Abstract
Background
Previous observational studies have shown that people with dental scaling (DS) had decreased risk of stroke. However, limited information is available on the association between DS and poststroke outcomes. The present study aimed to evaluate the effects of regular DS on the complications and mortality after stroke.
Methods
We conducted a retrospective cohort study of 49,547 hospitalized stroke patients who received regular DS using 2010–2017 claims data of Taiwan’s National Health Insurance. Using a propensity-score matching procedure, we selected 49,547 women without DS for comparison. Multiple logistic regressions were used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) of poststroke complications and in-hospital mortality associated with regular DS.
Results
Stroke patients with regular DS had significantly lower risks of poststroke pneumonia (OR 0.58, 95% CI 0.54–0.63), septicemia (OR 0.58, 95% CI 0.54–0.63), urinary tract infection (OR 0.68, 95% CI 0.66–0.71), intensive care (OR 0.81, 95% CI 0.78–0.84), and in-hospital mortality (OR 0.66, 95% CI 0.62–0.71) compared with non-DS stroke patients. Stroke patients with regular DS also had shorter hospital stays (p < 0.0001) and less medical expenditures (p < 0.0001) during stroke admission than the control group. Lower rates of poststroke adverse events in patients with regular DS were noted in both sexes, all age groups, and people with various types of stroke.
Conclusion
Stroke patients with regular DS showed fewer complications and lower mortality compared with patients had no DS. These findings suggest the urgent need to promote regular DS for this susceptible population of stroke patients.
Similar content being viewed by others
Background
Stroke was considered one of the leading causes of death worldwide, and the number of stroke deaths increased 41.4% between 1990 and 2017 with approximately 5.5 million stroke deaths per year [1, 2]. The high lifetime prevalence and economic burden to society implicated the importance of stroke prevention and poststroke care [3]. Stroke in many patients is caused by atherosclerosis, which is a sustained, dynamic disease hallmarked by chronic inflammation in the vasculature. Previous studies have demonstrated that microbial infections accelerate vascular inflammation, suggesting that chronic infection also plays an important role in the development of atherosclerosis [4, 5]. Although the epidemiology, pathogenesis, prevention, and treatment of stroke have been well established [6,7,8], the investigation of protective factors remains an area of research interest.
Oral hygiene is crucial for general health, with periodontitis being one of the most prevalent chronic inflammatory diseases worldwide [9, 10]. Several pro-inflammatory cytokines, such as interleukin (IL)-1, IL-6, C-reactive protein, fibrinogen and serum amyloid A, have been shown to be elevated in patients with periodontitis [11, 12]. Additionally, major disease-causing bacterial strains of periodontitis are also present in atherosclerotic plaques [13]. Many observational studies and meta-analysis have reported that patients with periodontitis have increased risk for stroke [9, 11, 14, 15]. In contrast, oral hygiene care such as tooth brushing at least twice a day and regular professional dental cleaning (scaling and root planing) reduced the risk of future Meniere’s disease, rheumatoid arthritis, stroke, and cardiovascular events in general population [16,17,18,19].
Dental scaling (DS), meaning deep tooth cleaning with removal of dental plaque and calculus, was associated with a decreased risk for stroke, irrespective of the presence of periodontitis or not [9,10,11]. Patients with periodontitis are more at risk for pyogenic liver abscess than controls, particularly when they have no DS [20]. DS was significantly associated with lower risks of progression and mortality to end-stage renal disease in patients with chronic kidney disease [21]. Both dental scaling and intensive treatment for periodontal disease are associated with a lower risk of further ischaemic stroke events [9]. Regular DS once a year or more was shown to reduce cardiovascular risk by 14% in one population-based cohort study [19]. However, limited evidence is available on the association between regular DS and poststroke outcomes. Thus, we conducted a nationwide matched study using research data from Taiwan’s National Health Insurance to investigate the effects of regular DS on the outcomes after stroke.
Methods
Source of data
We mined the research database of Taiwan’s National Health Insurance to conduct this study. The National Health Insurance program has been implemented in Taiwan since March 1995. The research database of the National Health Insurance collected all medical reimbursement claims since 1996 and is available to researchers with beneficiaries’ identification scrambled to protect privacy. The available information of this database includes sex, birth date, diagnoses, examinations, prescriptions, treatments, and medical expenditures related to outpatient visits, emergency care, and hospitalization. The reliability of this database has been well accepted by important scientific journals worldwide [22, 23]. This study was approved by the institutional review board of Taipei Medical University (TMU-JIRB-202203134; TMU-JIRB-202006057).
Study design
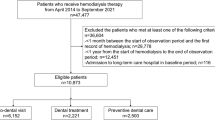
We examined medical claims and identified 378,006 first-ever stroke patients aged ≥ 20 years who underwent inpatient care by a neurologist (defined as patients with a physician’s primary diagnosis of stroke as well as hospitalization for > 1 day) in 2010–2017. After excluding ineligible study subjects (those that received irregular DS), we identified 62,174 stroke patients who had received regular DS (defined as receiving four DS within the previous 24 months before stroke admission) and 178,603 stroke patients who had no DS (defined as receiving no DS within the previous 24 months before stroke admission). Each patient who underwent inpatient care for stroke and received DS was randomly matched to a patient without DS who underwent inpatient care for stroke using a propensity score matched-pair procedure to adjust for sociodemographics, characteristics of stroke hospitalization, and coexisting medical conditions. After propensity score matching (case-control ratio, 1:1), 49,547 patients with and 49,547 without prestroke regular DS were included.
Measures and definitions
According to the recommendation of Taiwan’s Ministry of Health and Welfare, people are encouraged to receive DS every six months, and the National Health Insurance Administration also provides corresponding medical payment for DS. Therefore, the people in Taiwan receive free DS every six months. In this study, we defined DS as people who received 4 times of DS services within 24 months before stroke admission. Irregular DS was defined as people who had 1, 2, or 3 visits of DS within 24 months before stroke admission. Low-income status is defined as having a low income within 2 years before the first-ever stroke admission. According to the regulations from the Agency of National Health Insurance in Taiwan, people with a low-income status were qualified to have the registration fee and medical copayment waived when receiving outpatient, emergency, and inpatient medical care.
The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) was used to define the physicians’ diagnoses. Based on our previous studies [22, 23], preoperative medical conditions determined from the medical claims for the 24-month preoperative period included hypertension (ICD-9-CM 401–405), diabetes (ICD-9-CM 250), mental disorders (ICD-9-CM 290–319), ischemic heart disease (ICD-9-CM 410–414), chronic obstructive pulmonary disease (ICD-9- CM 491,492, 496), hyperlipidemia (ICD-9-CM 272.0, 272.1, 272.2, 272.4), heart failure (ICD-9-CM 428), Parkinson’s disease (ICD-9-CM 332), and liver cirrhosis (ICD-9-CM 571.2, 571.5,571.6). Renal dialysis was defined by administration codes (D8 and D9). Postoperative pneumonia (ICD-9-CM 480–486), septicemia (ICD-9-CM 038 and 998.5), urinary tract infection (ICD-9-CM 599.0), and in-hospital mortality during the index stroke admission were considered the study’s primary outcomes. Admission to the intensive care unit, hospital stay length, and medical expenditures during the index stroke admission were also compared between patients with and without prestroke regular DS.
Statistical analysis
We used propensity score-matched pair analysis to determine the associations between regular DS and poststroke outcomes. A nonparsimonious multivariable logistic regression model was used to estimate a propensity score for stroke patients who did or did not receive regular DS. Clinical significance guided the initial choice of covariates in this model and included age, sex, low income, types of stroke, hypertension, diabetes, mental disorders, ischemic heart disease, chronic obstructive pulmonary disease, hyperlipidemia, heart failure, Parkinson’s disease, liver cirrhosis, and renal dialysis. We matched stroke patients with regular DS to non-DS patients using a greedy matching algorithm (without replacement) with a caliper width of 0.2 SD of the log odds of the estimated propensity score. Categorical variables were summarized using frequency (percentage) and were compared between DS and non-DS stroke patients using chi-square tests. Continuous variables were summarized using the mean ± standard deviation and were compared using t tests. Logistic regressions were used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) of poststroke outcomes associated with regular DS. Additional sensitivity analyses stratified by age, sex, number of medical conditions and types of stroke were also performed to examine poststroke adverse events in patients with and without DS within these strata.
Results
The baseline characteristics of 62,174 stroke patients with regular DS and 178,603 stroke patients without DS are shown in Table 1. After matching by propensity-score, no significant differences in age, sex, low-income status, types of stroke, hypertension, diabetes, mental disorders, ischemic heart disease, chronic obstructive pulmonary disease, hyperlipidemia, heart failure, Parkinson’s disease, liver cirrhosis, and renal dialysis were identified between stroke patients with and without regular DS (Table 2).
Compared with non-DS controls (Table 3), stroke patients who received regular DS previously had lower risks of poststroke pneumonia (OR 0.58, 95% CI 0.54–0.63), septicemia (OR 0.58, 95% CI 0.54–0.63), urinary tract infection (OR 0.68, 95% CI 0.66–0.71), intensive care (OR 0.81, 95% CI 0.78–0.84), and in-hospital mortality (OR 0.66, 95% CI 0.62–0.71). Hospital stay length (9.3 ± 8.8 vs. 10.2 ± 9.3 days, P < 0.0001) and medical expenditure (2113 ± 3209 vs. 2233 ± 3198 US dollars, P < 0.0001) during the index stroke admission were also lower in patients who received regular DS compared to non-DS controls. The adverse outcome in stroke patients with and without dental scaling (before matching) was showed in Table S1. In Table 4, the stratification analysis showed that receiving regular DS was associated with reduced poststroke adverse events (including pneumonia, septicemia, urinary tract infection, and mortality) among men (OR 0.57, 95% CI 0.55–0.60), women (OR 0.65, 95% CI 0.62–0.68), patients aged 20–49 years (OR 0.49, 95% CI 0.44–0.55), patients aged 50–59 years (OR 0.56, 95% CI 0.52–0.61), patients aged 60–69 years (OR 0.61, 95% CI 0.57–0.65), patients aged 70–79 years (OR 0.62, 95% CI 0.59–0.66), and patients aged ≥ 80 years (OR 0.68, 95% CI 0.63–0.73). Subgroup analysis showed that regular DS lowered the risk of poststroke adverse events in patients with subarachnoid hemorrhage (OR 0.71, 95% CI 0.61–0.81), intracerebral hemorrhage (OR 0.65, 95% CI 0.61–0.70), other and unspecified intracerebral hemorrhage (OR 0.56, 95% CI 0.46–0.68), occlusion of precerebral arteries (OR 0.49, 95% CI 0.40–0.59), occlusion of cerebral arteries (OR 0.58, 95% CI 0.56–0.61), transient cerebral ischemia (OR 0.69, 95% CI 0.62–0.78), acute but ill-defined cerebrovascular disease (OR 0.33, 95% CI 0.22–0.49), and other ill-defined cerebrovascular disease (OR 0.56, 95% CI 0.42–0.75). Table S2 showed the stratified analysis for stroke patients with dental scaling associated with adverse events by medical conditions.
Table S3 showed the adverse outcomes after stroke in patients with and without irregular DS (having 1, 2, or 3 visits of DS). Irregular DS was associated with reduced risks of post-stroke pneumonia (OR 0.75, 95% CI 0.71–0.78), septicemia (OR 0.71, 95% CI 0.66–0.77), urinary tract infection (OR 0.85, 95% CI 0.81–0.89), and 30-day in-hospital mortality (OR 0.88, 95% CI 0.84–0.93).
Discussion
In this retrospective cohort study matched by propensity score, we found that stroke patients with regular DS had lower risks of poststroke pneumonia, septicemia, urinary tract infection, intensive care, and in-hospital mortality compared with those that did not receive DS. The medical expenditure and length of hospital stay were also lower in the stroke patients with DS compared to the control group. The association between DS and reduced poststroke adverse events was significant in both genders, every age group, and all stroke subtypes.
Factors associated with stroke and poststroke outcomes that were identified in previous studies include sex, age, hypertension, diabetes, mental disorders, ischemic heart disease, chronic obstructive pulmonary disease, hyperlipidemia, atrial fibrillation, heart failure, liver cirrhosis, dialysis, and Parkinson’s disease [6,7,8]. To avoid bias when investigating the relationships between DS and poststroke outcomes, we used propensity-score matching to adjust these potential confounding factors. We also considered socioeconomic status, number of hospitalizations and emergency visits as potential confounding factors in the multivariable regression models.
One case-control study reported that periodontal inflammation was associated with poor functional prognosis in patients diagnosed with minor stroke [24]. In another cohort study, systematic oral hygiene care was associated with decreased odds of hospital-acquired pneumonia in patients with acute-subacute stroke [25]; however, these studies had a relatively small sample size, limited types of stroke (ischemic or hemorrhagic) and lacked important prognostic implications (e.g., mortality). Our study correlated with the aforementioned reports in that maintenance of oral hygiene by DS is beneficial in post-stroke patients. Furthermore, our results demonstrated that DS has more beneficial effects on health outcomes in patients with stroke, which is rarely present in the literature.
Poor dentition increases the risk of bacteremia and the levels of serum IL-1 and IL-6 [11, 12, 26, 27]. Prior evidence has shown that oral bacterial pathogens may be identified in atherothrombotic tissues [13, 27]. Poor oral hygiene is also associated with a continuous infection and systemic inflammation, which could represent the underlying mechanism that links oral health and stroke. Routine dental examinations help patients identify dental problems and resolve them early. The Taiwan’s National Health Insurance program enrolled nearly all residents and provided dental checkups and scaling to all beneficiaries once per six months [28]. Previous studies found that these inflammatory biomarkers significantly decreased after the improvement of oral hygiene [11, 29]. Infectious complications commonly occurred after stroke and affect approximately 15-30% of stroke patients [30]. Poststroke infections directly contribute to high mortality in stroke patients [31,32,33,34]. We suggest that regular DS is beneficial in reducing inflammation, infectious complications and subsequent mortality after stroke [9, 13, 24, 25].
The beneficial effects of DS on poststroke outcomes could be partly explained by the following reasons. Firstly, the brain central nervous system and the immune system are closely linked via the hypothalamic-pituitary-adrenal axis and the sympathetic nervous system [30]. The mechanism of poststroke immunosuppression and immune exhaustion may increase the risk of infection [30,31,32,33, 35, 36]. The oral cavity serves as an endogenous reservoir for gut microbial strains [37], which intensifies the complex pathways to poststroke infection [32]. Receiving DS is helpful in reducing systemic inflammation [9, 13], gut dysbiosis, dissemination and subsequent infections in an immunosuppressive state [25, 38]. Secondly, people with tooth loss have increased risk of stroke mortality [39]. Tooth loss is also associated with pneumonia mortality [40]. Because regular DS is effective in maintaining functional oral intake and preventing tooth loss [28], we hypothesize that regular DS is beneficial in poststroke infections and mortality. Thirdly, some evidence indicates that poor oral hygiene may increase the risk of poststroke pneumonia [41]. In addition, patients who received regular DS are more likely to have better health awareness, socioeconomic status, family support and ambulatory independence [42,43,44,45], which are considered potential determinants of poststroke outcomes [46].
Billions of bacteria live inside our mouths at any given time, and many of these bacteria build up as plaque that causes tooth decay (cavities) and gingivitis, which can lead to periodontal disease. For a healthy oral cavity, the prevention of stroke, and improvement of poststroke outcomes, we recommend that people practice good oral hygiene. Teeth brushing, using antimicrobial mouthwash, and dental flossing every day, in addition to receiving dental scaling at least once per six months helps to reduce inflammation, atherosclerosis, stroke, and poststroke complications and mortality.
Our study has some limitations. Firstly, information regarding the participants’ detailed socioeconomics, lifestyle (such as smoking, alcohol consumption, physical activity), and biochemical laboratory measures were unavailable in the research data of Taiwan’s National Health Insurance. Future work can aim to include information on smoking habits, which affects both periodontal health and pulmonary conditions (pneumonia, etc.). Secondly, we could not consider the severity of stroke in this study because clinical data of brain infarct size, location, and the risk scores (such as National Institutes of Health Stroke Scale, modified Rankin scale or Barthel index) were not available in the current insurance database. Thirdly, we could not evaluate the protective effects of DS against specific oral pathogens because we had no information regarding the detailed dental data. Fourthly, we are unable to determine how well patients were able to maintain good daily oral hygiene habits, such as brushing twice a day with fluoridated toothpaste for 2 min, using floss, interproximal brushes, etc. In addition, no information was available regarding the self-paid (insurance-uncovered) dental medical services. Finally, residual confounding bias may exist in our study, although we attempted to control for potential confounders to the best of our ability.
In conclusion, the current study demonstrated that DS is associated with a reduced risk of poststroke complications and mortality. Our study suggests that the maintenance of oral hygiene by receiving regular DS (at least two times per year) may be an efficient way to manage cerebrovascular health. Further prospective studies are encouraged to confirm a causal relationship and potential biological mechanisms underlying the protective effects of DS for stroke patients.
Data Availability
The datasets used and/or analyzed during the current study available from the Ministry of Health and Welfare. Interested researchers can obtain the data through formal application to the Health and Welfare Data Science Center, Department of Statistics, Ministry of Health and Welfare, Taiwan (http://dep.mohw.gov.tw/DOS/np-2497-113.html) and contact the agency with email (stpeicih@mohw.gov.tw).
Abbreviations
- CI:
-
Confidence interval
- ICD-9-CM:
-
International Classification of Diseases, 9th Revision, Clinical Modification
- OR:
-
Odds ratio
References
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. Heart disease and stroke statistics-2020 update: a report from the american heart association. Circulation. 2020;141(9):e139–596.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88.
Feigin VL, Nguyen G, Cercy K, Johnson CO, Alam T, Parmar PG, Abajobir AA, Abate KH, Abd-Allah F, Abejie AN, et al. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018;379(25):2429–37.
Herzberg MC, Nobbs A, Tao L, Kilic A, Beckman E, Khammanivong A, Zhang Y. Oral streptococci and cardiovascular disease: searching for the platelet aggregation-associated protein gene and mechanisms of streptococcus sanguis-induced thrombosis. J Periodontol. 2005;76(11 Suppl):2101–5.
Vercellotti GM. Overview of infections and cardiovascular diseases. J Allergy Clin Immunol. 2001;108(4 Suppl):117–20.
Bang OY, Ovbiagele B, Kim JS. Nontraditional risk factors for ischemic stroke: an update. Stroke. 2015;46(12):3571–8.
Boehme AK, Esenwa C, Elkind MS. Stroke risk factors, genetics, and prevention. Circ Res. 2017;120(3):472–95.
O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, Rao-Melacini P, Zhang X, Pais P, Agapay S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (interstroke): a case-control study. Lancet. 2016;388(10046):761–75.
Lin HW, Chen CM, Yeh YC, Chen YY, Guo RY, Lin YP, Li YC. Dental treatment procedures for periodontal disease and the subsequent risk of ischaemic stroke: a retrospective population-based cohort study. J Clin Periodontol. 2019;46(6):642–9.
de Oliveira C, Watt R, Hamer M. Toothbrushing, inflammation, and risk of cardiovascular disease: results from scottish health survey. BMJ. 2010;340:c2451.
Chen ZY, Chiang CH, Huang CC, Chung CM, Chan WL, Huang PH, Lin SJ, Chen JW, Leu HB. The association of tooth scaling and decreased cardiovascular disease: a nationwide population-based study. Am J Med. 2012;125(6):568–75.
Moutsopoulos NM, Madianos PN. Low-grade inflammation in chronic infectious diseases: paradigm of periodontal infections. Ann N Y Acad Sci. 2006;1088:251–64.
Lee YL, Hu HY, Huang N, Hwang DK, Chou P, Chu D. Dental prophylaxis and periodontal treatment are protective factors to ischemic stroke. Stroke. 2013;44(4):1026–30.
Lafon A, Pereira B, Dufour T, Rigouby V, Giroud M, Béjot Y, Tubert-Jeannin S. Periodontal disease and stroke: a meta-analysis of cohort studies. Eur J Neurol. 2014;21(9):1155–61.
Leira Y, Seoane J, Blanco M, Rodríguez-Yáñez M, Takkouche B, Blanco J, Castillo J. Association between periodontitis and ischemic stroke: a systematic review and meta-analysis. Eur J Epidemiol. 2017;32(1):43–53.
Park JH, Kim JW, Lee H, Hong I, Song TJ. Better oral hygiene is associated with a decreased risk of meniere’s disease: a nationwide cohort study. J Pers Med. 2022;13(1):80.
Chang Y, Chung MK, Park JH, Song TJ. Association of oral health with risk of rheumatoid arthritis: a nationwide cohort study. J Pers Med. 2023 Feb;15(2):340.
Chang Y, Woo HG, Lee JS, Song TJ. Better oral hygiene is associated with lower risk of stroke. J Periodontol. 2021 Jan;92(1):87–94.
Park SY, Kim SH, Kang SH, Yoon CH, Lee HJ, Yun PY, Youn TJ, Chae IH. Improved oral hygiene care attenuates the cardiovascular risk of oral health disease: a population-based study from Korea. Eur Heart J. 2019;40(14):1138–45.
Yeh YT, Wang BY, Lin CW, Yang SF, Ho SW, Yeh HW, Huang JY, Chang YC, Yeh CB. Periodontitis and dental scaling associated with pyogenic liver abscess: a population-based case-control study. J Periodontal Res. 2018;53(5):785–92.
Chung YH, Kuo HC, Liu HY, Wu MY, Chang WJ, Chen JT, Cherng YG, Chen TJ, Dai YX, Wu HL, Liu WC, Tai YH. Association between dental scaling and reduced risk of end-stage renal disease: a nationwide matched cohort study. Int J Environ Res Public Health. 2021;18(17):8910.
Liao CC, Chou YC, Yeh CC, Hu CJ, Chiu WT, Chen TL. Stroke risk and outcomes in patients with traumatic brain injury: 2 nationwide studies. Mayo Clin Proc. 2014;89(2):163 – 72.
Huang SY, Lo PH, Liu WM, Cherng YG, Yeh CC, Chen TL, Liao CC. Outcomes after nonobstetric surgery in pregnant patients: a nationwide study. Mayo Clin Proc. 2016;91(9):1166-72.
Leira Y, Rodríguez-Yáñez M, Arias S, López-Dequidt I, Campos F, Sobrino T, D’Aiuto F, Castillo J, Blanco J. Periodontitis as a risk indicator and predictor of poor outcome for lacunar infarct. J Clin Periodontol. 2019;46(1):20–30.
Wagner C, Marchina S, Deveau JA, Frayne C, Sulmonte K, Kumar S. Risk of stroke-associated pneumonia and oral hygiene. Cerebrovasc Dis. 2016;41(1–2):35–9.
Maharaj B, Coovadia Y, Vayej AC. An investigation of the frequency of bacteraemia following dental extraction, tooth brushing and chewing. Cardiovasc J Afr. 2012;23(6):340–4.
Sanz M, Marco Del Castillo A, Jepsen S, Gonzalez-Juanatey JR, D’Aiuto F, Bouchard P, Chapple I, Dietrich T, Gotsman I, Graziani F, et al. Periodontitis and cardiovascular diseases: consensus report. J Clin Periodontol. 2020;47(3):268–88.
Tai TW, Lin TC, Ho CJ, Kao Yang YH, Yang CY. Frequent dental scaling is associated with a reduced risk of periprosthetic infection following total knee arthroplasty: a nationwide population-based nested case-control study. PLoS ONE. 2016;11(6):e0158096.
Paraskevas S, Huizinga JD, Loos BG. A systematic review and meta-analyses on c-reactive protein in relation to periodontitis. J Clin Periodontol. 2008;35(4):277–90.
Vermeij JD, Westendorp WF, van de Beek D, Nederkoorn PJ. Post-stroke infections and preventive antibiotics in stroke: update of clinical evidence. Int J Stroke. 2018;13(9):913–20.
Wastfelt M, Cao Y, Strom JO. Predictors of post-stroke fever and infections: a systematic review and meta-analysis. BMC Neurol. 2018;18(1):49.
Shim R, Wong CHY. Complex interplay of multiple biological systems that contribute to post-stroke infections. Brain Behav Immun. 2018;70:10–20.
Westendorp WF, Nederkoorn PJ, Vermeij J-D, Dijkgraaf MG, van de Beek D. Post-stroke infection: a systematic review and meta-analysis. BMC Neurol. 2011;11:110.
Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003;60(4):620–5.
Rashid MH, Kabir A, Waris MU, Salman U, Zain S. Role of prophylactic antibiotics in critical care of stroke patients - a preventive approach to post-stroke infections? Cureus. 2020;12(3):e7158.
Urra X, Laredo C, Zhao Y, Amaro S, Rudilosso S, Renú A, Prats-Galino A, Planas AM, Oleaga L, Chamorro Á. Neuroanatomical correlates of stroke-associated infection and stroke-induced immunodepression. Brain Behav Immun. 2017;60:142–50.
Schmidt TS, Hayward MR, Coelho LP, Li SS, Costea PI, Voigt AY, Wirbel J, Maistrenko OM, Alves RJ, Bergsten E, et al. Extensive transmission of microbes along the gastrointestinal tract. Elife. 2019;8:e42693.
Olsen I, Yamazaki K. Can oral bacteria affect the microbiome of the gut? J Oral Microbiol. 2019;11(1):1586422.
Abnet CC, Qiao YL, Dawsey SM, Dong ZW, Taylor PR, Mark SD. Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a chinese population-based cohort. Int J Epidemiol. 2005;34(2):467–74.
Suma S, Naito M, Wakai K, Naito T, Kojima M, Umemura O, Yokota M, Hanada N, Kawamura T. Tooth loss and pneumonia mortality: a cohort study of japanese dentists. PLoS ONE. 2018;13(4):e0195813.
Lyons M, Smith C, Boaden E, Brady MC, Brocklehurst P, Dickinson H, Hamdy S, Higham S, Langhorne P, Lightbody C, et al. Oral care after stroke: where are we now? Eur Stroke J. 2018;3(4):347–54.
Mittal R, Wong ML, Koh GC, Ong DLS, Lee YH, Tan MN, Allen PF. Factors affecting dental service utilisation among older Singaporeans eligible for subsidized dental care - a qualitative study. BMC Public Health. 2019;19(1):1075.
Chandra Shekar BR, Manjunath BC, Reddy CK, Suma S. Dental health awareness, attitude, oral health-related habits, and behaviors in relation to socio-economic factors among the municipal employees of mysore city. Ann Trop Med Public Health. 2011;4(2):99–106.
Thomas PA, Liu H, Umberson D. Family relationships and well-being. Innov Aging. 2017;1(3):igx025.
Tsouna-Hadjis E, Vemmos KN, Zakopoulos N, Stamatelopoulos S. First-stroke recovery process: the role of family social support. Arch Phys Med Rehabil. 2000;81(7):881–7.
Das S, Das SK. Knowledge, attitude and practice of stroke in India versus other developed and developing countries. Ann Indian Acad Neurol. 2013;16(4):488–93.
Acknowledgements
This study is based in part on data obtained from Taiwan’s Ministry of Health and Welfare. The authors’ interpretations and conclusions do not represent those of the Ministry of Health and Welfare, Taiwan.
Funding
This work was supported by Taiwan’s Ministry of Science and Technology (MOST111-2320-B-532-001-MY3; MOST110-2314-B‐038–108‐MY2; MOST108-2320-B-038-070-MY3).
Author information
Authors and Affiliations
Contributions
All authors contributed to collected the data of participants and clinical grading. LC Sung drafted the manuscript. CC Liao analyzed the data. LC Sung and CC Liao conceived the idea and corrected the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval, guidelines and consent to participate
This research was conducted in accordance with international guidelines and the ethical standards outlined in the Declaration of Helsinki. As these reimbursement claims were used in this study, the electronic database was decoded with patient identifications scrambled for further academic access for research to protect privacy. Although the Ministry of Health and Welfare exempt such uses from informed consent, because patient identifications are decoded and scrambled. This study was approved by the institutional review board of Taipei Medical University (TMU-JIRB-202203134; TMU-JIRB-202006057).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sung, LC., Chang, CC., Yeh, CC. et al. The effects of regular dental scaling on the complications and mortality after stroke: a retrospective cohort study based on a real-world database. BMC Oral Health 23, 487 (2023). https://doi.org/10.1186/s12903-023-03178-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03178-6