Abstract
Background
There is no agreement about the best reconstructive option following resection of proximal humerus tumors. The purpose of this study was to compare the functional outcomes of endoprosthesis reconstruction versus nail cement spacer reconstruction after wide resection of proximal humeral tumors.
Methods
This retrospective comparative study included 58 patients with proximal humerus tumors who had undergone tumor resection and reconstruction with modular endoprosthesis (humeral hemiarthroplasties) or cement spacer. Medical records were reviewed for the epidemiological, clinical, radiological, and operative data. Lung metastasis, local recurrence, and complication were also reviewed. The functional outcome was evaluated using the Musculoskeletal Tumor Society scoring (MSTS) system.
Results
Nineteen patients with a mean age of 33.4 ± 17.5 years underwent reconstruction by modular endoprosthesis, and 39 patients with a mean age of 24.6 ± 14.3 years underwent reconstruction by cement spacer. The mean MSTS score was 24.8 ± 1.1 in the endoprosthesis group and 23.9 ± 1.4 in the spacer group, P = 0.018. Complications were reported in 5 (26.3%) patients in the endoprosthesis group and 11 (28.2%) patients in the spacer group, P = 0.879. There were no statistically significant differences in the functional outcomes in both patient groups with or without axillary or deltoid resection.
Conclusions
Both endoprostheses and cement spacers are durable reconstructions with almost equal functional outcomes with no added advantage of the expensive endoprosthesis.
Similar content being viewed by others
Background
The proximal humerus is a frequent location of primary malignant tumors and metastatic bone disease [1]. In the past, the main treatment options for these tumors were amputation and shoulder disarticulation [2]. Currently, limb salvage surgery with reconstruction is the treatment of choice as it offers functional and cosmetic advantages, in addition to social and emotional patient acceptance [3].
Limb salvage surgery for these tumors is challenging to orthopedic oncologists and usually requires wide resection and subsequent reconstruction [4]. There is no agreement about the best reconstruction method, and the literature is limited regarding the potential variations in functional results and survival of different constructs [1, 4].
After extensive bone resection, different reconstructive options are employed to regain limb function [3, 5,6,7,8,9]. Each reconstructive method has its advantages and disadvantages [10, 11]. Factors that should be considered when evaluating a reconstruction method include the ease of the procedure, functional outcome, morbidity, complications, and durability [2, 4].
Most frequently utilized are tumor endoprosthesis, arthrodesis implants, autografts, allografts, and custom-made implants [3, 9]. Arthrodesis reconstruction makes patients rely on the scapulothoracic motion for performing daily living activities. Functional results are comparable between arthrodesis and motion-preserving reconstructions and between primary or secondary arthrodesis [12, 13].
Currently, the proximal humerus endoprosthesis is most commonly used after resecting the humerus with good functional outcomes, but it has the disadvantage of being expensive [1, 5,6,7, 9, 12, 14,15,16,17,18]. Nail cement spacer reconstruction is the alternative way to reconstruction that benefits from cost-effectiveness [3].
Tumor resections have significant challenges due to the need to sacrifice part of the deltoid and rotator cuff muscles in addition to the axillary nerve in most cases to achieve a wide margin. This leads to a compromise in the shoulder function and motion [12, 19]. Even with preserving the axillary nerve, sacrificing parts of the rotator cuff will lead to deltoid muscle malfunction and insufficiency of the abductor mechanism with limitation of the shoulder motion [20, 21].
We hypothesized that in the absence of sufficient abductor mechanism following tumor resection, any mobile reconstructive option would just act as a hanger with a limited range of motion. Hence, an expensive hanger will provide the exact function of an inexpensive one.
This study aimed to compare the functional and oncological outcomes of endoprosthesis reconstruction versus nail cement spacer reconstruction following wide resection of proximal humeral tumors.
Methods
This comparative study was a prospective analysis of retrospective data of patients with primary malignant, benign aggressive, or metastatic tumors of the proximal humerus who had proximal humeral resection and reconstruction by modular tumor endoprosthesis (humeral hemiarthroplasties) or cement spacer. Surgeries were performed at a single orthopedic oncology center between September 2004 and December 2018. The minimum follow-up period was one year. Patients who did not complete the one-year follow-up, died of disease, or lost to follow-up, were excluded. Endoprosthesis reconstruction was in the form of humeral hemiarthroplasties and cement spacers were made of antibiotic-loaded polymethylmethacrylate (PMMA) augmented by a rush pin or Kuntscher nail inside it, acting as a stem. The study was conducted after approval from Menoufia University Institutional Review Board. Written informed consent was obtained from adult patients and from parents of patients below 16 years of age.
Medical records were reviewed for the epidemiological and clinical data, including the presentation, history of previous interventions, condition of the overlying skin, shoulder joint range of motion, and neurovascular examination.
Revision of available imaging studies, including full-length standard anteroposterior and lateral radiographs of the involved humerus, bone scintigraphy, chest computed tomography (CT), and magnetic resonance imaging (MRI) of the whole humerus was performed for assessment of the intramedullary and soft tissue extent of the tumor and relation of the tumor to the neurovascular structures. Lung metastasis was assessed in with chest CT scans.
Type of biopsy, whether open or closed, as well as neoadjuvant chemotherapy, were recorded. Histopathological reports following biopsy, as well as following tumor resection, were reviewed. Operative data included the approach, type of resection according to the classification system proposed by Malawer et al. [22], margin type, length of resection, reconstruction method, and implant type.
The functional outcomes were evaluated using the Musculoskeletal Tumor Society scoring (MSTS) system [23]. The postoperative shoulder range of motion was assessed. Any complications were recorded.
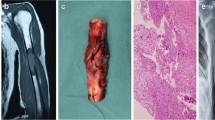
Oncological outcomes were also assessed, including local recurrence and lung metastasis. In addition, follow-up radiographs were evaluated for the implant position, any loosening, subluxation, or local recurrence, Figs. 1 and 2.
A 24-year-old female patient with osteosarcoma of the proximal humerus had undergone tumor resection and reconstruction with endoprosthesis. A Plain X-ray of the shoulder, anteroposterior view. B MRI axial view. C Postoperative X-rays, anteroposterior and lateral views. D Two-year follow-up X-rays, anteroposterior view
A 22-year-old female patient with giant cell tumor of the proximal humerus had undergone tumor resection and reconstruction with cement spacer. A Plain X-ray of the shoulder, anteroposterior view. B MRI sagittal view. C Postoperative X-rays, anteroposterior and lateral views. D Two-year follow-up X-rays, anteroposterior and lateral views
Statistical analysis
IBM SPSS version 25.0 (SPSS Inc., Armonk, NY) was used for the data analysis. Categorical data were compared using the chi-square or Fisher’s exact tests, while continuous data were compared using the student’s t-test or Mann-Whitney U test. Statistical significance was set at a P-value of less than 0.05.
Results
This study included 58 patients; 19 patients underwent reconstruction by modular endoprosthesis, while 39 patients underwent reconstruction by cement spacer. The endoprosthesis group included 9 (47.4%) males, and 10 (52.6%) females, with a mean age of 33.4 ± 17.5 (range, 13–77) years. The cement spacer group included 26 (66.7%) males, and 13 (33.3%) females, with a mean age of 24.6 ± 14.3 (range, 5–61) years, P = 0.061 and 0.159 for age and gender, respectively.
The most common diagnosis in the endoprosthesis group was chondrosarcoma (n = 7, 36.8%), followed by osteosarcoma (n = 5, 26.3%), while in the spacer group it was osteosarcoma (n = 17, 43.6%), followed by Ewing’s sarcoma (n = 12, 30.8%), P = 0.008.
Three (15.8%) and 8 (20.5%) patients were presented as recurrent cases in the endoprosthesis and spacer groups, respectively, P = 0.738. Seven (36.8%) and 11 (28.2%) patients were presented with a pathological fracture in the endoprosthesis and the spacer groups, respectively, P = 0.505, Table 1.
Operative results
The most commonly used approach was the anteromedial approach, 13 (68.4%) and 29 (74.4%) patients, followed by the deltopectoral, 6 (31.6%), and 8 (20.5%), in the endoprosthesis and spacer groups, respectively, P = 0.784.
Regarding the type of resection, in the endoprosthesis group, it was type I (intra-articular proximal humeral resection) in 18 (94.7%) patients and type V (extra-articular humeral and glenoid resection) in one (5.3%) patient. In the spacer group, it was type I in 36 (92.3%) patients and type V in 3 (7.7%) patients, P = 0.999.
A wide margin was achieved in 18 (94.7%) patients in the endoprosthesis group and 38 (97.4%) patients in the spacer group, P = 0.999.
The mean length of resection was shorter in the endoprosthesis group, 13.7 ± 3.5 (range, 8–20) cm, than in the spacer group, 14.9 ± 3.7 (range, 9–26) cm, but the difference was statistically insignificant, P = 0.250.
A significant part of the deltoid (at least the anterior and the middle parts) was resected in 13 (68.4%) and 28 (71.8%) patients in the endoprosthesis and spacer groups, respectively, P = 0.791.
The axillary nerve was resected in 3 (15.8%) patients in the endoprosthesis and 20 (51.3%) patients in the spacer group, P = 0.010.
Additionally, the musculocutaneous nerve was resected in one patient in the endoprosthesis group and two patients in the spacer group. The radial nerve was resected in two patients in the spacer group.
The operative time was not different between the two groups, 3.3 ± 0.9 (range, 2–5) hours in the endoprosthesis group and 3.4 ± 0.9 (range, 2–6) hours in the spacer group, P = 0.958, Table 2.
Functional outcomes
The mean follow-up period was 79 ± 57 (range, 15–168) months in the endoprosthesis group, and 42.4 ± 36 (range, 12–149) months in the spacer group, P = 0.020.
Overall, the mean MSTS score for all patients was 24.2 ± 1.4 (range, 22–27). The mean MSTS score in the endoprosthesis group was 24.8 ± 1.1 (range, 23–27) points, while it was 23.9 ± 1.4 (range, 22–27) points in the spacer group, P = 0.018.
The mean MSTS score was 24.1 ± 1.3 points in patients who had deltoid resection and 24.5 ± 1.5 points in patients without deltoid resection, P = 0.384.
The mean MSTS score was lower in patients with axillary nerve resection than in patients with preserved axillary nerve, 23.7 ± 1.2 and 24.6 ± 1.6 points, respectively, P = 0.019.
When analyzing each group separately, there were no statistically significant differences in the functional outcomes in patients with or without axillary or deltoid resection, Table 3.
At the latest follow-up, the mean active shoulder forward flexion was 30.3 ± 35.8 (range, 0° – 140°) and 17.3 ± 20.0° (range, 0° – 70°) in the endoprosthesis and spacer groups, respectively, P = 0.184. Four patients were able to achieve forward flexion of more than 60° (two in each group). The mean active shoulder extension was 48.0 ± 25.3° (range, 30° – 90°) and 16.6 ± 18.7° (range, 0° – 60°) in the endoprosthesis and spacer groups, respectively, P = 0.075. The mean active shoulder abduction was 33.4 ± 18.7° (range, 10° – 90°) and 16.6 ± 18.7° (range, 0° – 70°) in the endoprosthesis and spacer groups, respectively, P = 0.006. Three patients achieved more than 60° of abduction (two in the endoprosthesis group and one in the spacer group), Table 4.
In patients with axillary nerve resection (n = 23) and those with spared axillary nerve (n = 35), there was no statistically significant difference in outcomes and range of motion between endoprosthesis and spacer in either group. In patients with deltoid resection, the functional outcome and range of extension and abduction were significantly higher in the endoprosthesis group, P = 0.007, 0.044, and 0.002, respectively, Table 5.
Overall, local recurrence occurred in 6 patients; 2 patients in the endoprosthesis group, both were diagnosed as chondrosarcoma, and 4 patients in the spacer group; osteosarcoma (n = 3) and Ewing’s sarcoma (n = 1), P = 0.975.
Lung metastasis was recorded in 8 patients; 3 patients in the endoprosthesis group; all were diagnosed with chondrosarcoma, and 5 patients in the spacer group; osteosarcoma (n = 4), Ewing’s sarcoma (n = 1), P = 0.758, Table 4.
Complications
Overall, complications occurred in 5 (26.3%) patients in the endoprosthesis group and 11 (28.2%) patients in the spacer group, P = 0.879.
Three patients developed radial nerve palsy following nerve resection with the tumor; all were in the spacer group. Two patients had a deep infection, one in the endoprosthesis group, treated by debridement and insertion of cement spacer, and one in the spacer group managed by debridement and spacer revision. Skin sloughing occurred in one patient in the spacer group and was treated by debridement. Wound gapping occurred in one patient in the spacer group and was treated by secondary sutures. One patient in the spacer group had anterior dislocation 10 months postoperatively and was managed by open reduction. Two patients in the endoprosthesis group and two in the spacer group had proximal migration of prosthesis treated conservatively. One patient in the endoprosthesis group and one in the spacer group had downward subluxation treated conservatively. Two patients in the spacer group had broken rush pin, which was revised by intramedullary nail, Table 4.
The 3-year survival rates were 94.7 and 94.9% for the endoprosthesis and spacer groups, respectively, P = 0.592.
Discussion
Limb salvage surgery rather than amputation has become the ideal management option for malignant tumors of the proximal humerus, providing functional and cosmetic benefits [24, 25]. Several reconstructive options are available following tumor resection, including autologous grafts, osteoarticular allografts, endoprosthesis, allograft–prosthesis composite, or nail cement spacer [7, 9, 16, 26].
Resection of proximal humeral tumors often includes resection of parts of the deltoid and rotator cuff muscles as well as the axillary nerve, which impacts the expected shoulder function following reconstruction [20]. In our study, soft tissue reconstruction and attachment of remaining muscles to each other (for example, deltoid to pectoralis major, capsule and rotators to the implant, deltoid remnants to short biceps, and short biceps to long biceps) and to the prosthesis or spacer was aided by Ethibond and FiberWire sutures that were wrapped around the prosthesis or passed through the cement spacer before the setting of cement. Other methods of attachments were proline mesh and trevira tube to provide better anchorage of muscles, sometimes providing a sling to the acromion. Coverage of the implant or the spacer was the primary aim of avoiding dead space, even in case of inclusion of axillary nerve in the resection.
In this study, we compared the functional and oncological outcomes, complications, and survival rates of the endoprosthesis reconstruction versus nail cement spacer reconstruction following wide resection of proximal humeral tumors.
The mean follow-up period of the endoprosthesis group was significantly longer than the spacer group as we originally used to do only endoprosthesis. Over time we became more selective, reserving endoprosthesis for patients with minimal muscle resections, preserved axillary nerve, and potentially less expected functional deficit. Accordingly, most of the patients in the endoprosthesis group had chondrosarcoma, whereas the commonest diagnosis in the spacer group was osteosarcoma, followed by Ewing’s sarcoma. Moreover, the mean age in the spacer group was lower, as the group included many children in which the spacer was more appropriate and available to match the size of the humeral medulla as well as the glenoid dimensions. Both reconstructive techniques had almost equal operative time.
The average MSTS score for all patients in this study was 24.2 (80%). This was similar to other reports. Van de Sande et al. [16] compared the functional outcomes of proximal humeral reconstructions with modular tumor prosthesis, osteoarticular allograft, and allograft-prosthesis composite in 37 patients after tumor resection with a mean follow-up of 10 years. The average MSTS scores were 77% for the endoprosthesis reconstruction, 76% for the osteoarticular allograft, and 72% for the allograft-prosthetic composite groups; however, endoprosthesis reconstruction had the highest implant survival and the lowest complication rate [16]. A systematic review by Teunis et al. [27] compared the functional outcomes of different reconstruction methods, and the average MSTS scores ranged from 61 to 77% in the prostheses, 50 to 78% in the osteoarticular grafts, and from 57 to 91% the allograft-prosthesis composites studies. The conclusion was that both endoprosthesis reconstruction and allograft-prosthesis composites have comparable functional outcomes and survival rates, with avoidance of fractures observed with osteoarticular allografts [27].
Studies reporting on the outcome of spacers had inferior results. Kundu et al. [1] treated 14 patients with nail cement spacer reconstruction after tumor excision of the proximal humerus and reported a mean MSTS score of 19.09 with a mean follow-up of 30.14 months. Singh et al. [28] reported two cases with Ewing’s sarcoma and metastatic tumor of the proximal humerus treated with radical excision and cement spacer reconstruction and reported satisfactory shoulder, elbow, and hand function.
In our study, the endoprosthesis group had a slightly better functional outcome compared to the nail spacer group. Moreover, the shoulder range of motion was better in the endoprosthesis group. The active abduction, forward flexion, and extension were almost double, yet only the difference in the abduction was statistically significant. Rafalla and Abdullah [3] reported similar functional outcomes between endoprosthesis and spacers. In our study, the better functional outcome in the endoprosthesis group was probably due to selection bias as the endoprosthesis was done more in smaller tumors with lesser muscle resection and more patients with preserved axillary nerve.
When we divided patients into 2 groups; patients with axillary nerve resection and those with spared axillary nerve, there was no statistically significant difference in outcome between endoprosthesis and spacer in either group. Thus, the difference in function is probably influenced by the available muscles and nerves rather than the reconstructive modality.
If we excluded the patients with radial nerve palsy due to the inclusion of the radial nerve with the resected specimen, most of the complications were due to instability, dislocation, superior migration, or downward subluxation. There was no statistically significant difference in the complication rate between both groups. In our study, there was no dislocation in the endoprosthesis group and the dislocation rate in the spacer group was 2.6%. Our rates were lower than the rate of 7.5% reported in Scotti et al. [29], who treated 40 patients with proximal humeral metastasis with endoprosthesis reconstruction. Rafalla and Abdullah [3] reported subluxation in one (12.5%) case out of 8 cases that had endoprosthesis reconstruction. Potter et al. [9] reported a 31% (5 out of 16 patients) rate of subluxation or dislocation following endoprosthesis reconstructions of the proximal humerus.
Only 2 patients in this study developed infection, one in each group. The endoprosthesis was treated by debridement, removal, and insertion of cement spacer, and the infected spacer was managed by debridement and spacer revision. Our study showed that both reconstructive techniques had similar durability and comparable 3-year survival rates.
Although the aim of this study was not to evaluate the oncological outcome of the patients with proximal humeral tumors, there was no statistically significant difference in local recurrence and lung metastases between the endoprosthesis and spacer groups.
Even with preserving the axillary nerve, sacrificing parts of the rotator cuff will lead to deltoid muscle malfunction and insufficiency of the abductor mechanism with limitation of the shoulder motion. Thus, in the absence of sufficient abductor mechanism following tumor resection, any mobile reconstructive option would just act as a hanger with a limited shoulder range of motion.
This study has some limitations, including its retrospective nature, selection bias, and the relatively low number of patients in each group. However, the study was done in one institution by the same surgeons and with a reasonable follow-up. Longer periods of follow-up will test the durability of both reconstructive options.
Conclusions
Both endoprostheses and spacers are durable reconstructions that will provide the patient with almost equal functional outcomes. This outcome is better if the axillary nerve is preserved.
Availability of data and materials
The dataset analyzed in this study is available from the corresponding author on reasonable request.
References
Kundu ZS, Gogna P, Gupta V, Kamboj P, Singla R, Sangwan SS. Proximal humeral reconstruction using nail cement spacer in primary and metastatic tumours of proximal humerus. Strategies Trauma Limb Reconstr. 2013;8(3):149–54.
Yang Q, Li J, Yang Z, Li X, Li Z. Limb sparing surgery for bone tumours of the shoulder girdle: the oncological and functional results. Int Orthop. 2010;34(6):869–75.
Rafalla AA, Abdullah ESA. Endoprosthetic replacement versus cement spacer in reconstruction of proximal humerus after tumor resection: cost and benefits. J Orthop Surg (Hong Kong). 2017;25(2):2309499017713937.
Nota S, Teunis T, Kortlever J, Ferrone M, Ready J, Gebhardt M, et al. Functional outcomes and complications after oncologic reconstruction of the proximal humerus. J Am Acad Orthop Surg. 2018;26(11):403–9.
Abdeen A, Hoang BH, Athanasian EA, Morris CD, Boland PJ, Healey JH. Allograft-prosthesis composite reconstruction of the proximal part of the humerus: functional outcome and survivorship. J Bone Joint Surg Am. 2009;91(10):2406–15.
Amin SN, Ebeid WA. Shoulder reconstruction after tumor resection by pedicled scapular crest graft. Clin Orthop Relat Res. 2002;397:133–42.
Bilgin SS. Reconstruction of proximal humeral defects with shoulder arthrodesis using free vascularized fibular graft. J Bone Joint Surg Am. 2012;94(13):e94.
Bonnevialle N, Mansat P, Lebon J, Laffosse JM, Bonnevialle P. Reverse shoulder arthroplasty for malignant tumors of proximal humerus. J Shoulder Elb Surg. 2015;24(1):36–44.
Potter BK, Adams SC, Pitcher JD Jr, Malinin TI, Temple HT. Proximal humerus reconstructions for tumors. Clin Orthop Relat Res. 2009;467(4):1035–41.
Ogink PT, Teunissen FR, Massier JR, Raskin KA, Schwab JH, Lozano-Calderon SA. Allograft reconstruction of the humerus: complications and revision surgery. J Surg Oncol. 2019;119(3):329–35.
Liu T, Zhang Q, Guo X, Zhang X, Li Z, Li X. Treatment and outcome of malignant bone tumors of the proximal humerus: biological versus endoprosthetic reconstruction. BMC Musculoskelet Disord. 2014;15:69.
Dubina A, Shiu B, Gilotra M, Hasan SA, Lerman D, Ng VY. What is the Optimal Reconstruction Option after the resection of proximal humeral tumors? A systematic review. Open Orthop J. 2017;11:203–11.
Fuchs B, O'Connor MI, Padgett DJ, Kaufman KR, Sim FH. Arthrodesis of the shoulder after tumor resection. Clin Orthop Relat Res. 2005;436:202–7.
Hriscu M, Mojallal A, Breton P, Bouletreau P, Carret JP. Limb salvage in proximal humerus malignant tumors: the place of free vascularized fibular graft. J Reconstr Microsurg. 2006;22(6):415–21.
DeGroot H, Donati D, Di Liddo M, Gozzi E, Mercuri M. The use of cement in osteoarticular allografts for proximal humeral bone tumors. Clin Orthop Relat Res. 2004;427:190–7.
van de Sande MA, Dijkstra PD, Taminiau AH. Proximal humerus reconstruction after tumour resection: biological versus endoprosthetic reconstruction. Int Orthop. 2011;35(9):1375–80.
Goryn T, Pienkowski A, Szostakowski B, Zdzienicki M, Lugowska I, Rutkowski P. Functional outcome of surgical treatment of adults with extremity osteosarcoma after megaprosthetic reconstruction-single-center experience. J Orthop Surg Res. 2019;14(1):346.
Sirveaux F. Reconstruction techniques after proximal humerus tumour resection. Orthop Traumatol Surg Res. 2019;105(1S):S153–S64.
Bohler C, Bronimann S, Kaider A, Puchner SE, Sigmund IK, Windhager R, et al. Surgical and Functional Outcome after endoprosthetic reconstruction in patients with osteosarcoma of the humerus. Sci Rep. 2018;8(1):16148.
El Beaino M, Liu J, Lewis VO, Lin PP. Do early results of proximal humeral allograft-prosthetic composite reconstructions persist at 5-year followup? Clin Orthop Relat Res. 2019;477(4):758–65.
Streitbuerger A, Henrichs M, Gosheger G, Ahrens H, Nottrott M, Guder W, et al. Improvement of the shoulder function after large segment resection of the proximal humerus with the use of an inverse tumour prosthesis. Int Orthop. 2015;39(2):355–61.
Malawer MM. Tumors of the shoulder girdle. Technique of resection and description of a surgical classification. Orthop Clin North Am. 1991;22(1):7–35.
Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–6.
Ozturk R, Arikan SM, Togral G, Gungor BS. Malignant tumors of the shoulder girdle: surgical and functional outcomes. J Orthop Surg (Hong Kong). 2019;27(2):2309499019838355.
Chauhan A, Joshi GR, Chopra BK, Ganguly M, Reddy GR. Limb salvage surgery in bone tumors: a retrospective study of 50 cases in a single center. Indian J Surg Oncol. 2013;4(3):248–54.
Yao W, Cai Q, Wang J, Hou J. Mid- to long-term effects of two different biological reconstruction techniques for the treatment of humerus osteosarcoma involving caput humeri. World J Surg Oncol. 2020;18(1):23.
Teunis T, Nota SP, Hornicek FJ, Schwab JH, Lozano-Calderon SA. Outcome after reconstruction of the proximal humerus for tumor resection: a systematic review. Clin Orthop Relat Res. 2014;472(7):2245–53.
Singh KA, Shankar V, Mohanty SP. Reconstruction of proximal humerus using custom made acrylic prosthesis in malignant bone tumors. J Orthop Case Rep. 2016;6(5):65–8.
Scotti C, Camnasio F, Peretti GM, Fontana F, Fraschini G. Modular prostheses in the treatment of proximal humerus metastases: review of 40 cases. J Orthop Traumatol. 2008;9(1):5–10.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). No financial support was received for the current study.
Author information
Authors and Affiliations
Contributions
No financial support was received for the current study. W.A.E. designed the study, performed measurements, analysis and interpretation of data, and manuscript preparation. S. E did acquisition of data, performed measurements and manuscript preparation. I.T.B participated in study design, statistical analysis, and manuscript preparation. M.K.M contributed to study design, statistical analysis, manuscript preparation, and final manuscript revision. B.Z.H contributed to study design, and final manuscript revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. This study was approved by Menoufia University Institutional Review Board (IRB). Each patient gave informed consent to participate in this study.
Consent for publication
Consent to publish individual data was obtained by patients, or parents of minors.
Competing interests
All authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ebeid, W.A., Eldaw, S., Badr, I.T. et al. Outcomes of modular endoprosthesis reconstruction versus cement spacer reconstruction following resection of proximal humeral tumors. BMC Musculoskelet Disord 23, 484 (2022). https://doi.org/10.1186/s12891-022-05432-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05432-4