Abstract
Background
Palliative care practitioners are increasingly caring for patients and families from diverse cultural backgrounds. There is growing awareness of the influence of culture on many aspects of care in the palliative phase of an illness. However, disparities have been noted in the provision of palliative care to patients from culturally diverse backgrounds and challenges have been reported in meeting their needs and those of their families.
Method
A qualitative systematic review of research papers identified through searching four databases. Papers were screened against inclusion criteria within the timeframe of January 2012 to March 2022. Data was extraction from all included studies and methodological quality assessed utilising the Critical Appraisal Skills Programme Tool. Thematic analysis followed Braun and Clarke’s framework and the review is reported in line with PRISMA guidelines.
Findings
The search yielded 1954 results of which 26 were included for appraisal and review. Four themes were identified: communication and connection, the role of the family in death and dying, the role of education in addressing uncertainty, and institutional and societal factors. The findings highlighted challenges of communication and a fear of acting in a culturally insensitive way, the pivotal role of the family, the need for an individualised approach to care, the universality of needs when approaching end of life and the need for education of practitioners.
Conclusion
These findings suggest that healthcare practitioners draw on their existing skills to adapt their practice to meet the needs of patients from culturally diverse backgrounds. However, results also indicate a need for further education and identification of educational approaches best suited to supporting healthcare professionals in practice.
Similar content being viewed by others
Introduction
The care provided to the dying should reflect the kind of society we have created and live in [1] and the philosophy of Cecily Saunders (1918–2005), that care and treatment of the ‘whole person’ is best facilitated by a team, is a cornerstone of modern palliative care throughout the world [2]. Culture is an integrated pattern of human behaviour that includes language, thoughts, actions, customs, beliefs, and institutions of racial, ethnic, and social or religious groups [3]. Culture incorporates learned, shared knowledge of values, beliefs, and lifeways, and has rules that influence attitudes and behaviours that can be overt or covert [4]. Thus, culture is multifaceted, fluid and complex creating the potential to impact significantly on both health and illness [5].
The number of persons currently residing outside their country of origin has never been greater and numbers of migrants have increased progressively over the past thirty years [6]. According to the International Organization for Migration in 2019, Europe hosted 82 million international migrants, North America 59 million and Northern Africa and Western Asia (combined) 49 million [7]. Migration patterns are a constantly evolving phenomenon and occur for a variety of reasons such as work opportunities, education, lifestyle factors and conflict/war. The World Health Organization (WHO) highlights that healthcare for migrant and refugee populations should be provided in a gender-sensitive, culturally, and linguistically appropriate manner without stigma [8]. Disparities in the care experiences of culturally diverse patients exist [9] identifying a lack of knowledge of services [10], inadequate exchanges of information [11, 12], difficulties with the use of interpreters [9], difficulties explaining feelings and emotions [13], issues around disclosure of serious illness [14] and a focus on cultural background rather than the individuals experience [15].
If culture is the lens through which we view the world [16], then it must be acknowledged that the culture of healthcare practitioners, healthcare organisations and wider society will also impact interactions with culturally diverse patients and their families. Providing healthcare to patients from culturally diverse backgrounds has become a more frequent occurrence in developed countries [17] and a layer of complexity can be encountered when culturally diverse patients interact with healthcare in general and that this is particularly noteworthy in countries where cultural diversity is a more recent development [9]. Difficulties forming therapeutic relationships and the stress that this caused healthcare practitioners [18] and the need for practitioners to be aware of their own cultural frame of reference and to be able to recognize their own bias is evident [19]. Cultural competence in healthcare practitioners has been offered as a means of tackling the disparities in care provided to culturally diverse patients and to addressing the concerns identified by healthcare practitioners [20]. Within palliative care, it is acknowledged that the role of culture is significant [21] as it shapes how serious illness is understood, how suffering is articulated and how grief manifests in patients and their families and in the healthcare practitioners whom they encounter [22].
Culturally diverse patients are underrepresented amongst service users [23] and do not represent a homogenous group [24]. It is recognised that within the palliative phase of illness the vulnerabilities of patients and families are particularly evident [25]. All healthcare professionals governing bodies highlight that patients’ cultural background and ethnicity have an important effect on their health outcomes and healthcare professionals should try to understand culture and respond to individual needs. Therefore, the requirement for practitioners to provide care that is sensitive to the cultural background of patients is identified, reinforced, and heightened in palliative care as failure to address such needs cannot often be redressed later [26]. Thus, examining the experiences of healthcare practitioners providing palliative care to persons from culturally diverse backgrounds is important and this paper explores these experiences through a qualitative systematic review. While van Eechoud et al. [27] examined the experiences of oncology healthcare workers caring for ethnic minority patients the authors are unaware of any review from a palliative care context.
Methods
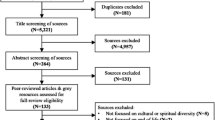
This qualitative systematic review aimed to explore the perspectives of healthcare practitioners providing palliative care to patients from culturally diverse backgrounds. Wakefield’s guide to searching and reviewing literature [28] guided and supported and the review is reported as per the PRISMA checklist (Supplementary file 1) and PRISMA flowchart [29] (Fig. 1).
Search sources and strategies
Searches were conducted within five electronic databases: PsycINFO, CINAHL, Academic Search Complete, Medline and Cochrane Library. The search strategy was based on the PICo framework (Population [healthcare practitioners], Phenomenon of Interest [perspectives] and Context [patients from culturally diverse background receiving palliative care]). The following terms were included in the search string strategy; first, for population ‘healthcare practitioners’, for phenomenon of interest ‘perspectives’ and for context ‘palliative care’ ‘culturally diverse’. All terms were joined utilizing the Boolean operators (“OR” within each search string and “AND” to combine - Table 1).
Criteria for considering studies in this review were set as follows:
Inclusion criteria
-
Primary research published in peer-reviewed journals.
-
Papers written in English or translation available.
-
Papers published between 01 January 2012 and 01 March 2022.
-
Papers referring to the adult population over the age of 18 years.
-
Studies which contain each of three elements: palliative intent to care, healthcare practitioners’ views or experiences and patients with culturally diverse background.
-
Qualitative research design.
Exclusion criteria
-
Secondary research – e.g., discussions, editorials, opinion papers, conference proceedings.
-
Literature reviews - e.g., systematic, scoping, rapid, narrative, expert, integrative.
-
Studies which focus primarily on advance directives and enrolment or access to hospice programmes.
-
Non-qualitative methodologies.
-
Studies where it is not possible to extract the views of the healthcare practitioner.
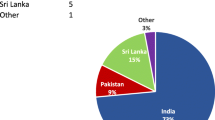
Study selection and data extraction
All search results were exported to Rayyan intelligent systematic review software and duplicates deleted. The remaining titles and abstracts were screened against the inclusion criteria led by the first author (CB) during which the team met to discuss the screening criteria and 20% were doubled screening by the author and the team. All studies remaining were retrieved for full text screening where the authors worked in pairs to reach a final verdict. Reasons for exclusion were noted and reported (Fig. 1). A total of 1954 papers were identified with 411 duplicates leaving 1543 for screening. Title and abstract screening resulted in 1506 been excluded, leaving 37 studies for full-text screening where full-text were read and 17 excluded. Resulting in 20 papers meeting the inclusion criteria for this review. 6 additional papers were found through backward chaining from reference lists of included papers. Data extracted was performed on all 26 papers by the first author (CB) and reviewed by the other authors (BL/OD). The data extraction table (Table 2) developed reports: authors, year, title, country, primary aim, methodology, data collection, sample size, key findings and quality appraisal score [30].
Quality assessment of the included studies
The Critical Appraisal Skills Programme (CASP) and its supporting user guide were utilized to assess the quality of the 26 included papers. CASP allowed the authors undertake a systematic and rigorous approach through a series of ten questions, prompting the authors to consider three areas when appraising qualitative studies, the validity of the results, the nature of the results and the contribution of the results [30]. The methodological quality of the papers assessed was generally good with CASP scores ranging from 50 to 100% (Supplementary file 2).
Data analysis
Braun and Clarke’s six-step thematic analysis inductive approach [31] guided the data analysis process. At first, each paper was thoroughly read to highlight relevant quotes and paragraphs, with open notes made of initial ideas and concepts. Following this quotes and paragraphs with their notes were collated into an entire data set and preliminary open coding conducted to help streamline and converge the data. Here a color-coding system assisted in highlighting patterns across the data and immersion assisted with familiarisation of the data and patterns were noted, reflected upon and discussed. This process enabled the development of broader, more conceptualized themes and the reflection and discussion process allowed for the merging and/or refining and discarding some preliminary themes. Themes were then defined and labelled followed by critically reviewing each theme and coding to assess the accuracy of the coding process leading to verification of theme.
Findings
Through data analysis four key themes emerged from the literature (communication and connection, the role of the family in death and dying, the role of education in addressing uncertainty and institutional and societal factors) and these are presented. In addition, the characteristics of the studies include in this review are presented in Table 3.
Communication and connection
Managing care when the patient does not speak the primary language of the country featured in the majority of studies [3, 34,35,36,37,38, 40,41,42,43, 45,46,47,48,49, 51,52,53, 55,56,57] and was commonly identified as a barrier to the provision of comprehensive care. Practitioners voiced concern that usual methods of providing support or comfort were impaired [34, 36, 48]. Participants in two studies noted that the snatches of conversations [38] and all of those small things that you say all the time [48] that help to build relationships, were missing in the absence of a common language. de Voogd et al. [36] highlights the risk of misinterpretation when statements of wishes are taken literally and viewed through the care providers’ own standpoint without exploration or clarification.
Interpreters were seen as key to addressing communication issues however, difficulties accessing the services of interpreter and variability in quality are noted [33, 37, 38, 45, 46, 48,49,50, 52,53,54,55,56, 56, 57, 57]. Green et al. [38] noted that interpreters tend only to be requested for more formal discussions around issues such as consent. Difficulties also existed when using telephone interpreter services with inadequacies of a relay conversation [37], difficulty with hearing [49] and the missing of non-verbal cues [45, 46] evident. Practitioners reported using interpreters infrequently, citing the need for advance planning and reported that in general, families preferred to interpret for themselves [34, 37, 38, 45]. The use of family interpreters raised concerns regarding the burden it may place on family members and the extent of the information conveyed [34,35,36,37,38, 45, 48, 53, 55, 57]. A number of studies note that practitioners at times felt that families may modify the information they were trying to convey in an attempt to shield the patient [34,35,36, 38, 45, 53, 56]. The utilisation of staff members as interpreters raises some concerns due to the perceived burden [53]. There was evidence of positive efforts made by practitioners to ensure patients could be understood and this was seen as a way of establishing trust [38, 40, 42, 43]. To support understanding, practitioners sometimes used unorthodox methods such as drawing up word lists [36], drawing pictures [49], using sign language [34, 55] and using an app on practitioners’ personal phones [49]. Communication triads involving healthcare practitioners, family members and the patient were utilised with support strategies such as additional time spent establishing relationships with the family [34]. While practitioners rated communication to be either moderate or good [34, 35] concerns existed regarding the content of translated information relayed to the patient as patients sometimes did not understand a particular issue but are reluctant to seek clarification [49]. Communicating in the patients’ preferred language is both an ethical and licencing responsibility [37, 38].
The importance of making connections with patients and families to forge relationships is documented in all studies. A specific emphasis on presence is discussed in a number of studies [36, 39,40,41,42, 49, 52] expressed as having a presence at the bedside, constantly checking yet giving space [40, 41]. Value is placed on building and maintaining trust [38, 41,42,43] and demonstrating acceptance and concern by asking about preference and ascertaining usual ways of operating while respecting difference [34, 36, 38, 40,41,42,43, 49, 51,52,53, 56]. Seeking and building on similarities is also thought to facilitate connection [34, 38, 43, 53]. Intense expressions of distress and grief by family members were noted in a number of studies [39, 48, 53, 54, 57]. Practitioners emphasised the importance of providing physical space to facilitate such expression [54, 57] and emotional support for families at such times [52]. The importance of not labelling families also features [42].
The role of family in death and dying
All studies revealed the central role played by the families of culturally diverse patients in receipt of palliative care as perceived by practitioners. The large number of visitors was commented by practitioners working in in-patient settings [30, 38, 39, 45, 48, 49, 52, 53, 55]. Practitioners sought to support and educate families to fulfil patient and family wishes for participation in care and endeavoured to work around the family so that they would feel included [30]. Strategies to develop relationships with family members such as actively involving family members…asking the family…listening to family suggest that family involvement is largely significant in achieving a good death [40, 42]. However, ambivalence to family involvement is expressed by some practitioners, suggesting that they could not care for the patient because the family want to care for their loved ones in a completely different way [55]. Preparation of the family for death was important and involved explanations of what was happening and what might broadly be expected [38, 40,41,42, 50, 52, 56]. The pressure that care provision places on family members themselves was acknowledged by practitioners reporting a sense of duty in addition to family and community expectations [35, 36, 38, 54, 57]. However, a general reluctance to discuss psychological distress by family members themselves may exist and this can hinder practitioners fulfilling their caregiving role [57].
Tensions between practitioner values and family wishes occurred in many of the studies where issues arose concerning different models of decision making, non-disclosure and differing attitudes to patient autonomy [30, 33,34,35,36,37,38, 45, 46, 48, 51,52,53,54,55,56]. Devolved or collective decision-making was discomfiting for many practitioners and was frequently thought to result in withholding information from the patient [30, 34,35,36,37,38, 45, 47, 52, 53]. Difficulties also arose in identifying the family spokesperson/decision-maker [34, 35, 45, 46] and such decision-making was sometimes thought to impede female autonomy [53]. While acknowledging on-going professional concerns about decision-making and autonomy, care providers used a variety of approaches to address these concerns including adapting word choices, allowing additional time to hear families views and striving for an approach that is acceptable to patient, family and practitioner [34,35,36,37,38, 42, 43, 45, 53]. A further tension involved family preferences around the administration of medications, particularly opioids and practitioners perceived that patients suffered because of family members opposition to medication use [36, 38, 39, 49]. Furthermore, when a trusting relationship had not been established, families and patients were more likely to reject medications [43] and fear of addiction, side -effects, stoicism and lack of understanding arising from attitudes to analgesia in country of origin were also identified [44].
There was a perception that speaking about death was disliked by patients and families from culturally diverse backgrounds [32, 33, 35, 38, 43, 45, 51,52,53,54,55,56]. Practitioners often held a view that death is a taboo topic that people did not want to talk about [33, 51, 54] and that patients were reluctant to die at home due to cultural influences [51]. However, practitioners also noted, within the same studies, that some families were very open to discussing impending death [51, 54] and that reluctance to die at home was possibly due to lack of knowledge of available supports and fear of burdening family members [51, 52]. A particular difficulty arose for practitioners when the parents of young children were involved and were reluctant to talk about death, here practitioners reported feeling complicit in concealing the truth and had considerable concern for the families post bereavement [33, 34]. The significance of rituals and practices around death and the resultant implications for practice were evident [38,39,40, 45, 47, 49, 52,53,54, 57] with efforts made to facilitate families they have very strong rituals and beliefs [49]. Practitioners expressed this willingness as doing the right thing [40] and expressed satisfaction with been able to support cultural practices where they were walking alongside patients and families [38]. Support varied from family to family highlighting an individualised approach [32, 38, 39, 47, 54] and there was a readiness to be flexible to accommodate family wishes and rituals which often required bending the rules [49, 52, 53]. Practitioners observed that although culture had a bearing on care, certain aspects of the approach of end of life were common to all people irrespective of culture, ethnicity or religion [32, 38, 43, 51] and cultural considerations were integrated into culturally responsive individualised patient care [32, 34,35,36, 38,39,40,41,42,43, 49, 51,52,53, 56].
The role of education in addressing uncertainty
All the studies documented challenges encountered by practitioners when providing palliative care to culturally diverse patients and their families, with uncertainty a common thread. Feelings of inexperience, unease, and helplessness [39, 40], overwhelmed and underprepared [40, 41], anxiety, helplessness, self-insufficiency and uncertainty [53, 54], and uncertainty, stress, frustration [48, 49] were expressed. Practitioners noted that they were more familiar with practices, communication cues and family dynamics in native born patients and families [33, 34, 38, 39, 48, 55] and were concerned about causing offence or upset by contravening unfamiliar customs [33, 34, 39, 40, 40, 41, 48, 48,49,50, 50]. These concerns resulted in practitioners questioning the quality of care they provided [33, 34, 36, 45, 46, 48, 54, 55] as family members views about care were sometimes at variance with their own professional ideals and values [33, 45, 46, 48, 55]. On occasions, practitioners stepped back from patients due to discomfort at the unfamiliarity of certain situations [48, 49]. Practitioners attempted to overcome uncertainties by a constant adjustment to reconcile differences in approaches [51], proceeding slowly and with care in partnership with the patient and family [38,39,40,41,42,43] .Other practitioners sought understanding and joint solutions while acknowledging conflicting opinions and on occasions, resolution did not occur [34, 35]. Where practitioners provided culturally appropriate care they reported satisfaction [38, 53] and found support and learning from colleague’s experiences [40].
A lack of knowledge or a need for further education was voiced by practitioners [33, 39, 40, 48, 49, 54,55,56]. Some nurses had requested training and education [33, 56] due to the changing landscape of care we are coming across more people from abroad, different culture, it’s time we knew, we need to know. [39] Healthcare practitioners felt that the lack of knowledge could hamper their ability to care for culturally diverse patients but that more knowledge about that which was less familiar would make cross-cultural encounters feel less unusual [33, 48, 55]. Few studies document previous education in cultural diversity. In one, there is evidence of a yearly class on cultural competence [37] and in another, only seven out of twenty participants had formal education in the area [40]. Practitioners in this study [40], acknowledged a lack of knowledge and understanding I was ignorant and purposefully sought to increase their knowledge informally through questioning and observing more experienced colleagues and engaging with family members. In addition, attending seminars and learning from interdisciplinary discussions were deemed helpful [47, 53].
Institutional and societal factors
The influence of factors rooted in the wider context of palliative care provision to culturally diverse patients occur in all the studies reviewed. There is a perception of low levels of awareness of and engagement with palliative care services amongst patients and families [32, 37, 46, 48, 49, 51, 53, 54]. Reasons for this are manifold, including late referrals to palliative care services [54],a perception of hospice as white and middle class [32], unfamiliarity with the concept of palliative care [34, 36, 37, 42, 44, 46, 51, 54] and a lack of familiarity with health and palliative care services [35, 37, 44, 46, 48, 49, 53,54,55]. Influences on care such as social isolation, economic disadvantage, experience of discrimination due to religion or other factors, having endured war or trauma, level of education, and length of time in host country were also perceived to influence interaction [35, 38, 46, 54]. Specific support, such as financial information, spiritual or bereavement support provided by the community from which the patient originates can play an important role in supporting engagement with palliative care services [36, 37, 39, 44, 46, 57].
Several factors pertaining to healthcare institutions, specifically related to resources occur throughout the studies. The provision of adequate pastoral care services was seen as particularly helpful [38, 39, 47, 53, 57]. For indigenous patients and families, remote geographical location had a significant impact on the provision of palliative care with limited infrastructure and personnel available [54, 56]. Environmental factors such as the importance of the physical environment to accommodate large family groups and facilitating gender preferences were seen as important aspects of care [32, 36, 45, 49, 52, 54, 55, 57]. However, it was not always possible to facilitate and while attempts were made to adjust rosters to try and meet patient preferences for carers of a particular gender, it could not be always facilitated/accommodated as we don’t have a list, sometimes there are only men on the night shift. [36]
The experience of a culturally diverse workforce is an important factor but assigning nurses to patients of a similar cultural background did not always result in language congruence and could result in stereotyping [51] and even with a shared migrant background, issues of unfamiliarity were still encountered [40]. In addition, practitioners reported challenges when dealing with patients and families from a similar cultural background, where increased workload [51] and unease when conflicts occurred were noted [45, 46, 53]. Practitioners reported sense of satisfaction at being able to assist those of a similar background [40, 43, 53] and diversity in personnel was viewed as a positive means of meeting patients’ needs [36, 40]. The management of issues which arise when caring for culturally diverse patients and families at ward level should be discussed as a team and efforts made to come to a consensus on approaches used [47, 53]. It is suggested that endeavours to accommodate patient preferences, such as extending visiting times etc., can be a source of disagreement within a team so ongoing dialogue, discussion and team support are warranted [53, 54].
Discussion
This systematic review explored the perspectives of healthcare practitioners on providing palliative care to patients with culturally diverse backgrounds in a variety of settings. Findings concur in some respects with van Eechoud et al’s. [27] systematic review of oncology health workers caring for ethnic minority patients. Of similarity is the principal challenges of communication and a fear of acting in a culturally insensitive way but extending on this the findings from this review highlights the pivotal role of the family, the need for an individualised approach to care, the universality of needs when approaching end of life and the need for education as voiced by practitioners. Challenges posed to healthcare practitioners by lack of a common language with patients were found in this review [32, 34,35,36,37,38, 40, 41, 45,46,47,48,49, 51,52,53, 55,56,57] and this is reflected in the wider literature concerning interactions between culturally diverse patients and healthcare practitioners in palliative care contexts [15, 58, 59]. Difficulty accessing professional interpreters, a reluctance to use them by staff, by family or patient or dissatisfaction with the service provided, suggests a myriad of factors influencing their use [34, 38, 45, 48, 49, 52, 53, 55, 56, 56, 57]. Nonetheless engagement with professional interpreters has been shown to aid in reducing healthcare disparities by reducing errors and through improved communication, leading to greater patient satisfaction [18] and demonstrates clinicians’ respect for patients [60]. Research identifies that interpreters are frequently not utilized even when practitioners are aware that their use is advisable with family and bilingual staff utilized instead [61, 62]. However, such an ad hoc means of translation is inadvisable and indicates that defaulting to use of family without exploration of alternatives or family and patient opinions does not best serve the interests of healthcare practitioners, families, or patients [63, 64].
A clear finding of the review is the means by which practitioners built relationships with patients and families [32, 36, 38,39,40,41,42,43, 49, 52, 53]. and it is recognised that intentional presence can convey compassion in intercultural encounters [65]. Culturally diverse patients report feelings of respect and support when practitioners spent time with them and try to communicate even in the absence of a common language [66] with a sense of exclusion reported in the absence of such efforts [60]. The need for time as an aid to communication and relationship building is acknowledged elsewhere [67]. Consistent with existing research this review also highlights the importance of family in the care of culturally diverse patients in receipt of palliative care [68, 69]. The importance of a physical environment which supports large families was noted in several studies [32, 52, 57] and is also seen in the literature as an important asset to inpatient care and helpful to both patients, families, and practitioners [70, 71]. While healthcare practitioners perceived that culturally diverse patients generally enjoyed good support from immediate and extended families, concerns are evident in one study regarding the difficulties family members have accepting responsibility for care of a patient at home [54]. Practitioners demonstrated awareness that particular aspects of patients and families migration history may have a bearing on care provision [34, 35, 37, 38, 42, 44,45,46, 49, 53, 57] and recognised the demand placed on female family carers [35, 38]. This burden is recognized in the wider research [72, 73] which also notes that a sense of responsibility for older family members in people with culturally diverse backgrounds does not automatically mean close emotional bonds [74, 75]. This is an important factor as support for family members is an integral part of palliative care [75] and that the presence family does not negate the pressures that the caring role may place on some family members of migrant and indigenous families [71,72,73].
An expected finding from the review which occurred within all studies, is the complexity involved for practitioners in negotiating with the patient and family around such matters as perceived cultural taboos. The review reveals that widely held views about death as a taboo subject in certain cultural groups is not consistently realised [42, 50, 51, 54]. This variability is echoed in the wider literature [76,77,78] further illustrating the need for individualized assessment and the need for practitioners to be aware that cultural taboos are a reality for some but that subscription to them is not uniform and individual consideration is necessary as other influences such as relationships, fear, lack of awareness of services may be relevant. A notable finding from the review is concern for patients’ autonomy where family play a greater role in decision making and disclosure [32, 33,34,35,36,37,38,39, 45, 46, 48, 49, 52, 53, 55, 57] and this resonates with research in oncology and palliative care where devolved decision making and a preference for non-disclosure are noted [79, 80]. Language barriers and the difficulties ascertaining patient preferences are found to make information sharing a complex matter [27, 81]. Thus practitioners adjust communication as each situation is assessed [36,37,38, 40,41,42,43, 45, 46, 49, 51,52,53] and particularly when home visiting is involved [34, 35, 39, 54, 57]. The desirability of ascertaining early from both patient and family, what their preferences are regarding information sharing and documenting their preferences is essential for working together [60].
Ascertaining the role of culture in the lives of patients, families, and clinicians themselves and negotiating and adapting care necessitates a nuanced and informed approach. Practitioners demonstrated an awareness of culture as a dynamic, evolving process i.e. that patients and families may embrace aspects of culture to varying degrees and specifically spoke of the need to avoid generalizations [32, 38, 40, 43, 47, 51]. Reliance on a patients’ cultural background and beliefs alone can result in cultural stereotyping [21] and individualised approaches were frequently utilised as a means to overcome this risk [32, 33,34,35,36,37,38,39,40,41,42,43, 45,46,47, 51,52,53,54] an approach supported by the wider literature [26, 63]. However, individualised care must be delivered with awareness of the myriad of potential influences on the intercultural encounter i.e. cultural, socioeconomic, educational and family relationships and where culture is seen as part of a patients’ complex personhood rather than a separate entity [82]. The findings of this review demonstrate that the ways care is adapted to try to meet the varying needs of patients and families are similar with all people irrespective of cultural background [32, 34, 35, 38,39,40,41,42,43, 45, 49, 51, 52], indicating that practitioners draw on skills such as sensitive communication, individualised care and family support which are integral to the practice of palliative care [83] and therefore familiar to practitioners. This suggests that the patient-centred practice of palliative care can provide a basis for incorporating cultural considerations into every encounter by acknowledging the universality of differing communication styles, need for information, family involvement and health beliefs and negotiating these with an awareness of of how culture interconnects with these [84, 85].
Generally, practitioners experienced uncertainty when encountering patients with an unfamiliar cultural background and this is reflected in the wider literature [18, 58, 59]. Within a systematic review of barriers to care of ethnic minority patients, nurses report communication difficulties, lack of culturally appropriate resources and insufficient education were primary concerns [86]. Practitioner reported knowledge deficits and requests for further education are evident in this review [33, 39, 40, 48, 49, 54,55,56] and acknowledged within the wider literature [19, 58, 87]. Although further education is seen as a means to improve the care offered and to help allay uncertainties [33, 39, 48, 57] culture specific knowledge is recognised as potentially contributing to stereotyping and encouraging generalisations [26, 84] and the literature does not offer a simple solution. Studies examining cultural competence education, report that there is little assessment of outcome [88] and are seldom evidence based [89]. Instead,it is suggested that enhancing communication skills and expanding awareness of the many factors, clinician, patient and family related, which influence communication may prove beneficial. [89]. A systematic review assessing the effectiveness of cultural competence on patient satisfaction found that while training improved patient satisfaction, concerns existed regarding the quality and methodological rigor of the reviewed studies, so caution was advised on interpretation of results [90]. Nonetheless, perceived gaps in knowledge contribute to a sense of uncertainty about aspects of care provision, thus within educational settings, teaching students to approach situations which are unfamiliar, with interest rather than unease is pivotal [91]. Education in intercultural communication and an ability to question how care is provided are required to equip future clinicians to provide appropriate care for all [91]. Within training programmes there needs to be an integration and assessment of culturally sensitive care throughout curricula [92, 93] and a combination of approaches is required to prepare nursing students to provide care to culturally diverse patients, including knowledge, simulation of cross-cultural encounters, reflection, and appropriate role models [94]. For existing practitioners, the training of staff members to become ethnic coordinators had a beneficial influence on patient related interactions and on the culture of care towards culturally diverse patients [95]. A combination of a broad knowledge of culture relating to health and to death and dying, enhanced communication skills development and self-reflection can offer practitioners a framework from which to approach clinical encounters [96]. It is also recognised that educating practitioners to use moral reasoning could help promote ethical and just decision making when exploring care for patients with culturally diverse backgrounds [97, 98].
While there is awareness amongst practitioners in all studies of the institutional and societal factors which may influence the delivery of care, the wider literatures evidences low levels of engagement with palliative care services among some culturally diverse patients [22, 25]. Palliative care is unfamiliar to some culturally diverse patients as the term does not translate directly in many languages [82]. A systematic review of referrals to palliative care from oncology/haematology services identified a lack of knowledge of palliative care amongst healthcare practitioners and low levels of awareness of palliative care amongst patients and families in the general population, is a significant and widespread obstacle to palliative care referrals [99]. It has been highlighted that gatekeeping by referrers who perceive that culturally diverse patients do not utilise palliative care services can occur [100] but it has also been shown that palliative care referrals were proportionally higher in hospital settings for culturally diverse patients and posited that more opportunity and time to explore understanding may have been a contributing factor [101]. The provision of time is of critical importance in the provision of patient-centred care during the palliative phase of illness and the ability to spend time with patients and families is vital to building trusting relationships [83, 102]. Limited time resources are recognised as a barrier to care for culturally diverse patients [103]. This highlights the role of organisational support in facilitating practitioners to have time as a resource [33, 47, 52, 54]. Furthermore, the existence of a culturally diverse workforce in healthcare settings is viewed as a facilitator of good care [14, 22, 104] but may place additional demands on culturally diverse practitioners which may impact the practitioners themselves [105].
Strengths and limitations
A strength of this review is the insight gained into the perspectives of healthcare practitioners providing palliative care to patients with a culturally diverse background. However, it is recognised that the time frame may have eliminated papers that were relevant and could have added to the current body of literature. This review included papers that were published in English, however given the subject topic of culturally diverse backgrounds the review may have eliminated papers of importance as there were not written in English. This review highlights the difficulties for healthcare practitioners caring for patients and their families from diverse cultural background and suggested strategies that could help meet the needs of their patients. Research into this topic is limited and so encompassed all multidisciplinary members and it is possible that had the review been restricted to a single professional group, the findings may be more transferable. However, given the review explored healthcare practitioner’s perspectives of providing palliative care to patients from a culturally diverse backgrounds all practitioners were included, and findings may be transferable.
Conclusion
In this review, it is apparent that healthcare practitioners face challenges providing palliative care to patients from a culturally diverse background. Language barriers, divergent views on autonomy, uncertainty about aspects of culture and a perception of a need for further education are all issues practitioners dealt with in practice. However, practitioners draw on their existing skills to adapt their practice to unfamiliar situations and utilise palliative care’s patient centred approach to ascertain needs and involve the family. This approach allows them to be aware of the influences that belonging to an indigenous or migrant community may bring but greater integration of culture needs to be incorporated within undergraduate and post graduate education. Ethnicity is not currently recorded in some countries for example on the Cancer Registry in Ireland therefore to help inform and develop services on a national level ethnicity should be included.
Availability of data and materials
Data used for analysis in this review are all extracted from the original published reviews and are presented in Table 2 (Data extraction table).
References
Ellershaw J. Care of the dying, a pathway to Excellence. 2nd ed. Oxford: Oxford University Press; 2011.
Connor SR. Hospice and Palliative Care: the essential guide. 3rd ed. New York: Routledge; 2018.
Ring JM. Psychology and medical education: collaborations for culturally responsive care. J Clin Psychol Med Settings. 2009;16(1):120–6. https://doi.org/10.1007/s10880-008-9141-8.
Hong Y. A dynamic constructivist approach to culture: moving from describing culture to explaining culture. In: Wyer RS, Chiu C, Hong Y, editors. Understanding culture: theory, research, and application. New York: Psychology Press; 2009. pp. 3–23.
Yancu CN, Farmer DF. Product or process: cultural competence or cultural humility? Palliat Med Hosp Care Open J. 2017;3(1):e1–4. https://doi.org/10.17140/PMHCOJ-3-e005.
McAuliffe M, Khadria B. Report overview: providing perspective on migration and mobility in increasingly uncertain times. World Migration Report 2020. International Organisation for Migration, Geneva. 2020. https://publications.iom.int/system/files/pdf/wmr_2020.pdf (Accessed August 18th 2022).
2019, United Nations Department of Economic and Social Affairs (UN DESA) International Migrant Stock, Division UNDESAP. New York. https://www.un.org/en/development/desa/population/migration/publications/migrationreport/docs/MigrationStock2019_TenKeyFindings.pdf (Accessed August 18th, 2022).
World Health Organisation. Strategy and action plan for refugee and migrant health in the WHO European Region. Copenhagen, WHO Regional office for Europe., 2016. Strategy and Action Plan for Refugee and Migrant Health in the WHO European Region 2016–2022 (Accessed August 20th 2022).
Sze M, Butow P, Bell M, Vaccaro L, Dong S, Eisenbruch M, Jefford M, Girgis A, King M, McGrane J, Ng W, Asghari R, Parente P, Liauw W, Goldstein D. Migrant health in cancer: outcome disparities and the determinant role of migrant-specific variables. Oncologist. 2015;20(5):523–31. https://doi.org/10.1634/theoncologist.2014-0274.
Berlin J, Smith D, Newton P. It’s because it’s cancer, not because you’re a Traveller-exploring lay understanding of cancer in English Romany Gypsy and Irish Traveller communities. Eur J Oncol Nurs. 2018;34:49–54. https://doi.org/10.1016/j.ejon.2018.02.010.
Mehus G, Bongo B, Engnes J, Moffitt P. Exploring why and how encounters with the Norwegian health-care system can be considered culturally unsafe by North Sami-speaking patients and relatives: a qualitative study based on 11 interviews. Int J Circumpolar Health. 2019;78(1):1612703. https://doi.org/10.1080/22423982.2019.1612703.
Periyakoil VS, Neri E, Kraemer H. Patient-reported barriers to high-quality, end-of-life care: a multiethnic, multilingual, mixed-methods study. J Palliat Med. 2016;19(4):373–9. https://doi.org/10.1089/jpm.2015.0403.
Alpers LM. Distrust and patients in intercultural healthcare: a qualitative interview study. Nurs Ethics. 2018;25(3):313–23. https://doi.org/10.1177/0969733016652449.
McCleskey SG, Cain CL. Improving end-of-life care for diverse populations: communication, competency, and system supports. Am J Hosp Palliat Med. 2019;36(6):453–9. https://doi.org/10.1177/1049909119827933.
Evans N, Meñaca A, Andrew EV, Koffman J, Harding R, Higginson IJ, Pool R, Gysels M. Appraisal of literature reviews on end-of-life care for minority ethnic groups in the UK and a critical comparison with policy recommendations from the UK end-of-life care strategy. BMC Health Serv Res. 2011;11:141. https://doi.org/10.1186/1472-6963-11-141.
Bourque Bearskin RL. A critical lens on culture in nursing practice. Nurs Ethics. 2011;18(4):548–59. https://doi.org/10.1177/0969733011408048.
Grandpierre V, Milloy V, Sikora L, Fitzpatrick E, Thomas R, Potter B. Barriers and facilitators to cultural competence in rehabilitation services: a scoping review. BMC Health Serv Res. 2018;18(1):1–4. https://doi.org/10.1186/s12913-017-2811-1.
Gerchow L, Burka L, Miner S, Squires A. Language barriers between nurses and patients: a scoping review. Patient Educ Counsel. 2021;104(3):534–53. https://doi.org/10.1016/j.pec.2020.09.017.
Weber O, Sulstarova B, Singy P. Cross-cultural communication in Oncology: challenges and training interests. Oncol Nurs Forum. 2016;43(1):534–53. https://doi.org/10.1188/16.ONF.E24-E33.
Cai DY. A concept analysis of cultural competence. Nurs Int J Sci. 2016;3(3):268–. https://doi.org/10.1016/j.ijnss.2016.08.002. 73.
Bosma H, Apland L, Kazanjian A. Cultural conceptualizations of hospice palliative care: more similarities than differences. Palliat Med. 2010;24(5):510–22. https://doi.org/10.1177/0269216309351380.
Cain CL, Surbone A, Elk R, Kagawa-Singer M. Culture and palliative care: preferences, communication, meaning, and mutual decision making. J Pain Symptom Manag. 2018;55(5):1408–19. https://doi.org/10.1016/j.jpainsymman.2018.01.007.
Gustafson C, Lazenby M. Assessing the unique experiences and needs of Muslim oncology patients receiving palliative and end-of-life care: an integrative review. J Palliat Care. 2019;34(1):52–61. https://doi.org/10.1177/0825859718800496.
Butow PN, Sze M, Dugal-Beri P, Mikhail M, Eisenbruch M, Jefford M, Schofield P, Girgis A, King M, Goldstein D. From inside the bubble: migrants’ perceptions of communication with the cancer team. Support Care Cancer. 2011;19(2):281–90. https://doi.org/10.1007/s00520-010-0817-x.
Davidson PM, Phillips JL, Dennison-Himmelfarb C, Thompson SC, Luckett T, Currow DC. Providing palliative care for Cardiovascular Disease from a perspective of sociocultural diversity: a global view. Curr Opin Support Palliat Care. 2016;10(1):11–7. https://doi.org/10.1097/SPC.0000000000000188.
Koffman J. Servicing multi-cultural needs at the end of life. J Ren Care. 2014;40(Suppl 1):6–15. https://doi.org/10.1111/jorc.12087.
van Eechoud IJ, Grypdonck M, Beekman D, Van Lancker A, Van Hecke A, Veraeghe S. Oncology health workers’ views and experiences on caring for ethnic minority patients: a mixed method systematic review. Int J Nurs Studies. 2016;53:379–98. https://doi.org/10.1016/j.ijnurstu.2015.09.007.
Wakefield A. Searching and critiquing the research literature. Nurs Standard. 2014;28(39):49–57. https://doi.org/10.7748/ns.28.39.49.e8867.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. https://doi.org/10.1136/bmj.n71.
CASP UK. CASP systematic review checklist [Internet]. Oxford: CASP UK. ; 2018 p.4. https://casp-uk.net/wp-content/uploads/2018/01/CASP-Systematic-Review-Checklist_2018.pdf (accessed March 20th 2022).
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–10. https://doi.org/10.1191/1478088706qp063oa.
Bellamy G, Gott M. What are the priorities for developing culturally appropriate palliative and end-of-life care for older people? The views of healthcare staff working in New Zealand. Health Soc Care Comm. 2013;21(1):26–34. https://doi.org/10.1111/j.1365-2524.2012.01083.x.
Debesay J, Harsløf I, Rechel B, Vike H. Facing diversity under institutional constraints: challenging situations for community nurses when providing care to ethnic minority patients. J Adv Nurs. 2014;70(9):2107–16. https://doi.org/10.1111/jan.12369.
de Graaff FM, Francke AL, Van den Muijsenbergh METC, van der Geest. S. Talking in triads: communication with Turkish and Moroccan immigrants in the palliative phase of cancer. J Clin Nurs 2012a Nov; 21(21–22):3143–52. https://doi.org/10.1111/j.1365-2702.2012.04289.x.
de Graaff FM, Francke AL, van den Muijsenbergh M, der Geest S. Understanding and improving communication and decision-making in palliative care for Turkish and Moroccan immigrants; a multiperspective study. Ethn Health 2012b Aug1;17(4):363–84. https://doi.org/10.1080/13557858.2011.645152.
de Voogd X, Willems DL, Onwuteaka-Philipsen B, Torensma M, Suurmond JL. Health care staff’s strategies to preserve dignity of migrant patients in the palliative phase and their families: a qualitative study. J Adv Nurs. 2021;77(6):2819–30. https://doi.org/10.1111/jan.14829.
Eckemoff E, Sudha S, Wang D. End of life care for older Russian immigrants - perspectives of Russian immigrants and hospice staff. J Cross-Cultural Gerontol. 2018;33(3):229–45. https://doi.org/10.1007/s10823-018-9353-9.
Green A, Jerzmanowska N, Green M, Lobb EA. Death is difficult in any language, a qualitative study of palliative care professionals’ experiences when providing end-of-life care to patients from culturally and linguistically diverse backgrounds. Palliat Med. 2018;32(8):1419–27. https://doi.org/10.1177/0269216318776850.
Henry A, Timmins F. An exploration of specialist palliative care nurses’ experiences of providing care to hospice inpatients from minority ethnic groups–implication for religious and spiritual care. Religions. 2016;7(2):18. https://doi.org/10.3390/rel7020018.
Johnstone MJ, Hutchinson AM, Redley B, Rawson H. Nursing roles and strategies in end-of-life decision making concerning elderly immigrants admitted to acute care hospitals. J Transcult Nurs 2016a Sep;27(5): 471–9. https://doi.org/10.1177/1043659615582088.
Johnstone MJ, Hutchinson AM, Rawson H, Redley B. Assuaging death anxiety in older overseas-born australians of culturally and linguistically diverse backgrounds hospitalised for end-of-life care, Contemp Nurs 2016b May 6;52(2–3):269–85. https://doi.org/10.1080/10376178.2016.1192953.
Johnstone M-J, Hutchinson MA, Rawson H, Redley B. Nursing strategies for engaging families of older immigrants hospitalized for end-of-life care: An Australian study, J Patient Exp. 2016c Sep;3(3):57–63. https://doi.org/10.1177/2374373516667004.
Johnstone MJ, Rawson H, Hutchinson AM, Redley B. Fostering trusting relationships with older immigrants hospitalised for end-of-life care. Nurs Ethics. 2018;25(6):760–72. https://doi.org/10.1177/0969733016664978.
Khosla N, Washington KT, Regunath H. Perspectives of health care providers on US South asians’ attitudes toward pain management at end of life. Am J Hosp Palliat Care. 2016;33(9):849–57. https://doi.org/10.1177/1049909115593063.
Khosla N, Washington KT, Shaunfield S, Aslakson R. Communication challenges and strategies of U.S. health professionals caring for seriously ill south Asian patients and their families. J Palliat Med. 2017;20(6):611–7. https://doi.org/10.1089/jpm.2016.0167.
Khosla N, Washington KT, Mukherjea PH, Aslakson R. Health-care providers’ perspectives on decision-making among seriously ill patients on south Asian origin in the United States. J Palliat Care. 2019;34(3):181–8. https://doi.org/10.1177/0825859719829480.
Mahilall R, Swartz L. Spiritual care practices in hospices in the western cape, South Africa: the challenge of diversity. BMC Palliat Care. 2021;20(1):1–8. https://doi.org/10.1186/s12904-020-00704-z.
Milberg A, Torres S, Ågård P. Health care professionals’ understandings of cross-cultural interaction in end-of-life care: a focus group study. PloS ONE 2016 Nov 11(11):e0165452. https://doi.org/10.1371/journal.pone.0165452.
Neiman T. Nurses’ perceptions of basic palliative care in the Hmong population. J Transcult Nurs. 2019;30(6):576–86. https://doi.org/10.1177/1043659619828054.
Nielsen LS, Angus JE, Gastaldo D, Howell D, Husain A. Maintaining distance from a necessary intrusion: a postcolonial perspective on dying at home for Chinese immigrants in Toronto, Canada. Eur J Oncol Nurs. 2013;17(5):649–56. https://doi.org/10.1177/1049909114527338.
Nielsen LS, Angus J, Howell D, Husain A, Gastaldo D. Patient-centered care or cultural competence: negotiating palliative care at home for Chinese Canadian immigrants. Am J Hosp Palliat Med. 2015;32(4):372–9. https://doi.org/10.1177/1049909114527338.
Roider-Schur S, Rumpold T, Kirchheiner K, Masel EK, Nemecek R, Amering M, Watzke H, Schrank B. Migrate your mind: the role of palliative care in transcultural cancer treatment: a qualitative analysis. Wiener Klinische Wochenschrift. 2019;131(9):191–9. https://doi.org/10.1007/s00508-019-1474-9.
Schrank B, Rumpold T, Amering M, Masel E, Watzke H, Schur S. Pushing boundaries—culture-sensitive care in oncology and palliative care: a qualitative study. Psycho-Oncol. 2017;26(6):763–9. https://doi.org/10.1002/pon.4217.
Shahid S, Bessarab D, van Schailk KD, Aoun SM, Thompson SC. Improving palliative care outcomes for Aboriginal australians: service providers’ perspectives. BMC Palliat Care. 2013;12(1):26–35. https://doi.org/10.1186/1472-684X-12-26.
Torres S, Ågård P, Milberg A. The other in end-of-life care: providers’ understandings of patients with migrant backgrounds. J Intercult Studies. 2016;37(2):103–17. https://doi.org/10.1080/07256868.2016.1141756.
Vincent D, Rice J, Chan J, Grasseau P. Provision of comprehensive, culturally competent palliative care in the Qikiqtaaluk region of Nunavut: Health care providers’ perspectives. Canadian family physician Medecin de famille canadien. 2019;65(4): e163–e9. https://www.cfp.ca/content/cfp/65/4/e163.full.pdf (accessed: 10th March 2022).
Washington K, Khosla N, Lero C. U.S. providers’ perceptions of the psychosocial needs of seriously ill patients of south Asian origin: implications for health social work. Health Soc Work. 2019;44(3):177–84. https://doi.org/10.1093/hsw/hlz015.
Bloomer M, Botti M, Runacres F, Poon P, Barnfield J, Hutchinson A. Cultural considerations at end of life in a geriatric inpatient rehabilitation setting. Collegian. 2019;26(1):165–70. https://doi.org/10.1016/j.colegn.2018.07.004.
Brighi N, Colazzo AL, Bolognesi D, Surbone A, Biasco G. Cross-cultural differences in hospices: a retrospective study in Italy. Eur J Oncol. 2014;19(1):34–42. https://mattioli1885journals.com/index.php/EJOEH/article/view/3786/3025.
Jansky M, Owusu-Boakye S, Nauck F. An odyssey without receiving proper care – experts’ views on palliative care provision for patients with migration background in Germany. BMC Palliat Care. 2019;18(1):1–0. https://doi.org/10.1186/s12904-019-0392-y.
Boyle PJ. An assessment of cultural competence of community public health nursing in Liffeyside Health Service Area, Dublin: unpublished thesis (D.Prof.), Middlesex University; 2014. http://eprints.mdx.ac.uk/13464/ (Accessed August 20th 2022).
Green A, Jerzmanowska N, Thristiawati S, Green M, Lobb E. Culturally and linguistically diverse palliative care patients’ journeys at the end-of-life. Palliat Support Care. 2019;17(2):227–33. https://doi.org/10.1017/S1478951518000147.
Watts K, Meiser B, Zilliacus E, Kaur R, Taouk M, Girgis A, Butow P, Kissane D, Hale S, Perry A, Aranda S, Goldstein D. Perspectives of oncology nurses and oncologists regarding barriers to working with patients from a minority background: systemic issues and working with interpreters. Eur J Cancer Care. 2018;27(2):e12758. https://doi.org/10.1111/ecc.12758.
McCarthy J, Cassidy I, Graham MM, Tuohy D. Conversations through barriers of language and interpretation. Br J Nurs. 2013;22(6):335–39. https://doi.org/10.12968/bjon.2013.22.6.335.
Papadopoulos I, Taylor G, Ali S, Aagard M, Akman O, Alpers LM, Apostolara P, Biglete-Pangilinan S, Biles J, García ÁM, González-Gil T. Exploring nurses’ meaning and experiences of compassion: an international online survey involving 15 countries. J Transcult Nurs. 2017;28(3):286–95. https://doi.org/10.1177/1043659615624740.
Degrie L, Gastmans C, Mahieu L, de Casterle BD, Denier Y, Dierckx de Casterle B. How do ethnic minority patients experience the intercultural care encounter in hospitals? A systematic review of qualitative research. BMC Med Ethics. 2017;18(1):1–17. https://doi.org/10.1186/s12910-016-0163-8.
Bramley L, Matiti M. How does it really feel to be in my shoes? Patients’ experiences of compassion within nursing care and their perceptions of developing compassionate nurses. J Clin Nurs. 2014;23(19–20):27. https://doi.org/10.1111/jocn.12537.
Cruz-Oliver DM, Sanchez-Reilly S. Barriers to quality end-of-life care for latinos: Hospice health care professionals’ perspective. J Hosp Palliat Nurs. 2016;18(6):505–11. https://doi.org/10.1016/j.jpainsymman.2012.10.149.
Weerasinghe S, Maddalena V. Negotiation, mediation and communication between cultures: end-of-life care for south Asian immigrants in Canada from the perspective of family caregivers. Soc Work Public Health. 2016;31(7):665–77. https://doi.org/10.1080/19371918.2015.1137521.
Slater T, Matgeson A, Davies C, Earp R, Gellatly K, Holdaway M, Ellison-Loschmann L. Exploring Māori cancer patients’, their families’, community and hospice views of hospice care. Int J Palliat Nurs. 2015 Sept 2;21(9):439–45. https://doi.org/10.12968/ijpn.2015.21.9.439.
Markham S, Islam Z, Faull C. I never knew that! Why do people from Black and Asian Minority ethnic groups in Leicester access hospice services less than other groups? A discussion with community groups. Divers Equality Health Care. 2014;11(3). https://doi.org/10.21767/2049-5471.100016.
Nielsen DS, Minet L, Zeraig L, Rasmussen D, Sodemann M. Caught in a generation gap: a generation perspective on refugees getting old in Denmark—a qualitative study. J Transcult Nurs. 2018;29(3):265–73. https://doi.org/10.1177/1043659617718064.
Fang M, Malcoe L, Sixsmith J, Wong, Callender M. Exploring traditional end-of-life beliefs, values, expectations, and practices among Chinese women living in England: informing culturally safe care. Palliat Support Care. 2015;13(5):1261–74. https://doi.org/10.1017/S1478951514001126.
Wang Y, Faas D. The economic and family experiences of Hong Kong Chinese in Ireland’. Ethnic Racial Studies. 2021;44(1):115–33. https://doi.org/10.1080/01419870.2020.1723670.
Ryan K, Connolly M, Charnley K, Ainscough A, Crinion J, Hayden C, Keegan O, Larkin P, Lynch M, McEvoy D, McQuillan R, O’Donoghue L, O’Hanlon M, Reaper-Reynolds S, Regan J, Rowe D, Wynne M. (2014) Palliative Care Competence Framework, Dublin: Health Service Executive. 2014. Competence Framework - HSE.ie. http://hdl.handle.net/10147/322310 (accessed August 18th 2022).
Zhang W. Is death taboo for older Chinese immigrants? OMEGA-J Death Dying. 2022;84(4):1061–80. https://doi.org/10.1177/0030222820927883.
Colclough YY, Brown GM. Moving towards openness: Blackfeet Indians’ perceptions changes regarding talking about end of life. Am J Hosp Palliat Med. 2019;36(4):282–9.
Chi H, Cataldo J, Ho E, Rehm R. Please Ask Gently: Using Culturally Targeted Communication Strategies to Initiate End-of-Life Care Discussions With Older Chinese Americans. Am J Hosp Palliat Care. 2018;35(10):1265–72. https://doi.org/10.1177/1049909118760310.
Watts KJ, Meiser B, Zilliacus E, Kaur R, Taouk M, Girgis A, Butow P, Goldstein D, Hale S, Perry A, Aranda SK, Kissane DW. Communicating with patients from minority backgrounds: individual challenges experienced by oncology health professionals. Eur J Oncol Nurs. 2017;1(26):83–90. https://doi.org/10.1016/j.ejon.2016.12.001.
Krystallidou D, Devisch I, Van de Velde D, Pype P. Understanding patient needs without understanding the patient: the need for complementary use of professional interpreters in end-of-life care. Med Health Care Philos. 2017;20(4):477–81. https://doi.org/10.1007/s11019-017-9769-y.
Kirby Kirby, Lwin Z, Kenny K, Broom A, Birman H, Good P. “It doesn’t exist”: negotiating palliative care from a culturally and linguistically diverse patient and caregiver perspective. BMC Palliat Care. 2018;17(1). https://doi.org/10.1186/s12904-018-0343-zhttps://rdcu.be/cT19v.
Broom A, Parker RB, Kirby E, Kokanović R, Woodland L, Lwin Z, Koh ES. A qualitative study of cancer care professionals’ experiences of working with migrant patients from diverse cultural backgrounds. BMJ open. 2019;9(3):e025956. https://doi.org/10.1136/bmjopen-2018-025956.
Merlane H, Cauwood L. Core principles of end-of-life care. Br J Nurs. 2020;29(5):290–2. https://doi.org/10.12968/bjon.2020.29.5.280.
Epner DE, Baile WF. Patient-centered care: the key to cultural competence. Annals Oncol. 2012;23:iii33-42. https://doi.org/10.1093/annonc/mds086.
Ammann E, Rauber G, Salis Gross C. Doing death” the Mediterranean way: end-of-life in a segregated nursing home. Mortality. 2019;24(3):271–89. https://doi.org/10.1080/13576275.2018.1483906.
Joo JY, Liu MF. Nurses’ barriers to care of ethnic minorities: A qualitative systematic review. West J Nurs Res. 2020;42(9):760–71. https://doi.org/10.1177/0193945919883395.
Shepherd SM, Willis-Esqueda C, Newton D, Sivasubramaniam D, Paradies Y. The challenge of cultural competence in the workplace: perspectives of healthcare providers. BMC Health Services Research. 2019;19(1):1–1. https://doi.org/10.1186/s12913-019-3959-7.
Boucher N, Johnson K. Cultivating cultural competence: how are hospice staff being educated to engage racially and ethnically diverse patients? Am J Hosp Palliat Med. 2021;38(2):169–74. https://doi.org/10.1177/1049909120946729.
Shepherd SM. Cultural awareness workshops: limitations and practical consequences. BMC Med Educ. 2019;19(1):1–0. https://doi.org/10.1186/s12909-018-1450.
Govere L, Govere E. How effective is cultural competence training of healthcare providers on improving patient satisfaction of minority groups? A systematic review of literature. Worldviews Evid-Based Nurs. 2016;13(6):402–10. https://doi.org/10.1111/wvn.12176.
Markey K, Okantey C. Nurturing cultural competence in nurse education through a values-based learning approach. Nurs Educ Pract. 2019;1(38):153–6. https://doi.org/10.1016/j.nepr.2019.06.011.
Suurmond J, Lantinga K, de Voogd X, Oueslati R, Boland G, van den Muijsenbergh M. Twelve tips to teach culturally sensitive palliative care. Med Teach. 202AD;43(7):845–50. https://doi.org/10.1080/0142159X.2020.1832650.
Zanting A, Meershoek A, Frambach JM, Krumeich A. The ‘exotic other’in medical curricula: Rethinking cultural diversity in course manuals. Medical teacher. 2020;42(7):791–8. https://doi.org/10.1080/0142159X.2020.1736534.
O’Brien E, O’ Donnell C, Murphy J, O’ Brien B, Markey K. Intercultural readiness of nursing students: an integrative review of evidence examining cultural competence educational interventions. Nurs Educ Pract. 2021;1(50):102966. https://doi.org/10.1016/j.nepr.2021.102966.
Nielsen DS, Korsholm K.M, Mottelson I, Sodemann M. Cultural competences gained through an education program as ethnic patient coordinator: a qualitative study. J Transcult Nurs. 2019;30(4):394–402. https://doi.org/10.1177/1043659618823923.
Semlali I, Tamches E, Singy P, Weber O. Introducing cross-cultural education in palliative care: focus groups with experts on practical strategies. BMC Palliat Care. 2020;19(1):1–0. https://doi.org/10.1186/s12904-020-00678-y.
Markey K. Moral reasoning as a catalyst for cultural competence and culturally responsive care. Nurs Philos. 2021;22(1) https://doi.org/10.1111/hsc.12556 .
Henderson S, Horne M, Hills R, Kendall E. (2018) ‘Cultural competence in healthcare in the community: a concept analysis.’ Health Soc Care Community. 2018;26(4):590–603. https://doi.org/10.1111/hsc.12556.
Bennardi M, Diviani N, Gamondi C, Stüssi G, Saletti P, Cinesi I, Rubinelli S. Palliative care utilization in oncology and hemato-oncology: a systematic review of cognitive barriers and facilitators from the perspective of healthcare professionals, adult patients, and their families. BMC Palliat Care. 2020;19(1):1–7. https://doi.org/10.1186/s12904-020-00556-7.
Frey R, Gott M, Raphael D, Black S, Teleo-Hope L, Lee H, Wang Z. “Where do I go from here”? A cultural perspective on challenges to the use of hospice services. Health Soc Care Community. 2013;21(5):519–29. https://doi.org/10.1111/hsc.12038.
Sharma RK, Cameron KA, Chmiel JS, Von Roenn JH, Szmuilowicz E, Prigerson HG, Penedo FJ. Racial/ethnic differences in inpatient palliative care consultation for patients with advanced cancer. J Clin Oncol. 2015;33(32):3802–8. https://doi.org/10.1200/JCO.2015.61.6458.
Carvajal A, Haraldsdottir E, Kroll T, McCormack B, Errasti-Ibarrondo B, Larkin P. Barriers and facilitators perceived by registered nurses to providing person-centred care at the end of life. A scoping review. Int Pract Dev J. 2019;9(2):1–22. https://doi.org/10.19043/ipdj.92.008.
Ogbolu Y, Scrandis D, Fitzpatrick G. Barriers and facilitators of care for diverse patients: nurse leader perspectives and nurse manager implications. J Nurs Manag. 2018;26(1):3–10. https://doi.org/10.1111/jonm.12498.
Betancourt JR, Renfrew MR. Unequal treatment in the US: lessons and recommendations for cancer care internationally. J Paedi Haemat Oncol. 2011;1(33):S149-53. https://doi.org/10.1097/MPH.0b013e318230dfea.
Hadziabdic E, Lundin C, Hjelm K. Boundaries and conditions of interpretation in multilingual and multicultural elderly healthcare. BMC health services research. 2015;15(1):1–3. https://doi.org/10.1186/s12913-015-1124-5.
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Study conception and design: CB, BL. Literature search, screening, and data extraction: CB, BL, and OD. Data synthesis and interpretation: CB. Checking, data synthesis and interpretation: BL and OD. Contribution in the discussion and final write-up all authors. Manuscript drafting and revision and approval of final manuscript, all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This was a retrospective record review without any direct patient interaction by the study team. The research was performed in accordance with the Declaration of Helsinki and approved by two ethics committees. The ethics boards of the University of the Witwatersrand and Boston University reviewed and approved the study protocols and provided a waiver of informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary file 1.
PRISMA CHECKLIST. Supplementary file 2. Quality appraisal - CASP Appraisal scores
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Burke, C., Doody, O. & Lloyd, B. Healthcare practitioners’ perspectives of providing palliative care to patients from culturally diverse backgrounds: a qualitative systematic review. BMC Palliat Care 22, 182 (2023). https://doi.org/10.1186/s12904-023-01285-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12904-023-01285-3