Abstract
Background
This study aimed to systematically review the literature to better understand the efficacy of electrical stimulation (ES) for the treatment of patients with diabetes-related ulcers.
Methods
We searched the Embase, Medline, and Cochrane Library databases through July 31, 2021. Original trials for ES treatment of patients with diabetes-related ulcers with placebo or standard care as the control group were included. The primary outcomes were ulcer area reduction and healing rates. Meta-analyses were performed to compare the standardized mean difference (SMD) in the percentage of ulcer reduction and risk ratio of non-healing rates between ES treatment and placebo or standard care. We used the Revised Cochrane risk-of-bias tool for randomized trials to assess the risk of bias for each included article. Funnel plots and Egger’s test were used to assess publication bias.
Results
Compared to placebo or standard care, ES had a significant benefit for the treatment of patients with diabetes-related ulcers in terms of percentage of ulcer reduction (SMD = 2.56, 95% CI: 1.43–3.69; P < 0.001 (Q-test), I2 = 93.9%) and ulcer healing rates [risk ratio of non-healing rates for the ES group was 0.72 (95% CI: 0.54–0.96; P = 0.38 (Q-test), I2 = 2.3%)]. Two, four, and three of the included studies were categorized into low risk of bias, some concerns, and high risk of bias, respectively. No publication bias was found.
Conclusions
Based on the findings of this meta-analysis, ES could be used to treat patients with diabetes-related ulcers. ES treatment was effective for ulcer area reduction and ulcer healing, although it had a high heterogeneity level among the included studies. Pulsed current ES has the potential benefit of increasing ulcer healing compared to direct current ES. Further large-scale clinical trials are needed to define the adverse events and potentiators of ES in the treatment of patients with diabetes-related ulcers.
Similar content being viewed by others
Background
In 2019, it was reported that 463 million people had diabetes worldwide, and this number is expected to reach 693 million by 2045 [1]. Diabetes-related neuropathy, peripheral arterial disease, and infection can lead to foot and lower leg ulcers, which can significantly impair a patient’s quality of life [2, 3]. Approximately 6.3% of patients with diabetes have foot ulcerations, and the prevalence of leg ulceration is approximately 1 to 2% [4, 5]. These ulcers often recur after healing and are associated with a high risk of amputation and death, as well as high medical expenses [2].
Debridement, negative pressure wound therapy, and antibacterial treatment are essential in the management of diabetes-related foot ulceration [2, 6]. However, these treatments are not always effective for all patients. Therefore, practitioners and researchers have been looking for alternative adjuvant treatments.
Electrical stimulation (ES) is a physical therapy modality that sends gentle electrical pulses through the skin [7]. The technique has been widely used in pain management and wound healing [8,9,10]. ES treatment is advantageous because it is cost-effective, simple, and has few complications. A recent meta-analysis showed that ES may be an effective adjunctive therapy for accelerating diabetes-related foot ulceration healing [11]. However, there is a lack of systematic evidence of the efficacy of ES for all diabetes-related ulcers. The objective of the present study was to systematically review the literature to better understand the efficacy of ES for the treatment of patients with diabetes-related ulcers.
Materials and methods
The reporting of the present review followed the PRISMA statement for systematic reviews and meta-analyses [12, 13]. The ethics review was waived because of the retrospective and anonymous characteristics of the study.
Literature search and study selection
We searched the Embase, Medline, and Cochrane Library databases through July 31, 2021. Search terms included “electric stimulation”, “electric stimulation therapy”, “transcutaneous electric nerve stimulation”, “skin ulcer”, and “ diabetes related ulcers”. The search strategies are provided in the Additional file 1: Appendix 1. The inclusion criteria of the articles were as follows: 1) randomized controlled trials (RCTs) and quasi-experimental studies in English, 2) patients with diabetes-related ulcers, including foot and leg ulcers, 3) ES as intervention, 4) having placebo or standard care as a control group, and 5) having information of target outcomes of healing rates or ulcer area reduction rates. The exclusion criteria were as follows: 1) not an original study (e.g., reviews, protocols, letters, or commentaries), 2) animal (non-human) studies, and 3) studies without information on target outcomes.
We included all ES types in the present review, including pulsed current type and direct current type, as the experiment arm. The primary outcomes were ulcer area reduction and healing rates. Other terms of standard care for the eligible control treatment were “usual care” and “standard treatment.”
After omitting duplicated studies, two independent reviewers (DX and ZYH) screened the titles and abstracts according to the eligibility criteria and defined the list of articles for full-text review. Title and abstract screening were performed using Endnote X9. The pre-test review form was used for the full-text review by the same independent reviewers. The reasons for excluding papers were discussed in detail between the reviewers. Any inconsistency regarding article inclusion was solved by discussion or with the help of a third-party reviewer (ZYH).
Data collection
YLH and LHY performed the data collection independently using the pre-test data collection sheet. The primary characteristics of the included studies - demographic characteristics of participants, sample size, countries, publication year, ES types, and follow-up period - were collected. Data of the two arms were collected for sample size, sex, and percentage of ulcer area reduction or ulcer healing.
Data analysis
All data analyses were performed using Stata, version 15.0 (Stata Corp. Texas, USA). Categorical variables are expressed as count and percentage/proportion. Continuous variables are expressed as mean with standard deviation (SD). Meta-analysis was performed for outcome measures. One of the primary outcomes was healing rate, which was calculated as the number of healing patients divided by total patients. Healing rates are presented as the risk ratio (RR) of non-healing rates with a 95% confidential interval (CI), and ulcer area reduction is presented as the standardized mean difference (SMD) with 95% CI. Heterogeneity was estimated using the Q-test and I2 score. When the P-value was < 0.1 (for Q-test) and I2 > 50%, the result was considered with heterogeneity, and the random-effects model was used for analysis. Otherwise, a fixed-effects model was applied for analysis. A P-value of < 0.05 was set as the threshold for statistical significance. Subgroup analysis was performed according to the ES types.
As limited data were available, meta-regression could not be performed. We evaluated the risk of bias using the Revised Cochrane risk-of-bias tool for randomized trials (RoB2) [14]. Funnel plots and the Egger’s test were used to determine publication biases.
Results
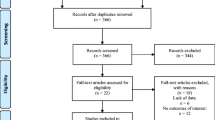
A total of 1042 articles were identified using our search criteria. After omitting duplicated studies, 794 articles were further screened for title and abstract. Of these, 20 articles were selected for full-text review. Finally, 10 articles were included in the data quality assessment and data analysis [15,16,17,18,19,20,21,22,23,24]. Study inclusion is present in Fig. 1.
Characteristics of the included studies
All studies were RCTs published from 1992 to 2021. Our analysis included a total of 352 patients with diabetes-related ulcers ranging in age from 48.4 to 65.1 years. The median follow-up period ranged from 4 to 12 weeks. There were two experimental groups with different adjuvant heat plus ES [18], three studies reported direct current ES as the treatment modality [22,23,24], and all other studies applied pulsed current ES as the intervention. Details of the study characteristics are described in Table 1.
Risk of bias assessment
None of the included studies had the bias of missing data. Seven of the nine included RCTs (7/10 studies, 70.0%) had some concerns of bias in selecting reported results due to lack of protocol information or trial registration. Five studies had some concerns about risk in randomization because there was no information in random sequence generation (6/10 studies, 60.0%). Three studies had some concerns in both deviations from intended intervention and measurement of the outcome due to the risk in allocation concealment or blinding of participants and personnel (3/10 studies, 30.0%). In summary, two studies [21, 22], four studies [15,16,17, 23], and four studies [18,19,20, 24] were categorized into low risk of bias, some concerns, and high risk of bias, respectively. The details of the risk of bias assessment can be found in Table 2.
Ulcer area reduction
The ES arm of our meta-analysis showed statistical benefit for ulcer area reduction compared to the control arm (Fig. 2). The percentage of ulcer area reduction was significantly greater in patients treated with ES than in those treated with standard care or placebo (SMD = 2.56, 95% CI: 1.43–3.69; P < 0.001 (Q-test), I2 = 93.9%). See data extraction results in Additional file 2: Appendix 2.
According to the subgroup analysis of current types, there was no statistical difference in ulcer area reduction between pulsed current ES (SMD = 3.01, 95% CI: 1.43–3.69) and direct current ES (SMD = 1.45, 95% CI: 0.86–2.04). The highest ulcer reduction was found in Petrofsky et al. (2007) with global heat plus ES. According to the subgroup analysis of ulcer types, there was no statistical difference in ulcer area reduction between leg ulcers (SMD = 1.58, 95% CI: 1.03–2.13) and foot ulcers (SMD = 2.41, 95% CI: 0.88–3.94). After omitting the studies with serious risk or some concerns of bias, the percentage of ulcer area reduction was still significantly greater in patients treated with ES than in those treated with standard care or placebo (SMD = 1.52, 95% CI: 1.11–1.92). The study reported by Zulbaran-Rojas et al. does not have available data to enter the meta-analysis. However, the four-week ulcer deduction was significant in the ES arm (P = 0.002) but not in the control placebo arm (P = 0.982) [24].
Healing rates
According to the pooled results, the diabetes-related ulcer healing rate was significantly higher in the ES arms than in the control arm (P < 0.05). Compared to the control group, the RR of non-healing rates for the ES group was 0.72 (95% CI: 0.54–0.96; P = 0.38 (Q-test), I2 = 2.3%; Fig. 3). According to the subgroup analysis of ulcer types, there was no statistical difference in healing rates between leg ulcers (0.36, 95% CI: 0.13–0.99) and foot ulcers (SMD = 0.71, 95% CI: 0.47–1.07). Only one study had risk of bias in the related data and was not about to perform sensitivity analysis. See data extraction results in Appendix 2.
Publication bias
The P-values of the Egger’s test for the percentage of ulcer area reduction and ulcer healing rates were 0.636 and 0.843, respectively. There was no obvious asymmetry in the funnel plots (Fig. 4), and Egger’s test suggested no publication bias although the number of studies was limited.
Discussion
In the present systematic review and meta-analysis, we found that ES has a significant benefit compared to placebo or standard care for the treatment of patients with diabetes-related ulcers with regards to the percentage of ulcer reduction (SMD = 2.79, 95% CI: 1.58–4.01) and ulcer healing rates (RR of non-healing rates for the ES group was 0.72, 95% CI: 0.54–0.96). We applied the random effect model to the meta-analysis of SMD in the percentage of ulcer reduction due to the study heterogeneity (P < 0.001 (Q-test), I2 = 93.9%). The sources of heterogeneity may be due to the different ulcer types and follow-up times. Our findings are similar to a recently published systematic review on ES for people with diabetes-related foot ulcers [11]. Again, the slight difference in effect size between our results and the review may be due to different follow-up periods and the defined outcomes. We also included all ulcer types, including leg ulcers, in this meta-analysis.
It has been reported in preclinical studies that ES can enhance cellular activities (e.g., DNA and collagen synthesis, generation of chemotaxis factor, and adenosine triphosphate concentration) [25, 26]. In addition, ES can promote wound healing by increasing tissue perfusion and enhancing angiogenesis [27, 28]. Based on the findings of the present study, ES can be used as a critical treatment for people with diabetes-related ulcers in clinical practice.
ES can be categorized into direct current types: alternating current type and pulsed current type. Pulsed current ES involves a 1 ms to 1 s electrical flow as a monophasic pulsed waveform. In contrast, direct current ES uses unidirectional flow for 1 s or longer. Low frequency alternating current ES has not been used in wound healing, but the other two techniques have been explored [29]. In the present study, we did not find a statistical difference between the two ES types for ulcer healing and ulcer area reduction. However, the mean SMD of pulsed current ES (3.01) was greater than that of direct current ES (1.45), indicating that pulsed current ES may promote better healing of ulcers than direct current ES. Future large-scale clinical trials are needed to confirm this hypothesis.
Studies have shown a promising result of ES on wound recovery in diabetes-related ulcers on diabetic fibroblasts in diabetic animals [30, 31]. The rationale may be that ES functions to accelerate angiogenesis and enhance epithelialization [23, 32]. ES can also enhance sensation in diabetic neuropathic patients using mechanical noise [33,34,35] and significantly improve ischemic diabetic foot ulcers [22, 36]. However, we do not have enough data in the present study to explore the effects of ES on different diabetes-related ulcers. Future research is needed to provide more valid evidence (e.g., using ankle-brachial pressure index (ABPI) or vibration perception threshold (VPT) testing) during ES treatment to confirm its reliability [37, 38].
Some limitations of the present study should be noted. 1) ES appeared safe for treating people with diabetes-related ulcers. Therefore, we did not have sufficient data to explore the adverse events of ES. 2) We could not perform a meta-regression analysis to explore possible potentiators of ES effects due to the limited data. 3) There was insufficient data to perform subgroup analysis according to different ulcer types, which will be addressed in our future research. 4) Although all included studies were RCTs, only two studies were categorized as having a low risk of bias. The main limitations focus on lack of protocol information to clarify, no selection reporting, no information on the generation of randomization, and some concerns in blinding or masking. Therefore, the low quality of the evidence could potentially reduce the impact of the present findings.
Conclusion
Based on the findings of this meta-analysis, ES could be used to treat people with diabetes-related foot or leg ulcers. ES treatment was effective for ulcer area reduction and ulcer healing, although it had a high heterogeneity level among the included studies. Pulsed current ES has the potential benefit of increasing ulcer healing compared to direct current ES. Further large-scale clinical trials are needed to define the adverse events and potentiators of ES in the treatment of people with diabetes-related foot or leg ulcers.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available since none of the data types requiring uploading to a public repository are contained in this manuscript but are available from the corresponding author on reasonable request.
Abbreviations
- ES:
-
Electrical stimulation
- SD:
-
Standard deviation
- CI:
-
Confidential interval
- SMD:
-
Standardized mean difference
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. https://doi.org/10.1016/j.diabres.2019.107843.
Boulton AJM, Whitehouse RW. The Diabetic Foot. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dungan K, Grossman A, Hershman JM, Hofland J, Kaltsas G, et al., editors. Endotext. South Dartmouth: MDText.com, Inc. Copyright © 2000-2021, MDText.com, Inc; 2000.
Boike A, Maier M, Logan D. Prevention and treatment of leg and foot ulcers in diabetes mellitus. In: Current Clinical Medicine. Elsevier; 2010. p. 387–90. e381. https://www.researchgate.net/publication/344866238_Prevention_and_Treatment_of_Leg_and_Foot_Ulcers_in_Diabetes_Mellitus.
Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis (†). Ann Med. 2017;49(2):106–16. https://doi.org/10.1080/07853890.2016.1231932.
Mekkes J, Loots M, Van Der Wal A, Bos J. Causes, investigation and treatment of leg ulceration. Br J Dermatol. 2003;148(3):388–401.
Doupis J, Veves A. Classification, diagnosis, and treatment of diabetic foot ulcers. Wounds. 2008;20(5):117–26.
Starkey C. Therapeutic modalities. 4th ed. Philadelphia: FA Davis Co.; 2004.
Barassi G, Pokorski M, Matteo CD, Supplizi M, Prosperi L, Guglielmi V, et al. Manual pressure release and low-grade electrical peripheral receptor stimulation in nonspecific low Back pain: a randomized controlled trial. Adv Exp Med Biol. 2021;1324:73–81. https://doi.org/10.1007/5584_2020_605.
Jeon YH. Spinal cord stimulation in pain management: a review. Korean J Pain. 2012;25(3):143–50. https://doi.org/10.3344/kjp.2012.25.3.143.
Thakral G, Lafontaine J, Najafi B, Talal TK, Kim P, Lavery LA. Electrical stimulation to accelerate wound healing. Diabet Foot Ankle. 2013;4. https://doi.org/10.3402/dfa.v4i0.22081.
Chen Z, Chen ZY, Liu WH, Li GS. Electric stimulation as an effective adjunctive therapy for diabetic foot ulcer: a Meta-analysis of randomized controlled trials. Adv Skin Wound Care. 2020;33(11):608–12. https://doi.org/10.1097/01.ASW.0000695784.82605.1e.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Lundeberg TCM, Eriksson SV, Malm M. Electrical nerve stimulation improves healing of diabetic ulcers. Ann Plast Surg. 1992;29(4):328–31. https://doi.org/10.1097/00000637-199210000-00009.
Baker LL, Chambers R, DeMuth SK, Villar F. Effects of electrical stimulation on wound healing in patients with diabetic ulcers. Diabetes Care. 1997;20(3):405–12. https://doi.org/10.2337/diacare.20.3.405.
Peters EJ, Lavery LA, Armstrong DG, Fleischli JG. Electric stimulation as an adjunct to heal diabetic foot ulcers: a randomized clinical trial. Arch Phys Med Rehabil. 2001;82(6):721–5. https://doi.org/10.1053/apmr.2001.23780.
Petrofsky JS, Lawson D, Suh HJ, Rossi C, Zapata K, Broadwell E, et al. The influence of local versus global heat on the healing of chronic wounds in patients with diabetes. Diabetes Technol Ther. 2007;9(6):535–44.
Petrofsky JS, Lawson D, Berk L, Suh H. Enhanced healing of diabetic foot ulcers using local heat and electrical stimulation for 30 min three times per week. J Diab. 2010;2(1):41–6. https://doi.org/10.1111/j.1753-0407.2009.00058.x.
Liani M, Trabassi E, Cusaro C, Zoppis E, Maduli E, Pezzato R, et al. Effects of a pulsatile electrostatic field on ischemic injury to the diabetic foot: evaluation of refractory ulcers. Primary Care Diabetes. 2014;8(3):244–9. https://doi.org/10.1016/j.pcd.2013.11.009.
Ortíz MCS, Villabona EH, Lemos DMC, Castellanos R. Effects of low level laser therapy and high voltage stimulation on diabetic wound healing. Revista de la universidad industrial de santander Salud. 2014;46(2):107–17.
Asadi MR, Torkaman G, Hedayati M, Mohajeri-Tehrani MR, Ahmadi M, Gohardani RF. Angiogenic effects of low-intensity cathodal direct current on ischemic diabetic foot ulcers: a randomized controlled trial. Diabetes Res Clin Pract. 2017;127:147–55. https://doi.org/10.1016/j.diabres.2017.03.012.
Mohajeri-Tehrani MR, Nasiripoor F, Torkaman G, Hedayati M, Annabestani Z, Asadi MR. Effect of low-intensity direct current on expression of vascular endothelial growth factor and nitric oxide in diabetic foot ulcers. J Rehabil Res Dev. 2014;51(5):815–24. https://doi.org/10.1682/jrrd.2013.08.0174.
Zulbaran-Rojas A, Park C, El-Refaei N, Lepow B, Najafi B. Home-based electrical stimulation to accelerate wound healing-a double-blinded randomized control trial. J Diabetes Sci Technol. 2021;19322968211035128. https://doi.org/10.1177/19322968211035128.
Kloth LC, Zhao M: Endogenous and exogenous electrical fields for wound healing. Physical Therapy Faculty Research and Publications: F.A. Davis Co.; 2010.
Shupack JL, Stiller MJ, Gropper C, Slue W Jr. High-tech dermatology. J Am Acad Dermatol. 1992;26(5 Pt 1):785–6. https://doi.org/10.1016/s0190-9622(08)80564-6.
Ennis WJ, Lee C, Plummer M, Meneses P. Current status of the use of modalities in wound care: electrical stimulation and ultrasound therapy. Plast Reconstr Surg. 2011;127(Suppl 1):93s–102s. https://doi.org/10.1097/PRS.0b013e3181fbe2fd.
Veith AP, Henderson K, Spencer A, Sligar AD, Baker AB. Therapeutic strategies for enhancing angiogenesis in wound healing. Adv Drug Deliv Rev. 2019;146:97–125. https://doi.org/10.1016/j.addr.2018.09.010.
Kloth LC. Electrical stimulation technologies for wound healing. Adv Wound Care. 2014;3(2):81–90. https://doi.org/10.1089/wound.2013.0459.
Sari Y, Hartono SE, Saryono. The effect of short duration of electrical stimulation on wound healing in acute wound in a rat model. Wound Medicine. 2019;24(1):36–44. https://doi.org/10.1016/j.wndm.2019.02.003.
Fraccalvieri M, Salomone M, Zingarelli EM, Rivarossa F, Bruschi S. Electrical stimulation for difficult wounds: only an alternative procedure? Int Wound J. 2015;12(6):669–73. https://doi.org/10.1111/iwj.12194.
Wang XF, Li ML, Fang QQ, Zhao WY, Lou D, Hu YY, et al. Flexible electrical stimulation device with chitosan-Vaseline® dressing accelerates wound healing in diabetes. Bioact Mater. 2021;6(1):230–43. https://doi.org/10.1016/j.bioactmat.2020.08.003.
Khaodhiar L, Niemi JB, Earnest R, Lima C, Harry JD, Veves A. Enhancing sensation in diabetic neuropathic foot with mechanical noise. Diabetes Care. 2003;26(12):3280–3. https://doi.org/10.2337/diacare.26.12.3280.
Cloutier R, Horr S, Niemi JB, D'Andrea S, Lima C, Harry JD, et al. Prolonged mechanical noise restores tactile sense in diabetic neuropathic patients. Int J Low Extrem Wounds. 2009;8(1):6–10. https://doi.org/10.1177/1534734608330522.
Janković A, Binić I. Frequency rhythmic electrical modulation system in the treatment of chronic painful leg ulcers. Arch Dermatol Res. 2008;300(7):377–83. https://doi.org/10.1007/s00403-008-0875-9.
Asadi MR, Torkaman G, Mohajeri-Tehrani MR, Hedayati M. Effects of electrical stimulation on the Management of Ischemic Diabetic Foot Ulcers. Babol-Jbums. 2015;17(7):7–14. https://doi.org/10.22088/jbums.17.7.7.
Liu M, Gao Y, Chen DW, Lin S, Wang C, Chen LH, et al. Quantitative vibration perception threshold in assessing diabetic polyneuropathy: should the cut-off value be adjusted for Chinese individuals with type 2 diabetes? J Diabetes Investig. 2021;12(9):1663–70. https://doi.org/10.1111/jdi.13515.
Al-Qaisi M, Nott DM, King DH, Kaddoura S. Ankle brachial pressure index (ABPI): an update for practitioners. Vasc Health Risk Manag. 2009;5:833–41. https://doi.org/10.2147/vhrm.s6759.
Acknowledgments
None.
Funding
The present study is a sub study of a Jilin Provincial Department of Education scientific research project (project ID: 46290) with contract No. of JJKH20221068KJ.
Author information
Authors and Affiliations
Contributions
XD performed data collection, data analysis, and article preparation. LQY and HYL performed the analysis and collation of the literature. YHZ conceived of the study idea and article review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Search strategy.
Additional file 2: Appendix 2.
Data collection table.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, Y., Du, X., Yin, L. et al. Effect of electrical stimulation on patients with diabetes-related ulcers: a systematic review and meta-analysis. BMC Endocr Disord 22, 112 (2022). https://doi.org/10.1186/s12902-022-01029-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-022-01029-z