Abstract
Background
Arthritis, regardless of cause, has significant physical, social and psychological impacts on patients. We aimed to identify the non-healthcare needs perceived by patients with inflammatory arthritis (IA) and osteoarthritis (OA), and to determine if these differ.
Methods
We electronically searched MEDLINE, PsycINFO, EMBASE and CINAHL (1990–2020) systematically to identify non-healthcare-related needs of people with IA or OA. All citations were screened and quality appraised by two reviewers. Data was extracted by a single reviewer.
Results
The search identified 7853 citations, with 31 studies included (12 for OA, 20 for IA). Six areas of need emerged and these were similar in both group These were: 1) Assistance with activities of daily living especially related to a lack of independence; 2) Social connectedness: need for social participation; 3) Financial security: worry about financial security and increased costs of health-seeking behaviours; 4) Occupational needs: desire to continue work for financial and social reasons, facilitated by flexibility of workplace conditions/environment; 5) Exercise and leisure: including limitation due to pain; 6) Transportation: limitations in ability to drive and take public transport due to mobility concerns. Many areas of need were linked; e.g. loss of employment and requiring support from family was associated with a sense of “failure” and loss of identity, as social isolation.
Conclusions
This review highlights the pervasive impact of arthritis on peoples’ lives, regardless of aetiology, albeit with a limited evidence base. Improved identification and targeting of non-healthcare needs of people with arthritis is likely to improve person-centred care.
Similar content being viewed by others

Significance and innovations
-
People with osteoarthritis and inflammatory arthritis perceive needs for support in many areas of life outside of direct healthcare, related to activities of daily living, exercise, social participation, environment, occupation and transport.
-
Despite differences in pathology, the non-healthcare-related needs of people with OA and IA are similar.
-
Improved identification and targeting of non-healthcare needs of people with arthritis is likely to improve person-centred care.
Background
Arthritis affects up to 80% of older adults in developed countries [1], with the two most common forms being osteoarthritis (OA) and rheumatoid arthritis (RA). Osteoarthritis accounts for 2.19% of all years lived with disability (YLDs) for any condition worldwide; while RA accounts for 0.28% of all YLDs [2]. The management of OA is limited with no disease modifying therapy available; the focus of therapy is symptom control and maintenance of function, with joint replacement an option for end-stage disease. For people living with OA, creating a healthcare and broader social environment that supports symptom management and capabilities to effectively self-manage a long-term disease is essential [3]. In contrast, biological therapies have improved morbidity and mortality outcomes in people with inflammatory arthritis (IA), particularly (RA) [4]. With effective treatments available for controlling disease activity, medical practitioners may focus care priorities in this area and other specific health needs (e.g. co-morbidity care), rather than broader health and social needs that may be relevant to the person. Notably, in people with other rheumatologic conditions, including lower back pain, addressing needs outside of direct medical care to provide holistic care, can improve quality of life [5].
While disease management may necessarily vary between individuals, all form of arthritis are associated with common impacts on people’s lives, in particular a loss of function, loss of dexterity, mental health sequelae and limitations in participation, often leading to unfavourable social consequences [6,7,8]. While these domains of impact are common, the nature of the impacts will vary between by disease. For example, those with inflammatory arthritis taking immunosuppressant medication may have specific occupational- and transport-related needs, to avoid situations that increase their risk of infection which are not relevant to those with osteoarthritis. To optimise holistic care, it is necessary to understand peoples’ non-healthcare related needs, beyond direct healthcare provision, such as the social determinants of health [9]. Accordingly, we aimed to identify current knowledge regarding the non-healthcare needs perceived by patients with OA and IA, and examine differences where identified.
Methods
A systematic scoping review was performed to provide an overview of the literature around the patient perceived non-healthcare needs of people with OA and IA, in line with the PRISMA guidelines for scoping reviews [10]. This was conducted within a larger project examining patients’ perceived needs relating to musculoskeletal health [11].
Search strategy
Medline, EMBASE, CINAHL and PsycINFO were electronically searched (1990 to September 2020) using a combination of keywords and MeSH terms related to perceived non-healthcare needs in people with OA and IA separately. A comprehensive search strategy was co-developed iteratively by a multidisciplinary team involving an academic librarian, input from a patient representative and four clinician researchers (Rheumatologists, Physiotherapist and public health physician) (Supplement Material Figures S1a, S1b, S2a, S2b, S3a, S3b, S4a, S4b).
Inclusion and exclusion criteria
English-language studies were included examining people older than 18 years with OA and IA. IA was defined as any joint disease where the primary mechanism was inflammation or synovitis, including RA, systemic lupus erythematosus (SLE) and psoriatic arthritis (PsA), excluding OA or crystal arthritis. Regarding OA, both clinical and radiological definitions were included. Studies had to report on perceived non-healthcare needs relevant to OA or IA. The concept of a “need” is complex, and currently without a consensus definition in the literature [12]. Broadly, we defined “need” in the context of health as a person’s desires, expectations and requirements [12], aligned with other work in this space [11, 13]. Non-healthcare services were defined as interventions, supports or structures not directly relating to healthcare, to support and assist people with functional limitation from their disease. Full text articles were included; no restrictions on study design were made to ensure a broad focus was maintained.
Study selection
Each title and abstract was screened for eligibility independently by 2 investigators (MS, SY, LC or JF). Full texts of studies meeting the inclusion criteria were retrieved and assessed (MS, LC or JF). Discrepancies were reviewed with an additional investigator (AW) to reach consensus.
Data extraction and analysis
Data were extracted by one author (MS, LC or JF) using a standardised data extraction form designed to capture demographic data, aims and description of study methods and outcomes. Included studies were reviewed by one author (MS, JF or AW) to identify aspects of non-healthcare needs, using principles of meta-ethnography to synthesise qualitative data [14]; the most common analytic approach for synthesising qualitative data from primary studies [15]. The principle of meta-ethnography is to empirically derive, though an inductive analytic frame, new concepts, interpretations, or theories that extend or go beyond findings of any individual study. In this way, a body of qualitative evidence contributes to the development of new themes or concepts [16]. The analytic approach used in this review followed the seven phases described by Noblit and Hare [17] and more recently described by France et al. [18]. Initially, one author (MS) reviewed each study in detail, reading the text several times to inductively derive an overarching framework of concepts and underlying themes from the yield of the qualitative studies. This framework was directly informed by data extracted from the primary studies and any pertinent points raised by the authors of the primary studies in the discussion, as recommended by France et al. [18]. In developing the framework of themes and subthemes each primary study was compared to the others to identify comparability, similarity or opposition based on grouping concepts. Once primary studies were translated into each other two senior rheumatologists (FC, AW) independently reviewed the framework of concepts and themes to ensure clinical meaningfulness and face validity.
Quantitative meta-analysis was not possible due to nature and heterogeneity of included studies. For this reason, quantitative data were reported narratively.
Risk of Bias assessments
Risk of bias assessments were performed independently by 2 investigators (JF, SA, AW or SY). Discrepancies were reviewed by a third investigator (AW) to reach consensus (Supplementary Material Table S1, S2). For qualitative studies, the Critical Appraisal Skills Programme (CASP) tool was used to assign risk of bias estimates [19]. For quantitative articles, the method described by Hoy et al. (Supplementary Material Appendix S1) was used to assess internal and external validity of studies [20]. Studies were deemed to be at low risk of bias if scoring eight or more “yes” answers, at moderate risk if scoring six to seven, and at high risk of bias when scoring less than six [20]. For qualitative studies, the Critical Appraisal Skills Programme (CASP) tool was used to assign risk of bias estimates [10].
Results
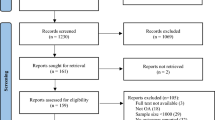
The search strategy identified 7853 potentially relevant abstracts, of which 891 were excluded as duplicates, and 6962 excluded after abstract screening (Fig. 1: PRISMA Diagram). Ninety-six manuscripts were retrieved for review, with 31 included in the final review. Twelve (39%) studies related to OA, and 20 (65%) related to IA, with one study involving participants with OA and IA with outcomes reported separately. Description of the included studies is presented in Table 1.
Twelve studies investigated the perceived non-healthcare needs of people with OA [21,22,23,24,25,26,27,28,29,30,31,32]. Included studies were all from high income countries except one (Nigeria [26]), involving 17–362 participants. Mean age ranged from 49.6 to 72.4 years, with studies including predominantly women (60–100% female). Participants were recruited from the ambulatory care settings in all studies; usually outpatient clinics (either rheumatology or orthopaedic [22, 28, 30, 31] or primary care [25].
Five studies included people with knee OA [22, 25, 26, 28, 32], four hand OA [24, 27, 29, 30], two a mixture of joint involvement [21, 23] and one did not specify [31]. OA was usually diagnosed clinically [21, 22, 24,25,26,27, 29,30,31,32]. OA was mild in two studies [28, 30] and end-stage in another [22] but most commonly severity was unspecified (9/12, 75%). Six studies used qualitative methods (semi-structured interviews [24, 25, 27, 28] or focus group discussions [22, 23], five quantitative methods [21, 26, 30,31,32], and one both [29]. Of qualitative studies, five were assessed as low risk of bias [22, 24, 25, 27, 28] and one moderate risk of bias [23] (Supplementary Material Table S1). Of quantitative studies, five were assessed as moderate risk of bias [21, 26, 29, 30, 32], and one at high risk of bias [31] (Supplementary Material Table S2).
Twenty studies discussed non-healthcare needs for IA [31, 33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51]. All but one study included predominantly female participants (58–100%) [41], with all studies from high-income countries. Included participants were generally over 50 years of age [31, 33,34,35,36,37,38,39,40, 42,43,44,45, 48, 49, 51], although in four studies mean age was in the 40s [41, 46, 47, 50]. IA was usually diagnosed clinically [31, 33, 35,36,37, 39, 40, 42,43,44,45,46,47,48,49,50]. RA was the most common diagnosis [34, 35, 37,38,39,40, 42,43,44,45,46,47,48, 50, 51] [33, 49], with participants usually recruited from outpatient clinics [31, 35, 36, 38, 40, 41, 43,44,45, 48,49,50]. Nine quantitative studies used questionnaires [31, 33, 37, 38, 40, 44, 46, 47, 51], while 11 qualitative studies used interviews [34,35,36, 39, 41, 42, 45, 48,49,50] or focus groups [43]. Of the qualitative studies, six were assessed as low risk of bias [34, 42, 45, 48,49,50] and five at moderate risk of bias [35, 36, 39, 41, 43] (Supplementary Material Table S1). Of the quantitative studies, one was assessed as low risk of bias [38], two at moderate risk of bias [44, 46] and six at high risk of bias [31, 33, 37, 40, 47, 51] (Supplementary Material Table S2).
Areas of need identified
This review identified six key areas of need in people with IA or OA, common to both groups (Table 2, Table 3).
-
1)
Activities of daily living (ADLs) both inside and outside the home
Ten OA studies (Table 2) [21, 22, 24,25,26,27,28,29, 31, 32] and 15 IA studies (Table 3) [23, 31, 33,34,35,36,37, 39, 42,43,44,45,46,47,48] discussed difficulties facing people regarding ADLs.
ADLs of people with OA were limited by symptoms [21, 32], including pain [28]. People with OA worried about needing help from others [21, 22, 24, 25, 28, 31]: 75% in one study [31]. For household chores, help was required either from within the family or external sources [22, 24, 25, 27, 28]. This sometimes contributed to a sense of “failure” to fulfil social obligations e.g. caring for children or partners [22]. People acknowledged that they may struggle to live alone [24]. Cleanliness and grooming were important to people with hand OA [24], who experienced difficulty with fine motor tasks including buttons and lacing shoes [27]. Moreover, hand OA limited the dexterity required for cell phones, cutlery and some payment systems (e.g. coins and notes) [24, 27]. Gadgets with an accessible design and assistive devices improved daily functioning [24, 29].
People with IA frequently received assistance with ADLs [31, 34, 35, 39, 42,43,44,45, 48]; up to 93% of people with RA [31]. Partners [42] or children [45] most commonly provided help. Participants disliked accepting assistance from children [34]. Daily activities, particularly housework, were difficult with IA [33, 34, 36, 37, 46, 51]; IA was associated with less enjoyment of life [37]. Pain and stiffness contributed to functional limitations [36, 48]. Functional difficulties could make people feel anxious, frustrated or “like a failure” [33]. Participants often lived alone (29%) [44] and worried about inability to obtain assistance when required [31]. Participants wanted to do more than they could [35]. Compared to amputees, people with IA were less independent and well-adjusted to their circumstances [23]. Participants wanted to tools to make ADLs easier [39], especially environmental modifications. Areas in the home, workplace and outdoors required modifications [23, 40]. Participants valued security and worried about falling victim to crime due to perceived invalidity [44].
-
2)
Social participation needs
Nine OA studies (Table 2) [22,23,24,25,26,27, 30,31,32] and 17 IA studies (Table 3) [33,34,35,36,37, 41,42,43,44, 46,47,48, 51, 53] identified issues relating to social participation and connectedness.
Of the OA studies, mobility restriction and lack of suitable transportation significantly limited social participation [24, 25]. Inability to participant in group activities restricted social contact [24], with family activities limited to avoid excluding family members [22]. Hand OA limited participants’ ability to conform to social norms [30] due to functional constraints [27], which could cause embarrassment [27]. Some participants worried about the appearance of their hands [30]. Strong social support was linked to better health perceptions [26]. Caring for grandchildren could be difficult, including limited ability to lift toddlers and change nappies [24, 25]. Both doctors and support networks sometimes failed to recognise OA as a “real” disease, contributing to communication difficulties [23]. People were frustrated by a lack of community support, and underestimation of pain and suffering [32]. Media coverage of, and research into OA was perceived as inadequate [23]. One study suggested that only 20% of people with OA desired access to support groups [31].
In people with IA, social connectedness [31, 35, 39,40,41, 43, 44, 48, 53] and peer support was critical. Loneliness and withdrawal were common [43, 44], especially for those living alone [44]. IA put strain on personal relationships [46] particularly ability to provide care for others [48], and relationships with partners including sexual function and intimacy [33, 46, 47]. Some experienced lowered mood due to pain [36]. Participants were desperate for support from family and often felt “alone” [37], needing to trust others to accept proffered support [35]. This was exacerbated by limitation of social activities [36, 51] and losing employment [43, 45]. Barriers to social connectedness included perceived lack of understanding [33, 35, 36, 43], financial difficulties, mobility problems and fear of falling victim to crime [44]. Overall, participants felt less able to participate in social events, community life and relationships [33, 36, 48]. Assistive devices made some participants feel embarrassed or “weird” [23]. Participants with PsA and foot involvement felt demoralised or stigmatised by their appearance and need for specialised footwear [36]. Participants were interested in self-help groups [31, 36], which helped with coping and self-management through support, recognition and legitimisation of personal experiences and problems [39, 43]. These groups facilitated participants building new relationships [39, 43], and proving that normality is possible [43]. Having relatives with the same condition helped with coping [36]. Peer groups supporting physical activity were desirable [40].
-
3)
Financial needs and security
Three OA studies (Table 2) [25, 27, 28] and three IA studies (Table 3) [31, 44, 46] investigated financial needs and security.
OA studies focussed on the cost of health-seeking behaviour [25] and need for financial security. Work capacity was limited by disease [27, 28].
In IA, financial stress was common [31, 44]. Income protection was accessed by 32% [46]. Participants from Estonia described financial concerns limiting their access to basic needs including food, running water and heating, as well as sociocultural experiences [44].
-
4)
Occupational needs
Four OA articles (Table 2) [24, 25, 28, 30] and 13 IA studies (Table 3) [31, 33, 36, 38, 39, 43,44,45,46,47, 50, 51] identified needs related to work.
People with OA wanted a flexible workplace [24, 25, 28] to facilitate work retention [24]. Flexibility entailed the need for regular breaks and environmental modification, although aides and environmental modifications were often not available [24]. Failure of these supports could require people to change employment [24, 25, 28]. Hand OA could limit work productivity [30].
IA often affected ability to work, particularly productivity, self-confidence, career progression or salary [33, 36, 46, 47]. However, people with IA valued working to maintain a normal life [31, 39, 43,44,45, 50], financial security [39, 44], self-esteem, identity [43] and social networks [43]. Disability pensions were seen as a “last resort” [39]. At least 34% percent experienced difficulties at work, increased absenteeism in 11% and premature retirement in 8–18% [33, 38] with 25% worrying about job losses [44]. The need for modified footwear impacts on job roles in those with PsA and foot disease (e.g. unable to wear dress shoes or safety boots) [36]. Factors improving work retention included physical ability [51], travel arrangements (parking, working from home) [50], flexibility of hours and conditions [45, 50] and modifications in the workplace [45, 50]. Participants wanted more information about their work-related rights [39, 50].
-
5)
Exercise and leisure related needs
Five OA studies (Table 2) [22, 24, 25, 28] identified barriers to exercise and leisure participation. Disease progression meant people needed to modify or swap exercise/leisure activities [24]. People worried about their inability to exercise [25], especially pain, inability to continue activities previously enjoyed [28, 32], missing out on activities with others [22] and needing to engage in more sedentary activities [24].
Seven studies investigated needs and attitudes of people with IA to exercise and leisure activities (Table 3) [34,35,36,37, 40, 47, 49]. Participants felt empowered by information about type and necessity of physical exercise [34]. In RA, physical, psychological, functional and social benefits from exercise were identified [35, 40]; exercise was identified as a critical part of self-management [49]. However, RA limited mobility and caused pain, restricting participation in specific exercises/sports [37, 40], with some activities wholly inaccessible [35]. Some participants found RA symptoms to be a motivator to be active [49]. Social, family and leisure activities were affected, limiting sports, fitness, hobbies and spontaneity [47]. Participants preferred options where physical activity served an additional purpose e.g. social contact, transportation, dog walking [49]. Participants identified a lack of RA-specific exercise programs, with exercise programs and instructors failing to consider limitations imposed by arthritis [40] or hesitation about joining general exercise classes due to being unable to keep up or lack of understanding [49]. Patients with PsA and foot disease struggled with walking, particularly on uneven ground [36].
-
6)
Transport needs and environmental modification
Four OA studies (Table 2) [21, 24, 25, 28] investigated needs related to transport. More than 20% of people experienced difficulties in one study [21]. Services to increase accessibility to public transport may improve people’s ability to socialise [25]. In people with hand OA, supports were needed to facilitate opening doors, holding the steering wheel and using bicycle hand brakes [24], with use of public transportation limited by their inability to hold straps/poles [24]. Travel required significant planning, including in getting in and out of cars, finding seated toilets in Taiwan and needing plan analgesia around going out [28].
Five IA studies (Table 3) [40, 41, 44, 47, 51] identified environmental limitations to moving about outside the home. These included lack of appropriate transport [44] and unsafe environment related to fear of falling related to environmental factors (uneven pavement, lack of ramps and lighting) [40, 41, 44]. Driving could be difficult [47, 51]. Some participants worried about falling victim of crime due to frailty [44].
Discussion
This review demonstrates the pervasive impact of arthritis on peoples’ lives, independent of aetiology. We have identified six key domains in which arthritis impacts life: daily living, social participation, financial security, occupation, exercise/leisure and transportation. All areas of need identified were common to OA and IA, illustrating that need appears to primarily be linked to symptoms common across musculoskeletal conditions, rather than aetiology or pathogenesis.
Non-healthcare needs related maintain daily functioning were identified by people with both OA and IA. Deficits lead to a sense of “failure”, particularly being unable to do household chores or care for children [22]. The pervasiveness of this theme highlights the importance of supporting functional ability in both ADLs and the workplace. People with arthritis appear to need robust social support systems to assist them with ADLs [22], and targeted assistive devices (e.g. for cooking) to enable participants to complete tasks and feel “normal” [23, 24, 40].
Needs related to social functioning were similar in people with IA and OA. Loneliness, withdrawal [24, 25, 43, 44], and lack of understanding from family, friends and communities were troublesome [23, 43], but partly negated by peer support groups [23]. People with both IA and OA wanted means to reduce social isolation. In the wider literature, social connectedness and “diffuse social relationships” have been identified as crucial to psychological wellbeing [54]. An individual’s health can be related to the strength of their social relationships, with participants in this review with “strong” social supports more likely to perceive good health [26]. Interestingly, in one study people with IA tended to be more interested (44%) in peer support groups than those with OA (20%) [31]. Further data are required regarding optimal delivery of peer support groups, particularly as self-management education groups are limited in effectiveness for most clinical outcomes [55].
The need for work retention was critical to people with both OA and IA, for financial security and social connectedness [43]. Arthritis is associated with reduced work productivity, early retirement and reduced wealth [6]. Flexibility and environmental adaptations in the workplace facilitated work retention in people with IA and OA [24, 25]. Maintaining employment is a key issue in people with RA, facilitated by both environmental adaptations and flexible work hours [56]. Use of modified schedules when required was associated with lower workplace activity limitation, fewer job disruptions and productivity losses [56]. Furthermore, loss of work or retirement exacerbated feelings of social isolation, highlighting the importance of employment in social connectedness and self-worth [43, 45]. Programs targeted to improve work retention in people with arthritis can reduce anxiety, improve mood and life satisfaction [57]. Given the importance of employment in financial wellbeing and social connectedness, further work is needed to identify contributors to work retention in people with arthritis and to support and educate employers and practitioners in providing these.
Both OA and IA had similar detrimental effects on physical and leisure activity participation. When activities couldn’t be modified/replaced, participants were excluded from activities with family and friends [22, 40]. Arthritis patients need assistance from healthcare providers with arthritis-specific exercise programs [58], as well as information about benefits and safety of exercise [34]. People with OA frequently report mobility and pain as barriers to participation in exercise [59], despite high quality evidence for its therapeutic benefits in OA and IA [60]. Access to practitioners with skills and knowledge in behaviour change, pain science and appropriate exercise programs/facilities is important for people with arthritis.
Transportation needs for those with IA and OA had broader impacts on other areas of need. Difficulties with transportation exacerbate dependence on others [40, 41], unemployment [50] and social isolation [32]. Transportation is intimately linked with freedom and independence in older adults, and has a pervasive impact on life [61]. Further research is required to understand factors limiting transportation and improve uptake in people with arthritis.
We have identified some contrasts between the experiences of people with OA and IA. Those with OA identified a lack of acknowledgement and community support [23, 43]. They felt OA and the resultant disability were underestimated with limited media coverage of, and research into, OA [23]. While participants with IA felt that sometimes their symptoms were underestimated [47], they did not report trivialisation of the disease itself. In the wider literature people with RA felt inadequate support and information were available, particularly in specific situations like pregnancy [62]. Public health campaigns could assist with educating the wider community about arthritis and its impact.
This study has limitations. Firstly, although these data highlight the impact of OA and IA, existing literature focusses on problems related to arthritis rather than evaluation of actual needs. Thus, due to a paucity of data, we have not directly questioned the “needs” of people with OA and IA. It remains unknown which services exist and meet current needs, and which are insufficient, an important gap in the literature. This is a focus of the World Health Organisation’s Integrated Care for Older people approach. However, in line with the Gothenburg model of person-centred care, a key step in providers being able to deliver effective, person-centred care is to understand the experience of the person [63]. Accordingly, we believe summarising the literature regarding these issues is an important step towards addressing non-healthcare needs of people with arthritis, and enabling the delivery of effective person-centred care. Given the limited data, it is difficult to comment on whether non-healthcare needs differ according to country or social setting. Furthermore, as participants included mainly post-menopausal females, generalizability may be limited to other groups (particularly men, younger people, and those in low- and middle-income settings). Studies included modest sample sizes. Heterogeneity of data collected means different areas were investigated in each study; this provides limited triangulation and/or validation of any single conclusion. Overall studies were at moderate risk of bias, with higher risk of bias in data collection and recruitment. Finally, we did not perform inter-rater reliability for study selection.
This review has numerous strengths. A comprehensive scoping literature search was performed across four different databases. Many qualitative studies were included to enable deeper exploration of participants’ non-healthcare needs and perspectives. This search captured data from multiple levels of care, including community-based populations, as well as a range of different disease stages. OA studies involved a range of joints.
Conclusions
Arthritis has a pervasive impact on different areas of life, regardless of disease aetiology. To patients, the similarities in functional impact far outweigh the differences in the disease pathogenesis. Whilst people with arthritis are acutely aware of their inability to perform tasks and perceived “failures”, little work has been performed to identify the patients’ perspective of non-healthcare needs to facilitate targeted service provision and provide holistic care. Future research is required to assess this, across a broader population and joint involvement, to identify whether there may be joint-specific non-healthcare needs. Improved characterization of the patients’ perceived non-healthcare needs is necessary to provide relevant support and services for people with arthritis.
Availability of data and materials
All data generated or analysed during the current study are included in this published article and its supplementary files.
Abbreviations
- ADLs:
-
Activities of daily living
- IA:
-
Inflammatory arthritis
- OA:
-
Osteoarthritis
- PsA:
-
Psoriatic arthritis
- RA:
-
Rheumatoid arthritis
- SLE:
-
Systemic lupus erythematosus
References
Foundation A. Arthritis by numbers. 2018.
IHME. The global burden of disease study 2019. Seattle; 2019. [updated 2019; cited 2021]; Available from: http://ghdx.healthdata.org/gbd-results-tool
Brand CA. The role of self-management in designing care for people with osteoarthritis of the hip and knee. Med J Aust. 2008;189(S10):S25–8. https://doi.org/10.5694/j.1326-5377.2008.tb02206.x.
Kahlenberg JM, Fox DA. Advances in the medical treatment of rheumatoid arthritis. Hand Clin. 2011;27(1):11–20. https://doi.org/10.1016/j.hcl.2010.09.002.
Chou L, Ranger TA, Peiris W, Cicuttini FM, Urquhart DM, Sullivan K, et al. Patients’ perceived needs for medical services for non-specific low back pain: a systematic scoping review. PLoS One. 2018;13(11):e0204885. https://doi.org/10.1371/journal.pone.0204885.
Schofield DJ, Callander EJ, Shrestha RN, Percival R, Kelly SJ, Passey ME. Labour force participation and the influence of having arthritis on financial status. Rheumatol Int. 2015;35(7):1175–81. https://doi.org/10.1007/s00296-015-3224-2.
Berkovic D, Ayton D, Briggs AM, Ackerman IN. “I would be more of a liability than an asset”: navigating the workplace as a younger person with arthritis. J Occup Rehabil. 2020;30(1):125–34. https://doi.org/10.1007/s10926-019-09853-2.
Restoux LJ, Dasariraju SR, Ackerman IN, Van Doornum S, Romero L, Briggs AM. Systematic review of the impact of inflammatory arthritis on intimate relationships and sexual function. Arthritis Care Res. 2020;72(1):41–62. https://doi.org/10.1002/acr.23857.
Luong ML, Cleveland RJ, Nyrop KA, Callahan LF. Social determinants and osteoarthritis outcomes. Aging Health. 2012;8(4):413–37. https://doi.org/10.2217/ahe.12.43.
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. Prisma extension for scoping reviews (prisma-scr): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Wluka A, Chou L, Briggs AM, Cicuttini FM. Understanding the needs of consumers with musculoskeletal conditions: consumers’ perceived needs of health information, health services and other non-medical services: a systematic scoping review; 2016.
Asadi-Lari M, Tamburini M, Gray D. Patients’ needs, satisfaction, and health related quality of life: towards a comprehensive model. Health Qual Life Outcomes. 2004;2(1):32. https://doi.org/10.1186/1477-7525-2-32.
Segan JD, Briggs AM, Chou L, Connelly KL, Seneviwickrama M, Sullivan K, et al. Patient-perceived health service needs in inflammatory arthritis: a systematic scoping review. Semin Arthritis Rheum. 2018;47(6):765–77. https://doi.org/10.1016/j.semarthrit.2017.10.019.
Walsh D, Downe S. Meta-synthesis method for qualitative research: a literature review. J Adv Nurs. 2005;50(2):204–11. https://doi.org/10.1111/j.1365-2648.2005.03380.x.
Hannes K, Macaitis K. A move to more systematic and transparent approaches in qualitative evidence synthesis: update on a review of published papers. Qual Res. 2012;12(4):402–42. https://doi.org/10.1177/1468794111432992.
Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess. 2011;15:1–164.
Noblit G, Hare R. Meta-ethnography: synthesizing qualitative studies; 1988. https://doi.org/10.4135/9781412985000.
France EF, Uny I, Ring N, Turley RL, Maxwell M, Duncan EAS, et al. A methodological systematic review of meta-ethnography conduct to articulate the complex analytical phases. BMC Med Res Methodol. 2019;19(1):35. https://doi.org/10.1186/s12874-019-0670-7.
(CASP) CSAP. Casp qualitative checklist: Oxford Centre for Triple Value Healthcare 2014 Contract No.: Document Number.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9. https://doi.org/10.1016/j.jclinepi.2011.11.014.
Ackerman IN, Buchbinder R, Osborne RH. Factors limiting participation in arthritis self-management programmes: an exploration of barriers and patient preferences within a randomized controlled trial. Rheumatology. 2013;52(3):472–9. https://doi.org/10.1093/rheumatology/kes295.
Al-Taiar A, Al-Sabah R, Elsalawy E, Shehab D, Al-Mahmoud S. Attitudes to knee osteoarthritis and total knee replacement in Arab women: a qualitative study. BMC Res Notes. 2013;6(1):406. https://doi.org/10.1186/1756-0500-6-406.
Baumann M, Euller-Ziegler L, Guillemin F. Evaluation of the expectations osteoarthritis patients have concerning healthcare, and their implications for practitioners. Clin Exp Rheumatol. 2007;25(3):404–9.
Bukhave EB, Huniche L. Activity problems in everyday life - patients' perspectives of hand osteoarthritis: 'Try imagining what it would be like having no hands. Disabil Rehabil. 2014;36(19):1636–43. https://doi.org/10.3109/09638288.2013.863390.
Chan KKW, Chan LWY. A qualitative study on patients with knee osteoarthritis to evaluate the influence of different pain patterns on patients' quality of life and to find out patients' interpretation and coping strategies for the disease. Rheumatol Rep. 2011;3:9–15.
Ilori T, Ladipo MM, Ogunbode AM, Obimakinde AM. Knee osteoarthritis and perceived social support amongst patients in a family medicine clinic. S Afr Fam Pract. 2016;58(6):202–6. https://doi.org/10.1080/20786190.2016.1198086.
Hill S, Dziedzic KS, Ong BN. The functional and psychological impact of hand osteoarthritis. Chronic Illness. 2010;6(2):101–10. https://doi.org/10.1177/1742395309345614.
Kao M-H, Tsai Y-F. Illness experiences in middle-aged adults with early-stage knee osteoarthritis: findings from a qualitative study. J Adv Nurs. 2014;70(7):1564–72. https://doi.org/10.1111/jan.12313.
Kjeken I, Darre S, Slatkowsky-Cristensen B, Hermann M, Nilsen T, Eriksen CS, et al. Self-management strategies to support performance of daily activities in hand osteoarthritis. Scand J Occup Ther. 2013;20(1):29–36. https://doi.org/10.3109/11038128.2012.661457.
Leung YY, Li JC, Thumboo J. Domains rated as important by patients with hand osteoarthritis. Int J Rheum Dis. 2019;22(11):2045–51. https://doi.org/10.1111/1756-185X.13709.
Neville C, Fortin PR, Fitzcharles M, Baron M, Abrahamowitz M, Du Berger R, et al. The needs of patients with arthritis: The patient’s perspective. Arthritis Care Res. 1999;12:85–95.
Tanimura C, Morimoto M, Hiramatsu K, Hagino H. Difficulties in the daily life of patients with osteoarthritis of the knee: scale development and descriptive study. J Clin Nurs. 2011;20(5-6):743–53. https://doi.org/10.1111/j.1365-2702.2010.03536.x.
Alten R, van de Laar M, De Leonardis F, Tietz N, Guerreiro M, van Vollenhoven R. Physical and emotional burden of rheumatoid arthritis: data from ra matters, a web-based survey of patients and healthcare professionals. Rheumatol Ther. 2019;6(4):587–97. https://doi.org/10.1007/s40744-019-00179-2.
Been-Dahmen JMJ, Walter MJ, Dwarswaard J, Hazes JMW, van Staa A, Ista E. What support is needed to self-manage a rheumatic disorder: a qualitative study. BMC Musculoskelet Disord. 2017;18:1–9.
Bergsten U, Bergman S, Fridlund B, Arvidsson B. “Striving for a good life”--the management of rheumatoid arthritis as experienced by patients. Open Nurs J. 2011;5:95–101. https://doi.org/10.2174/1874434601105010095.
Carter K, Walmsley S, Chessman D, Rome K, Turner DE. Perspectives of patients and health professionals on the experience of living with psoriatic arthritis-related foot problems: a qualitative investigation. Clin Rheumatol. 2019;38(6):1605–13. https://doi.org/10.1007/s10067-018-04411-2.
Cunha-Miranda L, Costa L, Ribeiro JS. Near study: needs and expectations in rheumatoid arthritis - do we know our patients needs? Acta Reumatol. 2010;35:314–23.
Giacomelli R, Gorla R, Trotta F, Tirri R, Grassi W, Bazzichi L, et al. Quality of life and unmet needs in patients with inflammatory arthropathies: results from the multicentre, observational rapsodia study. Rheumatology. 2015;54(5):792–7. https://doi.org/10.1093/rheumatology/keu398.
Hamnes B, Hauge MI, Kjeken I, Hagen KB. ‘I have come here to learn how to cope with my illness, not to be cured’: A qualitative study of patient expectations prior to a one-week self-management programme. Musculoskelet Care. 2011;9(4):200–10. https://doi.org/10.1002/msc.212.
Henchoz Y, Zufferey P, So A. Stages of change, barriers, benefits, and preferences for exercise in ra patients: a cross-sectional study. Scand J Rheumatol. 2013;42(2):136–45. https://doi.org/10.3109/03009742.2012.724707.
Herrera-Saray P, Pelaez-Ballestas I, Ramos-Lira L, Sanchez-Monroy D, Burgos-Vargas R. Usage problems and social barriers faced by persons with a wheelchair and other aids. Qualitative study from the ergonomics perspective in persons disabled by rheumatoid arthritis and other conditions. Reumatology. 2013;9(1):24–30. https://doi.org/10.1016/j.reuma.2012.05.010.
Kostova Z, Caiata-Zufferey M, Schulz PJ. The impact of social support on the acceptance process among ra patients: a qualitative study. Psychol Health. 2014;29(11):1283–302. https://doi.org/10.1080/08870446.2014.925895.
Kristiansen TM, Primdahl J, Antoft R, Hørslev-Petersen K. Everyday life with rheumatoid arthritis and implications for patient education and clinical practice: a focus group study. Musculoskelet Care. 2012;10(1):29–38. https://doi.org/10.1002/msc.224.
Laidmae VI, Leppik L, Tulva T, Haal ML. Disease-related social and family life: people coping with rheumatoid arthritis in Estonia. Crit Public Health. 2009;19(1):87–105. https://doi.org/10.1080/09581590802375871.
Lempp H, Scott D, Kingsley G. The personal impact of theumatoid arthritis on patients' identity: a qualitative study. Chronic Illness. 2006;2(2):109–20. https://doi.org/10.1177/17423953060020020601.
Sato M, Yamazaki Y, Sakita M, Bryce TJ. Benefit-finding among people with rheumatoid arthritis in Japan. Nurs Health Sci. 2008;10(1):51–8. https://doi.org/10.1111/j.1442-2018.2007.00372.x.
Strand V, Wright GC, Bergman MJ, Tambiah J, Taylor PC. Patient expectations and perceptions of goal-setting strategies for disease management in rheumatoid arthritis. J Rheumatol. 2015;42(11):2046–54. https://doi.org/10.3899/jrheum.140976.
Sverker A, Ostlund G, Thyberg M, Thyberg I, Valtersson E, Bjork M. Dilemmas of participation in everyday life in early rheumatoid arthritis: a qualitative interview study (the swedish tira project). Disabil Rehabil. 2015;37(14):1251–9. https://doi.org/10.3109/09638288.2014.961658.
Thomas R, Hewlett S, Swales C, Cramp F. Keeping physically active with rheumatoid arthritis: semi-structured interviews to explore patient perspectives, experiences and strategies. Physiotherapy. 2019;105(3):378–84. https://doi.org/10.1016/j.physio.2018.09.001.
Van der meer M, Hoving JL, Vermeulen MIM, Herenius MMJ, Tak PP, Sluiter JK, et al. Experiences and needs for work participation in employees with rheumatoid arthritis treated with anti-tumour necrosis factor therapy. Disabil Rehabil. 2011;33:2587–95.
Wollenhaupt J, Ehlebracht-Koenig I, Groenewegen A, Fricke D. Prioritizing the patient: optimizing therapy in rheumatoid arthritis. Results of a patient questionnaire in northern Germany. Open Access Rheumatol. 2013;5:51–67. https://doi.org/10.2147/OARRR.S38032.
Bank TW. World bank country and lending groups. 2019 [updated 2019; cited]; Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
Lempp H, Hofmann D, Hatch SL, Scott DL. Patients’ views about treatment with combination therapy for rheumatoid arthritis: a comparative qualitative study. BMC Musculoskelet Disord. 2012;13(1):200. https://doi.org/10.1186/1471-2474-13-200.
Fitzpatrick R, Newman S, Lamb R, Shipley M. Social relationships and psychological well-being in rheumatoid arthritis. Soc Sci Med. 1988;27(4):399–403. https://doi.org/10.1016/0277-9536(88)90275-4.
Lefevre-Colau MM, Buchbinder R, Regnaux JP, Roren A, Poiraudeau S, Boutron I. Self-management education programmes for rheumatoid arthritis. Cochrane Database Syst Rev. 2014;2014:CD011338.
Gignac MA, Cao X, McAlpine J. Availability, need for, and use of work accommodations and benefits: are they related to employment outcomes in people with arthritis? Arthritis Care Res. 2015;67(6):855–64. https://doi.org/10.1002/acr.22508.
Barlow J, Wright C, Kroll T. Overcoming perceived barriers to employment among people with arthritis. J Health Psychol. 2001;6(2):205–16. https://doi.org/10.1177/135910530100600201.
Wilcox S, Der Ananian C, Abbott J, Vrazel J, Ramsey C, Sharpe PA, et al. Perceived exercise barriers, enablers, and benefits among exercising and nonexercising adults with arthritis: results from a qualitative study. Arthritis Rheum. 2006;55(4):616–27. https://doi.org/10.1002/art.22098.
Dobson F, Bennell KL, French SD, Nicolson PJ, Klaasman RN, Holden MA, et al. Barriers and facilitators to exercise participation in people with hip and/or knee osteoarthritis: synthesis of the literature using behavior change theory. Am J Phys Med Rehabil. 2016;95(5):372–89. https://doi.org/10.1097/PHM.0000000000000448.
Rausch Osthoff AK, Niedermann K, Braun J, Adams J, Brodin N, Dagfinrud H, et al. 2018 eular recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018;77(9):1251–60. https://doi.org/10.1136/annrheumdis-2018-213585.
Commission P. Caring for older australians, report no. 53, final inquiry report. Canberra; 2011. Contract No.: Document Number
Ackerman IN, Jordan JE, Van Doornum S, Ricardo M, Briggs AM. Understanding the information needs of women with rheumatoid arthritis concerning pregnancy, post-natal care and early parenting: a mixed-methods study. BMC Musculoskelet Disord. 2015;16(1):194. https://doi.org/10.1186/s12891-015-0657-4.
Britten N, Ekman I, Naldemirci O, Javinger M, Hedman H, Wolf A. Learning from Gothenburg model of person centred healthcare. BMJ. 2020;370:m2738.
Acknowledgements
Nil additional.
Funding
This work was supported by a partnership grant awarded by Musculoskeletal Australia. Musculoskeletal Australia contributed to the conception of the review question but they did not influence the review execution, results or interpretation. L.C. is the recipient of an Australian Postgraduate Award and Arthritis Foundation Scholarship. A.E.W is the recipient of the recipient of the Career Development Fellowship, Royal Australasian College of Physicians.
Author information
Authors and Affiliations
Contributions
JF, MS and AW contributed to conception and design of study, analysis and interpretation of data, drafting the article, revising it critically for important intellectual content and final approval of the version to be submitted. SY and SA contributed to analysis and interpretation of data, revising the article critically for important intellectual content and final approval of version to be submitted. LC contributed to acquisition, analysis and interpretation of data, revising the article critically for important intellectual content and final approval of the version to be submitted. KS contributed to conception and design of the study, drafting the article and final approval of the version to be submitted. FM and AMB contributed to conception/design of the study, interpretation of the data, revising the article critically for important intellectual content and final approval of the version to be submitted. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not required as this systematic review did not involve data collection or patient recruitment.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest or competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fairley, J.L., Seneviwickrama, M., Yeh, S. et al. Person-centred care in osteoarthritis and inflammatory arthritis: a scoping review of people’s needs outside of healthcare. BMC Musculoskelet Disord 22, 341 (2021). https://doi.org/10.1186/s12891-021-04190-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-021-04190-z