Abstract
Background
The rising demand for improved aesthetics has driven the utilization of recently introduced aesthetic materials for creating custom post and core restorations. However, information regarding the fracture resistance of these materials remains unclear, which limits their practical use as custom post and core restorations in clinical applications.
Aim of the study
This study aimed to evaluate the fracture resistance of three non-metallic esthetic post and core restorations and their modes of failure.
Materials and methods
Thirty-nine single-rooted human maxillary central incisors were endodontically treated. A standardized post space preparation of 9mm length was performed to all teeth to receive custom-made post and core restorations. The prepared teeth were randomly allocated to receive a post and core restoration made of one of the following materials (n=13): glass fiber-reinforced composite (FRC), polyetheretherketone (PEEK) and polymer-infiltrated ceramic-network (PICN). An intraoral scanner was used to scan all teeth including the post spaces. Computer-aided design and computer-aided manufacturing (CAD-CAM) was used to fabricate post and core restorations. Post and core restorations were cemented using self-adhesive resin cement. All specimens were subjected to fracture resistance testing using a universal testing machine. Failure mode analysis was assessed using a stereomicroscope and SEM. The data was statistically analyzed using One-Way ANOVA test followed by multiple pairwise comparisons using Bonferroni adjusted significance level.
Results
Custom PEEK post and core restorations displayed the least fracture load values at 286.16 ± 67.09 N. In contrast, FRC exhibited the highest average fracture load at 452.60 ± 105.90 N, closely followed by PICN at 426.76 ± 77.99 N. In terms of failure modes, 46.2% of specimens with PICN were deemed non-restorable, while for PEEK and FRC, these percentages were 58.8% and 61.5%, respectively.
Conclusions
Within the limitation of this study, both FRC and PICN demonstrated good performance regarding fracture resistance, surpassing that of PEEK.
Similar content being viewed by others
Background
Endodontically treated teeth (ETT) exhibit an elevated susceptibility to fracture, primarily attributable to the substantial loss of tooth structure resulting from decay and cavity preparation. Furthermore, the occurrence of biochemical and structural alterations within dental structure can impede the long-term viability of ETT [1]. In order to mitigate the risk of fracture in ETT, restorative approaches involving cuspal coverage, such as onlays, overlays, endocrowns, and single crown restorations, are recommended [2]. However, in instances where there is insufficient dental structure to support a restoration, the utilization of post and core restorations becomes necessary to provide the requisite retention for a single crown restoration [3].
While prefabricated posts are a commonly employed solution for enhancing the retention of core materials within ETT, they face a notable challenge due to their circular cross-sectional shape, which does not conform precisely to the elliptical nature of root canals [4]. This incongruence results in an increased thickness of the cement layer between the post and root dentin, ultimately diminishing post retention and clinical efficacy [5]. On the other hand, custom post and core restorations handle the issue of excessive cement space and offer superior retention and internal fit [6]. Nevertheless, the intricate fabrication processes associated with custom posts may introduce distortions and irregularities to the metal surface following casting, potentially compromising the adaptation of the restoration [7].
Computer-Aided Design and Computer-Aided Manufacturing (CAD-CAM) technology has emerged as an effective method for fabricating post and core restorations with exceptional precision [8, 9]. This technology facilitates the utilization of various CAD-CAM materials, including zirconia, glass ceramic, and hybrid ceramics. It is worth noting that while zirconia and glass ceramic are among the materials that can be employed, they exhibit high moduli of elasticity, which can increase the risk of root fracture [10, 11].
Glass fiber-reinforced composite (FRC), polyetheretherketone (PEEK) and polymer-infiltrated ceramic-network (PICN) have emerged as promising alternatives to traditional materials like metal, zirconia, and glass ceramics in the field of restorative dentistry [12]. One notable advantage of these materials is that their modulus of elasticity closely approximates that of dentin, allowing them to function as effective shock absorbers, thereby reducing the stresses transmitted to the underlying tooth structure [13, 14]. The evolution of these materials, coupled with the integration of digital impressions and CAD-CAM systems, has made them a viable and practical option for restoring ETT [15,16,17].
Unlike prefabricated glass fiber posts containing unidirectional glass fibers combined within epoxy resin, the CAD-CAM FRC blank comprises a mixture of multidirectional glass fibers embedded within an epoxy resin matrix, exhibiting a modulus of elasticity of 26 GPa [18]. Polyetheretherketone (PEEK), possessing a modulus of elasticity of 4 GPa, [19, 20] represents a thermoplastic, partially crystalline high-performance polymer (HPP) [21]. It comprises an aromatic benzene molecular chain linked by interconnected ether and ketone functional groups [22]. Hybrid ceramic refers to a polymer-infiltrated ceramic network (PICN) exhibiting a modulus of elasticity of 30 GPa. The primary fine structure comprises a ceramic network constituting 86% by weight, reinforced by an acrylate polymer network. Both networks are intricately interlinked, forming a fully integrated composite [23, 24].
The field of digital dentistry has advanced with the aim of enhancing precision and expediting the production process [25]. Traditionally, the use of CAD-CAM technology for fabricating customized posts was constrained to the scanning of plaster models derived from conventional impressions [26]. However, alternative approaches have been proposed by different researchers, including the use of a traditional silicone impression that is scanned to manufacture a customized CAD-CAM post and core [27]. In contrast, the in vitro study conducted in this context employed an intraoral scanner for the direct scanning of the post space, thereby achieving a fully digital workflow [9].
The primary objective of this in vitro study was to assess the fracture resistance and failure patterns exhibited by three non-metallic esthetic custom post and core restorations, all of which have been produced using CAD-CAM technology. The null hypothesis posited that no difference would be observed in fracture resistance among these three materials.
Materials and methods
The materials used in the current study are listed in (Table 1). Power analysis was performed using a statistical software program (GPower 3.1.9.4; Henrich Heine University Dus-seldorf) [28]. Sample size was estimated assuming alpha error= 5% and study power= 80%. Eid et al. [29] reported a mean fracture resistance of post and core material manufactured from fiber reinforced composite of 367.06 ± 72.34, while AlKhatri et al. [30] reported a mean fracture resistance of 271.06 ± 69.57 in polymer infiltrated ceramic network group. Teixeira et al. [20] reported mean ± SD fracture resistance= 379.4 ± 119.8 in case of PEEK post and core. Calculations were performed using the formula stated below [31]. Based on comparison of means, with an effect size of 0.55, the sample size was calculated to be 12 per group, increased to 13 to make up for laboratory processing errors. The total sample size required = number of groups × number per group= 3 x 13 = 39 [32].
N is the required sample size, t is the two-tailed T distribution, \(\sigma\) represents the standard deviation, \(\alpha\) is the given probability value, \(\beta\) represents the study power, and d is the effect size.
This study received ethical approval from the Institutional Review Board of the Faculty of Dentistry at Alexandria University (IORG: 0008839, approval no. 0439-05/2022). Sample preparation and examination was done at the Conservative Dentistry Department laboratory at the Faculty of Dentistry, Alexandria University. A total of thirty-nine human maxillary central incisors, which had been extracted due to periodontal reasons, were obtained from the Department of Oral Surgery at the Faculty of Dentistry, Alexandria University. The selected teeth underwent a comprehensive visual and radiographic assessment to verify their absence of prior endodontic treatment, restorations, carious lesions, structural cracks, or signs of internal resorption. Additionally, this examination served to confirm the presence of a straight, single root canal with a fully matured apex. Cracks in teeth were identified visually through the utilization of a 6x magnifying loupe, coupled with transillumination employing an LED light source directed perpendicular to the tooth [33]. This method facilitated the detection of cracks by observing the diffraction of light when it intersected the crack, thereby enabling the precise localization of the crack and the exclusion of affected specimens [34]. Following these assessments, the teeth were subjected to a thorough ultrasonic cleaning procedure.
Specimens preparation
The collected specimens were preserved in a 0.9% saline solution at room temperature to prevent desiccation. Subsequently, the teeth were carefully sectioned, using a double-sided diamond disk (Dynex Separating discs Brillant; Renfert), approximately 2 mm coronal to the cement-enamel junction. This cutting process was carried out with a low-speed handpiece, while ensuring a constant flow of copious coolant. Each tooth underwent endodontic treatment utilizing rotary files (PROTAPER-GOLD; Dentsply Sirona) up to size F5. Canal irrigation was performed using 5.25% sodium hypochlorite. Following this, paper points were used to dry the canals, and obturation was carried out using the lateral compaction technique with gutta-percha cones (Spident; Meta Biomed Co) and resin sealer (AD Seal; Meta Biomed) [9]. The remaining structure of every tooth was prepared with a 2 mm ferrule coronal to the CEJ. To remove the gutta-percha, Gates Glidden drill size 3 (Dentsply Sirona) was used. Subsequently, post spaces were standardized at a length of 9 mm with a black color-coded drill (Unimetric; Dentsply Sirona). The teeth were embedded in an auto-polymerizing acrylic resin (Acrostone Acrylic Material-Cold Cure; ACROSTONE Co) to a level 2mm apical to the CEJ to simulate the bone level.
Grouping of the specimens
All 39 teeth were randomly allocated to receive post and core restorations using one of the following materials (n=13): FRC (Trilor; Bioloren), PEEK (breCam.BioHPP; Bredent), and PICN (Vita Enamic; VITA Zahnfabrik). The randomization procedures were performed by a statistical website (Randomizer.org).
Scanning of the post space
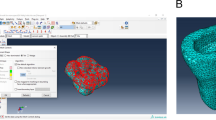
The post spaces that had been prepared were scanned using an intraoral scanner (MEDIT i700; Medit), to acquire standard tessellation language (STL) files [8, 9]. The justification for utilizing intraoral scanners for post space scanning stems from their ability to precisely capture intricate impressions of the post space inside the tooth, as stated in previous studies [8, 35, 36].
Designing and milling of post and core restorations
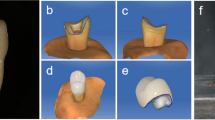
The post and core 3D models were designed using a dental CAD program (exocad Dental DB; exocad GmbH) with an 80 µm cement space for adhesive bonding [37]. The core had dimensions of 4 mm in height and 3 mm in thickness, measured diagonally from the fossa to the buccal surface, as illustrated in (Fig. 1), to simulate the abutment of prepared teeth. The CAD files of the post and core restorations were exported to a CAM program (HyperDent; FOLLOW ME! Technology) to be nested in the corresponding materials. A dental milling machine (CORiTEC 250i touch; imes-icore) was used for the fabrication of post and core restorations.
Cementation of post and core restorations
The PEEK and FRC restorations were sandblasted using 50 µm aluminum oxide (Al2 O3) at 2 bar for 10 seconds [9, 29]. Following this, a silane coupling agent (SILAN-IT; iTena) was applied to the FRC restorations [29]. Visiolink primer (Visio.Link, bredent) was applied to the surface of PEEK posts, followed by a 90-second light-curing process [38, 39]. Polymer infiltrated ceramic network restorations were etched with 9% hydrofluoric acid (CERAM-ETCH; iTena) for 60 seconds, followed by rinsing with water for 60 seconds, air drying for 20 seconds, and the application of a silane coupling agent (SILAN-IT; iTena), with subsequent air drying in accordance with the manufacturer’s instructions [40].
To cement the post and core restorations in their respective teeth, a dual-cure resin cement (TOTALCEM; iTena) was utilized. The cement was placed within the post space of the teeth using a spiral rotary instrument (Lentulo; Dentsply Sirona) followed by the application of a static load of 2 kg for 5 minutes This ensured the full seating of the restorations and the creation of a uniform cement film thickness [9]. In this study, crown fabrication was not employed due to the acknowledged effect of crowns in augmenting fracture resistance values [39, 41,42,43,44]. The main aim of this research was to amplify the focus on the intrinsic behavior of the materials themselves.
Aging of the specimens
The samples underwent 500 thermal cycles ranging from 5℃ to 55℃ with a dwell time of 1 minute and a 30-second transfer time using the thermocycling machine (Custom made in dental biomaterials dept; faculty of dentistry Alexandria University). Following the thermocycling process, all specimens were subjected to cyclic loading consisting of 50,000 load cycles at a frequency of 2Hz, with a load of 50N, utilizing a load cycling machine [45, 46]. Before testing, all specimens were stored in distilled water at 37°C for 7 days.
Fracture resistance test
The specimens were mounted in a cylindrical metal holder with an inclination of 45-degree as shown in (Fig. 2). The specimens were subjected to fracture test using a universal testing machine (5ST; Tinius Olsen). A custom-made blunt rounded chisel head (2 mm in size) was used to apply force at a crosshead speed of 1 mm/min. The force was applied at a 135-degree angle to the tooth’s long axis, targeting the palatal surface, positioned 2 mm cervical to the incisal edge [47]. Each specimen’s failure load was recorded in Newton. Failure was defined as the point at which the strain-stress diagram abruptly dropped, and fracture resistance was recorded as the moment at which the loading force reached its maximum value [48].
Assessment of mode of failure
Specimens, fragments and failure patterns were examined using stereomicroscope (Olympus; Olympus Co) at x4 magnification and scanning electron microscope (SEM) at x13 and x500 magnification with an accelerating voltage of 20 KV (Jeol JSM-IT200; Jeol Ltd).
In cases where failure manifested as a fracture in the core, post, or a tooth fracture occurring above the level of the cement-enamel junction, it was considered a favorable fracture that could potentially be repaired. Conversely, an unfavorable fracture encompassed root fractures occurring below the level of the cement-enamel junction, including vertical, horizontal, or oblique root fractures [49,50,51].
Statistical analysis
Descriptive statistics were calculated as means standard deviation (SD), median, interquartile range (IQR), and range (Min – Max) for the fracture resistance variable, in addition to frequencies and percentages for the restorability variable. Normality was tested for the fracture resistance variable using descriptive statistics, plots (histogram and Q-Q plots), and normality tests. The variable showed normal distribution, so parametric analysis was adopted. Comparison between the three study groups was done using One-way ANOVA, followed by multiple pairwise comparisons using Bonferroni adjusted significance level. Comparison of restorablitiy was performed using Chi-square test. Significance level was set at p value <.05. Data were analyzed using IBM SPSS for Windows (Version 26.0)
Results
The mean fracture resistance of all groups is shown in (Table 2). The highest mean fracture resistance was recorded in FRC (452.60 ±105.90 N), followed by PICN (426.76 ±77.99 N), and the lowest mean fracture resistance PEEK (286.16 ±67.09 N) are presented in (Table 2). The one-way ANOVA test indicated a statistically significant difference among the tested groups.
Bonferroni adjusted post-hoc tests revealed that there was no statistically significant difference between FRC and PICN, while PEEK exhibited a statistically significant difference when compared to the other two groups (P<.05) (Table 2). There was no significant difference in failure mode and restorability between the tested groups (Table 3).
Examining samples visually and using scanning electron microscope (SEM) and stereomicroscope imaging revealed distinct fracture patterns. In FRC samples, observations indicated favorable fractures marked by core separation that didn’t impact the post or tooth (Figs. 3A, 6A). Conversely, unfavorable outcomes included post damage and vertical root fractures below the CEJ (Figs. 4A, 7A). SEM images also revealed a pattern of brush-like cracking attributed to the rupture of these fibers (Fig. 5A )[52].
Scanning electron micrographs at 13 X magnification of three tested groups displaying favorable failure patterns: A FRC with core separated from post. B PEEK specimen with a gap between post and core restoration and tooth indicating dislodgement of restoration. C PICN specimen with fracture within core
Scanning electron micrographs with 13 X magnification of three tested groups with non-favorable failure patterns. A FRC sample displayed fractures in both post and core restoration and vertical root fracture below CEJ. B PEEK sample exhibited vertical root fracture below CEJ, while post and core restoration remained intact. C PICN sample showed fractures in both post and core restoration, and vertical root fracture below CEJ
PEEK samples that exhibited favorable fractures underwent dislodgement without causing fractures in any component (Figs. 3B, 6B). Nevertheless, the unfavorable failures were distinguished by vertical root fractures occurring below the CEJ without any accompanying fractures in the post or the core (Figs. 4B, 7B). The SEM analysis notably showed a smooth surface on the PEEK post (Fig. 5B).
Stereomicroscope images with 4 X magnification showing nonfavorable fracture patterns in three tested groups: A, FRC sample displayed fractures in both post and core restoration and vertical root fracture below CEJ. B, PEEK sample exhibited vertical root fracture below CEJ, while post and core restoration remained intact. C, PICN sample showed fractures in both post and core restoration, and vertical root fracture below CEJ
In PICN, the favorable failure mode involved fractures within the core segments (Figs. 3C, 6C), contrasting with the unfavorable pattern represented by a vertical root fracture below the CEJ and a fracture in the post (Figs. 4C, 7C). Additionally, SEM micrographs displayed a rough surface, showcasing the heterogeneity of components (Fig. 5C).
Discussion
This in vitro study examined the fracture resistance of three aesthetic materials utilized as post and core restorations manufactured using CAD-CAM technology. Among the three tested groups, the custom PEEK post and core restorations showed the least values in fracture resistance. The fracture resistance of the custom FRC and PICN post and core restorations showed notably superior results when compared to the customized PEEK post and core restorations. The null hypothesis, suggesting no difference in fracture resistance among these three materials, was rejected.
In the present study, the selection of the maxillary central incisors was based on their pronounced need for aesthetic restoration. In addition to their characteristic feature of possessing a straight, single, and flared root canal. This choice was made to facilitate standardization and enhance validity of the study in comparison to utilizing artificial teeth. A standardized post space of 9 mm in length was created to align with the protocols followed in previous studies [43, 53].
An intraoral scanner was utilized to scan the teeth, including post spaces, enabling the fabrication of post and core restorations through a fully digital workflow. This method aimed to enhance precision, reduce time consumption, and confront the limitations associated with traditional methods. Alhasher et al. [8] proposed that employing intraoral scanners for constructing single-piece post and core restoration could offer a reliable alternative to conventional methods. Elter et al. [35] suggested that intraoral scanners are viable for capturing impressions of the post space when the post depth measures less than 14 mm, thus facilitating a streamlined impression procedure. Additionally, Vogler et al. [36] concluded that the fully digital chairside workflow, coupled with CAD-CAM-fabricated post and core, displayed superior accuracy of fit and practicality in impression-taking compared to conventionally fabricated cast post and core. Consequently, CAD-CAM technology holds the potential for enabling single-session restoration of endodontically treated teeth with customized post and core solutions, offering efficiency and precision in dental practice.
Previous studies employed ceramic materials with high elastic modulus such as lithium disilicate and zirconia to construct custom post and core restorations. It was found that there was stress concentration on root dentin resulting in catastrophic failure [44, 47, 54,55,56,57,58]. The investigated materials in the current study exhibit a modulus of elasticity close to dentin, approximately 18 GPa, [59] leading to a more uniform distribution of stress along the root. Consequently, this even distribution mitigates the occurrence of vertical root fractures.
In the present study, the exclusion of crown fabrication aimed to amplify the effect of post and core materials in the assessment of fracture resistance of endodontically treated teeth [41,42,43,44]. On the other hand, studies [40, 60, 61] that used a crown or coping to cover post and core restorations had fracture resistance higher than the current study, however, this might conceal the actual differences between the used custom made post and core materials. Thermal and mechanical aging have significant impacts on the bonding and fracture resistance of endodontically treated teeth restored with post and core restorations. Despite the relatively brief duration of thermomechanical aging in our study, the observed outcomes align with findings from comparable studies, [45, 46] which also reported similar statistical differences and failure modes. Notably, mechanical loading exerted direct effect on the integrity of the post and core restoration, while thermal cycling notably affected the interface of cemented surfaces, exacerbating the degradation of bond strength and mechanical properties of the post and core restoration [62, 63]. Moreover, several studies [9, 30, 42, 47, 55, 64] refrained from conducting artificial aging, emphasizing that their investigations were specifically focused on the materials and methodology rather than projecting outcomes under different conditions.
The applied force was oriented at a 135-degree angle in relation to the long axis of the tooth, targeting the palatal surface. This was achieved using a specially designed chisel head designed to emulate the lower central incisor, thereby replicating the clinical situation [47].
While PEEK exhibits comparable elastic modulus and flexural strength to dentin, excessive loading on PEEK post and core restorations tends to concentrate stress on the surrounding cement layer [19]. This often results in debonding, given that the sole bonding mechanism relies on mechanical interlocking attained through sandblasting [9]. Heightened stress can concentrate on the tooth, potentially causing catastrophic root fractures. The recorded values for PEEK posts and core restorations were 286.16 ± 67.09 N, aligning with findings by Özarslan et al. [65] who similarly assessed fracture resistance across PEEK, zirconia, and glass fiber. Their study revealed that the average failure loads of PEEK posts and core restorations were 306.7 ± 74.0 N.
Additionally, there is agreement with Teixeira et al. [20] who conducted a comparison of the fracture resistance between custom-made post-and-cores of PEEK and Nano-ceramic Composite. Their findings reported a mean fracture resistance of PEEK post and core restoration at 379.46 ± 119.8 N.
In contrast to our findings, Abdelmohsen et al. [39] investigated the fracture resistance of various post and core systems. They reported mean values of fracture resistance for CAD-CAM milled PEEK post and core restorations at 1055.25 ± 119.31 N. This discrepancy may be attributed to the study’s focus on premolars and the varied angulations of applied force.
The fracture resistance mean values for the PICN group in this investigation were measured at 426.76 ±77.99N. These findings were consistent with the observations of Spina et al. [43] where they reported mean fracture resistance values of 414.5 ±83.9N for PICN and 407.6 ±109N for FRC. Additionally, Elmaghraby et al. [45] also observed agreement in their research, noting fracture resistance mean values of 386.6 ±25.78N for one-piece post and core PICN restorations.
The findings in this study contrasted with those of Alkhatri et al. [30] who investigated the impact of materials on the apical extension of root fracture. Alkhatri et al. reported mean fracture resistance values of PICN as 271.06 ±69.57N. The variations in observed values could stem from employing diverse approaches in fabricating the post and core utilizing acrylic resin. These differences might arise due to distinct methodologies, such as variations in resin composition, application techniques, curing processes, or the specific protocols followed during fabrication.
The FRC group exhibited the highest mean failure load value of 452.60 ±105.90N. This finding is consistent with the results of Eid et al. [29] who investigated the fracture resistance and failure mode of endodontically treated teeth restored with custom-made FRC post and core restorations. They noted a mean fracture resistance of 367.06 ±72.34N for CAD-CAM glass fiber post and core restorations, further supporting the consistent performance of glass fiber reinforced composite materials in enhancing fracture resistance.
In the current study, the fracture resistance among the three tested groups fiber reinforced composite samples, PEEK, and polymer infiltrated ceramic network measured 452.60 ± 105.90 N, 286.16 ± 67.09 N, and 426.76 ± 77.99 N, respectively. These values exceed the recorded maximal occluding force generated by maxillary incisors, which stands at 146 ± 44 N [30]. This indicates that each of the three tested groups could be considered acceptable materials of choice for anterior tooth restoration requiring a customized post and core.
In terms of the failure mode, no significant difference was noted among the tested groups. PICN demonstrated the most favorable results, followed by PEEK, while the fewest number of restorable specimens were found in FRC, with counts of 7, 6, and 5, respectively. These findings align with the majority of previous studies [30, 43, 45, 61, 65].
Due to its relatively rigid molecular chain structure, PEEK demonstrates notable ductility, allowing for substantial deformation under unilateral stress during compression [20]. When subjected to stresses within its yield limit, the material undergoes elastic deformation. However, when these stresses surpass the yield limit, [19] PEEK experiences plastic deformation and bending without encountering fracture or chipping [21]. This behavior contributes to understanding the prevalent failure patterns observed in PEEK post and core restorations. Applied force tends to transfer to the intermediate cement, causing dislodgement without inducing fracture in any component, whether the post, core, or the tooth structure itself. Alternatively, this force concentration on the root can lead to a vertical root fracture as reported in the current study.
According to the study conducted by Özarslan et al. [65] which focused on comparing the fracture strength of endodontically treated teeth restored with different post-core systems, it was found that 40% of the specimens experienced decementation without fracture. This finding is consistent with our research results. On the other hand, Pourkhalili et al. [64] in their study on the fracture resistance of various post and core systems, reported that none of the specimens exhibited debonding. This disparity in results could be attributed to their use of premolars instead of anterior teeth and the application of force in a different direction in their study. Additionally, Kasem et al. [66] utilized customized PEEK post and core restorations for compromised teeth, documented a successful five-year follow-up. However, the favorable outcome observed can be explained by the ferrule effect of several millimeters used in the case report.
The failure of the FRC material stemmed from the rupture of its fibers. In instances where a fiber-reinforced material experiences failure, a crack initiates within the matrix and proceeds along the interface encircling a dispersed fiber, resulting in the rupture of the fiber itself. Subsequently, the load transfers to adjacent fibers, causing them to rupture in sequence. This mode of failure is commonly described as ‘brush-like’ cracking [37, 52]. The fractured samples in the PICN group exhibited a crack propagation failure mechanism, aligning with the observations made by Aboushelib et al. [24] They reported a diminished resistance in the polymeric matrix of resin-infiltrated ceramics, resulting in a linear crack and the formation of a slipstream path in the direction of crack propagation.
In the current study, the unfavorable outcomes were 61.5%, 53.8%, and 46.2% for glass fiber reinforced composite, PEEK, and polymer infiltrated ceramic network, respectively. However, these results still outperformed those reported by Hamdy et al. [55] where 80% of translucent zirconia post specimens were deemed non-restorable, as well as by Özarslan et al. [65] who found that 72.5% of zirconia post-core group samples were irreparable. Additionally, Alkhatri et al. [30] investigated the impact of post and core materials on the apical extension of root fracture in root canal treated teeth. It was observed that in the PICN group, the extension of root fracture tended to be more coronal compared to the metal and zirconia groups, likely due to variations in the modulus of elasticity among the tested materials. Additionally, Bittner et al. [57] conducted a study comparing a one-piece milled zirconia post and core with other post-and-core systems. Their findings indicated that all specimens in the one-piece milled zirconia post and core group experienced catastrophic root failure.
Similar to any other in vitro study, it’s important to note that the current research couldn’t entirely replicate in vivo conditions as most fractures occurring in vivo would likely be due to fatigue conditions rather than a compressive static load. This study doesn’t fully replicate the clinical situation as it doesn’t consider the use of crown restoration, which, when applied with adequate ferrule, significantly increases the fracture resistance of endodontically treated teeth (ETT).
Conclusions
Within the limitation of this study, it could be concluded that:
-
1. CAD-CAM milled FRC and PICN post and core restorations possess satisfactory fracture resistance in comparison to PEEK post and core restorations.
-
2. In terms of failure mode, there were no noteworthy distinctions observed among the tested groups regarding the restorability of teeth after failure.
Availability of data and materials
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- EET:
-
Endodontically treated teeth
- CAD-CAM:
-
Computer aided design and computer aided manufacturing
- FRC:
-
Fiber reinforced composite
- PEEK:
-
Polyether ether ketone
- PICN:
-
Polymer infiltrated ceramic network
References
Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int. 2008;39:117–29.
Kalay TS, Yildirim T, Ulker M. Effects of different cusp coverage restorations on the fracture resistance of endodontically treated maxillary premolars. J Prosthet Dent. 2016;116:404–10.
Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004;30:289–301.
Kul E, Yeter KY, Aladag LI, Ayrancı LB. Effect of different post space irrigation procedures on the bond strength of a fiber post attached with a self-adhesive resin cement. J Prosthet Dent. 2016;115:601–5.
Vano M, Goracci C, Monticelli F, Tognini F, Gabriele M, Tay F, et al. The adhesion between fibre posts and composite resin cores: the evaluation of microtensile bond strength following various surface chemical treatments to posts. Int Endod J. 2006;39:31–9.
Balkenhol M, Wöstmann B, Rein C, Ferger P. Survival time of cast post and cores: a 10-year retrospective study. J Dent. 2007;35:50–8.
de Moraes AP, Neto VP, Boscato N, Pereira-Cenci T. Randomized clinical trial of the influence of impression technique on the fabrication of cast metal posts. J Prosthet Dent. 2016;116:47–51.
Alhasher HK, Alfarsi MA. A Fully Digital Method to Fabricate Custom Hybrid Ceramic One-Piece Post-and-Core: A Proof of Concept. Res Square 2022:doi: https://doi.org/10.21203/rs.3.rs-2308075/v1.
Attia MA, Shokry TE, Abdel-Aziz M. Effect of different surface treatments on the bond strength of milled polyetheretherketone posts. J Prosthet Dent. 2022;127:866–74.
Luthardt RG, Holzhüter MS, Rudolph H, Herold V, Walter MH. CAD/CAM-machining effects on Y-TZP zirconia. Dent Mater. 2004;20:655–62.
Vinothkumar TS, Kandaswamy D, Chanana P. CAD/CAM fabricated single-unit all-ceramic post–core–crown restoration. J Conserv Dent. 2011;14:86–9.
Awada A, Nathanson D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J Prosthet Dent. 2015;114:587–93.
Georgiev J, Vlahova A, Kissov H, Aleksandrov S, Kazakova R. Possible application of BioHPP in prosthetic dentistry: a literature review. J IMAB-Ann Proceed Sci Papers. 2018;24:1896–8.
Coldea A, Swain MV, Thiel N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent Mater. 2013;29:419–26.
Libonati A, Di Taranto V, Gallusi G, Montemurro E, Campanella V. CAD/CAM customized glass fiber post and core with digital intraoral impression: a case report. Clin Cosmet Investig Dent. 2020;12:17–24.
Pinto A, Arcuri L, Carosi P, Nardi R, Libonati A, Ottria L, et al. In vitro evaluation of the post-space depth reading with an intraoral scanner (IOS) compared to a traditional silicon impression. Oral Implantol (Rome). 2017;10:360–8.
Yamada Y, Tsubota Y, Fukushima S. Effect of restoration method on fracture resistance of endodontically treated maxillary premolars. Int J Prosthodont. 2004;17:94–8.
Ruschel GH, Gomes ÉA, Silva-Sousa YT, Pinelli RGP, Sousa-Neto MD, Pereira GKR, et al. Mechanical properties and superficial characterization of a milled CAD-CAM glass fiber post. J Mech Behav Biomed Mater. 2018;82:187–92.
Reda R, Zanza A, Galli M, De Biase A, Testarelli L, Di Nardo D. Applications and clinical behavior of biohpp in prosthetic dentistry: A short review. J Compos Sci. 2022;6:90.
Teixeira K, Duque T, Maia H, Gonçalves T. Fracture resistance and failure mode of custom-made post-and-cores of polyetheretherketone and nano-ceramic composite. Oper Dent. 2020;45:506–15.
Papia E, Brodde SAC, Becktor JP. Deformation of polyetheretherketone, PEEK, with different thicknesses. J Mech Behav Biomed Mater. 2022;125:104928.
Najeeb S, Zafar MS, Khurshid Z, Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J Prosthet Dent. 2016;60:12–9.
Lauvahutanon S, Takahashi H, Shiozawa M, Iwasaki N, Asakawa Y, Oki M, et al. Mechanical properties of composite resin blocks for CAD/CAM. Dent Mater J. 2014;33:705–10.
Aboushelib MN, Elsafi MH. Survival of resin infiltrated ceramics under influence of fatigue. Dent Mater. 2016;32:529–34.
Mangano FG, Hauschild U, Veronesi G, Imburgia M, Mangano C, Admakin O. Trueness and precision of 5 intraoral scanners in the impressions of single and multiple implants: a comparative in vitro study. BMC Oral Health. 2019;19:1–14.
Chen Z, Li Y, Deng X, Wang X. A novel computer-aided method to fabricate a custom one-piece glass fiber dowel-and-core based on digitized impression and crown preparation data. J Prosthodont. 2014;23:276–83.
Spina DRF, da Costa RG, Correr GM, Rached RN. Scanning of root canal impression for the fabrication of a resin CAD-CAM-customized post-and-core. J Prosthet Dent. 2018;120:242–5.
Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91.
Eid R, Juloski J, Ounsi H, Silwaidi M, Ferrari M, Salameh Z. Fracture resistance and failure pattern of endodontically treated teeth restored with computer-aided design/computer-aided manufacturing post and cores: a pilot study. J Contemp Dent Pract. 2019;20:56–63.
Alkhatri R, Saleh ARM, Kheder W. Impact of post and core materials on the apical extension of root fracture in root canal treated teeth. J Mater Res Technol. 2021;10:730–7.
Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35:121–6.
Petrie A, Sabin C. Medical Statistics at a Glance. 3rd ed. Oxford: Blackwell; 2009.
Bhanderi S. Facts about cracks in teeth. Prim Dent J. 2021;10:20–7.
Yu M, Li J, Liu S, Xie Z, Liu J, Liu Y. Diagnosis of cracked tooth: Clinical status and research progress. Jpn Dent Sci Rev. 2022;58:357–64.
Elter B, Diker B, Tak Ö. The trueness of an intraoral scanner in scanning different post space depths. J Dent. 2022;127:104352.
Vogler JAH, Billen L, Walther K-A, Wöstmann B. Conventional cast vs. CAD/CAM post and core in a fully digital chairside workflow–An in vivo comparative study of accuracy of fit and feasibility of impression taking. J Dent. 2023;136:104638.
Eid R, Tribst JPM, Juloski J, Özcan M, Salameh Z. Effect of material types on the fracture resistance of maxillary central incisors restored with CAD/CAM post and cores. Int J Comput Dent. 2021;24:41–51.
Wang J, Gu JT, Meng M, Wang CY, Chen JH, Niu LN. Polyetheretherketone framework for implant-supported full-arch fixed dental prostheses in a periodontitis patient with a 6-year follow-up: a case report. Chin J Dent Res. 2022;25:149–58.
Abdelmohsen NA, Zohdy MM, Abdelsattar GA, Wahsh MM. Fracture resistance of different post-core systems restoring mandibular premolars. Mansoura Journal of Dentistry 2022. https://doi.org/10.21608/MJD.2021.223397. https://mjd.journals.ekb.eg/article_223397.html.
Borzangy SS, Saker SM, Al-Zordk WA. Effect of restoration technique on resistance to fracture of endodontically treated anterior teeth with flared root canals. J Biomed Res. 2019;33:131–8.
Dilmener FT, Sipahi C, Dalkiz M. Resistance of three new esthetic post-and-core systems to compressive loading. J Prosthet Dent. 2006;95:130–6.
Das G, Rana MH, Khan SA, Chaudhary MAG, Sibghatullah M, Kumar B. Assessment of Fracture Resistance of PEEK and Fibre Posts of the Endodontically Treated Teeth. Material Plast. 2022;59:207–13.
Spina D, Costa R, Farias I, Cunha L, Ritter A, Gonzaga C, et al. CAD/CAM post-and-core using different esthetic materials: Fracture resistance and bond strengths. Am J Dent. 2017;30:299–304.
Saad KB, Bakry SI, AboElhassan RG. Fracture resistance of endodontically treated teeth, restored with two post-core systems in different post space diameters (in vitro study). BMC Oral Health. 2023;23:992.
Maghraby A, Shalaby YA, Alabbassy FH, Azer AS. Fracture resistance of cad/cam one-piece and two-piece post-core-crown restorations using two different materials (In vitro study). Alex Dent J. 2023;48:146–53.
Schmoldt SJ, Kirkpatrick TC, Rutledge RE, Yaccino JM. Reinforcement of simulated immature roots restored with composite resin, mineral trioxide aggregate, gutta-percha, or a fiber post after thermocycling. J Endod. 2011;37:1390–3.
Alkhatri R, Saleh ARM, Kheder W. Evaluating fracture resistance and failure modes of root filled teeth restored with CAD/CAM-fabricated post and core. Clin Cosmet Investig Dent. 2019;11:349–55.
Fragou T, Tortopidis D, Kontonasaki E, Evangelinaki E, Ioannidis K, Petridis H, et al. The effect of ferrule on the fracture mode of endodontically treated canines restored with fibre posts and metal-ceramic or all-ceramic crowns. J Dent. 2012;40:276–85.
Akkayan B, Gülmez T. Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent. 2002;87:431–7.
Pontius O, Nathanson D, Giordano R, Schilder H, Hutter JW. Survival rate and fracture strength of incisors restored with different post and core systems and endodontically treated incisors without coronoradicular reinforcement. J Endod. 2002;28:710–5.
A. Alharbi F, Nathanson D, Morgano SM, Baba NZ. Fracture resistance and failure mode of fatigued endodontically treated teeth restored with fiber-reinforced resin posts and metallic posts in vitro. Dent Traumatol. 2014;30:317–25.
Kompiš V, Kopernik M, Trebacz L, Pietrzyk M. Modelling of fatigue behaviour of hard multilayer nanocoating system in nanoimpact test. In: Kamipis V, (ed). Composites with Micro-and Nano-Structure: Computational Modeling and Experiments: Springer; 2008. 137-59. https://link.springer.com/chapter/10.1007/978-1-4020-6975-8_8.
Nahar R, Mishra SK, Chowdhary R. Evaluation of stress distribution in an endodontically treated tooth restored with four different post systems and two different crowns-A finite element analysis. J Oral Biol Craniofac Res. 2020;10:719–26.
de Andrade GS, Bottino MA, Valandro LF, Özcan M. A study on stress distribution to cement layer and root dentin for post and cores made of CAD/CAM materials with different elasticity modulus in the absence of ferrule. J Clin Exp Dent. 2019;11:e1–8.
Hamdy A. Fracture resistance of different esthetic post and core materials and assessment their mode of failure. Egypt Dent J. 2017;63:3617–24.
Lee JH. Fabricating a custom zirconia post-and-core without a post-and-core pattern or a scan post. J Prosthet Dent. 2018;120:186–9.
Bittner N, Hill T, Randi A. Evaluation of a one-piece milled zirconia post and core with different post-and-core systems: An in vitro study. J Prosthet Dent. 2010;103:369–79.
Sipahi C, Toksoy F, Ayyildiz S, Özcan M. Effect of physical and physicochemical surface treatment methods on the tensile strength of CAD/CAM-fabricated zirconia posts and cores luted to root canals. Int J Periodontics Restorative Dent. 2011;31:563.
Zhang YR, Du W, Zhou XD, Yu HY. Review of research on the mechanical properties of the human tooth. Int J Oral Sci. 2014;6:61–9.
Haralur SB. Fracture resistance of endodontically treated teeth restored with various esthetic posts. Technol Health Care. 2021;29:243–52.
Pang J, Feng C, Zhu X, Liu B, Deng T, Gao Y, et al. Fracture behaviors of maxillary central incisors with flared root canals restored with CAD/CAM integrated glass fiber post-and-core. Dent Mater J. 2019;38:114–9.
Vilde T, Stewart CA, Finer Y. Simulating the Intraoral Aging of Dental Bonding Agents: A Narrative Review. Dentist J. 2022;10:13.
Szczesio-Wlodarczyk A, Fronczek M, Ranoszek-Soliwoda K, Grobelny J, Sokolowski J, Bociong K. The First Step in Standardizing an Artificial Aging Protocol for Dental Composites. Dent Mater. 2023;39:e73.
Pourkhalili H, Maleki D. Fracture resistance of polyetheretherketone, Ni-Cr, and fiberglass postcore systems: An: in vitro: study. Dent Res J. 2022;19:20.
Özarslan M, Büyükkaplan UŞ, Özarslan MM. Comparison of the fracture strength of endodontically treated teeth restored with polyether ether ketone, zirconia and glass-fibre post-core systems. Int J Clin Pract Suppl. 2021;75:e14440.
Kasem AT, Shams M, Tribst JPM. The use of polyetheretherketone (PEEK) as an alternative post and core material: Five-year follow-up report. Dentist J. 2022;10:237.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This study was not funded by any agency in the public, commercial, or non-profit sectors.
Author information
Authors and Affiliations
Contributions
I.F. contributed to the study design, the data acquisition, analysis, and interpretation, and wrote the manuscript draft. I.A. contributed to the study design, and the interpretation of the results, and revised the manuscript. A.A. contributed to the study design, revised the manuscript, and supervised the work. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the Faculty of Dentistry, Alexandria University (IORG:0008839, approval no. 0439-05/2022). All methods were performed in accordance with the Declaration of Helsinki and the ethical guidelines adopted by the Research Ethics Committee of the Faculty of Dentistry, Alexandria University. No human participants were involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fathey, I.T., Azer, A.S. & Abdelraheem, I.M. Fracture resistance and failure mode of three esthetic CAD-CAM post and core restorations. BMC Oral Health 24, 523 (2024). https://doi.org/10.1186/s12903-024-04273-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04273-y