Abstract
This study aims to investigate the impact of dental care utilization status on the occurrence of fatal complications such as cerebral/cardiovascular disease (CVD) and infectious diseases in patients with end-stage renal disease (ESRD) undergoing hemodialysis. This retrospective cohort study was performed using the Japanese claims database and included patients who first underwent hemodialysis between April 2014 and September 2020. The exposure variable of interest was the pattern of dental utilization, which was categorized into three groups, “dental treatment group”, “preventive dental care group”, and “no-dental visit group”. The primary outcomes were the time interval until a composite end point of first major cardiovascular event (acute myocardial infarction, heart failure, or cerebral infarction) of infectious disease (pneumonia and sepsis). The secondary outcomes were the time interval until the incidence of each component of primary outcomes. Survival analyses, including log-rank tests and Cox proportional hazards regression analyses, were performed. Among the 10,873 patients who underwent the first dialysis treatment, 6152 were assigned to the no-dental visit group, 2221 to the dental treatment group, and 2500 to the preventive dental care group. The preventive dental care group had significantly lower hazard ratios (HRs) of the incidence of CVD (adjusted hazard ratio [aHR]: 0.86, 95% confidence interval [CI]: 0.77–0.96) and infectious diseases (aHR: 0.86, 95% CI: 0.76–0.97). As for pneumonia, preventive dental care and dental treatment groups had significantly lower HRs (aHR: 0.74 and 0.80, 95% CI: 0.61–0.88, 0.66–0.96) than the no-dental visit group. This study demonstrated that dental visits for preventive dental care were associated with a significant risk reduction in CVD and infectious complications in patients with ESRD undergoing hemodialysis.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a tremendous burden on global health, both as a direct cause of morbidity and mortality worldwide and as an important risk factor for the incidence of cerebral/cardiovascular disease (CVD) and infectious diseases1. Hemodialysis is a renal replacement therapy for patients with end-stage renal disease (ESRD). Patients undergoing hemodialysis have a significantly reduced quality of life (QoL), high medical costs, and a high crude mortality rate of > 20% per year2. CVD and infectious diseases are the major causes of death among patients undergoing hemodialysis, accounting for 50%3 and 14% of deaths, respectively4.
Oral health status influences mortality in patients undergoing hemodialysis. Several studies have demonstrated the effect of periodontitis on mortality in patients undergoing hemodialysis5,6,7,8. Furthermore, dental caries9, decayed-missing-filled teeth index10, and poor oral hygiene9,10 were associated with mortality in patients undergoing hemodialysis9. Previous reports have also revealed the dental-related diseases with major causes of death under hemodialysis maintenance; for example, between dental caries and aortic calcification11, as well as between oral candidiasis and infectious diseases12. Recent studies have emphasized the effectiveness of periodontal therapy in suppressing fatal events such as CVD3, infectious disease13, and mortality3 in patients undergoing hemodialysis. However, no studies have examined the impact of dental interventions other than periodontal therapy in patients undergoing hemodialysis. Therefore, we hypothesized that general dental care and treatments, such as dental caries treatment, prosthodontic treatment, tooth extraction, and periodontal therapy, and the preventive dental care may reduce the incidence of fatal complications such as CVD and infectious disease in patients undergoing hemodialysis.
This study aimed to investigate the impact of dental care utilization status on the occurrence of fatal complications such as CVD and infectious diseases in patients undergoing hemodialysis using the Japanese claims database.
Methods
Data source
This retrospective cohort study used data from the DeSC database, which contains claims data provided by DeSC Healthcare Inc., Tokyo, Japan (https://desc-hc.co.jp/company)14. This database includes individuals insured with the following three types: (1) society-managed, employment-based health insurance associations (provided for employees of Japanese companies and their families), (2) national health insurance (provided for individuals aged < 75 years who are not covered by other public health insurance), and (3) the latter-stage elderly healthcare system (provided for individuals aged 75 years or more). DeSC Healthcare Inc. possesses epidemiological claims data for three million insurance subscribers. This data are available for academic research with anonymized information on medical, dental, and drug prescription claims and health check-ups14. A previous study reported that the distribution of age and sex in the database was comparable to that of the population estimates. Furthermore, the same study reported that the prevalence of certain non-communicable diseases in the database was comparable to that in a previously reported national survey14. In this claims data, all medical diagnoses were made according to the International Classification of Diseases 10th Revision (ICD-10) codes and recorded in Japanese free texts.
Ethics statement
This study was approved and informed consent was waived by the Dental Research Ethics Committee of the Tokyo Medical and Dental University (approval number: D2022-017). This study was conducted according to the Helsinki Declaration of 1975, as revised in 2013.
Sampled patients
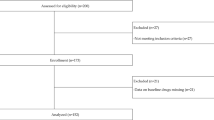
A flowchart of the patient selection for this study is presented in Fig. 1. We identified patients who underwent hemodialysis between April 2014 and September 2020. Among them, we extracted patients who had at least 1 month between the start of the observation period and the first hemodialysis record to identify newly introduced hemodialysis patients. Patients on maintenance hemodialysis generally undergo hemodialysis three times a week. Patients who survived for at least 1 year during the follow-up period were selected to identify hemodialysis patients in the chronic maintenance period. The baseline period was defined as 1 year after the first hemodialysis. Patients admitted to hospitals requiring long-term care during the baseline period were excluded. Individuals diagnosed with each outcome during the baseline period were also excluded.
Exposure
The exposure variable of interest in this study was the pattern of dental care utilization, which was categorized into three groups: “dental treatment group”, “preventive dental care group”, and “no-dental visit group”. In clinical practice, people who visit dentists only when they experience symptoms may discontinue their dental visit after treatment for chief complaints, even if further treatment is recommended. In contrast, some patients regularly visit dentists and continue to take preventive dental care, oral hygiene instructions, prophylaxis, and prosthesis maintenance after the symptomatic therapy. Among these people accessing dental clinics, people exist with different attributes: treatment and preventive dental care groups.
We defined patients who did not have a dental visit during the baseline period as the “no-dental visit group.” Patients who had received dental treatments, such as cavity fillings, pulpectomies, periodontal surgeries, tooth extractions, and placement of prostheses, were assigned to the “dental treatment group.” Patients who had a dental visit during the baseline period but did not receive the treatment mentioned above were assigned to the “preventive dental care group” (see Supplementary Table 1 for more details). Regarding the additional analyses conducted to examine the effect of different dental procedures, the dental treatment group was further divided into the “minor dental treatment group,” which included the patients who had undergone cavity filling and placement of prostheses, and “major dental treatment group,” which included patients who had undergone pulpectomies, periodontal surgeries, and tooth extractions.
Outcome measurement
The primary outcome of this study was the time interval until the incidence of CVD and infectious diseases. CVD included diagnoses of acute myocardial infarction (ICD-10 code: I21), heart failure (ICD-10 code: I50), and cerebral infarction (ICD-10 code: I63) during the observation period. Infectious diseases included sepsis (ICD-10 code: A40 and 41), and pneumonia (ICD-10 code: J15 and 69). The secondary outcome was the time interval until the incidence of acute myocardial infarction, heart failure, cerebral infarction, sepsis, or pneumonia. For survival time analysis, survival time was defined as the time from the start of observation to the earliest of (1) event occurrence, (2) death, (3) censoring, and (4) the end of the observation period. Regarding the sensitivity analyses, survival time analyses for the outcome were performed, with an event defined a disease recorded more than twice during the observation period. Survival time was defined as the period from the start of observation to the time when a disease is recorded for the first time in the observation period.
Covariates
Health and socio-demographic variables were used as covariates. Diagnoses of the following comorbidities based on the Charlson comorbidity index between baseline periods were identified: diabetes, hypertension, dementia, chronic pulmonary disease, rheumatic disease, liver disease, hemiplegia, paraplegia, malignancy, metastatic solid tumor, and human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) (see Supplementary Table 2 for more details). For the history of hospitalization in the baseline period, the patient was hospitalized for any reason during the baseline period was extracted. As a proxy for socioeconomic status, the type of health insurance was categorized as (1) society-managed employment-based health insurance associations, (2) national health insurance, and (3) the latter-stage elderly healthcare system. Age and sex were also considered.
Statistical analysis
Survival time analyses were conducted to examine the effects of dental utilization patterns on the incidence of each outcome. The cumulative incidence of each outcome was illustrated using Kaplan–Meier curves and compared between groups using log-rank tests. Hazard ratios (HRs) and 95% confidence intervals (CIs) of the selected outcomes were estimated using Cox proportional hazard regression models. In the multivariable models, the following covariates were included: age, sex, diabetes, hypertension, congestive heart failure, dementia, chronic pulmonary disease, rheumatic disease, liver disease, hemiplegia, paraplegia, malignancy, metastatic solid tumor, HIV/AIDS, history of hospitalization in the baseline period, and type of health insurance. Schoenfeld residual plots were plotted to confirm that the proportional hazards assumption of the Cox proportional regression models was not violated for each outcome15 (Supplementary Fig. 1). All statistical analyses were performed using Stata software (version 17.0; StataCorp). All tests were two-tailed, and statistical significance was set at p < 0.05.
Results
We included 47,477 patients who underwent hemodialysis during the study period. Among them, 29,778, 12,451, and 116 participants were excluded due to the duration from the start of the observation period to the first record of hemodialysis of less than 1 month, the duration from the start of hemodialysis to the end of observation period of less than 1 year, and admission to a long-term care hospital during the baseline period, respectively. We identified 10,873 as eligible patients. Of the eligible patients, 6152 (56.6%) were assigned to the no-dental visit group, 2221 (20.4%) to the dental treatment group, and 2500 (23.0%) to the preventive dental care group (Fig. 1).
The baseline characteristics of the patients are shown in Table 1. The mean age was 74.0 years (standard deviation [SD]: 12.2), with the majority being older than 65 (80.6%). Males accounted for 7190 (66.1%) of the total. Among the patients in this study, many had multiple comorbidities, and more than half were hospitalized in the baseline period.
Figure 2a shows the survival curve for the incidence of CVDs stratified by dental care utilization patterns. We found differences in the occurrence of CVD according to dental care utilization patterns (Fig. 2a, p < 0.001 for log-rank test). Although there was no significant difference in the incidence of heart failure (Fig. 2d, p = 0.072 for log-rank test), the incidences of acute myocardial infarction and cerebral infarction differed according to dental care utilization patterns (Fig. 2c,e, p = 0.003 and 0.01 for log-rank test). Tables 2 and 3 show the results of the Cox proportional regression model used to estimate survival time for the incidence of CVD. The preventive dental care group had a lower HR of the incidence of CVD (adjusted hazard ratio [aHR]: 0.86, 95% CI: 0.76–0.97), whereas the dental treatment group had a higher HR of 1.11 (95% CI: 1.00–1.22) compared to the no-dental visit group. The preventive dental care group showed a lower risk for acute myocardial infarction with aHR of 0.79 (95% CI: 0.67–0.93) compared to the no-dental visit group, respectively.
Figure 2b shows the survival curve of the incidence of infectious diseases stratified by dental care utilization patterns. Although there was no significant difference in the incidence of sepsis (Fig. 2f, p = 0.23 for log-rank test), the incidence of pneumonia differed according to dental utilization patterns (Fig. 2g, p = 0.003 for log-rank test). In the preventive dental care group, the aHR for infectious diseases was lower at 0.86 (95% CI: 0.76–0.97) compared to the no-dental visit group (Table 2). The aHR for the incidence of pneumonia in the preventive dental care groups was 0.74 (95% CI: 0.62–0.88) (Table 3). Furthermore, for pneumonia, the dental treatment group showed a lower aHR of 0.80 (95% CI: 0.66–0.96).
The sensitivity analysis conducted by setting different definitions for the outcomes yielded results that were consistent with those of the main analysis (Supplementary Tables 1 and 2). Furthermore, additional analysis, which categorized exposure into four groups including no-dental visit, minor dental treatment, major dental treatment, or preventive dental care groups, yielded results that were consistent with those of the main analysis (Supplementary Tables 3 and 4).
Discussion
Summary
This study evaluated the effects of dental care utilization status in patients undergoing hemodialysis. Of the 10,873 patients undergoing hemodialysis extracted from a Japanese claims database, more than half had no-dental visits, 20.4% were in the dental treatment group and approximately 23.0% were in the preventive dental care group. The preventive dental care group had a lower incidence of CVD and infectious diseases. The HR of CVD was higher in the dental treatment group, whereas the HR of pneumonia was lower in the dental treatment group. These findings suggest that appropriate dental care utilization may be beneficial in reducing the risk of CVDs and infectious diseases, which are fatal complications in patients undergoing hemodialysis.
Comparison with previous studies
In the general population, periodontal disease is significantly associated with CVD16. A study using the national health insurance system database in South Korea has shown that severe periodontitis significantly increases the incidence of acute myocardial and cerebral infarctions17. However, no clear evidence of the preventive effects of periodontal therapy on the incidence of CVD events exist, although improvements in inflammatory markers and endothelial function have been reported18. Meanwhile, in patients undergoing hemodialysis with lower immune function and higher risk of developing CVD events compared with that observed in the general population, periodontal therapy may have a greater impact. In periodontal therapy for patients undergoing hemodialysis, several studies have elucidated the effect of controlling inflammation19,20,21 and preventing cardiovascular events22. Two studies using Taiwanese claims data reported that intensive periodontal therapy (scaling and root planing and flap procedure) lowered the risk of infection-related hospitalization13, hospitalization due to CVD, and all-cause mortality3 in patients undergoing hemodialysis.
However, multidisciplinary dental treatments may be provided in clinical practice because many patients who visit dentists suffer from various dental problems as well as periodontitis. Patients visiting dentists undergo two primary dental treatment modalities. Patients with dental problems should receive the active dental treatments for dental caries, endodontic treatment, tooth extraction, prosthodontic preparation, and intensive periodontal therapy. Patients without major dental problems may receive prophylaxis, including toothbrushing instructions, mechanical tooth polishing, scaling, root planing, and maintenance of the prosthodontic apparatus. This study focused on differences in patients’ dental care utilization patterns. No study has examined how multidisciplinary dental care, not only periodontal therapy, affects the prognosis of patients undergoing hemodialysis. In this study, patients who underwent nonsurgical periodontal therapy were assigned to the preventive dental care group because of its secondary preventive aspect. The results showed a significantly lower HR for the incidence of CVD and infectious diseases in the preventive dental care group were consistent with those of previous studies.
Possible explanations
Some possible mechanisms by which professional dental care affects CVD and infectious diseases in patients undergoing hemodialysis can be assumed, although detailed information on the participants, such as blood and bacteriological test results, were not available in this study. In general, the mechanisms by which oral health affects systemic health include the impact of local inflammation in the oral cavity due to dental diseases, systemic repercussions of the local inflammation through circulation, and influence of dental plaque containing abundant oral bacteria. In addition to these, specific mechanisms pertinent to patients undergoing dialysis may include the mediating effect of malnutrition–inflammation–atherosclerosis (MIA) syndrome.
Patients with periodontitis have systemic inflammation with raised levels of high-sensitivity C-reactive protein (CRP)23,24,25, and periodontal treatments reduce this inflammatory reaction19,20,21. A high CRP level is a decisive risk factor for CVD events26, and previous cohort studies have reported that the presence of periodontitis increases mortality from CVD in patients undergoing hemodialysis6,7. Therefore, well-achieved periodontal therapy has the potential to contribute to reducing the incidence of CVD. Regarding heart failure and cerebral infarction, a tendency toward reduced incidence risk was observed with preventive dental care, although no significant effects were found. CVDs are influenced by various factors including oral health, as well as lifestyle habits and environmental factors. Hence, this study’s sample size was likely insufficient to detect an impact of oral health.
In patients undergoing hemodialysis, the risks of infections including nosocomial infections are heightened. These risks are not only because these patients are immunocompromised but also because their rate of exposure to infection risks, such as hospitalizations, frequent outpatient visits27, and the placement of vascular access devices28, is high. Reducing the total number of bacteria in the oral cavity can help prevent infectious diseases. Poor oral health may increase the number of bacteria transferred into the bloodstream through daily oral activities such as tooth brushing and chewing29. These bacteria can trigger bacteremia and, eventually, sepsis in patients undergoing hemodialysis. However, in this study, dental care did not significantly reduce the risk of sepsis. Further larger-scale studies might detect the statistically significant effect of oral care on sepsis. Reducing the number of oral bacteria can prevent aspiration pneumonia30,31,32. Considering that patients undergoing hemodialysis are an immunocompromised population, preventive dental care may lower the incidence of pneumonia. Interestingly, a significantly lower incidence of pneumonia was observed not only in the preventive dental care group but also in the dental treatment group. Because we could not conduct stratified analyses for each type of dental treatment due to limited sample size, which specific dental treatments are associated with this lower incidence remains unclear. However, a reduction in oral bacterial load following caries treatment or extractions, professional denture cleaning33,34, or improved nutritional status through enhanced chewing efficiency following prosthodontic treatment35 could have enhanced immune responses. The additional analysis in this study suggests that major dental treatments involving pulpectomies, periodontal surgeries, or tooth extractions can be effective in reducing the risk of pneumonia.
Poor oral health may affect the incidence of CVD and infectious diseases through the MIA syndrome36,37. Some patients undergoing hemodialysis experience MIA syndrome, which is a combination of chronic systemic inflammation, malnutrition, and arteriosclerosis38. Oral problems, such as pain, ill-fitting dentures, and missing teeth with no prosthodontic treatment, may enhance malnutrition in patients undergoing hemodialysis patients39,40,41. Periodontitis increases systemic inflammation23,24,25. Malnutrition and inflammation proceed in a mutually conducive vicious cycle, leading to the risk of atherosclerosis and infections due to a depressed immune system in patients undergoing hemodialysis42.
Differences in the effects of dental treatments on the incidence of CVD and infectious diseases have been reported. The dental treatment visit group included people who visited for dental problems rather than for maintenance. The effect of poor oral health on the cardiovascular system before the baseline period may have been reflected in the significantly higher HR for CVD in the dental treatment group. The dental treatment group may represent a subpopulation with different health-related behaviors compared to the other groups, and this divergence in health-related behavior could potentially contribute to the observed results. In contrast, for pneumonia, when the number of oral bacteria is reduced by dental treatment, the effect may have been immediately apparent in the reduction in the risk of aspiration pneumonia.
Implications
In this study, a significant association was observed between preventive dental care and the incidence of CVD and infectious diseases. These findings suggest that preventive dental care, including prophylactic programs and maintenance of the prosthodontic apparatus, may be beneficial in patients undergoing hemodialysis. Oral care can reduce the risk of aspiration pneumonia in the older residents of nursing homes32, and that of cardiovascular diseases in the Scottish general population with a mean age of 50.0 years43. Patients undergoing hemodialysis are more susceptible to cardiovascular disease and infectious diseases, and have poor oral health. Therefore, the impact of dental utilization in our study population may have been more pronounced than in the general population. Effective prevention of CVD includes control of comorbidities, such as hypertension and conditions that cause inflammation, while prevention of infectious diseases includes primary infection control and vaccination. In addition, dental care may serve as a preventive measure. Patients undergoing hemodialysis have poor oral health44,45,46 because of salivary gland atrophy and drinking restrictions45. However, they were unlikely to visit dental clinics because of anxiety about dental treatment and financial concerns47,48. This study suggests that dental care provided by dental health professionals is beneficial for preventing fatal complications. Healthcare professionals should establish a system in which patients undergoing hemodialysis can receive preventive dental care without concern.
Dental visits, either dental treatment or preventive dental care, are associated with a lower risk of pneumonia, possibly owing to a reduction in oral bacteria. However, the finding that dental treatment is associated with a higher OR of the incidence of CVD needs to be examined in more detail in the future, including the type of treatment and the duration of time to CVD events.
Strength and limitations
To the best of our knowledge, this is the first study to demonstrate that regular dental visits may be beneficial in the primary prevention of CVDs and infectious diseases in patients with ESRD undergoing hemodialysis. Another strength of this study is that our longitudinal claims data included a large sample size without selection bias. Utilizing real-world data, we generated real-life clinical evidence for patients with ESRD undergoing hemodialysis.
However, this study also had several limitations. First, several potentially confounding factors, such as body mass index, smoking status, severity of periodontitis, unadjusted comorbidities that may affect physical activity, and socioeconomic status, were unavailable in the database. Regarding socioeconomic status, we adjusted for the type of health insurance as a proxy for income and educational background due to its correlation with income49. The data regarding income nor educational background were not available in the database used in this study. Second, our findings require careful interpretation for application to populations of different races or other dialysis modalities, such as peritoneal dialysis. Third, individuals without an observation period of 1 year after the initiation of hemodialysis were excluded in this study, potentially introducing survivor bias. This means artificially selecting a population with better health status, which may have led to an underestimation of the actual hazard ratios. Additionally, the no-dental visit group may include individuals who refrained from dental visits despite their poor oral health and those who refrained due to their good oral health. While this might be a potential bias, it may introduce variability in the results rather than skew them in a particular direction, thus ensuring the robustness of the study findings. Fourth, individuals were categorized into three groups based on their dental visit history during the baseline period, and each group was considered to exhibit a different dental utilization behavior. However, dental utilization behavior may change during the lifetime, and the potential effects of such changes require further investigation in future research. Furthermore, we did not account for dental visit behaviors prior to the baseline period. While the preventive dental care group may include individuals who received preventive dental care after undergoing significant dental procedures such as tooth extraction before the baseline period, we believe they are equivalent to those who continued preventive dental care without significant dental procedures prior to the baseline period, provided their oral health had improved by the start of the baseline period. Thus, to enhance the interpretability of the study findings, allocations were based solely on dental visit behaviors during the baseline period. Finally, the disease and procedure codes in the claims data were consistent. Previous studies that examined the validity of Japanese claims data demonstrated their usefulness in research using administrative data50,51,52. In Japan, no procedure code links directly to disease codes, leading to both dental treatments and preventive dental care being provided under the same disease codes. Therefore, exposure was defined based on dental procedure codes according to a previous study53.
Conclusion
This study demonstrated that dental visits for preventive dental care were associated with a significant risk reduction of CVD and infectious complications in patients with ESRD undergoing hemodialysis. Healthcare professionals should be aware of oral health issues and promote the patients' dental visits.
Data availability
The data that support the findings of this study are available from DeSC Healthcare Inc. but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of DeSC Healthcare Inc.
References
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 395, 709–733. https://doi.org/10.1016/s0140-6736(20)30045-3 (2020).
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E. & Hsu, C. Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 351, 1296–1305. https://doi.org/10.1056/NEJMoa041031 (2004).
Huang, S. T. et al. Intensive periodontal treatment reduces risks of hospitalization for cardiovascular disease and all-cause mortality in the hemodialysis population. J. Clin. Med. https://doi.org/10.3390/jcm7100344 (2018).
National Institute of Diabetes and Digestive and Kidney disease. 8. Mortality, and cause of death, H.12_HD. https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/usrds/prior-data-reports/2019
Iwasaki, M. et al. Periodontal disease and pneumonia mortality in haemodialysis patients: A 7-year cohort study. J. Clin. Periodontol. 45, 38–45. https://doi.org/10.1111/jcpe.12828 (2018).
Ruospo, M. et al. Periodontitis and early mortality among adults treated with hemodialysis: A multinational propensity-matched cohort study. BMC Nephrol. 18, 166. https://doi.org/10.1186/s12882-017-0574-x (2017).
Kshirsagar, A. V. et al. Periodontal disease adversely affects the survival of patients with end-stage renal disease. Kidney Int. 75, 746–751. https://doi.org/10.1038/ki.2008.660 (2009).
Chen, L. P. et al. Relationship between periodontal disease and mortality in patients treated with maintenance hemodialysis. Am. J. Kidney Dis. 57, 276–282. https://doi.org/10.1053/j.ajkd.2010.09.016 (2011).
Mizutani, K. et al. Poor oral hygiene and dental caries predict high mortality rate in hemodialysis: A 3-year cohort study. Sci. Rep. 10, 21872. https://doi.org/10.1038/s41598-020-78724-1 (2020).
Palmer, S. C. et al. Dental health and mortality in people with end-stage kidney disease treated with hemodialysis: A multinational cohort study. Am. J. Kidney Dis. 66, 666–676. https://doi.org/10.1053/j.ajkd.2015.04.051 (2015).
Misaki, T., Fukunaga, A. & Nakano, K. Dental caries status is associated with arteriosclerosis in patients on hemodialysis. Clin. Exp. Nephrol. 25, 87–93. https://doi.org/10.1007/s10157-020-01966-w (2021).
Yeter, H. H. et al. Oral Candida colonization as a risk factor for chronic inflammation and atherosclerosis in hemodialysis patients. Ther. Apher. Dial. 23, 542–549. https://doi.org/10.1111/1744-9987.12803 (2019).
Huang, S. T., Lin, C. L., Yu, T. M., Wu, M. J. & Kao, C. H. Intensive periodontal treatment reduces risk of infection-related hospitalization in hemodialysis population: A nationwide population-based cohort study. Medicine (Baltimore) 94, e1436. https://doi.org/10.1097/md.0000000000001436 (2015).
Okada, A. & Yasunaga, H. Prevalence of noncommunicable diseases in Japan using a newly developed administrative claims database covering young, middle-aged, and elderly people. JMA J. 5, 190–198. https://doi.org/10.31662/jmaj.2021-0189 (2022).
Gregson, J. et al. Nonproportional hazards for time-to-event outcomes in clinical trials: JACC review topic of the week. J. Am. Coll. Cardiol. 74, 2102–2112. https://doi.org/10.1016/j.jacc.2019.08.1034 (2019).
Sanz, M. et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 47, 268–288. https://doi.org/10.1111/jcpe.13189 (2020).
Cho, H. J. et al. Severe periodontal disease increases acute myocardial infarction and stroke: A 10-year retrospective follow-up study. J. Dent. Res. 100, 706–713. https://doi.org/10.1177/0022034520986097 (2021).
Ye, Z. et al. Periodontal therapy for primary or secondary prevention of cardiovascular disease in people with periodontitis. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD009197.pub5 (2022).
Tasdemir, Z. et al. The effect of periodontal disease treatment in patients with continuous ambulatory peritoneal dialysis. Int. Urol. Nephrol. 50, 1519–1528. https://doi.org/10.1007/s11255-018-1913-y (2018).
Yazdi, F. K., Karimi, N., Rasouli, M. & Roozbeh, J. Effect of nonsurgical periodontal treatment on C-reactive protein levels in maintenance hemodialysis patients. Ren. Fail. 35, 711–717. https://doi.org/10.3109/0886022x.2013.777890 (2013).
Yue, H. et al. Effects of non-surgical periodontal therapy on systemic inflammation and metabolic markers in patients undergoing haemodialysis and/or peritoneal dialysis: A systematic review and meta-analysis. BMC Oral Health 20, 18. https://doi.org/10.1186/s12903-020-1004-1 (2020).
Santos-Paul, M. A. et al. Cardiovascular risk reduction with periodontal treatment in patients on the waiting list for renal transplantation. Clin. Transplant. 33, e13658. https://doi.org/10.1111/ctr.13658 (2019).
Schöffer, C., Oliveira, L. M., Santi, S. S., Antoniazzi, R. P. & Zanatta, F. B. C-reactive protein levels are associated with periodontitis and periodontal inflamed surface area in adults with end-stage renal disease. J. Periodontol. 92, 793–802. https://doi.org/10.1002/jper.20-0200 (2021).
Nadeem, M., Stephen, L., Schubert, C. & Davids, M. R. Association between periodontitis and systemic inflammation in patients with end-stage renal disease. SADJ 64, 470–473 (2009).
Paraskevas, S., Huizinga, J. D. & Loos, B. G. A systematic review and meta-analyses on C-reactive protein in relation to periodontitis. J. Clin. Periodontol. 35, 277–290. https://doi.org/10.1111/j.1600-051X.2007.01173.x (2008).
Kaptoge, S. et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: An individual participant meta-analysis. Lancet 375, 132–140. https://doi.org/10.1016/s0140-6736(09)61717-7 (2010).
Dalrymple, L. S. & Go, A. S. Epidemiology of acute infections among patients with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 3, 1487–1493. https://doi.org/10.2215/cjn.01290308 (2008).
Nassar, G. M. & Ayus, J. C. Infectious complications of the hemodialysis access. Kidney Int. 60, 1–13. https://doi.org/10.1046/j.1523-1755.2001.00765.x (2001).
Lockhart, P. B. et al. Bacteremia associated with toothbrushing and dental extraction. Circulation 117, 3118–3125. https://doi.org/10.1161/CIRCULATIONAHA.107.758524 (2008).
Yoneyama, T., Yoshida, M., Matsui, T. & Sasaki, H. Oral care and pneumonia. Oral Care Working Group. Lancet 354, 515. https://doi.org/10.1016/s0140-6736(05)75550-1 (1999).
Ishimaru, M., Ono, S., Matsui, H. & Yasunaga, H. Association between perioperative oral care and postoperative pneumonia after cancer resection: Conventional versus high-dimensional propensity score matching analysis. Clin. Oral Investig. 23, 3581–3588. https://doi.org/10.1007/s00784-018-2783-5 (2019).
Khadka, S. et al. Poor oral hygiene, oral microorganisms and aspiration pneumonia risk in older people in residential aged care: A systematic review. Age Ageing 50, 81–87. https://doi.org/10.1093/ageing/afaa102 (2021).
Fujinami, W., Nishikawa, K., Ozawa, S., Hasegawa, Y. & Takebe, J. Correlation between the relative abundance of oral bacteria and Candida albicans in denture and dental plaques. J. Oral Biosci. 63, 175–183. https://doi.org/10.1016/j.job.2021.02.003 (2021).
Kusama, T., Aida, J., Yamamoto, T., Kondo, K. & Osaka, K. Infrequent denture cleaning increased the risk of pneumonia among community-dwelling older adults: A population-based cross-sectional study. Sci. Rep. 9, 13734. https://doi.org/10.1038/s41598-019-50129-9 (2019).
Yaparathna, N., Hettiarachchi, R. M., Love, R., Robb, N. D. & Abuzar, M. Impact of removable partial dentures on masticatory performance in partial edentulism: A systematic review. Int. J. Prosthodont. https://doi.org/10.11607/ijp.8278 (2023).
Mizutani, K., Mikami, R., Saito, N., Sakaniwa, E. & Iwata, T. Periodontal disease and chronic kidney disease: The impact of oral health on inflammation and nutrition in patients undergoing hemodialysis. Curr. Oral Health Rep. 9, 81–88. https://doi.org/10.1007/s40496-022-00313-0 (2022).
Mikami, R. et al. Malnutrition–inflammation–atherosclerosis (MIA) syndrome associates with periodontitis in end-stage renal disease patients undergoing hemodialysis: A cross-sectional study. Sci. Rep. 13, 11805. https://doi.org/10.1038/s41598-023-38959-0 (2023).
Stenvinkel, P. et al. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 55, 1899–1911. https://doi.org/10.1046/j.1523-1755.1999.00422.x (1999).
Toniazzo, M. P., Amorim, P. S., Muniz, F. & Weidlich, P. Relationship of nutritional status and oral health in elderly: Systematic review with meta-analysis. Clin. Nutr. 37, 824–830. https://doi.org/10.1016/j.clnu.2017.03.014 (2018).
Kiesswetter, E. et al. Functional determinants of dietary intake in community-dwelling older adults: A DEDIPAC (DEterminants of DIet and Physical ACtivity) systematic literature review. Public Health Nutr. 21, 1886–1903. https://doi.org/10.1017/s1368980017004244 (2018).
Zelig, R. et al. Tooth loss and nutritional status in older adults: A systematic review and meta-analysis. JDR Clin. Trans. Res. 7, 4–15. https://doi.org/10.1177/2380084420981016 (2022).
Pecoits-Filho, R., Lindholm, B. & Stenvinkel, P. The malnutrition, inflammation, and atherosclerosis (MIA) syndrome—The heart of the matter. Nephrol. Dial. Transplant. 17(Suppl 11), 28–31. https://doi.org/10.1093/ndt/17.suppl_11.28 (2002).
de Oliveira, C., Watt, R. & Hamer, M. Toothbrushing, inflammation, and risk of cardiovascular disease: Results from Scottish Health Survey. BMJ 340, c2451. https://doi.org/10.1136/bmj.c2451 (2010).
Naugle, K., Darby, M. L., Bauman, D. B., Lineberger, L. T. & Powers, R. The oral health status of individuals on renal dialysis. Ann. Periodontol. 3, 197–205. https://doi.org/10.1902/annals.1998.3.1.197 (1998).
Oduncuoğlu, B. F., Alaaddinoğlu, E. E., Çolak, T., Akdur, A. & Haberal, M. Effects of renal transplantation and hemodialysis on patient’s general health perception and oral health-related quality of life: A single-center cross-sectional study. Transplant. Proc. 52, 785–792. https://doi.org/10.1016/j.transproceed.2020.01.016 (2020).
Abou-Bakr, A., Hussein, R. R., Khalil, E. & Ahmed, E. The frequency of periodontitis in end-stage renal disease on hemodialysis in a sample of Egyptian population: Multi-center clinical cross-sectional study. BMC Oral Health 22, 1. https://doi.org/10.1186/s12903-021-02032-x (2022).
Yoshioka, M. et al. Current status of collaborative relationships between dialysis facilities and dental facilities in Japan: Results of a nationwide survey. BMC Nephrol. 16, 17. https://doi.org/10.1186/s12882-015-0001-0 (2015).
Dumitrescu, A. L., Gârneaţă, L. & Guzun, O. Anxiety, stress, depression, oral health status and behaviours in Romanian hemodialysis patients. Rom. J. Intern. Med. 47, 161–168 (2009).
Ikegami, N. et al. Japanese universal health coverage: Evolution, achievements, and challenges. Lancet 378, 1106–1115. https://doi.org/10.1016/s0140-6736(11)60828-3 (2011).
Yamana, H. et al. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J. Epidemiol. 27, 476–482. https://doi.org/10.1016/j.je.2016.09.009 (2017).
Hara, K. et al. Association measures of claims-based algorithms for common chronic conditions were assessed using regularly collected data in Japan. J. Clin. Epidemiol. 99, 84–95. https://doi.org/10.1016/j.jclinepi.2018.03.004 (2018).
Ono, S. et al. Validity of diagnoses and procedures in Japanese dental claims data. BMC Health Serv. Res. 21, 1116. https://doi.org/10.1186/s12913-021-07135-3 (2021).
Taira, K. et al. Regional inequality in dental care utilization in Japan: An ecological study using the national database of health insurance claims. Lancet Reg. Health West Pac. 12, 100170. https://doi.org/10.1016/j.lanwpc.2021.100170 (2021).
Acknowledgements
This work was supported by a Grant-in-Aid for Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (grant number 20K18497 to RM).
Author information
Authors and Affiliations
Contributions
RM, KM, MI, TG, TI, and JA contributed to the conception. RM, KM, MI, and JA contributed to data acquisition and interpretation. RM and MI performed drafted the manuscript. RM, KM, MI, TG, TI, and JA critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mikami, R., Mizutani, K., Ishimaru, M. et al. Preventive dental care reduces risk of cardiovascular disease and pneumonia in hemodialysis population: a nationwide claims database analysis. Sci Rep 14, 12372 (2024). https://doi.org/10.1038/s41598-024-62735-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62735-3
- Springer Nature Limited