Abstract
Background
Multiple surgical interventions exist for the treatment of symptomatic knee osteoarthritis, but the surgeon and patient may often have difficulty deciding which interventions are the best option.
Methods
We conducted a systematic review to identify randomized clinical trials (RCTs) that compared complications, revisions, reoperations, and functional outcomes among TKA (total knee arthroplasty), UKA (unicompartmental knee arthroplasty), HTO (high tibial osteotomy), BCA (bicompartmental knee arthroplasty), BIU (bi-unicompartmental knee arthroplasty), and KJD (knee joint distraction). The PubMed, Embase, and Cochrane databases were reviewed for all studies comparing two or more surgical interventions. Direct-comparison meta-analysis and network meta-analysis (NMA) were performed to combine direct and indirect evidence. The risk of bias was assessed using the revised Cochrane risk of bias tool for RCTs.
Results
This NMA and systematic review included 21 studies (17 RCTs), with a total of 1749 patients. The overall risk-of-bias assessment of the RCTs revealed that 7 studies had low risk, 5 had some concerns, and 9 had high risk. SUCRA (the surface under the cumulative ranking curve) rankings revealed that KJD had the greatest risk of appearing postoperative complications, revisions, and reoperations, and UKA or TKA had the lowest risk. The majority of comparisons among various treatments showed no difference for functional outcomes.
Conclusion
Each surgical intervention is noninferior to other treatments in functional outcomes, but UKA and TKA are better options to treat OA according to SUCRA rankings by comparing complications, revisions, and reoperations. KJD is an imperfect option for treating OA. Other treatments should be carefully considered for each patient in accordance with their actual conditions. However, this conclusion is limited by the selection of reviewed publications and individual variation of surgical indications for patients.
Trial registration
This study was registered with Research Registry (reviewregistry1395).
Similar content being viewed by others
Introduction
Knee osteoarthritis (OA) is a common joint disease in older patients that may cause severe pain and lead to an increasing financial burden and a reduced quality of life [1]. Although knee OA may involve any one or all 3 compartments, up to 30% of patients have evidence of only single compartmental degeneration [2].
The optimal surgical treatment for OA of the knee remains in question. To date, several surgical solutions have been proposed to address OA, such as TKA (total knee arthroplasty), UKA (unicompartmental knee arthroplasty), HTO (high tibial osteotomy), BCA (bicompartmental knee arthroplasty), BIU (bi-unicompartmental knee arthroplasty), or KJD (knee joint distraction), disagreements often exist between surgeons regarding the best choice of procedure and the best decision for patients with OA [3].
For example, although TKA is a primary surgical treatment for OA, as many as 15-20% of patients are dissatisfied with their surgical outcome [4,5,6]. Good or excellent long-term results with high patient satisfaction were reported for UKA, but its survival has been found to be inferior to that of TKA [7,8,9,10]. Unlike TKA and UKA, HTO accomplishes the reconstruction of joint function by correcting varus malalignment; however, some HTOs may need a conversion to TKA due to the progression of OA, and TKA following HTO has worse outcomes and higher complications [11,12,13]. Compared to TKA, BCA is a less invasive procedure but might have a relevant change in the leg axis and poor long-term survivorship [14, 15]. BIU demonstrates good functional outcomes, but data on its long-term outcomes remain limited [16]. KJD is a new surgical joint-preserving treatment that also appears to be associated with joint tissue regeneration, but relevant evidence is sparse [17]. Hence, for surgical interventions for knee OA, there is high variation in treatment choice and little robust evidence to guide selection.
The purpose of the present study was to perform a systematic review and network meta-analysis (NMA) of randomized control trials (RCTs) comparing different surgical treatments (TKA, UKA, HTO, BCA, BIU, and KJD) and assessing their complications, revisions, reoperations, and functional outcomes.
Materials and methods
Study selection
This NMA is reported following the standards proposed by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [18]. This study was registered with Research Registry (reviewregistry1395). Two researchers independently performed the literature search, and any discrepancies were reappraised and arbitrated by a third investigator. The titles and abstracts were screened, and the full-text was reviewed whenever necessary to evaluate the eligibility of each study. The search was performed in PubMed, Embase, and the Cochrane Library Database through March 20, 2022. The search terms included: total knee replacement, unicompartmental joint replacement, high tibial osteotomy, bicompartmental knee arthroplasty, bi-unicompartmental knee arthroplasty, and knee joint distraction. Furthermore, the corresponding references of all included studies were manually screened according to the selection criteria for consideration of inclusion in the study. There was no restriction regarding the publication date.
Eligibility criteria
We included all multiarm RCTs of human subjects that compared complications, revisions, reoperations, and functional outcomes among TKA, UKA, HTO, BCA, BIU, or KJD with a minimum 1-year follow-up.
The exclusion criteria were as follows: (1) nonrandomized and nonclinical studies, (2) single-arm clinical trials, (3) case reports and series, (4) conference abstracts, and (5) non-English language publications.
Data extraction and risk of bias assessment
All relevant information regarding the study characteristics was collected: study design, population characteristics, surgical approaches, indications, prosthesis, clinical outcomes, and follow-up time points. Two independent reviewers extracted data using a predetermined data sheet and evaluated the risk of bias using the revised Cochrane risk of bias tool for randomized trials (ROB 2) [19]. In cases of disagreement, a third reviewer was consulted to reach an agreement. The clinical outcomes evaluated included complications, revisions, reoperations, and functional outcomes. The complications were defined as any issues related to the surgical procedure that might require readmission, reoperation, additional treatment or longer hospital stays. Postoperative death from any relevant cause was also considered as a complication. Revisions of UKA, HTO, BCA, BIU and KJD were defined as failures equating to revision to TKA. The reoperations were defined as any unscheduled operations resulting from surgical site complications, including irrigation and wound revision, debridement, implant revision, open reduction internal fixation, and others.
Statistical analysis
For dichotomous outcomes, the relative effect sizes were reported as odds ratios (ORs) with 95% confidence intervals (CIs). When the 95% CI of the OR contained 1, the comparison was considered to have no statistical significance. For direct comparisons, a conventional meta-analysis was conducted to synthesize the results using random-effects models as sensitivity analyses (Supplementary Figs. 1–3). An NMA using a frequentist approach with a random effects model was used to estimate direct and indirect comparisons. NMA aims to test whether superiority exists for one of the comparator interventions. The potential inconsistency between the indirect and direct comparisons was inferred by global inconsistency, local inconsistency (a node-splitting approach), and loop inconsistency. Heterogeneity was quantified using the tau value, and P < 0.05 was considered statistically significant. A global network diagram was used for each prespecified outcome to demonstrate direct comparisons between interventions. A comparative hierarchy was obtained by calculating the relative ranking probabilities between the effects of all interventions for the target outcomes and SUCRA (the surface under the cumulative ranking curve). The SUCRA value showed the percentage of procedural efficacy and safety of each treatment and ranged from 0 to 100%. Hence, the larger the SUCRA value, the higher the rank of the intervention, indicating generally a better or worse effect. The contribution plot for the network is summarized in Supplementary Fig. 4, and the size of each circle is proportional to the weight attached to each direct summary effect for the estimation of each network summary effect. The comparison-adjusted funnel plot was used to assess the possibility of publication bias (Supplementary Fig. 5). All statistical analyses were performed using Stata 14 software (StataCorp LP, USA).
Results
Literature review and risk of bias assessment
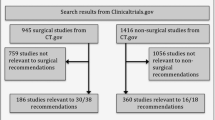
The initial literature search identified a total of 2916 studies. Then, 2883 studies were excluded after screening the titles and abstracts. Twenty-one studies were included in this review [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. Due to different durations of follow-up or clinical outcomes, studies 8–10 (one RCT) [27,28,29], 14–15 (one RCT) [33, 34] and 19–21 (two RCTs) [38,39,40] were all included to avoid omitting any clinical outcome. Finally, 21 studies were included in this review, with a total of 1749 patients. There were 709 patients treated using TKA, 711 treated using UKA, 153 treated using HTO, 91 treated using BCA, 42 treated using BIU, and 43 treated using KJD. The details of the literature review are presented in Fig. 1. The characteristics of the included studies are summarized in Table 1.
A network diagram summarizing the NMA geometry involving complications, revisions and reoperations is presented in Fig. 2A–C. In 14 studies [20,21,22,23, 25, 26, 29, 31,32,33, 35,36,37,38], the authors reported complications, and, in 13 studies [20,21,22,23, 25,26,27, 31, 33, 35,36,37,38], the authors reported revisions and reoperations. The results of the NMA, including the OR with 95% CIs, are reported in Figs. 3, 4 and 5, and the rank probabilities and cumulative probabilities are plotted in Fig. 6. Because an NMA involving functional outcomes was not possible due to the heterogeneity or deficiency of the functional data, a systematic review was performed for functional outcomes in all studies. The risk of bias of the RCTs is depicted in Fig. 7. Five studies (23.8%) showed some concerns, and 9 studies (42.9%) had a high risk for overall bias. In those RCTs, the majority of risk of biases arose from the randomization process, where it was unclear if the allocation sequence was random and concealed. All NMAs showed that heterogeneity and inconsistency were low.
Complications
Complications were reported in 14 studies [20,21,22,23, 25, 26, 29, 31,32,33, 35,36,37,38]. The NMA revealed that the likelihood of complications for each method was as follows: KJD (99.8%), BCA (68.0%), BIU (47.7%), TKA (41.6%), HTO (40.0%), and UKA (3.0%) (Fig. 6A and B). These findings indicate KJD had the greatest probability of postoperative complications, followed by BCA, while UKA had the lowest probability of postoperative complications. There were statistically significant differences in the incidence of complications when performing the following comparisons: KJD vs. TKA, UKA, HTO, BCA, and BIU, UKA vs. TKA, and BCA vs. UKA (Fig. 3). The above NMA results are consistent with direct comparisons among different interventions (Fig. 3 and Supplementary Fig. 1).
Revisions and reoperations
Revisions were reported in 13 studies [20,21,22,23, 25,26,27, 31, 33, 35,36,37,38]. The NMA SUCRA rankings indicating the likelihood of revisions were as follows: KJD (73.5%), BCA (71.3%), HTO (55.8%), BIU (41.7%), UKA (33.9%), and TKA (23.8%) (Fig. 6C and D), but there was no difference among all treatments (Fig. 4). No differences in the risk of revision among different treatments were observed with direct-comparison meta-analysis and NMA (Fig. 4 and Supplementary Fig. 2).
Reoperations were also reported in 13 studies [20,21,22,23, 25,26,27, 31, 33, 35,36,37,38]. The NMA SUCRA rankings indicating the likelihood of reoperations were as follows: KJD (94.8%), BCA (69.9%), HTO (52.0%), BIU (37.8%), TKA (24.3%), and UKA (21.2%) (Fig. 6E and F). There were statistically significant differences in the incidence of reoperations when comparing KJD with TKA, UKA, and HTO (Fig. 5). The above NMA results are consistent with the direct comparison among the different interventions (Fig. 5 and Supplementary Fig. 3).
Functional outcomes
Functional outcomes were reported in all studies. The follow-up durations of these RCTs ranged from was 1 to 15 years. The majority of comparisons among various treatments showed no difference for functional outcomes in Table 2. Compared with TKA, only one RCT (1/8) definitely showed that UKA had a better functional enhancement after 3 years of follow-up [20] and three RCTs (3/8) revealed that UKA had a superior ROM (range of motion) [20, 21, 29]. For UKA vs. HTO, the functional outcomes were not different in all 3 RCTs [30,31,32]. During a follow-up period of 1 to 10 years, BCA and BIU resulted in similar clinical and functional scores as TKA in 5 studies [33,34,35,36,37]. KJD was noninferior to TKA and HTO in the primary functional outcomes in 3 studies [38,39,40], but a high incidence of pin track infection associated with KJD was found.
Discussion
To date, there has been no consensus regarding the best surgical option for symptomatic knee osteoarthritis. To assist in providing robust evidence to guide surgical selection for surgeons and patients, the current NMA of 21 studies involving 1749 participants compared 6 surgical interventions (TKA, UKA, HTO, BCA, BIU, and KJD) and revealed that UKA and TKA are better options to treat symptomatic knee osteoarthritis, according to SUCRA rankings. KJD has the highest incidence of complications, revisions, and reoperations, thereby limiting its application. To our knowledge, this is the first NMA to compare the impacts of six surgical methods on the treatment of symptomatic knee osteoarthritis.
Some similar findings were also observed in other assessments of syntheses studies:(1) Most evidence-based studies showed that UKA is a better option than TKA, such as Wilson et al. who reported that UKA had significantly shorter operating times and hospital stays, fewer complications, and quicker recovery, but the revision rates for TKA were low [41]; Migliorini et al. and Arirachakaran et al. also showed that UKA reported reduced survivorship but better clinical and functional performances than TKA [42, 43]; Chawla’s meta-analysis indicated that revisions of medial UKA and lateral UKA occur at an annual rate of 2.18 and 2.31-fold that of TKA, respectively [44]; Only one meta-analysis showed that there were no statistically significant differences between UKA and TKA in terms of function scores, complications and survivorships, but they still supported the routine use of UKA for OA because of shorter hospital stay, faster recovery and less need for rehabilitation [45]; and Tripathy et al. reported that patients with UKA are better able to forget about their artificial joint than patients with TKA [46]. The reason why the rate of revision of TKA is lower than that of UKA is controversial. Revision of unsatisfactory TKA has a lower frequency because the reason for unsatisfactory results is also not known, but replacing with another TKA is risky when the reason for revisions is unknown and the solution is the same as the original. Most unsatisfactory UKA can be revised with TKA, so the relatively high revision rate of UKA can also be explained. In addition, UKA also has an obvious drawback in which the revised UKA to TKA had inferior outcomes compared to those of the primary TKA; hence, primary TKA may be a preferable procedure to UKA for patients for whom UKA and TKA are both applicable [47,48,49]. (2) Several meta-analyses demonstrated that UKA resulted in better clinical outcomes, greater improvement in physical activity levels, and fewer postoperative complications than HTO [50,51,52], and HTO is more appropriate for younger patients whereas UKA is appropriate for older patients [52, 53]; The Postoperative rate of revision and complications did not differ significantly between UKA and HTO [54]. Nevertheless, TKA following HTO provides similar clinical outcomes compared to TKR without previous HTO, but the conversion process of HTO to TKR is technically challenging [13, 55, 56]. (3) The majority of meta-analyses showed that BCA did not prove to be an equivalent alternative to TKA in knee OA due to more postoperative complications and poorer long-term survivorship [15, 57, 58]. (4) Wada’s and Takahashi’s systematic reviews reported that bi-UKA or KJD is a feasible and viable surgical option for knee OA in carefully selected patients, but long-term outcomes remain limited [17]. Moreover, 74% of KJD patients had complications, and 56% experienced pin tract infections [38].
Combined with the aforementioned literature review and the analysis of this NMA, most surgical methods for patients with OA have little difference in postoperative functional recovery of the knee joint; hence, patients and surgeons should pay more attention to complications, revisions, and reoperations when multiple options are available. According to our analysis, UKA is the preferred treatment for medial compartment OA patients with appropriate indications, followed by TKA. HTO is suitable for younger patients. Because there is little evidence for the applications of BCA, BIU and KJD, their indications need to be strictly controlled. Clinical decision-making for surgical options of patients with OA is meant to be informed by the best medical evidence, clinical judgment, surgeon’s experience and patient requirements. Treatment options should be carefully considered for each patient in accordance with their individual requirements and actual condition.
Limitations
Our study has some limitations. First, to improve the quality of this NMA, only RCTs were included, which resulted in a small number of studies. There were few RCTs included, which might reduce the robustness of our conclusions, especially for BIU and KJD evaluations. Second, it is difficult to conduct an ideal RCT as a result of clinical ethics. The overall allocation process was unclear in most studies, leading to a moderate to high risk of selection bias. Third, these included RCTs varied in inclusion criteria, population demographics, end assessment points and methods, and varying degrees of statistical adjustment. Fourth, implant survival and revision rates are likely to be affected by the experience of the operating surgeon and hospital performing the procedure. Fifth, because only BIU was involved in lateral compartment OA, stratified analysis was not performed according to the number of affected compartments. Sixth, the conclusion is limited by the selection of reviewed publications and individual variation of surgical indications for patients. The strengths of this NMA are the comprehensive nature of the literature search along with the strict eligibility criteria, and only high-quality RCTs were included in the analysis.
Conclusions
This study may provide evidence to support informed shared decision-making in the care of patients with knee OA. Based on our analysis, any surgical intervention is noninferior to other treatments in functional outcomes, but UKA and TKA are better options to treat symptomatic knee osteoarthritis according to SUCRA rankings by comparing complications, revisions, and reoperations. KJD is an imperfect option for treating OA. It needs to be emphasized that other treatment options should be carefully considered for each patient in accordance with their individual requirements and actual condition. Moreover, further well-designed and large-scale clinical trials and systemic reviews are required to confirm our findings.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RCT:
-
randomized clinical trials
- TKA:
-
total knee arthroplasty
- UKA:
-
unicompartmental knee arthroplasty
- HTO:
-
high tibial osteotomy
- BCA:
-
bicompartmental knee arthroplasty
- BIU:
-
bi-unicompartmental knee arthroplasty
- KJD:
-
knee joint distraction
- NMA:
-
network meta-analysis
- OA:
-
osteoarthritis
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- ROB2:
-
the revised Cochrane risk of bias tool for randomized trials
- Cis:
-
confidence intervals
- SUCRA:
-
the surface under the cumulative ranking curve
- ROM:
-
range of motion
References
Mahmoudian A, Lohmander LS, Mobasheri A, Englund M, Luyten FP. Early-stage symptomatic osteoarthritis of the knee - time for action. Nat Rev Rheumatol. 2021;17(10):621–32. https://doi.org/10.1038/s41584-021-00673-4.
Ledingham J, Regan M, Jones A, Doherty M. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Ann Rheum Dis. 1993;52(7):520–6. https://doi.org/10.1136/ard.52.7.520.
Beard DJ, Holt MD, Mullins MM, Malek S, Massa E, Price AJ. Decision making for knee replacement: variation in treatment choice for late stage medial compartment osteoarthritis. Knee. 2012;19(6):886–9. https://doi.org/10.1016/j.knee.2012.05.005.
Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, Beard DJ. Knee replacement. Lancet. 2012;379(9823):1331–40. https://doi.org/10.1016/s0140-6736(11)60752-6.
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. https://doi.org/10.1007/s11999-009-1119-9.
Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee. 2014;21(1):180–4. https://doi.org/10.1016/j.knee.2013.08.004.
Panni AS, Vasso M, Cerciello S, Felici A. Unicompartmental knee replacement provides early clinical and functional improvement stabilizing over time. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):579–85. https://doi.org/10.1007/s00167-011-1613-y.
Knifsund J, Reito A, Haapakoski J, Niinimäki T, Eskelinen A, Leskinen J, Puhto AP, Kettunen J, Manninen M, Mäkelä KT. Short-term survival of cementless Oxford unicondylar knee arthroplasty based on the finnish Arthroplasty Register. Knee. 2019;26(3):768–73. https://doi.org/10.1016/j.knee.2019.03.004.
Niinimäki T, Eskelinen A, Mäkelä K, Ohtonen P, Puhto AP, Remes V. Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year finnish registry study. Clin Orthop Relat Res. 2014;472(5):1496–501. https://doi.org/10.1007/s11999-013-3347-2.
Collier MB, Eickmann TH, Sukezaki F, McAuley JP, Engh GA. Patient, implant, and alignment factors associated with revision of medial compartment unicondylar arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):108–15. https://doi.org/10.1016/j.arth.2006.04.012.
Katz MM, Hungerford DS, Krackow KA, Lennox DW. Results of total knee arthroplasty after failed proximal tibial osteotomy for osteoarthritis. J Bone Joint Surg Am. 1987;69(2):225–33.
Tunggal JA, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy. Int Orthop. 2010;34(2): 255 – 61. https://doi.org/10.1007/s00264-009-0819-9.
Sun X, Wang J, Su Z. A meta-analysis of total knee arthroplasty following high tibial osteotomy versus primary total knee arthroplasty. Arch Orthop Trauma Surg. 2020;140(4):527–35. https://doi.org/10.1007/s00402-020-03333-6.
Shamdasani S, Vogel N, Kaelin R, Kaim A, Arnold MP. Relevant changes of leg alignment after customised individually made bicompartmental knee arthroplasty due to overstuffing. Knee Surg Sports Traumatol Arthrosc. 2022;30(2):567–73. https://doi.org/10.1007/s00167-020-06271-3.
Amit P, Singh N, Soni A, Bowman NK, Maden M. Systematic review of modular bicompartmental knee arthroplasty for Medio-Patellofemoral Osteoarthritis. J Arthroplasty. 2020;35(3):893–899e3. https://doi.org/10.1016/j.arth.2019.09.042.
Wada K, Price A, Gromov K, Lustig S, Troelsen A. Clinical outcome of bi-unicompartmental knee arthroplasty for both medial and lateral femorotibial arthritis: a systematic review-is there proof of concept? Arch Orthop Trauma Surg. 2020;140(10):1503–13. https://doi.org/10.1007/s00402-020-03492-6.
Takahashi T, Baboolal TG, Lamb J, Hamilton TW, Pandit HG. Is knee joint distraction a viable treatment option for knee OA?-A literature review and Meta-analysis. J Knee Surg. 2019;32(8):788–95. https://doi.org/10.1055/s-0038-1669447.
Zorzela L, Loke YK, Ioannidis JP, Golder S, Santaguida P, Altman DG, Moher D, Vohra S. PRISMA harms checklist: improving harms reporting in systematic reviews. BMJ. 2016;352:i157. https://doi.org/10.1136/bmj.i157.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Wu LP, Mayr HO, Zhang X, Huang YQ, Chen YZ, Li YM. Knee scores of patients with non-lateral compartmental knee osteoarthritis undergoing Mobile, fixed-bearing unicompartmental knee and total knee arthroplasties: a Randomized Controlled Trial. Orthop Surg. 2022;14(1):73–87. https://doi.org/10.1111/os.13111.
Knifsund J, Niinimaki T, Nurmi H, Toom A, Keemu H, Laaksonen I, Seppänen M, Liukas A, Pamilo K, Vahlberg T, Äärimaa V, Mäkelä KT. Functional results of total-knee arthroplasty versus medial unicompartmental arthroplasty: two-year results of a randomised, assessor-blinded multicentre trial. BMJ open. 2021;11(6):e046731. https://doi.org/10.1136/bmjopen-2020-046731.
Beard DJ, Davies LJ, Cook JA, MacLennan G, Price A, Kent S, Hudson J, Carr A, Leal J, Campbell H, Fitzpatrick R, Arden N, Murray D, Campbell MK. The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet. 2019;394(10200):746–56. https://doi.org/10.1016/S0140-6736(19)31281-4.
Kulshrestha V, Datta B, Kumar S, Mittal G. Outcome of Unicondylar knee arthroplasty vs total knee arthroplasty for early medial compartment arthritis: a randomized study. J Arthroplasty. 2017;32(5):1460–9. https://doi.org/10.1016/j.arth.2016.12.014.
Murray DW, MacLennan GS, Breeman S, Dakin HA, Johnston L, Campbell MK, Gray AM, Fiddian N, Fitzpatrick R, Morris RW, Grant AM. A randomised controlled trial of the clinical effectiveness and cost-effectiveness of different knee prostheses: the knee arthroplasty trial (KAT). Health Technol Assess. 2014;18(19):1–235. https://doi.org/10.3310/hta18190.
Sun PF, Jia YH. Mobile bearing UKA compared to fixed bearing TKA: a randomized prospective study. Knee. 2012;19(2):103–6. https://doi.org/10.1016/j.knee.2011.01.006.
Costa CR, Johnson AJ, Mont MA, Bonutti PM. Unicompartmental and total knee arthroplasty in the same patient. J Knee Surg. 2011;24(4):273–8. https://doi.org/10.1055/s-0031-1280970.
Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. 2009;91(1):52–7. https://doi.org/10.1302/0301-620X.91B1.20899.
Weale AE, Murray DW, Newman JH, Ackroyd CE. The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br. 1999;81(5):790–5. https://doi.org/10.1302/0301-620x.81b5.9590.
Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br. 1998.80(5): 862-5, 1998. https://doi.org/10.1302/0301-620x.80b5.8835.
Börjesson M, Weidenhielm L, Mattsson E, Olsson E. Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5-year follow-up study. Knee. 2005;12(2):121–7. https://doi.org/10.1016/j.knee.2004.04.002.
Stukenborg-Colsman C, Wirth CJ, Lazovic D, Wefer A. High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-year follow-up prospective randomised study. Knee. 2001;8(3):187–94. https://doi.org/10.1016/s0968-0160(01)00097-7.
Weidenhielm L, Svensson OK, Broström L, Rudberg U. Change in adduction moment about the knee after high tibial osteotomy and prosthetic replacement in osteoarthrosis of the knee. Clin Biomech (Bristol Avon). 1992;7(2):91–6. https://doi.org/10.1016/0268-0033(92)90021-U.
Goh JKM, Chen JY, Yeo NEM, Liow MHL, Chia SL, Yeo SJ. Ten year outcomes for the prospective randomised trial comparing unlinked, modular bicompartmental knee arthroplasty and total knee arthroplasty. Knee. 2020;27(6):1914–22. https://doi.org/10.1016/j.knee.2020.08.013.
Yeo NE, Chen JY, Yew A, Chia SL, Lo NN, Yeo SJ. Prospective randomised trial comparing unlinked, modular bicompartmental knee arthroplasty and total knee arthroplasty: a five years follow-up. Knee. 2015;22(4):321–7. https://doi.org/10.1016/j.knee.2015.04.007.
Schrednitzki D, Beier A, Marx A, Halder AM. No major functional benefit after bicompartmental knee arthroplasty compared to total knee arthroplasty at 5-Year Follow-Up. J Arthroplasty. 2020;35(12):3587–93. https://doi.org/10.1016/j.arth.2020.07.003.
Engh GA, Parks NL, Whitney CE. A prospective randomized study of bicompartmental vs. total knee arthroplasty with functional testing and short term outcome. J Arthroplasty. 2014;29(9):1790–4. https://doi.org/10.1016/j.arth.2014.04.016.
Blyth MJG, Banger MS, Doonan J, Jones BG, MacLean AD, Rowe PJ. Early outcomes after robotic arm-assisted bi-unicompartmental knee arthroplasty compared with total knee arthroplasty: a prospective, randomized controlled trial. Bone Joint J. 2021;103–b(10):1561–70. https://doi.org/10.1302/0301-620X.103B10.BJJ-2020-1919.R2.
Jansen MP, Besselink NJ, van Heerwaarden RJ, Custers RJH, Emans PJ, Spruijt S, Mastbergen SC, Lafeber F. Knee joint distraction compared with high tibial osteotomy and total knee arthroplasty: two-year clinical, Radiographic, and biochemical marker outcomes of two randomized controlled trials. Cartilage. 2021;12(2):181–91. https://doi.org/10.1177/1947603519828432.
van der Woude JAD, Wiegant K, van Heerwaarden RJ, Spruijt S, van Roermund PM, Custers RJH, Mastbergen SC, Lafeber F. Knee joint distraction compared with high tibial osteotomy: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):876–86. https://doi.org/10.1007/s00167-016-4131-0.
van der Woude JA, Wiegant K, van Heerwaarden RJ, Spruijt S, Emans PJ, Mastbergen SC, Lafeber FP. Knee joint distraction compared with total knee arthroplasty: a randomised controlled trial. Bone Joint J. 2017.99-b(1): 51–58. https://doi.org/10.1302/0301-620X.99B1.BJJ-2016-0099.R3.
Wilson HA, Middleton R, Abram SGF, Smith S, Alvand A, Jackson WF, Bottomley N, Hopewell S, Price AJ. Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ. 2019;364:l352. https://doi.org/10.1136/bmj.l352.
Migliorini F, Tingart M, Niewiera M, Rath B, Eschweiler J. Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur J Orthop Surg Traumatol. 2019;29(4):947–55. https://doi.org/10.1007/s00590-018-2358-9.
Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J. Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol. 2015;25(5):799–806. https://doi.org/10.1007/s00590-015-1610-9.
Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD. Annual revision rates of partial versus total knee arthroplasty: a comparative meta-analysis. Knee. 2017;24(2):179–90. https://doi.org/10.1016/j.knee.2016.11.006.
Longo UG, Loppini M, Trovato U, Rizzello G, Maffulli N, Denaro V. No difference between unicompartmental versus total knee arthroplasty for the management of medial osteoarthtritis of the knee in the same patient: a systematic review and pooling data analysis. Br Med Bull. 2015;114(1):65–73. https://doi.org/10.1093/bmb/ldv009.
Tripathy SK, Varghese P, Srinivasan A, Goyal T, Purudappa PP, Sen RK, Chandrappa MH. Joint awareness after unicompartmental knee arthroplasty and total knee arthroplasty: a systematic review and meta-analysis of cohort studies. Knee Surg Sports Traumatol Arthrosc. 2021;29(10):3478–87. https://doi.org/10.1007/s00167-020-06327-4.
Lee JK, Kim HJ, Park JO, Yang JH. Inferior outcome of revision of unicompartmental knee arthroplasty to total knee arthroplasty compared with primary total knee arthroplasty: systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26(11):3403–18. https://doi.org/10.1007/s00167-018-4909-3.
Sun X, Su Z. A meta-analysis of unicompartmental knee arthroplasty revised to total knee arthroplasty versus primary total knee arthroplasty. J Orthop Surg Res. 2018;13(1):158. https://doi.org/10.1186/s13018-018-0859-1.
Zuo W, Ma J, Guo W, Zhang Q, Wang W, Liu Z. Comparison of the clinical outcomes of revision of failed UKAs to TKAs with primary TKAs: a systematic review and meta-analysis. Medicine. 2018;97(50):e13408. https://doi.org/10.1097/MD.0000000000013408.
Han SB, Kyung HS, Seo IW, Shin YS. Better clinical outcomes after unicompartmental knee arthroplasty when comparing with high tibial osteotomy. Medicine. 2017;96(50):e9268. https://doi.org/10.1097/MD.0000000000009268.
Belsey J, Yasen SK, Jobson S, Faulkner J, Wilson AJ. Return to physical activity after high tibial osteotomy or unicompartmental knee arthroplasty: a systematic review and Pooling Data Analysis. Am J Sports Med. 2021;49(5):1372–80. https://doi.org/10.1177/0363546520948861.
Santoso MB, Wu L. Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review. J Orthop Surg Res. 2017;12(1):50. https://doi.org/10.1186/s13018-017-0552-9.
Spahn G, Hofmann GO, von Engelhardt LV, Li M, Neubauer H, Klinger HM. The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):96. https://doi.org/10.1007/s00167-011-1751-2.
Fu D, Li G, Chen K, Zhao Y, Hua Y, Cai Z. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty in the treatment of unicompartmental osteoarthritis: a meta-analysis. J Arthroplasty. 2013;28(5):759–65. https://doi.org/10.1016/j.arth.2013.02.010.
Ramappa M, Anand S, Jennings A. Total knee replacement following high tibial osteotomy versus total knee replacement without high tibial osteotomy: a systematic review and meta analysis. Arch Orthop Trauma Surg. 2013;133(11):1587–93. https://doi.org/10.1007/s00402-013-1838-y.
Chen X, Yang Z, Li H, Zhu S, Wang Y, Qian W. Higher risk of revision in total knee arthroplasty after high tibial osteotomy: a systematic review and updated meta-analysis. BMC Musculoskelet Disord. 2020;21(1):153. https://doi.org/10.1186/s12891-020-3177-9.
Ma JX, He WW, Kuang MJ, Sun L, Lu B, Wang Y, Ma XL. Efficacy of bicompartmental knee arthroplasty (BKA) for bicompartmental knee osteoarthritis: a meta analysis. Int J Surg. 2017;46:53–60. https://doi.org/10.1016/j.ijsu.2017.08.556.
Elbardesy H, Awad AK, McLeod A, Farahat ST, Sayed SZE, Guerin S, Harty J. Does bicompartmental knee arthroplasty hold an advantage over total knee arthroplasty? Systematic review and meta-analysis. SICOT J. 2021;7:38. https://doi.org/10.1051/sicotj/2021036.
Acknowledgements
Thank you to my wife for always encouraging and helping me.
Funding
This study was supported by the Natural Science Foundation of Gansu Province for Distinguished Young Scholars (22JR5RA943); Cuiying Scientific and Technological Innovation Program of Lanzhou University Second Hospital (CY2021-MS-A07).
Author information
Authors and Affiliations
Contributions
GB and XY were responsible for the conception and design, data synthesis and analysis, interpretation of data and drafting the manuscript. GB, LJ and TC screened the literature and assessed risk of bias independently. TY and ZX contributed to conception and design, and reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bin, G., Jinmin, L., Cong, T. et al. Surgical interventions for symptomatic knee osteoarthritis: a network meta-analysis of randomized control trials. BMC Musculoskelet Disord 24, 313 (2023). https://doi.org/10.1186/s12891-023-06403-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06403-z