Abstract
Background
Cumulating evidence indicates that the systemic inflammatory response (SIR) plays a crucial role in the prognosis of various cancers. We aimed to generate a preoperative risk grade (PRG) by integrating SIR markers to preoperatively predict the long-term prognosis of intrahepatic cholangiocarcinoma (ICC).
Methods
468 consecutive ICC patients who underwent hepatectomy between 2010 and 2017 were enrolled. The PRG and a nomogram were generated and their predictive accuracy was evaluated.
Results
The PRG consisted of two non-tumor-specific SIR markers platelet-to-lymphocyte ratio (PLR) and albumin (ALB), which were both the independent predictors of overall survival (OS). Multivariate analysis showed that the PRG was significantly associated with OS (PRG = 1: hazard ratio (HR) = 3.800, p < 0.001; PRG = 2: HR = 7.585, p < 0.001). The C-index of the PRG for predicting survival was 0.685 (95% CI 0.655 to 0.716), which was statistically higher than that of the following systems: American Joint Committee on Cancer (AJCC) 8th edition (C-index 0.645), Liver Cancer Study Group of Japan (LCSGJ) (C-index 0.644) and Okabayashi (C-index 0.633) (p < 0.05). Besides, the C-index of the nomogram only consisting of the tumor-specific factors (serum carcinoembryonic antigen, carbohydrate antigen 19-9, tumor number) could be improved to 0.737 (95% CI 0.062–0.768) from 0.625 (95% CI 0.585–0.665) when the PRG was incorporated (p < 0.001).
Conclusions
The PRG integrating two non-tumor-specific SIR markers PLR and ALB was a novel method to preoperative predicting the prognosis of ICC.
Similar content being viewed by others
Background
The intrahepatic cholangiocarcinoma (ICC) has been the second most common primary liver tumor after hepatocellular carcinoma, and accounts for 10% to 15% of all primary liver malignancies [1]. The incidence of ICC has been increased and may be as high as 1–2 per 100,000 persons [2, 3]. Complete surgical resection remains the only potentially curative treatment option [4]. Unfortunately, only about 20% to 40% of ICC patients have the chance to receive surgical resection and the prognosis is unsatisfactory, with a median survival ranging from 24 to 36 months [3, 5]. The long-term survival is worse for unresectable ICC patients, with 5-year survival rate less than 5% to 10% after diagnosis [6]. Although several studies have described some prognostic factors and developed the relative staging systems for classification of ICC to provide the information of anticipated long-term outcomes, no one has had the excellent prognostic discrimination of ICC [2]. What’s more, the majority of these factors are tumor-specific pathologic markers, which are only available after surgery [7, 8].
The systemic inflammatory response (SIR) could influence the occurrence, development and prognosis of cancer [9]. Cancer-related inflammation is currently recognized as the seventh hallmark of cancer [10]. Many studies have suggested that the prognostic SIR markers based on the circulating blood cells could predict the long-term outcomes of patients in various tumors [11, 12]. Among these SIR markers, the preoperative lymphocyte-to-monocyte ratio (LMR), neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) have been revealed to be associated with the prognosis of ICC [13, 14]. Besides, preoperative haemoglobin and serum albumin (ALB) levels are also reported as the prognostic predictors for long-term prognosis of cancers [11, 15]. However, there are few studies have evaluated the value of these markers as independent predictors analyzed together and the extent how to integrate them to strengthen the predictive ability for ICC patients.
Therefore, the objective of the present study was to generate a preoperative risk grade by integrating the prognostic SIR markers to preoperatively predict the long-term prognosis of ICC.
Methods
Study population
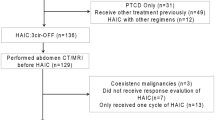
468 consecutive ICC patients who underwent curative liver resection at the Hepatic Surgery Center, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology (HUST) from January 2010 to December 2017 were enrolled retrospectively in this study. The inclusion criteria were: (1) ICC diagnosed pathologically; (2) liver function of Child–Pugh class A or class B; (3) no distant metastasis; (4) no previous treatment of ICC; (5) no history of other malignancies; and (6) detailed and precise follow-up records. This study was approved by the Institutional Review Boards of Tongji hospital, Tongji Medical College, HUST.
Surgical resection procedure
The indications for liver resection in our center included that the liver function was Child–Pugh class A or class B, the tumors was resectable based on the preoperative imaging and the residual liver volume was enough predicted by volumetric computed tomography (CT) [16]. All the operations were performed by experienced surgeons in open and laparoscopic hepatectomy. The intraoperative ultrasound was routinely performed to determine the tumor location and the relation to the major blood vessels. The Pringle maneuver was only used in cases with uncontrolled bleeding. Major resection was defined as equal to or more than three Couinaud segments resection.
Data collection and follow-up
The clinicopathological data including the SIR parameters of all patients were collected at admission and retrospectively reviewed and analyzed. Generally, the patients would receive the surgical treatment for ICC within 1 week after admission. After discharge, all patients were undertaken regular follow-up examination of serum α-fetoprotein (AFP), carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9), liver function and ultrasonogrphy every 4–6 weeks, and chest radiography every 8–12 weeks during the first 2 years. Thereafter, the intervals changed to 3–6 months. Investigations with CT, magnetic resonance imaging (MRI) or positron emission tomography (PET) were performed if recurrence was suspected. Once the intrahepatic tumor recurrence was identified, repeated liver resection, salvage transplantation, local ablation, transarterial chemoembolization (TACE), ethanol injection or systemic chemotherapy was performed based on the status of recurrence and the liver function.
Statistical analysis
All the data were analyzed with SPSS version 21.0 software (SPSS, Chicago, IL) and R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria). Continuous variables were expressed as the median with interquartile range (IQR), and categorical variables were expressed as the number and percentage. Prior to analyzing, the levels of tumor markers, including AFP, CEA and CA19-9, were log10 transformed. Comparisons of continuous variables were performed using Mann–Whitney U-test or Welch’s ANOVA, while Pearson chi-square analysis or Fisher’s exact test were used to compare categorical variables. The overall survival rates (OS) were estimated by the Kaplan–Meier method and were compared with the log-rank test. After the univariate analysis, the significant variables associated with the OS were then used for multivariate analysis using the Cox’s proportional hazards model. In both the univariate analysis and multivariate analysis, all the continuous clinicopathological characteristics were analyzed as continuous variables without dichotomization. After that, the software X-tile (Yale University, New Haven, CT, USA) was performed to determine the optimal cut-off value of PLR and ALB. The variables independently associated with OS were used to create a nomogram by R software using “rms” package. Calibration plots were generated to examine the performance characteristics of the predictive nomogram. The Concordance index (C-index) was measured and compared between the nomogram-predicted and observed Kaplan–Meier estimates of survival probability. The C-index ranges from 0.5 (no predictive power) to 1 (perfect prediction) [17]. p < 0.05 was considered to be significant difference.
Results
Clinicopathological characteristics
The clinicopathological characteristics of the patients were summarized in Table 1. Totally 468 patients were enrolled in the present study. The median age was 58 (IQR: 51–65). There were more male patients (282, 60.3%) than female patients (186, 39.7%). Median LMR, NLR and PLR were 3.3 (IQR: 2.1–4.8), 2.4 (IQR: 1.7–3.7) and 154.8 (IQR: 102.0–245.3), respectively. 107 (22.9%) patients had more than one tumor and 208 (44.4%) patients had tumors with diameter larger than 5 cm. Patients with vascular invasion (VI) and lymph node metastasis were 100 (21.4%) and 158 (33.8%), respectively. Most of patients had moderate differentiated tumor (346, 73.9%). More than half of patients received major hepatectomy (256, 54.7%). 134 (28.6%) patients had intraoperative blood transfusion and 90 (19.2%) patients received adjuvant chemotherapy.
Development of the preoperative risk grade with SIR markers for preoperatively predicting the long-term prognosis of ICC
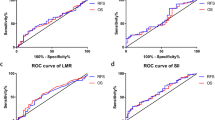
The 1-, 3-, and 5-year OS of the patients were 60.7%, 43.1% and 31.3%, respectively. Univariate analysis showed that alanine aminotransferase (ALT), ALB, PLR, CEA and CA19-9, tumor number, VI and lymph node metastasis were significantly associated with the OS, while just the ALB, PLR, CA19-9, tumor number, VI and lymph node metastasis could independently predict the OS in multivariate analysis (Table 2). All those significant variables, except the ALB and the PLR, were tumor-related factors, and have been commonly considered to be associated with the long-term prognosis of ICC. The ALB and the PLR were two SIR markers, which could be detected preoperatively. Therefore, we tried to generate a preoperative risk grade (PRG) by integrating those two non-tumor-specific SIR markers to preoperatively predict the long-term prognosis of ICC. The optimal cutoff levels of the PLR and the ALB were 143.5 and 40.0 g/L, respectively, using the software X-tile. The OS was significant different between the different levels of the PLR, as well as the ALB (p < 0.001) (Fig. 1a, b). Thus, there were four subgroups when integrating the PLR and the ALB. Significant difference of OS existed among the four subgroups (p < 0.001), except between the subgroup PLR < 143.5 and ALB < 40 g/L and the subgroup PLR ≥ 143.5 and ALB ≥ 40 g/L (p = 0.066) (Fig. 1c). Therefore, we generated a PRG, which were defined as the follows: patients with PLR < 143.5 and ALB ≥ 40 g/L were defined as grade 0; patients with PLR < 143.5 and ALB < 40 g/L or PLR ≥ 143.5 and ALB ≥ 40 g/L were defined as grade 1; and patients with PLR ≥ 143.5 and ALB < 40 g/L were defined as grade 2 (see Additional file 1: Table S1). The patients with higher PRG had higher levels of NLR, PLR, AFP, CEA and CA19-9, and had more possibility of VI, and lymph node metastasis (all p < 0.05). Besides, the ALT, ALB, TBIL, Child–Pugh grade, LMR and tumor diameter were also associated with the PRG (all p < 0.001) (Table 3).
Kaplan–Meier analysis of patient survival with different levels of platelet to lymphocyte ratio (PLR), albumin (ALB) and the combination of them. a Overall survival (OS) between patients with PLR ≥ 143.5 and PLR < 143.5 (p < 0.001); b OS between patients with ALB < 40 g/L and ALB ≥ 40 g/L (p < 0.001); OS between the four subgroups with different combination of PLR and ALB (PLR < 143.5 and ALB < 40 g/L vs PLR ≥ 143.5 and ALB ≥ 40 g/L p = 0.066, all other p < 0.05)
Comparison of the predictive accuracy for OS between the PRG and three conventional staging systems of ICC
Kaplan–Meier analysis showed that a significant difference of OS exited among the three PRG subgroups (p < 0.001) (Fig. 2a). Besides, multivariate analysis revealed that the PRG was significantly associated with the OS (PRG = 1: hazard ratio (HR) = 3.800, p < 0.001; PRG = 2: HR = 7.585, p < 0.001) (Table 4). Both the American Joint Committee on Cancer (AJCC) 8th edition staging system (p < 0.05) (Fig. 2b) and the Liver Cancer Study Group of Japan (LCSGJ) staging system (p < 0.05) (Fig. 2c) showed good predictive accuracy for patients with different stages, while the OS showed no significant difference between the patients with stages II and stage III in the Okabayashi staging system (p = 0.626) (Fig. 2d). Furthermore, the C-index of the PRG for predicting the OS was 0.685 (95% CI 0.655 to 0.716), which was significantly higher than that of the AJCC 8th edition (C-index 0.645; 95% CI 0.612 to 0.679), the LCSGJ (C-index 0.644; 95% CI 0.611 to 0.678) and the Okabayashi (C-index 0.633; 95% CI 0.600 to 0.666) (p < 0.05). No significant difference of predictive accuracy was found among the three conventional staging systems (p > 0.05).
Predictive nomogram for the long-term prognosis of ICC
Cox’s proportional hazards model showed that the CEA, CA19-9, tumor number, VI, lymph node metastasis and the PRG were the independent prognostic predictors for ICC (p < 0.05) (Table 4). All those prognostic predictors, except the VI and lymph node metastasis, could be detected preoperatively, and were integrated to construct a nomogram for providing an effective way to preoperatively predict the long-term prognosis by a quantitative method (Fig. 3a). In internal validation, the calibration plots of the nomogram predicting 1-, 3- and 5-year survival performed well with the ideal model (Fig. 3b–d). Besides, the C-index of the multivariate prognostic model only consisting of the tumor-specific factors (CEA, CA19-9 and tumor number) could be improved to 0.737 (95% CI 0.062–0.768) from 0.625 (95% CI 0.585–0.665) when the PRG was incorporated (p < 0.001).
Nomogram for predicting 1-, 3- and 5-year overall survival (OS) of intrahepatic cholangiocarcinoma (ICC) patients. a Nomogram for predicting 1-, 3- and 5-year OS; calibration plot of nomogram for predicting patient survival at b 1-year, c 3-year and d 5-year. The 45-degree blue line represents the performance of the ideal model and the red line represents the performance of the proposed nomogram. Nomogram predicting OS is plotted on the x-axis and the actual OS is plotted on the y-axis. (CEA carcinoembryonic antigen, CA199 carbohydrate antigen 19-9, No tumor number, PRG preoperative risk grade)
Discussion
Surgery as the only effective treatment method could improve the long-term survival of patients with hilar cholangiocarcinoma and well-differentiated grading and R0 resection are significantly associated with a better outcomes for those patients [18]. Similarly, surgical resection remains the only potentially curative treatment option for ICC patients. However, only about 20% to 40% of the ICC patients are suitable to get surgical resection when diagnosed [3]. Even for these patients received hepatectomy, the long-term prognosis is still unsatisfactory with 5-year tumor recurrence rate 53% to 79% and the corresponding survival rate 23.0% to 35.2% [3, 4, 19]. In addition, major hepatic resection (54.7% in the present study) is commonly needed in resection of ICC and therefore associated with high risk of postoperative morbidity [8, 20]. Although several staging systems have been developed to predict the prognosis of ICC after liver resection, there still have some controversies over the development and the implementation of these models [4, 19]. Thus, accurately preoperative assessment of the long-term survival benefit from hepatectomy would be particularly important for preoperative patients selection.
As Virchow firstly described the links between cancer and inflammation in 1876, cumulating evidence has suggested that inflammation played an important role in tumors [9]. The SIR markers, such as C-reactive protein (CRP), ALB, LMR, NLR and PLR, have been reported as the independent prognostic predictors of various solid tumors [12, 21,22,23,24,25]. In the present study, we evaluated the relationship of clinicopathological characteristics and the long-term prognosis of 468 ICC patients, and found that the PLR and the ALB, two non-tumor-specific SIR markers, were significantly associated with OS. Further, we generated a novel PRG by integrating the PLR and the ALB after dichotomization, and found a significant difference of OS exited among the three PRG subgroups. Cox’s proportional hazards model showed that the PRG was an independent predictor of OS. Besides, the patients with higher PRG tended to have higher levels of CEA and CA19-9, and have greater possibility of VI and lymph node metastasis, all of which had been widely considered to be associated with poor prognosis of ICC and were the indications of and systemic therapy for ICC [3, 4, 26, 27]. Therefore, we believe that the ICC patients with high PRG should be advised to receive the neoadjuvant or prolonged systemic therapy to improve the long-term prognosis, although which need more studies to validate. Although several previous studies have reported the relationship between the PLR and hepato-pancreatico-biliary malignancies, only Chen and colleagues have reported that the PLR was an independent adverse prognostic factor for survival of ICC [13, 24, 28]. The ALB has been widely reported to be associated with the long-term outcomes of various cancers, including ICC [29, 30]. Inflammation-based scores consisting of CRP and ALB as the Glasgow prognostic score have been proven to be significantly associated with survival in various cancers [31, 32]. Besides, Saito and colleagues have reported that a prognostic scoring system, consisting of PLR, CRP, ALB and CEA, could predict the postoperative survival after resection of perihilar cholangiocarcinoma [29]. However, to our knowledge, the present study is the first time to evaluate the prognostic value of the PLR and the ALB in ICC.
To date, the conventional staging systems of ICC include the AJCC 8th, LCSGJ and Okabayashi. In the present study, all the three staging systems performed well in predicting the OS of ICC, except the Okabayashi staging system for no significant difference of OS existing between the patients with stages II and stage III. However, the prognostic prediction of ICC is traditionally based on the tumor-specific factors such as tumor number, tumor size, VI, lymph node metastasis and extrahepatic metastasis, some of which are only available after surgery. Whereas, the circulating platelet and lymphocyte of PLR, and serum albumin adopted in the PRG are routinely detected before surgery in clinical setting. Thus, PRG is an accessible and accurate method to preoperatively predict the long-term prognosis of ICC patients. A nomogram consisting of CEA, CA19-9, tumor number and PRG, which were the independent predictors of OS and could be detected preoperatively, were generated and performed well in internal validation for predicting the prognosis. The PRG played an important role in the nomogram with C-index improved from 0.68 to 0.75 when the PRG was incorporated.
The biological reason behind the prognostic value of PRG should be elucidate by the function of platelet, lymphocytes and ALB, respectively. The platelet, reported in previous studies, could promote the tumor-induced angiogenesis and invasiveness of tumor cells [33]. Besides, elevated blood platelet count might also reflect the tumor-induced SIR because the inflammatory mediators released in difference type of cancers could stimulate the proliferation of platelet progenitor cells [34, 35]. On the other hand, lymphocytes could enhance tumor immune-surveillance to inhibit tumor cell proliferation, invasion, as well as metastasis [36]. Several studies have suggested that the absolute lymphocyte count can predict the OS of various cancers [37]. Accordingly, an elevated circulating platelet count may reflect the progression of tumor and a low circulating lymphocytes count might be responsible for the impaired and insufficient host immune response to malignancy. Thus, high PLR is associated with poor prognosis in various cancers, including the ICC in the present study [24, 38]. It has been reported that the ALB level might correlate with the systemic inflammation [30]. Besides, the ALB is commonly used as the marker for assessing patient’s nutritional status [30]. Malignancy frequently causes patient malnutrition reflected in hypoalbuminemia, which may in turn affect the host immune response to tumors [30, 39]. Thus, hypoalbuminemia suggests the systemic inflammation as well as immune suppression, and therefore associated with the prognosis of various cancers [25, 30, 40, 41].
The SIR markers reflected the biological characteristics of tumors and could be used to predict the long-term prognosis whether the tumor is resectable or unresectable [42, 43]. Studies have showed that the systemic therapy including chemotherapy, radiotherapy and the chemoradiotherapy benefits the unresectable ICC [44,45,46,47]. More recently, the molecularly targeted therapy and immnuotherapy for ICC have achieved inspiring outcomes [48,49,50,51]. Therefore, we think the ICC patients with high PRG should receive more aggressive systemic therapy, no matter if they would have an operation. In our center, locoregional therapies such as transcatheter arterial chemoembolization (TACE), radioembolization, or external-beam radiation therapy (EBRT) would be recommended to the unresectable advanced-stage ICC. Of cause, the gemcitabine plus cisplatin therapy as the current first-line cytotoxic chemotherapy for advanced-stage cholangiocarcinoma would be considered firstly. At the same time, the target therapy combination with the immunotherapy might be recommended to unresectable ICC, especially for those patients with resistance to chemotherapy or actionable mutations [52, 53].
There are limitations in this study. First of all, this is retrospective study containing a small sample of 468 ICC patients from a single-center. Second, although there is no significant difference of ALB between the patients with and without cirrhosis (37.6 ± 4.6 g/L vs 38.1 ± 4.9 g/L, p = 0.220) in the present study, the cirrhosis and the situation that some patients with cirrhosis may have received albumin treatment before admission for surgery might have influenced the level of ALB. Third, the external validation should have been conducted to further verify the prognostic predicting value of the nomogram and PRG, although the nomogram incorporating PRG performed well in internal validation. Finally, the other systemic inflammation response marker such as CRP was not analyzed because it is not detected routinely in our center.
Conclusions
We generated a novel prognostic predicting model PRG by integrating two non-tumor-specific SIR markers PLR and ALB. The PRG is an accessible and accurate method to preoperatively predict the long-term prognosis of ICC.
Availability of data and materials
Data are available upon request from the corresponding author.
Abbreviations
- ICC:
-
Intrahepatic cholangiocarcinoma
- SIR:
-
Systemic inflammatory response
- LMR:
-
Lymphocyte-to-monocyte ratio
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- ALB:
-
Albumin
- CT:
-
Computed tomography
- AFP:
-
α-Fetoprotein
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19-9 (CA19-9)
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography (PET)
- TACE:
-
Transarterial chemoembolization
- IQR:
-
Interquartile range
- OS:
-
Overall survival
- C-index:
-
Concordance index
- VI:
-
Vascular invasion
- ALT:
-
Alanine aminotransferase
- PRG:
-
Preoperative risk grade
- AJCC:
-
American Joint Committee on Cancer
- LCSGJ:
-
Liver Cancer Study Group of Japan
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Buettner S, Spolverato G, Kimbrough CW, Alexandrescu S, Marques HP, Lamelas J, Aldrighetti L, Gamblin TC, Maithel SK, Pulitano C, et al. The impact of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio among patients with intrahepatic cholangiocarcinoma. Surgery. 2018;164:411–8.
Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, Pawlik TM, Gores GJ. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60(6):1268–89.
Wang Y, Li J, Xia Y, Gong R, Wang K, Yan Z, Wan X, Liu G, Wu D, Shi L, et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol. 2013;31(9):1188–95.
Endo I, Gonen M, Yopp AC, Dalal KM, Zhou Q, Klimstra D, D’Angelica M, DeMatteo RP, Fong Y, Schwartz L, et al. Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg. 2008;248(1):84–96.
Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis. 2004;24(2):115–25.
Nathan H, Aloia TA, Vauthey JN, Abdalla EK, Zhu AX, Schulick RD, Choti MA, Pawlik TM. A proposed staging system for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2009;16(1):14–22.
Sasaki K, Margonis GA, Andreatos N, Bagante F, Weiss M, Barbon C, Popescu I, Marques HP, Aldrighetti L, Maithel SK, et al. Preoperative risk score and prediction of long-term outcomes after hepatectomy for intrahepatic cholangiocarcinoma. J Am Coll Surg. 2018;226(4):393–403.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7.
Mantovani A. Cancer: inflaming metastasis. Nature. 2009;457(7225):36–7.
Chang Y, An H, Xu L, Zhu Y, Yang Y, Lin Z, Xu J. Systemic inflammation score predicts postoperative prognosis of patients with clear-cell renal cell carcinoma. Br J Cancer. 2015;113(4):626–33.
Krenn-Pilko S, Langsenlehner U, Thurner EM, Stojakovic T, Pichler M, Gerger A, Kapp KS, Langsenlehner T. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer. 2014;110(10):2524–30.
Spolverato G, Maqsood H, Kim Y, Margonis G, Luo T, Ejaz A, Pawlik TM. Neutrophil-lymphocyte and platelet-lymphocyte ratio in patients after resection for hepato-pancreatico-biliary malignancies. J Surg Oncol. 2015;111(7):868–74.
Zhang C, Wang H, Ning Z, Xu L, Zhuang L, Wang P, Meng Z. Prognostic nutritional index serves as a predictive marker of survival and associates with systemic inflammatory response in metastatic intrahepatic cholangiocarcinoma. Onco Targets Ther. 2016;9:6417–23.
McMillan DC. The systemic inflammation-based Glasgow Prognostic Score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–40.
Huang ZY, Liang BY, Xiong M, Dong KS, Zhang ZY, Zhang EL, Li CH, Chen XP. Severity of cirrhosis should determine the operative modality for patients with early hepatocellular carcinoma and compensated liver function. Surgery. 2016;159(2):621–31.
Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15(4):361–87.
Ramacciato G, Nigri G, Bellagamba R, Petrucciani N, Ravaioli M, Cescon M, Del Gaudio M, Ercolani G, Di Benedetto F, Cautero N, et al. Univariate and multivariate analysis of prognostic factors in the surgical treatment of hilar cholangiocarcinoma. Am Surg. 2010;76(11):1260–8.
Si A, Li J, Xiang H, Zhang S, Bai S, Yang P, Zhang X, Xia Y, Wang K, Yan Z, et al. Actual over 10-year survival after liver resection for patients with intrahepatic cholangiocarcinoma. Oncotarget. 2017;8(27):44521–32.
Zhang XF, Bagante F, Chakedis J, Moris D, Beal EW, Weiss M, Popescu I, Marques HP, Aldrighetti L, Maithel SK, et al. Perioperative and long-term outcome for intrahepatic cholangiocarcinoma: impact of major versus minor hepatectomy. J Gastrointest Surg. 2017;21(11):1841–50.
Lin JX, Lin JP, Xie JW, Wang JB, Lu J, Chen QY, Cao LL, Lin M, Tu R, Zheng CH, et al. Prognostic importance of the preoperative modified systemic inflammation score for patients with gastric cancer. Gastric Cancer. 2018;22:403–12.
Kwon HC, Kim SH, Oh SY, Lee S, Lee JH, Choi HJ, Park KJ, Roh MS, Kim SG, Kim HJ, et al. Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers. 2012;17(3):216–22.
Liu Y, Chen S, Zheng C, Ding M, Zhang L, Wang L, Xie M, Zhou J. The prognostic value of the preoperative c-reactive protein/albumin ratio in ovarian cancer. BMC Cancer. 2017;17(1):285.
Kitano Y, Yamashita YI, Yamamura K, Arima K, Kaida T, Miyata T, Nakagawa S, Mima K, Imai K, Hashimoto D, et al. Effects of preoperative neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios on survival in patients with extrahepatic cholangiocarcinoma. Anticancer Res. 2017;37(6):3229–37.
Li C, Zhang XY, Peng W, Wen TF, Yan LN, Li B, Yang JY, Wang WT, Xu MQ, Chen LP. Preoperative albumin-bilirubin grade plus platelet-to-lymphocyte ratio predict the outcomes of patients with BCLC stage A hepatocellular carcinoma after liver resection. Medicine (Baltimore). 2018;97(29):e11599.
Weber SM, Ribero D, O’Reilly EM, Kokudo N, Miyazaki M, Pawlik TM. Intrahepatic cholangiocarcinoma: expert consensus statement. HPB (Oxford). 2015;17(8):669–80.
Shroff RT, Kennedy EB, Bachini M, Bekaii-Saab T, Crane C, Edeline J, El-Khoueiry A, Feng M, Katz MHG, Primrose J, et al. Adjuvant therapy for resected biliary tract cancer: ASCO clinical practice guideline. J Clin Oncol. 2019;37(12):1015–27.
Li W, Tao L, Lu M, Xiu D. Prognostic role of platelet to lymphocyte ratio in pancreatic cancers: a meta-analysis including 3028 patients. Medicine (Baltimore). 2018;97(8):e9616.
Saito H, Noji T, Okamura K, Tsuchikawa T, Shichinohe T, Hirano S. A new prognostic scoring system using factors available preoperatively to predict survival after operative resection of perihilar cholangiocarcinoma. Surgery. 2016;159(3):842–51.
Shen J, Wen T, Li C, Yan L, Li B, Yang J. The prognostic prediction role of preoperative serum albumin level in patients with intahepatic cholangiocarcinoma following hepatectomy. Dig Dis. 2018;36(4):306–13.
Pan QX, Su ZJ, Zhang JH, Wang CR, Ke SY. Glasgow prognostic score predicts prognosis of intrahepatic cholangiocarcinoma. Mol Clin Oncol. 2017;6(4):566–74.
Yu X, Wen Y, Lin Y, Zhang X, Chen Y, Wang W, Wang G, Zhang L. The value of preoperative Glasgow Prognostic Score and the C-Reactive Protein to Albumin Ratio as prognostic factors for long-term survival in pathological T1N0 esophageal squamous cell carcinoma. J Cancer. 2018;9(5):807–15.
Suzuki K, Aiura K, Ueda M, Kitajima M. The influence of platelets on the promotion of invasion by tumor cells and inhibition by antiplatelet agents. Pancreas. 2004;29(2):132–40.
Klinger MH, Jelkmann W. Role of blood platelets in infection and inflammation. J Interferon Cytokine Res. 2002;22(9):913–22.
Alexandrakis MG, Passam FH, Moschandrea IA, Christophoridou AV, Pappa CA, Coulocheri SA, Kyriakou DS. Levels of serum cytokines and acute phase proteins in patients with essential and cancer-related thrombocytosis. Am J Clin Oncol. 2003;26(2):135–40.
Chen Q, Dai Z, Yin D, Yang LX, Wang Z, Xiao YS, Fan J, Zhou J. Negative impact of preoperative platelet-lymphocyte ratio on outcome after hepatic resection for intrahepatic cholangiocarcinoma. Medicine (Baltimore). 2015;94(13):e574.
Ege H, Gertz MA, Markovic SN, Lacy MQ, Dispenzieri A, Hayman SR, Kumar SK, Porrata LF. Prediction of survival using absolute lymphocyte count for newly diagnosed patients with multiple myeloma: a retrospective study. Br J Haematol. 2008;141(6):792–8.
Smith RA, Bosonnet L, Raraty M, Sutton R, Neoptolemos JP, Campbell F, Ghaneh P. Preoperative platelet-lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg. 2009;197(4):466–72.
Ohki S, Shibata M, Gonda K, Machida T, Shimura T, Nakamura I, Ohtake T, Koyama Y, Suzuki S, Ohto H, et al. Circulating myeloid-derived suppressor cells are increased and correlate to immune suppression, inflammation and hypoproteinemia in patients with cancer. Oncol Rep. 2012;28(2):453–8.
Liu X, Meng QH, Ye Y, Hildebrandt MA, Gu J, Wu X. Prognostic significance of pretreatment serum levels of albumin, LDH and total bilirubin in patients with non-metastatic breast cancer. Carcinogenesis. 2015;36(2):243–8.
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, O’Beirne J, Fox R, Skowronska A, Palmer D, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33(6):550–8.
Huh G, Ryu JK, Chun JW, Kim JS, Park N, Cho IR, Paik WH, Lee SH, Kim Y-T. High platelet-to-lymphocyte ratio is associated with poor prognosis in patients with unresectable intrahepatic cholangiocarcinoma receiving gemcitabine plus cisplatin. BMC Cancer. 2020;20(1):907.
Omichi K, Cloyd JM, Yamashita S, Tzeng C-WD, Conrad C, Chun YS, Aloia TA, Vauthey J-N. Neutrophil-to-lymphocyte ratio predicts prognosis after neoadjuvant chemotherapy and resection of intrahepatic cholangiocarcinoma. Surgery. 2017;162(4):752–65.
Cuneo KC, Lawrence TS. Growing evidence supports the use of radiation therapy in unresectable intrahepatic cholangiocarcinoma. Cancer J. 2016;22(4):243–4.
Strobel O, Büchler MW. Unresectable intrahepatic cholangiocarcinoma: 50 % resectability after neoadjuvant therapy. Chirurg. 2018;89(3):241.
Hong TS, Wo JY, Yeap BY, Ben-Josef E, McDonnell EI, Blaszkowsky LS, Kwak EL, Allen JN, Clark JW, Goyal L, et al. Multi-institutional phase II study of high-dose hypofractionated proton beam therapy in patients with localized, unresectable hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Clin Oncol. 2016;34(5):460–8.
Rahnemai-Azar AA, Weisbrod AB, Dillhoff M, Schmidt C, Pawlik TM. Intrahepatic cholangiocarcinoma: current management and emerging therapies. Expert Rev Gastroenterol Hepatol. 2017;11(5):439–49.
Mazzaferro V, El-Rayes BF, Droz Dit Busset M, Cotsoglou C, Harris WP, Damjanov N, Masi G, Rimassa L, Personeni N, Braiteh F, et al. Derazantinib (ARQ 087) in advanced or inoperable FGFR2 gene fusion-positive intrahepatic cholangiocarcinoma. Br J Cancer. 2019;120(2):165–71.
Piha-Paul SA, Oh D-Y, Ueno M, Malka D, Chung HC, Nagrial A, Kelley RK, Ros W, Italiano A, Nakagawa K, et al. Efficacy and safety of pembrolizumab for the treatment of advanced biliary cancer: results from the KEYNOTE-158 and KEYNOTE-028 studies. Int J Cancer. 2020;147(8):2190–8.
Gilbert JA. BGJ398 for FGFR-altered advanced cholangiocarcinoma. Lancet Oncol. 2018;19(1):e16.
Jing C-Y, Fu Y-P, Yi Y, Zhang M-X, Zheng S-S, Huang J-L, Gan W, Xu X, Lin J-J, Zhang J, et al. HHLA2 in intrahepatic cholangiocarcinoma: an immune checkpoint with prognostic significance and wider expression compared with PD-L1. J Immunother Cancer. 2019;7(1):77.
Chen W-X, Li G-X, Hu Z-N, Zhu P, Zhang B-X, Ding Z-Y. Significant response to anti-PD-1 based immunotherapy plus lenvatinib for recurrent intrahepatic cholangiocarcinoma with bone metastasis: a case report and literature review. Medicine. 2019;98(45):e17832.
Koay EJ, Odisio BC, Javle M, Vauthey J-N, Crane CH. Management of unresectable intrahepatic cholangiocarcinoma: how do we decide among the various liver-directed treatments? Hepatobiliary Surg Nutr. 2017;6(2):105–16.
Acknowledgements
Not applicable.
Funding
This work was supported by the State Key Project on Infectious Diseases of China (Grant number: 2018ZX10723204-003-002), the National Natural Science Foundation of China (Grant number: 81874149). The funding was mainly used for the study designation, data collection, analysis and manuscript writing in the current study.
Author information
Authors and Affiliations
Contributions
WGZ, XPC, JPZ and YC designed this study. JPZ, YC, JJW, JW, YW, SSC and YXZ collected the data and die the analysis. JPZ and YC wrote the draft. WGZ, XPC, JPZ and YC revised the draft. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Boards of Tongji hospital, Tongji Medical College, Huazhong University of Science and Technology (HUST). Written consent was given by the patients for their information to be stored in the hospital database and used for research.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
The definition of the preoperative risk grade.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, J., Chen, Y., Wang, J. et al. Preoperative risk grade predicts the long-term prognosis of intrahepatic cholangiocarcinoma: a retrospective cohort analysis. BMC Surg 21, 113 (2021). https://doi.org/10.1186/s12893-020-00954-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-020-00954-x