed that no new themes relating to the topics of study were likely to be identified from further interviews.
Results
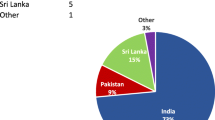
Participants were recruited from 1 public hospital, and 1 private hospital which had provision for public patients through government-funded beds within the private setting. Twenty-two patients and 17 caregivers volunteered to participate, 30 of whom were recruited (16 patients and 14 caregiversFootnote 4). All of the patients had advanced cancer, were no longer receiving potentially curative treatments, 8 of the patients were hospital inpatients at the time of interview, and 8 were outpatients. The caregivers were all family members of the patient for whom they were caring, including daughters (n = 4), wives (n = 4), husbands (n = 4), a granddaughter, and an ex-wife. Several participants spoke multiple languages; the majority of participants spoke some English. Five patients and 5 caregivers were interviewed with the assistance of a professional accredited interpreter. These participants were given a participant information and consent form in a language of their choosing, and were given time to ask any questions about the project and their participation through the interpreter present, prior to giving written consent. Four of the caregiver participants were caring for patients who were also participating in interviews. For these patient-carer dyads, participants were given the option to be interviewed separately or together. Two of patient-carer dyads chose to be interviewed together. Semi-structured interviews lasted up to 60 min (median: 33 min). Table 1 provides a summary of participant characteristics.
Here we report on the emergent themes following our systematic analysis of the interview transcripts. Participants offered varying degrees of information about their experiences and perspectives on their cancer, supportive and/or palliative care. What was clear, throughout the participant cohort of both patients and caregivers, was that managing hospital treatment for serious illness had the potential to entail significant physical and emotional vulnerability, compounded by communication problems and cultural divergence. Our analysis revealed four predominant themes: (1) Terminology in the transition to palliative care; (2) Communication, culture and pain management; (3) (Not) Talking about death and dying; and, (4) Religious faith as a coping strategy: challenging the terminal diagnosis.
Terminology in the transition to palliative care
A key theme within the interviews was the variable, or complete lack of, understanding of the concept and meaning of palliative care. Given that there is no equivalent term for ‘palliative care’ in many languages, the majority of participants experienced difficulties in understanding the meaning of the term, and the consequences of the transition to palliative care for treatment and prognosis. As shown in the indicative quotes in Table 2, the expectation of more traditional forms of home-based care for the dying (provided by family or informal caregivers) meant that hospital-based palliative care was difficult to comprehend for several participants. At times, patients confused in-patient palliative care with ongoing ‘active’ treatment that would be aimed at prolonging their lives. That is, some patients believed a return home was indicative of the onset of the dying process and thus, in contrast, that remaining in hospital entailed hope for recovery. Many caregivers lacked a working understanding of the meaning of palliative care, and we heard many accounts of caregivers around ‘doing homework’ in order to understand what ‘palliative’ meant and what ‘palliative care’ entailed. Other participants wished to avoid discussions around terminal prognoses and were reluctant to discuss plans for end of life care. In still other cases (and as with diagnosis), patients and caregivers felt that the meaning of palliative care had been explained by clinicians in ways that were not clear. Thus we found a number of difficulties in participants’ understandings and comprehension of the notion of ‘palliative care’, the precise nature of which varied across patients and caregivers. While various cultural ‘taboos’ around dying played a role, so too did difficulties at the level of translation including the lack of ability to translate and explain the term. What ‘palliative’ meant was, for many participants, lost in translation. Alternatively, in other cases, where ‘palliative’ was taken by participants to be synonymous with approaching the end of life, use of the term was consciously withheld by clinicians at the request of family caregivers.
Communication, culture and pain management
A key facet of the transition to palliative care in Australia is the focus on pain and symptom management for patients with advanced cancer [39, 40]. During the interviews with both patients and caregivers, we heard multiple accounts of the difficulties in communicating with clinicians in terms of expectations of treatment, which were shaped by the variable understandings of and meanings attached to palliative care (discussed above). This was most evident in relation to pain and symptom management, with the interviews revealing a variety of different cultural scripts around the expectation of pain and pain relief, as shown in Table 3. As noted above, a significant proportion of the patients we interviewed talked of their belief that by virtue of being in hospital and receiving hospital-based expert medical treatment, they might or would get better and recover. Moreover, the majority of participants (both patients and caregivers) discussed the importance of stoicism and tolerance in the face of physical pain. Thus, participants told us that, when asked about pain by clinicians, patients were likely to down-play the extent of their pain, potentially making it difficult for clinicians to manage pain effectively, or indeed understand the patient experience. One participant provided a poignant anecdote about how this initial hesitation was overcome by a nurse who persisted with their queries until the patient finally felt they could rely on them and fully disclose the extent of their discomfort. For others, communication with clinicians about pain and symptoms was very difficult in the absence of an interpreter. For a few participants, this was experienced as frustrating and isolating, as they felt they could not adequately communicate their needs, nor were their needs well-understood by clinicians. Caregivers discussed similar issues with us, and were often particularly concerned that the Australian medical system was not well equipped to deal with either their cultural or linguistic requirements.
(Not) talking about death and dying
The avoidance of talking about cancer, death and dying was a predominant theme within the participants’ accounts, and one that was explicitly linked to cultural background (see Table 4 for indicative quotations). Talking about death and dying, or terminal illness was frequently associated by participants with ‘giving up’ or hastening death. That is, participants understood death to be more likely to happen, or more likely to happen quickly, if openly acknowledged, verbalised or discussed. As such, participants spoke of strictly limiting talk about cancer or the end of life, as it was in stark contrast to the strong desire to maintain hope. Both patients and caregivers within our sample spoke of their unwillingness to talk about the prospect of dying as part of their culture or underlying belief system. Such discussions were described as being viewed as demoralising and unnecessarily upsetting for those who are already unwell. Such active avoidance of discussing the terminal diagnosis was also linked to issues around disclosure of information, as well as religion, faith and hope, as we discuss below.
Religious faith as a coping strategy: Challenging the terminal diagnosis
Many patients – often with the support of their caregivers – talked about the centrality of their faith and religion as a means of coping, as shown in Table 5. Patients and caregivers frequently commented on their preference to focus on religious faith (which they associated with hope) instead of medical futility (which they associated with ‘giving up’ and death). As one caregiver noted about the counselling offered to them and their partner, talking about particular problems only made it more difficult to cope. For some patients, religious faith presented a challenge to their doctor’s expertise and authority, with implication that God knows better, or that God would intervene and assist their healing. One participant admonished herself for saying the word ‘cancer’, explaining this this would anger God, and chose instead to attribute any negative wording about her condition to medical reports by prefacing them with ‘according to the report’. Faith and religion was a particularly prominent coping strategy among our participants. These belief systems were frequently talked about by participants as part of the cultural fabric with which experiences of illness and care were interwoven.
Discussion
A significant body of existing research has revealed multiple cultural factors which can shape experiences of discussing and managing death and dying [6, 13]. The findings presented in this paper have provided additional insight into the experiences of CALD patients and their caregivers, and how they manage the challenging nexus of formal care; beliefs about treatment, death and dying; linguistic difficulties; communication around diagnosis, prognosis, pain and symptoms, with clinicians. For clinicians, understanding these complex dynamics is important for effectively communicating, establishing trust and making decisions with both CALD patients and their families. This requires a nuanced negotiation and understanding of both the broader cultural perspective of the patient and the interpersonal relationships within the family unit of care.
Our findings novel data from during the transition to palliative care, which support previous research highlighting the difficulties of communicating with CALD patients about the meaning of palliative care [4, 9], as understandings of the context and services offered by palliative care were incomplete or absent for the majority of participants. The data highlights the importance of clinicians’ ability to identify and remedy misunderstandings about (or lack of understanding of) the meaning and context of palliative care, and what patients and caregivers might expect from this stage in the patient’s care plan. Indeed, our findings point to the significance of ensuring the meaning of language is understood, while maintaining a culturally sensitive disposition (though this is no straightforward task). Moreover, given that several participants described their deliberate avoidance of such discussions, our findings provide new insight into the importance of sensitivity to cultural taboos and scripts around cancer, death and dying.
The findings presented here suggest that such cultural taboos are interpreted in a variety of ways with a variety of consequences. While some (sometimes quite specific) cultural taboos exist in relation to discussing cancer or death, the primary reason given by our participants for such avoidance strategies was the desire to maintain hope and, in the case of patients withholding their status from loved ones, to prevent suffering or concern. In many cultures (including in many western contexts) the maintenance of hope is particularly pertinent approaching the end of life [41], where the transition to palliative care may be seen as giving up hope and provides challenges in terms of denial and acceptance [42]. While the majority of participants recounted avoiding talking about the terminal diagnosis, all of the patients we interviewed were receiving treatment and transitioning to palliative care, suggesting difficulties in communicating the full implications of the transition to palliative care (whether because of difficulties of language, conversational reticence, or avoidance as discussed above). That is not to say that patients or their caregivers were ignorant or uninformed about the details of their diagnosis, but rather that they frequently did not wish to verbalise or discuss them. While such accounts at the end of life are hardly exclusive to CALD patients and caregivers [40,41,42,43], our findings point to the complex interplay of culture and care in the every day experience of the transition to palliative care for CALD patients and caregivers.
Successfully engaging in discussions with CALD families around palliative care issues, then, is clearly not as straightforward as simply identifying a particular nationality or cultural background and the associated beliefs and norms, which would amount to a form of cultural stereotyping. Instead, a patient or caregiver’s willingness (or disinclination) to discuss cancer and dying can be recognised as necessarily influenced by a multitude of factors, including individual biography, family relationships, educational attainment and cultural background including, most notably in this study, elements of faith and hope. This highlights some of the challenges palliative care and oncology clinicians may face when working with CALD patients and caregivers, and the importance of approaching each case as unique, with good communication between clinicians and the patient about their particular cultural, linguistic and spiritual values and needs. A number of researchers have argued the importance of clinicians actively exploring case-by-case cultural preferences for how end of life contexts are approached, in particular around patient and caregiver preferences for decision-making and information about their diagnosis and prognosis [8, 22, 26].
Our study has various limitations which are somewhat similar to those faced by clinicians involved in the transition to palliative care. Given the linguistic barriers, the sensitive topic of the interviews, and the conducting of interviews within a busy hospital setting (albeit in a private room), conversations between the researchers and participants were at times stunted, short, and interrupted. Our participants were recruited from two hospitals in one Australian city. As such, our findings may not be indicative of the experiences of CALD patients and caregivers elsewhere. Participants self-selected by volunteering, and were from a wide range of cultural backgrounds, with varying levels of health-literacy in relation to the Australian health system. It is noteworthy to stress again that our findings should not be generalised to all CALD patients and caregivers. Indeed, we reiterate here the almost infinite spectrum of experience for those within CALD communities, and the use of ‘CALD’ to describe a static or homogenous group, or indeed as particular categories (e.g. country of birth), as unhelpful. Finally, we note here the complexities of interviews conducted in English with participants for whom English is not their first language, or through an interpreter, and the potential consequences for data collection, analysis and reporting.Footnote 5 The process of cross language qualitative research has been shown to be complicated and often flawed [44]. While we engaged with issues around competence (using only accredited interpreters) and style (using consecutive interpreting), as well as strategies for building rapport (including making the interpreter ‘visible’ and part of the conversation), we acknowledge the limitations of having an interpreter present, and the limitations in terms of translation of data [44, 45].
Conclusions
CALD patients and caregivers’ experiences are multifaceted, particularly in negotiating linguistic difficulties, beliefs about treatment, and issues related to death and dying. Greater attention is needed to develop effective communication skills, recognise CALD patients’ particular cultural, linguistic and spiritual values and needs, and acknowledge the unique nature of each doctor-patient interaction. Our findings point to some of the shared barriers and challenges experienced by CALD patients and caregivers in the transition to palliative care which can be broadly attributed to a lack of cultural and linguistic concordance with the Australian hospital system, and the clinicians therein, as well as revealing the difficulties in dealing with sensitive topics such as the end of life. Future research focusing on the meanings of various serious, life-limiting or terminal illnesses is needed across a diverse range of CALD patients and caregivers to better understand CALD experiences of the Australian health system and the ways by which culture and biography inflect illness (and care) experience. Further, to explore what can be learned from CALD communities as well as how to include and engage with CALD populations to continue to improve outcomes.
Notes
We define the transition to palliative care as the referral and transfer to the care of a palliative care service. This transitional process may entail initial or ongoing consultation with a palliative care specialist within the current clinical setting, and may occur alongside potentially curative treatment, but eventually involves movement to another setting under the care of a palliative care service.
Participants were approached using an interpreter in cases where participating clinician researchers determined the need for an interpreter as part of the patients care/consultations. That is, if a patient requested, or was deemed by clinicians to require an interpreter for their hospital appointments, we also used an interpreter to approach them about participation in the study.
All interviews were conducted by the same research assistant interviewer, a sociologist with experience in conducting qualitative interviews, who was female and from an Anglo-Australian background. The interviewer was supported by the other members of the research team, including regular debriefing, redevelopment of the interview schedule and strategies/approaches to interviewing people within sensitive or vulnerable contexts, and interviewing through interpreters.
Thirty nine potential participants were approached in total, all of whom initially agreed to participate; six dropped out of the study following initial interest and prior to taking part in an interview; three participants were not interviewed due to repeated difficulties in scheduling and availability.
For example, several of our codes and subthemes were clear when getting a ‘whole’ sense of an interview transcript, but because of differences in linguistic style or proficiency in English among our participants, do not lend themselves straightforwardly to being depicted through quotations within a paper in a conventional sense. A consequence of this is that some participants’ voices are not privileged (or seemingly valued) within this paper, and as a research team we acknowledge the contribution made by all participants, and the value of every participant’s data within our analytic process.
Abbreviations
- CALD:
-
Culturally and Linguistically Diverse
- COREQ:
-
COnsolidated criteria for REporting Qualitative research
- HREC:
-
Human Research Ethics Committee
References
Broom A, Kirby E. The end of life and the family: hospice patients' views on dying as relational. Sociology of Health and Illness. 2013;35(4):499–513.
Broom A. Dying: a social perspective on the end of life. Surrey, England: Ashgate; 2015.
Broom A, Good P, Kirby E, Lwin Z. Negotiating palliative care in the context of culturally and linguistically diverse patients. Intern Med J. 2013b;43(9):1043–6.
Broom A, Kirby E, Good P, et al. The art of letting go: referral to palliative care and its discontents. Soc Sci Med. 2013c;78:9–16.
Kirby E, Broom A, Good P, et al. Families and the transition to specialist palliative care. Mortality. 2014;19(4):323–41.
Kaufert JM, Lavallee M. End-of-life decision making among aboriginal Canadians: interpretation, mediation, and discord in the communication of "bad news". J Palliat Care. 1999;15(1):31–8.
Robb N, Greenhalgh T. "You have to cover up the words of the doctor": the mediation of trust in interpreted consultations in primary care. J Health Organ Manag. 2006;20(5):434–55.
Barclay JS, Blackhall LJ, Tulsky JA. Communication strategies and cultural issues in the delivery of bad news. J Palliat Med. 2007;10(4):958–77.
Kirby E, Broom A, Good P, Bowden V, Lwin Z. Experiences of interpreters in supporting the transition from oncology to palliative care: a qualitative study. Asia Pac J Clin Oncol. 2017;13(5):e497–505.
Clark K, Phillips J. End of life care - the importance of culture and ethnicity. Aust Fam Physician. 2010;39(4):210–3.
Rao DV, Warburton J, Bartlett H. Health and social needs of older Australians from culturally and linguistically diverse backgrounds: issues and implications. Australas J Ageing. 2006;25(4):174–9.
de Graaf FM, Franke AL, van den Muijsenbergh ME, van der Geest S. ‘Palliative care’: a contradiction in terms? A qualitative study of cancer patients with a Turkish or Moroccan background, their relatives and care providers. BMC Palliat Care. 2010;9:19.
de Graaff FM, Francke AL, van den Muijsenbergh ME, van der Geest S. Talking in triads: communication with Turkish and Moroccan immigrants in the palliative phase of cancer. J Clin Nurs. 2012;21:21–2.
Xue D, Wheeler JL, Abernethy AP. Cultural differences in truth-telling to cancer patients: Chinese and American approaches to the disclosure of ‘bad news’. Progress in Palliat Care. 2011;19(3):125–31.
Perkins HS, Cortez JD, Hazuda HP. Cultural beliefs about a Patient’s right time to die: an exploratory study. J Gen Intern Med. 2009;24(11):1240–7.
Gysels M, Evans N, Meñaca A, et al. Culture is a priority for research in end-of-life care in Europe: a research agenda. J Pain Symptom Manag. 2012;44(2):285–94.
Huang YL, Yates P, Prior D. Accommodating the diverse cultural needs of cancer patients and their families in palliative care. Cancer Nurs. 2009;32(1):E12–21.
Goodall KT, Newman LA, Ward PR. Improving access to health information for older migrants by using grounded theory and social network analysis to understand their information behaviour and digital technology use. Eur J Cancer Care. 2014;23(6):728–38.
Gordon D. Tenacious assumptions in western medicine. In: Lock M, Gordon D, editors. Biomedicine Examined. Dordrecht: Kluwer Academic Publishers; 1988. p. 19–56.
Girgis A, Sanson-Fisher RW. Breaking bad news: consensus guidelines for medical practitioners. J Clin Oncol. 1995;13(9):2449–56.
Butow P, Tattersall MHN, Clayton J, Goldstein D. Breaking bad news and truth disclosure in Australia. In: Surbone A, Zwitter M, Rajer M, Stiefel R, editors. New challenges in communication with Cancer patients. Boston, MA: Springer US; 2013. p. 377–87.
Blackhall LJ, Murphy ST, Frank G, et al. Ethnicity and attitudes toward patient autonomy. J Am Med Assoc. 1995;274(10):820–5.
Beauchamp TL, Childress JF. Principles of biomedical ethics. New York: Oxford University Press; 2001.
Kwak J, Haley W. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45:634–41.
Butow P, Lobb E, Jefford M, et al. A bridge between cultures: interpreters’ perspectives of consultations with migrant oncology patients. Support Care Cancer. 2012;20(2):235–44.
Chiu C, Feuz M, McMahan R, et al. “Doctor, make my decisions”: decision control preferences, advance care planning, and satisfaction with communication among diverse older adults. J Pain Symptom Manag. 2016;51(1):33–40.
Huang X, Butow P, Meiser B, Goldstein D. Attitudes and information needs of Chinese migrant cancer patients and their relatives. Aust NZ J Med. 1999;29(2):207–13.
Mitchison D, Butow P, Sze M, et al. Prognostic communication preferences of migrant patients and their relatives. Psycho-Oncology. 2012;21(5):496–504.
Broom A, Kirby E, Good P, et al. The troubles of telling: managing communication about the end of life. Qual Health Res. 2014;24(2):151–62.
Gray B, Hilder J, Donaldson H. Why do we not use trained interpreters for all patients with limited English proficiency? Is there a place for using family members? Aust J Prim Health. 2011;17:240–9.
Farini F. The pragmatics of emotions in interlinguistic healthcare settings. Res Lang. 2013;11:163.
Leanza Y, Boivin I, Rosenberg E. Interruptions and resistance: a comparison of medical consultations with family and trained interpreters. Soc Sci Med. 2010;70(12):1888–95.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Charmaz K. ‘Discovering’ chronic illness: using grounded theory. Soc Sci Med. 1990;30(11):1161–72.
Pope C, Ziebland S, Mays N. Analysing qualitative data. In: Pope C, Mays N, editors. Qualitative research in health care. 3rd ed. Oxford: Blackwell Publishing; 2006. p. 63–81.
Ezzy D. Qualitative analysis. Allen and Unwin: Australia; 2002.
Fitzpatrick R, Boulton M. Qualitative research in health care: the scope and validity of methods. J Eval Clin Pract. 1996;2:123–30.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies. Qual Health Res. 2015;26:1753–60.
Boström B, Sandh M, Lundberg D, Fridlund B. Cancer-related pain in palliative care: patients’ perceptions of pain management. J Adv Nurs. 2004;45(4):410–9.
Mitchell G. Palliative care in Australia. Ochsner J. 2011;11:334–7.
Borneman T, Stahl C, Ferrell BR, Smith D. The concept of hope in family caregivers of patients at home. J Hosp Paliat Nurs. 2002;4(1):21–33.
Zimmerman C. Death denial: obstacle or instrument for palliative care? An analysis of clinical literature. Sociol Health Illn. 2017;29(2):297–314.
Markovic M, Manderson L, Wray N, Quinn M. He’s telling us something. Anthropol Med. 2004;11(3):327–41.
Squires A. Methodological challenges in cross-language qualitative research: a research review. Int J Nurs Stud. 2009;46:277–87.
Temple B. Crossed wires: interpreters, translators, and bilingual workers in cross-language research. Qual Health Res. 2002;12(6):844–54.
Acknowledgements
The authors thank the study participants who generously offered their time and crucial insight into this research topic.
Funding
The authors gratefully acknowledge the interviewed participants and the financial support of the Australian Research Council (nos. LP120200268 and DE150100285) and the RACP Foundation (Cottrell Research Establishment Fellowship).
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to ethics approval restrictions, but are available from the corresponding author on reasonable request from researchers who meet the criteria for access to confidential data.
Author information
Authors and Affiliations
Contributions
The project was designed and developed by AB, EK, ZL and PG. Data was collected by a research assistant with support from EK and AB. Data analysis was led by AB and EK with substantial input from ZL, PG, KK and HB. All authors contributed to the drafting and revising of the manuscript, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was granted by Mater Human Research Ethics Committee (HREC) (NHMRC certified; approval number: HREC/14/MHS/22). Written informed consent was obtained by all participants prior to each interview.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kirby, E., Lwin, Z., Kenny, K. et al. “It doesn’t exist…”: negotiating palliative care from a culturally and linguistically diverse patient and caregiver perspective. BMC Palliat Care 17, 90 (2018). https://doi.org/10.1186/s12904-018-0343-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-018-0343-z