Abstract
Purpose
To evaluate the short-term clinical efficacy and complications of en bloc resection and intercalary prosthesis implantation for the treatment of humeral diaphyseal bone metastases.
Methods
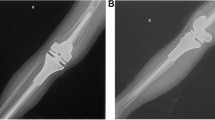
A total of 21 patients with humeral diaphyseal bone metastases treated with en bloc resection and intercalary prosthesis implantation from August 2014 to August 2019 were retrospectively analysed. The visual analogue scale (VAS), Musculoskeletal Tumour Society (MSTS) scale, International Society of Limb Salvage (ISOLS) scoring system, Karnofsky Performance Status (KPS) scale, and Nottingham Health Profile (NHP) scale were used to assess pain, limb function, and quality of life. Survival of the patients was analysed using the Kaplan-Meier method.
Results
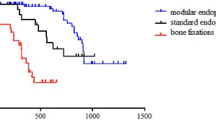
The patients were followed up for 12–57 months (mean: 22 months); the operative time was 68–114 minutes (mean: 76.24 min); the osteotomy length was 6.5–10 cm (mean: 8.02 cm); and the intra-operative blood loss was 95–125 ml (mean: 104.71 ml). At three, six and 12 months after surgery, the VAS and NHP scores were lower, whereas the MSTS, ISOLS, and KPS scores were higher than those before surgery, and the differences were statistically significant (P < 0.05). The survival time was four to 24 months (mean: 19.46 months). Thesix month and one year survival rates were 80.95% and 52.38%, respectively. During the follow-up period, no complications occurred except for aseptic prosthesis loosening in one patient.
Conclusions
En bloc resection and intercalary prosthesis implantation can reduce pain, improve limb function, prolong survival time, and improve quality of life in patients with humeral diaphyseal bone metastases.


Similar content being viewed by others
References
Frassica FJ, Frassica DA (2003) Metastatic bone disease of the humerus. J Am Acad Orthop Surg 11(4):282–288
Kask G, Nieminen J, Parry MC et al (2019) Revision rate of reconstructions in surgically treated diaphyseal metastases of bone. Eur J Surg Oncol 45(12):2424–2430
Casadei R, Drago G, Di Pressa F et al (2018) Humeral metastasis of renal cancer: surgical options and review of literature. Orthop Traumatol Surg Res 104(4):533–538
Wedin R, Hansen BH, Laitinen M et al (2012) Complications and survival after surgical treatment of 214 metastatic lesions of the humerus. J Shoulder Elb Surg 21(8):1049–1055
Janssen SJ, van Dijke M, Lozano-Calderón SA et al (2016) Complications after surgery for metastatic humeral lesions. J Shoulder Elb Surg 25(2):207–215
Zhao LM, Tian DM, Wei Y et al (2018) Diaphyseal segmental defect reconstruction. Orthop Surg 10(1):23–31
Sakellariou VI, Mavrogenis AF, Babis GC et al (2012) Comparison of four reconstructive methods for diaphyseal defects of the humerus after tumor resection. J Appl Biomech 28(5):568–578
Zhang JF, Wang F, Hu YC (2018) Reconstruction of humeral shaft defect with an intercalary endoprosthesis following resection of tumor. Orthop Surg 10(3):281–284
Zhao J, Xu M, Zheng K et al (2019) Limb salvage surgery with joint preservation for malignant humeral bone tumors: operative procedures and clinical application. BMC Surg 19(1):57
Huang HC, Hu YC, Lun DX et al (2017) Outcomes of intercalary prosthetic reconstruction for pathological diaphyseal femoral fractures secondary to metastatic tumors. Orthop Surg 9(2):221–228
Chin HC, Frassica FJ, Hein TJ et al (1989) Metastatic diaphyseal fractures of the shaft of the humerus. The structural strength evaluation of a new method of treatment with a segmental defect prosthesis. Clin Orthop Relat Res 248(11):231–239
Windhager R (2016) CORR Insights(®): outcomes of a modular intercalary endoprosthesis as treatment for segmental defects of the femur, tibia, and humerus. Clin Orthop Relat Res 474(2):549–550
Henry JC, Damron TA, Weiner MM et al (2002) Biomechanical analysis of humeral diaphyseal segmental defect fixation. Clin Orthop Relat Res 396(3):231–239
Aldlyami E, Abudu A, Grimer RJ et al (2005) Endoprosthetic replacement of diaphyseal bone defects. Long-term results. Int Orthop 29(1):25–29. https://doi.org/10.1007/s00264-004-0614-6
Benevenia J, Kirchner R, Patterson F et al (2016) Outcomes of a modular intercalary endoprosthesis as treatment for segmental defects of the femur, tibia, and humerus. Clin Orthop Relat Res 474(2):539–548
Ruggieri P, Mavrogenis AF, Bianchi G et al (2011) Outcome of the intramedullary diaphyseal segmental defect fixation system for bone tumors. J Surg Oncol 104(1):83–90
Sung YT, Wu JS (2018) The visual analogue scale for rating, ranking and paired-comparison (VAS-RRP): a new technique for psychological measurement. Behav Res Methods 50(4):1694–1715
Uehara K, Ogura K, Akiyama T et al (2017) Reliability and validity of the musculoskeletal tumor society scoring system for the upper extremity in Japanese patients. Clin Orthop Relat Res 475(9):2253–2259
Jones CW, Shatrov J, Jagiello JM et al (2017) Clinical, functional and radiological outcomes of extracorporeal irradiation in limb salvage surgery for bone tumours. Bone Joint J 99-B(12):1681–1688
Schag CC, Heinrich RL, Ganz PA (1984) Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol 2(3):187–193
Chung YL, Mitchell HL, Houssien DA et al (2001) A comparative study of outcome in myositis and other musculoskeletal disorders assessed using the Nottingham health profile. Clin Exp Rheumatol 19(4):447–450
Szczerba P, Guzik G, Bohatyrewicz A et al (2019) Bone diaphysis metastases, the ways and results of surgical treatment saving the joints. Ortop Traumatol Rehabil 21(2):107–115
Aponte-Tinao L, Farfalli GL, Ritacco LE et al (2012) Intercalary femur allografts are an acceptable alternative after tumor resection. Clin Orthop Relat Res 470(3):728–734
Chang DW, Weber KL (2005) Use of a vascularized fibula bone flap and intercalary allograft for diaphyseal reconstruction after resection of primary extremity bone sarcomas. Plast Reconstr Surg 116(7):1918–1925
Vijayan S, Bartlett W, Lee R et al (2011) Use of irradiated autologous bone in joint sparing endoprosthetic femoral replacement tumor surgery. Indian J Orthop 45(2):161–167
Puri A, Gulia A, Jambhekar N et al (2012) The outcome of the treatment of diaphyseal primary bone sarcoma by resection, irradiation and re-implantation of the host bone: extracorporeal irradiation as an option for reconstruction in diaphyseal bone sarcomas. J Bone Joint Surg (Br) 94(7):982–988
Lesensky J, Prince DE (2017) Distraction osteogenesis reconstruction of large segmental bone defects after primary tumor resection: pitfalls and benefits. Eur J Orthop Surg Traumatol 27(6):715–727
Zekry KM, Yamamoto N, Hayashi K et al (2019) Reconstruction of intercalary bone defect after resection of malignant bone tumor. J Orthop Surg (Hong Kong) 27(1):2309499019832970
Errani C, Ceruso M, Donati DM et al (2019) Microsurgical reconstruction with vascularized fibula and massive bone allograft for bone tumors. Eur J Orthop Surg Traumatol 29(2):307–311
Pesenti S, Peltier E, Pomero V et al (2018) Knee function after limb salvage surgery for malignant bone tumor: comparison of megaprosthesis and distal femur allograft with epiphysis sparing. Int Orthop 42(2):427–436. https://doi.org/10.1007/s00264-017-3608-x
Aurégan JC, Pietton R, Bégué T et al (2016) Effect of anatomic site and irradiation on the rates of revision and infection of allograft-prosthesis composites after resection of a primary bone tumor: a meta-analysis. Arch Orthop Trauma Surg 136(10):1371–1380
Sun W, Zan P, Ma X et al (2019) Surgical resection and reconstructive techniques using autologous femoral head bone-grafting in treating partial acetabular defects arising from primary pelvic malignant tumors. BMC Cancer 19(1):969
Pilge H, Ruppert M, Bittersohl B et al (2018) Lengthening of newly formed humerus after autologous fibula graft transplantation following intercalary tumor resection. J Pediatr Orthop B 27(4):322–325
Li Y, Yang Y, Huang Z et al (2020) Bone defect reconstruction with autologous bone inactivated with liquid nitrogen after resection of primary limb malignant tumors: an observational study. Medicine (Baltimore) 99(24):e20442
Yu XC, Xu SF, Xu M et al (2014) Alcohol-inactivated autograft replantation with joint preservation in the management of osteosarcoma of the distal femur: a preliminary study. Oncol Res Treat 37(10):554–560
Verdiyev V, Verdiyev F (2014) Application of distraction osteogenesis in managing bone cysts. J Orthop Traumatol 15(2):103–109
Zhao J, Yu XC, Xu M et al (2018) Intercalary prosthetic reconstruction for pathologic diaphyseal humeral fractures due to metastatic tumors: outcomes and improvements. J Shoulder Elb Surg 27(11):2013–2020
Zheng K, Yu XC, Hu YC et al (2019) Outcome of segmental prosthesis reconstruction for diaphyseal bone tumors: a multi-center retrospective study. BMC Cancer 19(1):638
Ma XL, Wang DB, Ma JX et al (2018) Custom-made prosthesis for reconstruction after radical resection for chondrosarcoma of manubrium. Orthop Surg 10(3):272–275
Ahlmann ER, Menendez LR (2006) Intercalary endoprosthetic reconstruction for diaphyseal bone tumours. J Bone Joint Surg (Br) 88(11):1487–1491
Damron TA, Leerapun T, Hugate RR et al (2008) Does the second-generation intercalary humeral spacer improve on the first? Clin Orthop Relat Res 466(6):1309–1317
Sewell MD, Hanna SA, McGrath A et al (2011) Intercalary diaphyseal endoprosthetic reconstruction for malignant tibial bone tumours. J Bone Joint Surg (Br) 93(8):1111–1117
McGrath A, Sewell MD, Hanna SA et al (2011) Custom endoprosthetic reconstruction for malignant bone disease in the humeral diaphysis. Acta Orthop Belg 77(2):171–179
Abudu A, Carter SR, Grimer RJ (1996) The outcome and functional results of diaphyseal endoprostheses after tumour excision. J Bone Joint Surg (Br) 78(4):652–657
Chen F, Pu F (2016) Safety of denosumab versus zoledronic acid in patients with bone metastases: a meta-analysis of randomized controlled trials. Oncol Res Treat 39(7–8):453–459
Zhang Z, Pu F, Shao Z (2017) The skeletal-related events of denosumab versus zoledronic acid in patients with bone metastases: a meta-analysis of randomized controlled trials. J Bone Oncol 9:21–24
Kimura T (2018) Multidisciplinary approach for bone metastasis: a review. Cancers (Basel) 10(6):156
Damron TA, Sim FH, Shives TC et al (1996) Intercalary spacers in the treatment of segmentally destructive diaphyseal humeral lesions in disseminated malignancies. Clin Orthop Relat Res 324(3):233–243
Schürmann M, Gradl G, Andress HJ et al (2000) Metastatic lesions of the humerus treated with the isoelastic diaphysis prosthesis. Clin Orthop Relat Res 380(11):204–214
Szendroi A, Dinya E, Kardos M et al (2010) Prognostic factors and survival of renal clear cell carcinoma patients with bone metastases. Pathol Oncol Res 16(1):29–38
Ratasvuori M, Wedin R, Hansen BH et al (2014) Prognostic role of en-bloc resection and late onset of bone metastasis in patients with bone-seeking carcinomas of the kidney, breast, lung, and prostate: SSG study on 672 operated skeletal metastases. J Surg Oncol 110(4):360–365
Yuasa T, Urakami S, Yamamoto S et al (2011) Treatment outcome and prognostic factors in renal cell cancer patients with bone metastasis. Clin Exp Metastasis 28(4):405–411
Baloch KG, Grimer RJ, Carter SR et al (2000) Radical surgery for the solitary bony metastasis from renal-cell carcinoma. J Bone Joint Surg (Br) 82(1):62–67
Lin PP, Mirza AN, Lewis VO et al (2007) Patient survival after surgery for osseous metastases from renal cell carcinoma. J Bone Joint Surg Am 89(8):1794–1801
Acknowledgements
We thank Editage for providing high-quality editing services.
Funding
The present study was supported by The National Natural Science Foundation of China (grant no. 81904231), the China Postdoctoral Science Foundation (grant no. 2020M672369), and the Postdoctoral Innovation Practice Post in Hubei Province (grant no. 34).
Author information
Authors and Affiliations
Contributions
Feifei Pu and Zhicai Zhang performed the study and wrote the manuscript. Feifei Pu and Zhicai Zhang made substantial contributions to conception and design of the study. Baichuan Wang and Jianxiang Liu were responsible for the design of the study. Jianxiang Liu and Zengwu Shao analysed the study data. Baichuan Wang and Zengwu Shao assisted with the statistical analysis. Jianxiang and Zengwu Shao critically revised the manuscript, provided final approval of the version to be published, and made substantial contributions to conception and design. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by the institutional review board of our hospital.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pu, F., Zhang, Z., Wang, B. et al. En bloc resection and intercalary prosthesis implantation for the treatment of humeral diaphyseal bone metastases. International Orthopaedics (SICOT) 45, 281–288 (2021). https://doi.org/10.1007/s00264-020-04845-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04845-x