Abstract
Background
In clinical practice, we often observed that patients who underwent total thyroidectomy due to clinically involved nodal disease (cN1a) actually had less extensive CLNM on final pathology. This study investigates whether total thyroidectomy and therapeutic bilateral CND are necessary for all PTC patients with cN1a.
Methods
This study retrospectively reviewed 899 PTC patients who underwent total thyroidectomy with bilateral CND from January 2012 to June 2017. The patients were divided into two groups according to pre-operative central lymph node (CLN) status: cN0, no suspicious CLNM; cN1a, suspicious CLNM. We compared the clinicopathological features of these two groups.
Results
There was no significant difference in recurrence between cN0 and cN1a groups after a mean follow-up time of 59.1 months. Unilateral cN1a was related to the largest central LN size ≥ 2 mm (OR = 3.67, p < 0.001) and number of CLNM > 5(OR = 2.24, p = 0.006). On the other hand, unilateral cN1a was not associated with an increased risk of contralateral lobe involvement (OR = 1.35, p = 0.364) and contralateral CLNM (OR = 1.31, p = 0.359). Among 106 unilateral cN1a patients, 33 (31.1%) were found to be pN0 or had ≤ 5 metastatic CLNs with the largest node smaller than 2 mm.
Conclusions
Most cN1a patients were in an intermediate risk group for recurrence and required total thyroidectomy. However, lobectomy with CND should have performed in approximately 30% of the cN1a patients. Pre-operative clinical examination, meticulous radiologic evaluation, and intra-operative frozen sections to check the nodal status are prerequisites for this approach.
Similar content being viewed by others
Background
According to the 2015 American Thyroid Association (ATA) guidelines, total thyroidectomy with therapeutic central-compartment neck dissection (CND) is recommended for papillary thyroid carcinoma (PTC) patients with suspicious central lymph node metastasis (CLNM) on preoperative imaging [1]. Total thyroidectomy can be also considered when more than five metastatic central lymph node are present or the maximal dimension of a metastatic lymph node is greater than 2 mm, as these pathologic features indicate an intermediate risk of disease recurrence [2].
In spite of advantages after total thyroidectomy the availability of radioactive iodine (RAI) for ablation therapy and thyroglobulin as a follow-up tumor marker, several current studies have reported little or no difference in long-term rates of recurrence between lobectomy and total thyroidectomy [3, 4]. In addition, total thyroidectomy is associated with increased surgery-related complications [5, 6] and a requirement for lifelong thyroid hormone replacement therapy.
We hypothesized that, to a certain point, clinically involved central lymph node metastasis (cN1a) may not represent extensive metastasis, and lobectomy with ipsilateral CND can therefore be performed in selected cN1a PTC patients.
Methods
Patient selection
This retrospective single-center study was approved by the Institutional Review Board at Samsung Medical Center. From January 2012 to June 2017, a total of 1859 patients diagnosed with PTC underwent total thyroidectomy with CND at the Thyroid Cancer Center of the Samsung Medical Center, which is a tertiary referral center in Korea. Among these, 230 cases with other variants of PTC (follicular variant, tall cell, cribriform-morular, etc.) were excluded, and 608 out of 1629 patients who had only unilateral CND were excluded, either. After excluding 122 patients who were suspicious of bilateral cN1a at pre-operative sonographic evaluation, a total of 899 patients were included in the final cohort (Fig. 1).
All patients were assessed preoperatively by ultrasonography (US) to evaluate primary tumors and identify abnormal lymph nodes. Suspicious thyroid lesions were diagnosed by fine-needle aspiration (FNA). Clinically involved lymph node disease (cN1a) was defined as lymph node metastases in the central neck compartment on preoperative US.
Surgical methods
Surgical strategies were performed according to the ATA guidelines [1]. Total thyroidectomy and therapeutic CND is typically performed after CLNM is detected during preoperative US. Patients who were node-negative at the time of preoperative ultrasonography underwent total thyroidectomy with prophylactic CND at the surgeon’s discretion. CND was defined as a central neck dissection extending superiorly to the hyoid bone, inferiorly to the innominate artery, laterally to the carotid sheaths, and dorsally to the prevertebral fascia. The term “ipsilateral” was used to indicate the same side as the main tumor, and “contralateral” was defined as the opposite side of the main tumor. In cases of bilateral tumors, the largest tumor was considered to be the main tumor. Central-compartment lymph nodes include pretracheal, prelaryngeal, and paraesophageal lymph nodes. For example, ipsilateral CLNs indicate pretracheal, prelaryngeal, and paraesophageal lymph nodes in the same side as the main tumor.
Histopathological examination of surgical specimens
Surgical specimens were examined microscopically by at least two experienced pathologists. The following histopathologic factors were assessed: main tumor size (longest diameter of the largest lesion), main tumor cell type, multifocality, bilaterality, microscopic or gross extrathyroidal extension (ETE), regional lymph node metastasis (central or lateral compartment), and underlying conditions of the thyroid, such as chronic lymphocytic thyroiditis (CLT). We checked the maximum dimension of metastatic foci in the lymph nodes if metastasis was present. With multiple tumor deposits in a single lymph node, the pathologists measured the largest dimension of the largest deposit. Multifocality was defined as the presence of two or more lesions in one lobe, regardless of bilaterality. ETE was defined as direct extension to perithyroidal soft tissues, strap muscles, nerves, or small vascular structures by the thyroid tumor. Minimal (microscopic) ETE was defined as an invasion detected only in a microscopic exam. If the involved tissue was completely removed along with the tumor, the resection margin was reported as negative. Staging of thyroid cancer was determined in accordance with the 7th edition of the American Joint Committee on Cancer’s Cancer Staging Manual and the Future of TNM [7].
Post-operative follow-up and management
After the initial surgery, all patients underwent regular follow-up at 6- to 12-month intervals with clinical evaluations including physical examinations, US, thyroid function tests (including T3, free T4, thyroid-stimulating hormone), and measurements of serum thyroglobulin (Tg) with its antibody. CT or iodine-131 (131I) scans was administrated if needed during follow up. Suspicious lesions for recurrence were evaluated by US-guided FNA biopsy with or without washout-thyroglobulin(wTg) levels and/or CT or positron emission tomography. Locoregional recurrence was defined as the presence of tumors or metastatic lymph nodes on cytology from FNA or the elevation of wTg level. RAI therapy was performed with 131I at 4–12 weeks after surgery according to ATA guidelines.1 RAI was administered after thyroid hormone withdrawal or after stimulation with recombinant thyroid-stimulating hormone. When RAI treatment was no longer required, patients resumed regular follow-ups.
Statistical analysis
Statistical analysis was performed using IBM SPSS version 24.0. Variables with a p value < 0.05 were considered statistically significant. The chi-square test and Student’s t-test were used to compare categorical variables between the group of unilateral cN1a patients and the group of cN0 patients. For factors that appeared to be related based on initial analysis, we used logistic regression to identify associated variables.
Results
Clinicopathological characteristics of 899 PTC patients
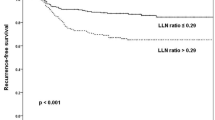
The 899 patients were divided into two groups according to preoperative physical and radiologic CLN status: 793 (88.2%) patients without clinically involved CLN (cN0) and 106 (11.8%) patients with clinically involved CLN (cN1a). The clinicopathological characteristics of the patients in each group are listed in Table 1. The mean age was significantly lower in the cN1a group (cN0: cN1a = 47.1 years: 43.4 yrs.; p = 0.002). Association with chronic lymphocytic thyroiditis was more common in the cN1a group (n = 44; 41.5%) than in the cN0 group (n = 230; 29%) (p = 0.009). The mean number of retrieved CLNs was 9.7 in the cN0 group and 11.7 in the cN1a group (p < 0.001). CLNM was more frequent in the cN1a group compared to the cN0 group (77.4% vs. 57.5%; p < 0.001). In contrast, contralateral central neck metastasis was not significantly different; 34.9% in the cN0 group and 37.8% in the cN1a group (p = 0.609). We analyzed the number and largest diameter of metastatic LNs in patients with pathologically proven CLNM (pN1, n = 538). The number of patients with more than 5 metastatic LNs was 81 (17.8%) in the cN0 group and 26 (31.7%) in the cN1a group, and this result was statistically significant (p = 0.004). There were more cases with largest LN diameter ≥ 2 mm in the cN1a group (82.8%) than in the cN0 group (66.7%) (p < 0.001). With a median follow-up of 59.1 months (range, 24 to 98 months), there was no difference in recurrence between the two groups (p = 1.000); 14 patients (1.8%) in the cN0 group and 2 patients (1.9%) in the cN1a group (Table 1).
Logistic analysis for factors related to contralateral lobe involvement & contralateral central lymph node metastasis
We performed a multivariate analysis with 643 patients who were pre-operatively diagnosed with unilateral PTC to verify factors related to contralateral lobe involvement. Multifocality was significantly associated with contralateral lobe involvement (OR = 3.164, p < 0.001), while unilateral cN1a was not (p = 0.364) (Table 2).
Further subgroup analysis including patients with pathologically-proven unilateral PTC (n = 619) indicated that factors of male sex (OR = 1.798, p < 0.010), tumor size (OR = 1.605, p = 0.001), multifocality (OR = 2.496, p < 0.001), and ipsilateral central neck metastasis (OR = 3.255, p < 0.001) increased the risk of contralateral central neck metastasis. Unilateral cN1a, however, was not significantly associated with contralateral central neck metastasis (p = 0.359) (Table 3).
Risk factors for the number of metastatic central lymph node > 5 & the largest metastatic central lymph node ≥ 2 mm
Table 4 shows that the risk factors for more than five metastatic LNs in pN1 patients were unilateral cN1a (OR = 2.240, p = 0.006), tumor size (OR = 1.613, p = 0.003), multifocality (OR = 1.799, p = 0.022), and contralateral central neck metastasis (OR = 3.550, p < 0.001). Table 5 indicated that the risk factors for a metastatic LN larger than 2 mm were unilateral cN1a (OR = 3.667, p < 0.001) and age (OR = 0.946, p < 0.001).
Final pathology of patients with unilateral cN1a
In 106 unilateral cN1a patients, 33 (31.1%) were found to be pN0 or had ≤ 5 metastatic CLNs with the largest node smaller than 2 mm. For the balance of the patients (69.2%), 1 patient (0.9%) had more than 5 metastatic CLNs with the largest node < 2 mm or pN0, 47 patients (44.3%) had fewer than 5 metastatic CLNs with the largest node ≥ 2 mm, and 25 patients (23.7%) had more than 5 metastatic CLNs with the largest node ≥ 2 mm (Table 6).
Discussion
For many decades, cN1a patients were expected to have more than five metastatic central LNs and/or the largest metastatic LN size greater than 2 mm, and total thyroidectomy and CND are considered because of the recurrence rate up to 20% [1, 8]. However, among cN1a patients who had total thyroidectomy and CND, some had less extensive or even no central neck metastasis on final pathology. This study was designed based on the results from previous study by our research team [9]. Among 295 papillary thyroid microcarcinoma patients with cN1a, about 73% of patients actually had micrometastasis and these low-risk patients shouldn’t have undergone total thyroidectomy and bilateral CND [9]. Since surgery has been decreasing in patient with tumor size less than 1 cm due to active surveillance, we wondered what results would be in patients with all sizes of PTC. We considered that including all tumor size will be more useful in real world practice. To improve a quality of study, we collected more sample size from different period and performed more test statistics this time. This study searched for the patients with cN1a disease who are candidates for lobectomy with unilateral CND rather than total thyroidectomy with bilateral CND by comparing patients with cN0 and cN1a.
The accuracy of preoperative diagnosis of LN status has improved markedly with the advent of high-resolution sonography and increased sonographer experience [10,11,12]. While identification of cN1a patients has improved with these advancements, detection of microscopic CLNM remains challenging [13]. In clinical practice, we often observed that patients who underwent total thyroidectomy due to cN1a actually had less extensive CLNM on final pathology. In these patients, a less-extensive surgery rather than total thyroidectomy may have been sufficient. We therefore hypothesized that lobectomy with unilateral CND instead of total thyroidectomy with bilateral CND could be safely performed for the selected patients with cN1a.
To support this hypothesis, several conditions should be considered. First, cN1a status does not always indicate having more than five metastatic LNs or largest metastatic LN size greater than 2 mm. Second, patients with a cN1a are not at increased risk of contralateral lobe involvement. Third, a cN1a patient does not have increased contralateral CLNM. Finally, intra-operative frozen exam should be available during the operation.
As described above, this study showed that cN1a was closely associated with more than five metastatic LNs or largest metastatic LN size greater than 2 mm, and approximately 69.0% of the patients required total thyroidectomy. However, the other 31.1% of patients (n = 33) had fewer than 5 metastatic CLNs with the largest metastatic LN size less than 2 mm, indicating that total thyroidectomy could have avoided. Furthermore, 13 of 33 patients did not have any lymph node metastasis. It is possible that lymph node enlargement with suspicious feature could be caused by a local benign condition [14] (e.g., underlying parenchymal disease). In patients with CLT, ultrasound features can be diverse depending on the severity and the phase of disease [15, 16]. CLT with CLN enlargement is common in Korean patients who live in iodine-rich areas [17, 18]. Among above 33 cN1a patients who had fewer than 5 metastatic CLNs with the largest node < 2 mm, 22 patients (67.0%) presented with CLT in the final pathology. This condition is the most common inflammatory disorder of the thyroid gland [19], and although its influence on PTC prognosis remains controversial [20], many authors maintain that coexistence of CLT with PTC is related to lower-stage disease and favorable prognostic factors [21,22,23,24]. If patients with cN1a have underlying thyroiditis, an intra-operative frozen exam, if available, is helpful to avoid unnecessary contralateral lobectomy and contralateral CND.
Despite a controversy over usefulness of frozen exam, several studies showed that intra-operative frozen exam had the effectiveness and clinical value [25, 26]. In addition, gross inspection by surgeons is not a precise method for differentiating CLNM [27]. Although this usually takes additional time and has limited accuracy of diagnosis, it is obvious that intraoperative frozen exam is more precise than intraoperative gross inspection or palpation. Intra-operative frozen biopsy can be helpful for reducing completion thyroidectomy or unnecessary overtreatment. However, comprehensive evaluation of whole dissected CLN is not feasible and recommendable in every practice. Collaborative discussions with pathologists can address these issues.
Although there is no consensus about the extent of CND in unilateral cN1a patients, many studies suggest that prophylactic contralateral CND is unnecessary [28,29,30,31] because of the low probability of contralateral CLNM and potential morbidity that can accompany an extensive surgery [32, 33]. Prophylactic contralateral CND was associated with increased rates of transient and permanent hypoparathyroidism [34, 35]. Our results indicate that unilateral cN1a does not increase the risk of contralateral lobe involvement or contralateral central neck metastasis, which means that contralateral CND may not be needed for unilateral cN1a patients. The clinical significance of contralateral CND remains unclear especially when contralateral CLNM is a microscopic. Not shown in this study, recurrence rate of patients who underwent total thyroidectomy with unilateral CND was only 2.6%, comparable to 1.9% in the recurrence rate of patients who underwent total thyroidectomy with bilateral CND. Further studies are required to confirm the necessity of prophylactic contralateral CND, as well as the relationships between contralateral CLNM and number, maximum size, and ipsilateral CLNM involvement.
There were several limitations of this study, which was a non-randomized, retrospective cohort study at a single institution. First, potential confounding variables may not have been identified. Second, subgroup analysis comparing pathologic nodal status and clinical nodal status was not performed. Since this study was retrospective study, difference between clinical nodal status and pathologic nodal status was one of the unavoidable discrepancies caused by radiologist’s or pathologist’s experience. Third, inter-observer variation in the detection and interpretation of cervical lymph node metastasis and inconsistent surgical management were involved because of the long-term follow-up. Lastly, our findings may not be applicable to all centers because availability and cooperation of skilled pathologists are essential for surgical decision-making. In spite of these limitations, our retrospective data showed that about 31% of patients with unilateral cN1a were able to avoid total thyroidectomy. Prospective study with larger cohort is essential to clarify this subject.
Conclusion
This study suggests that, although the majority of PTC patients with unilateral cN1a still needs total thyroidectomy with bilateral CND, lobectomy and unilateral CND can be considered in selected patients. Intra-operative frozen exam may help to identify low risk patients among cN1a patients and reduce overtreatment.
Availability of data and materials
The data that support the findings of this study are available from Samsung Medical Center but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Samsung Medical Center.
Abbreviations
- CND:
-
Central central-compartment neck dissection
- PTC:
-
Papillary thyroid carcinoma
- CLNM:
-
Central lymph node metastasis
- cN1a:
-
Clinically involved central lymph node disease
- cN0:
-
Clinically not involved central lymph node disease
- CLN:
-
Central lymph node
- RAI:
-
Radioactive iodine
- Tg:
-
Serum thyroglobulin
- wTg:
-
Washout-thyroglobulin
- US:
-
Ultrasonography
- FNA:
-
Fine-needle aspiration
- ETE:
-
Extrathyroidal extension
- CLT:
-
Chronic lymphocytic thyroiditis
References
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: the American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1–133.
Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012;22:1144–52.
Lee J, Park JH, Lee CR, Chung WY, Park CS. Long-term outcomes of total thyroidectomy versus thyroid lobectomy for papillary thyroid microcarcinoma: comparative analysis after propensity score matching. Thyroid. 2013;23:1408–15.
Kuba S, Yamanouchi K, Hayashida N, Maeda S, Adachi T, Sakimura C, et al. Total thyroidectomy versus thyroid lobectomy for papillary thyroid cancer: comparative analysis after propensity score matching: a multicenter study. Int J Surg. 2017;38:143–8.
Hauch A, Al-Qurayshi Z, Randolph G, Kandil E. Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol. 2014;21:3844–52.
Ryu J, Ryu YM, Jung YS, Kim SJ, Lee YJ, Lee EK, et al. Extent of thyroidectomy affects vocal and throat functions: a prospective observational study of lobectomy versus total thyroidectomy. Surgery. 2013;154:611–20.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471–4.
Sivanandan R, Soo KC. Pattern of cervical lymph node metastases from papillary carcinoma of the thyroid. Br J Surg. 2001;88:1241–4.
Back K, Lee J, Choe JH, Kim JH, Oh YL, Kim JS. Total thyroidectomy can be overtreatment in cN1a papillary thyroid carcinoma patients whose tumor is smaller than 1 cm. Am J Surg. 2021. https://doi.org/10.1016/j.amjsurg.2021.08.015.
Liu Z, Zeng W, Liu C, Wang S, Xiong Y, Guo Y, et al. Diagnostic accuracy of ultrasonographic features for lymph node metastasis in papillary thyroid microcarcinoma: a single-center retrospective study. World J Surg Oncol. 2017;15:32.
Yoo YH, Kim JA, Son EJ, Youk JH, Kwak JY, Kim EK, et al. Sonographic findings predictive of central lymph node metastasis in patients with papillary thyroid carcinoma: influence of associated chronic lymphocytic thyroiditis on the diagnostic performance of sonography. J Ultrasound Med. 2013;32:2145–51.
Sipos JA. Advances in ultrasound for the diagnosis and management of thyroid cancer. Thyroid. 2009;19:1363–72.
Noda S, Onoda N, Morisaki T, Kashiwagi S, Takashima T, Hirakawa K. The significance and the predictive factors of microscopic lymph node metastasis in patients with clinically node negative papillary thyroid cancer: a retrospective cohort study. Int J Surg. 2015;20:52–7.
Chan JM, Shin LK, Jeffrey RB. Ultrasonography of abnormal neck lymph nodes. Ultrasound Q. 2007;23:47–54.
Nam SY, Shin JH, Ko EY, Hahn SY. A comparison of lymphocytic thyroiditis with papillary thyroid carcinoma showing suspicious ultrasonographic findings in a background of heterogeneous parenchyma. Ultrasonography. 2015;34:45–50.
Moon HJ, Kim EK, Kim MJ, Kwak JY. Lymphocytic thyroiditis on fine-needle aspiration biopsy of focal thyroid nodules: approach to management. AJR Am J Roentgenol. 2009;193:W345–9.
Sahlmann CO, Meller J, Siggelkow H, Homayounfar K, Ozerden M, Braune I, et al. Patients with autoimmune thyroiditis. Prevalence of benign lymphadenopathy. Nuklearmedizin. 2012;51:223–7.
Jones MR, Mohamed H, Catlin J, April D, Al-Qurayshi Z, Kandil E. The presentation of lymph nodes in Hashimoto’s thyroiditis on ultrasound. Gland Surg. 2015;4:301–6.
Caturegli P, De Remigis A, Rose NR. Hashimoto thyroiditis: clinical and diagnostic criteria. Autoimmun Rev. 2014;13:391–7.
Babli S, Payne RJ, Mitmaker E, Rivera J. Effects of chronic lymphocytic thyroiditis on the clinicopathological features of papillary thyroid cancer. Eur Thyroid J. 2018;7:95–101.
Matsubayashi S, Kawai K, Matsumoto Y, Mukuta T, Morita T, Hirai K, et al. The correlation between papillary thyroid carcinoma and lymphocytic infiltration in the thyroid gland. J Clin Endocrinol Metab. 1995;80:3421–4.
Loh KC, Greenspan FS, Dong F, Miller TR, Yeo PP. Influence of lymphocytic thyroiditis on the prognostic outcome of patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 1999;84:458–63.
Kim EY, Kim WG, Kim WB, Kim TY, Kim JM, Ryu JS, et al. Coexistence of chronic lymphocytic thyroiditis is associated with lower recurrence rates in patients with papillary thyroid carcinoma. Clin Endocrinol (Oxf). 2009;71:581–6.
Kashima K, Yokoyama S, Noguchi S, Murakami N, Yamashita H, Watanabe S, et al. Chronic thyroiditis as a favorable prognostic factor in papillary thyroid carcinoma. Thyroid. 1998;8:197–202.
Lee DH, Yoon TM, Kim HK, Lee JK, Kang HC, Lim SC. Intraoperative frozen biopsy of central lymph node in the management of papillary thyroid microcarcinoma. Indian J Otolaryngol Head Neck Surg. 2016;68:56–9.
Kim MJ, Kim CS, Kim JR, Park YS. Efficiency of intraoperative frozen section analysis of central neck lymph node dissection in patients with papillary thyroid carcinoma. Int J Surg Oncol. 2018;3: e67.
Ji YB, Lee DW, Song CM, Kim KR, Park CW, Tae K. Accuracy of intraoperative determination of central node metastasis by the surgeon in papillary thyroid carcinoma. Otolaryngol Head Neck Surg. 2014;150:542–7.
Gyorki DE, Untch B, Tuttle RM, Shaha AR. Prophylactic central neck dissection in differentiated thyroid cancer: an assessment of the evidence. Ann Surg Oncol. 2013;20:2285–9.
Nixon IJ, Wang LY, Ganly I, Patel SG, Morris LG, Migliacci JC, et al. Outcomes for patients with papillary thyroid cancer who do not undergo prophylactic central neck dissection. Br J Surg. 2016;103:218–25.
Hennessy M, Goldenberg D. The role of prophylactic central neck dissection in the treatment of differentiated thyroid cancer. Rambam Maimonides Med J. 2016;7:e0007.
Pacini F, Basolo F, Bellantone R, Boni G, Cannizzaro MA, De Palma M, et al. Italian consensus on diagnosis and treatment of differentiated thyroid cancer: joint statements of six Italian societies. J Endocrinol Invest. 2018;41:849–76.
Bozec A, Dassonville O, Chamorey E, Poissonnet G, Sudaka A, Peyrottes I, et al. Clinical impact of cervical lymph node involvement and central neck dissection in patients with papillary thyroid carcinoma: a retrospective analysis of 368 cases. Eur Arch Otorhinolaryngol. 2011;268:1205–12.
Calo PG, Pisano G, Medas F, Marcialis J, Gordini L, Erdas E, et al. Total thyroidectomy without prophylactic central neck dissection in clinically node-negative papillary thyroid cancer: is it an adequate treatment? World J Surg Oncol. 2014;12:152.
Giordano D, Valcavi R, Thompson GB, Pedroni C, Renna L, Gradoni P, et al. Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid. 2012;22:911–7.
Lee DY, Oh KH, Cho JG, Kwon SY, Woo JS, Baek SK, et al. The benefits and risks of prophylactic central neck dissection for papillary thyroid carcinoma: prospective cohort study. Int J Endocrinol. 2015;2015: 571480.
Acknowledgements
Not applicable.
Funding
This work had no specific funding.
Author information
Authors and Affiliations
Contributions
KB: Methodology, Software, Validation, Formal analysis, Investigation, Original Draft, Writing—Review and Editing. JSK: Conceptualization, Resources, Writing—Original Draft, Writing—Review and Editing, Supervision, Project administration. JL: Resources. AC: Visualization. J-HC: Resources, Visualization. J-HK: Resources, Visualization. YLO: Resources. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board at Samsung Medical Center (IRB number: 2020-06-146) and informed consent form was obtained from all subjects and/or their legal guardian(s). All methods were performed according to the relevant guidelines and regulations by including a statement in the Declarations section to this effect.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Back, K., Lee, J., Cho, A. et al. Is total thyroidectomy with bilateral central neck dissection the only surgery for papillary thyroid carcinoma patients with clinically involved central nodes?. BMC Surg 22, 251 (2022). https://doi.org/10.1186/s12893-022-01699-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-022-01699-5