Abstract
Background
Critically evaluation and summarization for the outcomes between autografts and artificial grafts using in anterior cruciate ligament (ACL) reconstruction have not been performed currently. The purpose of this study is to compare the clinical outcomes between artificial ligaments and autografts at a short- to mid-term follow-up.
Methods
A computerized search of the databases was conducted including Medline, Embase, and the Cochrane library. Only prospective or retrospective comparative studies with a minimum 2-year follow-up and a minimum sample size of 15 for each group were considered for inclusion. Two independent reviewers performed data extraction and methodological quality assessment. A Mantel-Haenszel analysis was used for pooling of results. Sensitivity analysis was performed in order to maintain the stability of results.
Results
Seven studies were included in this study. The total sample size was 403 (autograft group: 206 patients; synthetic graft group: 197 patients). Four studies were randomized controlled trials. Two studies were retrospective comparative studies and one study was non-randomized prospective comparative study. In terms of instrumented laxity, patient-oriented outcomes and complications, no significant difference was occurred between new artificial ligaments and autografts. But the results of IKDC grades and instrumented laxity were worsen in early artificial ligaments compared to autografts.
Conclusions
The outcomes of new generation of artificial ligaments are similar to autografts at a short- to mid-term follow-up. However, the early artificial ligaments are not suggested for ACL reconstruction compared to autografts.
Similar content being viewed by others
Background
Anterior cruciate ligament (ACL) injury is a main cause of recurrent knee instability and may result in secondary damages to other structures of the knee, such as meniscal tears and articular cartilage degeneration [1]. Currently, ACL reconstruction is the gold-standard surgical technique for ACL injury [2]. Reconstruction can be performed by using autograft, allograft or synthetic graft [3]. Despite the vast amount of researches, there still have a great deal of debates concentrating on the clinical outcomes of using different grafts in ACL reconstruction.
Autograft is a well-recognized and widely used material for ACL reconstruction due to a good graft stability and a well return to high-level sports [4]. And bone-patella tendon-bone (BPTB) autograft has historically served as the gold standard for ACL reconstruction based not only on widespread global use but also as the first autograft option. Reconstruction with synthetic grafts has the advantage of eliminating both the donor-site morbidity and disease transmission with fast rehabilitation [5]. High graft failures, no so-called ligamentization and severe synovitis have been reported as major disadvantages of synthetic grafts [6,7,8].
A few conventional narrative reviews have addressed related issues about the graft selection for ACL reconstruction [9,10,11,12]. Firm conclusions regarding the clinical outcomes with autografts or synthetic grafts cannot be drawn from those narrative reviews due to some inherent bias. Moreover, there have already been systematic reviews and meta-analysis which compared the clinical outcomes between allografts and autografts using in ACL reconstruction [13,14,15,16]. Critically evaluation and summarization for the outcomes between autografts and synthetic grafts using in ACL reconstruction have not been performed currently.
Using the best available evidence, the purpose of this research is to compare synthetic grafts with autografts in ACL reconstruction by evaluation the clinical outcomes including the results of instrumented laxity, patient-oriented outcomes, complications and graft failures.
Methods
Searching strategy
This research was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [17]. Two researchers searched the international databases independently up to December 30th, 2016, including Medline, Embase, and the Cochrane library. OpenGrey, the World Health Organization International Clinical Trials Registry Platform, the International Standard Randomised Controlled Trial Number (ISRCTN) registry, and Current Controlled Trials were searched to review the trial registry and grey literature. There was no restriction to years of publication and languages.
Eligibility criteria
Eligibility criteria were as follows: 1) a clinical study with a prospective or retrospective comparative design (Level of Evidence I, II, or III) [18]; 2) patients with no limitation of race and sex undergoing primary ACL reconstruction; 3) a study of ACL reconstruction comparing autografts with synthetic grafts and no restriction for types; 4) the outcomes being evaluated including physical examinations, complications, or patient-oriented outcomes etc.; 5) at least 2 years follow-ups; 6) at least 15 sample size for each group [15]. Knee laxity assessments included the arthrometer test and physical examinations (Lachman test and pivot-shift test). The details were shown in Table 1.
Any researches that failed to meet the inclusion criteria were excluded. In addition, a study was excluded if data from the same patients were reported in another study that had longer follow-up.
Data extraction and quality assessment
Two reviewers independently performed data extraction and quality assessment. In case of discrepancies, any controversy was resolved by further discussion with the corresponding author. The extraction included the following: (1) the characteristics of included researches (author, publication date, study design, participants’ demography, sample size, and duration of follow-up); (2) the details of methodology (implant type and drilling technique); (3) the details of outcomes. In our research, Newcastle-Ottawa Scale (NOS) was used to assess quality for cohort study while Jadad scale was used to assess quality for randomized controlled trial (RCT) [19, 20].
Statistical analysis
The meta-analysis was conducted using RevMan Manager 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). Using the same format, two reviewers independently collected data and crosschecked the results. Disagreements were discussed with the corresponding author and reached consensus in order to ensure accuracy.
Odds ratio (OR) with 95% confidence interval (CI) was calculated for dichotomous while mean difference (MD) with corresponding 95% CI was calculated for continuous outcomes. Statistical heterogeneity was assessed by calculating the heterogeneity index I2. When heterogeneity was significant (I2 > 50%), a Mantel-Haenszel analysis utilizing a random-effects model was used; otherwise a fixed-effects model was used when heterogeneity was considered as low (I2 ≤ 0.50). Funnel plots were used to test publication bias and a relatively symmetric funnel plot indicated inexistence of obvious publication bias. Sensitivity analysis was performed in order to maintain the stability of results.
Results
Article selection results
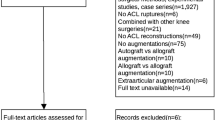
Three hundred and six relevant articles were initially selected according to the search strategy (Fig. 1). There were 161 articles left after checking for duplicates by using the literature management software Endnote X7. One hundred and forty-five articles were removed by screening the title and abstract. After reviewing the full text, 9 articles were excluded through assessment for eligibility. Eventually, 7 articles were included in qualitative and quantitative synthesis [21,22,23,24,25,26,27].
Characteristics of selected articles
All eligible studies were written in English from 1993 to 2013 (Table 2). Two studies were conducted in a North American country, and three studies were conducted in a European country. The other two studies were conducted in China. Among these studies, the synthetic graft used to compare with autograft included the Ligament Advanced Reinforcement System (LARS) artificial ligament (3 studies), the Leeds-Keio (LK) artificial ligament (2 studies), the Ligament Augmentation Device (LAD) (1 study) and the polyglycolic acid Dacron (PGA-Dacron) graft (1 study). The autograft used for comparison was BPTB (6 studies) and hamstring tendon (1 study). The rate of follow-up was ≥90% and the follow-up periods were ≥24 months in all included studies. The total sample size was 403 patients (autograft group: 206 patients; synthetic graft group: 197 patients). The release source and release date of each artificial ligament were shown in Table 3.
The synthetic grafts were divided into two groups (Group 1: early generation; Group 2: new generation) for analysis. In this study, the early generation of the artificial ligaments contained the LK artificial ligament and the LAD, while the new generation included the LARS artificial ligament and the PGA-Dacron graft [2, 26]. Among all included articles, 4 articles were related to the new generation and 3 articles were related to the old generation (Table 2).
Quality of selected articles
Assessment of the methodological quality revealed that there were four RCTs (Level I). Two studies were retrospective comparative studies (Level III) and one study was non-randomized prospective comparative study (Level II). Among these four RCTs, only one article was of high quality with scores ≥4 while the other three articles were of low quality with scores ≤3 according to Jadad scale (Table 4). Assessed by NOS scale, two retrospective studies and one prospective study were of high quality. All demographic data were compared between two groups and showed no significant difference in eligible studies.
Meta-analysis
Instrumented laxity
All included studies tested instrumented laxity. The study of Nau et al. was excluded for providing quantitative data other than grade data of instrumented laxity (> 5 mm or ≤5 mm), which could not be compared with other studies [22]. No heterogeneity was found among the studies. Using the fixed-effects model in analysis, the early generation of synthetic grafts had a significant difference in knee laxity compared with autografts and the synthetic graft had a poorer result (OR = 11.44; 95% CI: 2.46, 53.16; p = 0.98; I2 = 0%; Fig. 2a). Conversely, the new generation of synthetic graft showed no significant difference in knee laxity compared with autografts (OR = 0.63; 95% CI: 0.21, 1.93; p = 0.44; I2 = 0%; Fig. 2b).
Physical examinations
Two studies assessed the anterior stability by Lachman test and two studies evaluated the rotational stability through pivot-shift test (Table 1). All included studies were related to the early artificial ligaments (LK artificial ligament and LAD). The Lachman test showed a poorer result in the early synthetic grafts than in the autografts (OR = 0.02, 95% CI: 0.00, 0.41), indicating a worse anterior stability. The result of pivot-shift test was poor in early synthetic grafts (OR = 0.03, 95% CI: 0.01, 0.16), documenting a worse rotational stability comparing to autografts.
International knee documentation committee (IKDC) grades
Six studies reported postoperative IKDC grades but the study of Nau et al. was excluded for providing the different type of categorical data comparing to other included studies [22]. No heterogeneity was found and a fixed-effects model was used to analysis (Fig. 3). There were 51 patients in the early synthetic graft group and 50 patients in the autograft group. The early synthetic grafts (LK, LAD) had worsen IKDC grades (OR = 3.41; 95% CI: 1.30, 8.89; p = 0.57; I2 = 0%; Fig. 3a). Altogether 95 cases in the new synthetic graft group and 97 cases in the autograft group were reported. The new synthetic grafts (LARS) had no difference in IKDC grades compared to autografts (OR = 0.72; 95% CI: 0.35, 1.48; p = 0.90; I2 = 0%).
Lysholm scores
Six eligible studies tested postoperative Lysholm scores but the results of two studies could not be analyzed in meta-analysis. One was excluded due to lack of standard deviation and the other was due to suppling Lysholm scores as grade data other than quantitative data [21, 24]. Three studies were in Group 2 while only one study was in Group 1. There were altogether 95 cases in Group 2 and 97 cases in the autograft group. Heterogeneity was not found among these three studies and a fixed-effects model was used (p = 0.88; I2 = 0%), showing no significant difference in the Lysholm scores between two groups (OR = 1.80; 95% CI: -0.52, 4.13).
Tegner scores
Six studies reported Tegner scores but only 3 studies applied mean scores and standard deviations [23, 25, 27]. The rest three studies documented there was no significant difference between two groups in their longest follow-up time. Two studies were related to the new generation of the synthetic grafts and one study were focused on the old generation. Heterogeneity was not significant and a fixed-effects model was used, no significant difference occurred in new synthetic grafts and autografts (OR = 0.40; 95% CI: -0.09, 0.89).
Complications
Six studies evaluated complications of ACL reconstruction. The study conducted by Endstrom et al. did not report the complications after ACL reconstruction and was excluded for analysis. No heterogeneity was found and a fixed-effects model was used (I2 = 0%; Fig. 4). Altogether 44 patients were included in the early synthetic graft group and 50 patients were included in the compared group. No significant difference was found in the rate of complications between two groups (OR = 0.50; 95% CI: 0.16, 1.49; Fig. 4a). Similarly, no significant difference occurred in the new synthetic grafts and autografts (OR = 0.75; 95% CI: 0.14, 3.89; Fig. 4b).
Sensitivity analysis indicated that the study with regard to four-strand HT graft had no obvious deviation compared to other studies concerning about BPTB in evaluation of knee laxity, patient-oriented outcomes and the rate of complications.
Publication bias
Funnel plots of instrumented laxity and complications were used to evaluate the publication bias, showing the lack of obvious bias among the eligible studies related to new synthetic grafts according to a relative symmetric funnel plot (Figs. 5 and 6).
Discussion
The key findings of present meta-analysis indicated that, in general, the patient-oriented outcomes and the rate of complications of ACL reconstruction with synthetic grafts were not significantly different from those with autograft, especially for new generation synthetic grafts (LARS and PGA- Dacron). However, with regard to knee laxity, ACL reconstruction with early artificial grafts had obviously poorer knee laxity from those with autografts (95% CI: 1.03, 4.72) while new artificial grafts showed no significant difference with autografts (95% CI: 0.21, 1.93).
The LK artificial ligament was a polyester mesh-like structure intended as a scaffold for soft tissue ingrowth [28]. The LAD, a band-like braid of polypropylene, was designed to protect the autogenous graft from excessive stresses [29]. Murray et al. reported that 28% of the group were known to have ruptured the LK ligament and 56% had increased laxity compared to the opposite normal knee at a 10–16 year follow-up [30]. A study conducted since 1983, included 856 patients accepted ACL reconstruction with LAD, showed 63 cases of complications and 73 cases of re-surgery [31]. Long-term follow-up results documented both the LK artificial ligament and the LAD were not suitable as an ACL substitute [30,31,32]. Moreover, the LAD caused effusions and reactive synovitis in the knee for provoking inflammatory reactions, and was found to delay maturation of autogenous graft [33]. The knee laxity and the IKDC grades were significantly different from autografts and early artificial ligaments, indicating that the short-term outcomes of early artificial ligaments were worsen than autografts. The results of our research for early artificial ligaments were consistent with previous studies. It was not suggested to use early synthetic grafts including the LK artificial ligament and the LAD due to their poor follow-up outcomes.
The LARS artificial ligament was made of polyethylene terephthalate, divided in two parts (intra-articular part and extra-articular part) [34]. Intra-articular part was composed of longitudinal external rotation fibers without transverse fibers as an imitation of ACL anatomic structure while extra-articular part was weaved by longitudinal and transverse fibers in order to avoid ligament deformation. Dericks et al. reported encouraging results in 220 cases of ACL reconstruction used LARS artificial ligament with a mean follow-up of 2.5 years [35]. In 2013, Parchi reported no case of complications and only one case of mechanical graft rupture after using LARS artificial ligament for ACL reconstruction at a mean follow-up of eight years [36]. In 2015, a study with a minimum follow-up of 10 years, showed almost half of the patients (8/18) were subjectively not satisfied with the surgical result using LARS artificial ligament [7]. The clinical outcomes were appealing at short-term but controversy at long-term [36,37,38,38]. In our research, 3 studies compared LARS artificial ligament with autografts, showing no significant difference in knee laxity, functions and the rate of complications [22, 25, 27]. The outcomes of LARS artificial ligament used in ACL reconstruction were appealing at least in short-term follow-up. Another new synthetic graft called PGA-Dacron graft, consisted of synthetic braided ligament made of 75% degradable PGA filaments and 25% non-degradable Dacron thread, showed a satisfied result compared to autograft including knee laxity, range of motion, patient-oriented questionnaires, muscle performance, degenerative changes of knee, and the rate of failure and complications [26].
Complications occurred in the autograft group were infection, patellofemoral pain, recurrent effusion and extension loss. In the synthetic graft group, complications included interference screw-related problems (pain and screw loosening), patellofemoral pain and extension loss. There were altogether 12 cases in the autograft group and 8 cases in the synthetic graft group. Extension loss was the most common complication in included studies and it might be associated with graft impingement and a formation of cyclops [39, 40]. Graft impingement was mainly caused by malposition of femoral bone tunnel and a “cyclops” was a fibrous nodule caused by proliferation of fibrovascular tissues similar to a healing scar after ACL reconstruction [41, 42]. The synthetic grafts were located in a non-anatomic but isometric placement while the autografts were usually located in an anatomic placement. The results of complications showed no significant difference between these two location methods.
Some studies documented that subjective outcomes were not correlated with objective outcomes including instrumented laxity test and clinical examination [43]. Among these included studies, three of them showed difference in objective parameters but no significant difference in patient-oriented outcomes [21, 22, 24]. Meanwhile, the opposite circumstance did not appear (similar in objective outcomes but different in subjective outcomes). Kraeutler et al. suggested that patient satisfaction is the most important measurable index for the outcomes of ACL reconstruction [13]. Only the overall IKDC grades showed better results in the autografts than in the early synthetic grafts and the rest indicators for patient satisfaction showed no significant difference between groups. However, it was still well recognized that a KT-1000 side-to-side difference of >5 mm was defined as a clinical failure [37]. Both objective parameters and subjective outcomes shoulder be considered for assessment of ACL reconstruction.
The limitations of this study were as follows: (1) Until now, there was still lack of high-quality RCT or large-scale multi-center retrospective comparable studies to prove the effectiveness of artificial ligaments compared to autografts. (2) The follow-up time was not sufficiently long for evaluation of ACL reconstruction. (3) In the included studies, the types of grafts used in ACL reconstruction were not the same (Hamstring tendon, BPTB, LK, LAD, LARS and PGA-Dacron). (4) The data included in the research did not cover all included studies due to the lack of relative data.
Conclusions
The outcomes of new generation of artificial ligaments are similar to autografts in terms of knee laxity, patient-oriented outcomes and the rate of complications at a short- to mid-term follow-up. However, the early artificial ligaments (LK, LAD) are not suggested for ACL reconstruction according to worse outcomes in knee laxity and functions compared to autografts.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- BPTB:
-
Bone-patella tendon-bone
- CI:
-
Confidence interval
- IKDC:
-
International Knee Documentation Committee
- ISRCTN:
-
International Standard Randomised Controlled Trial Number
- LAD:
-
Ligament Augmentation Device
- LARS:
-
Ligament Advanced Reinforcement System
- LK:
-
Leeds-Keio
- MD:
-
mean difference
- NOS:
-
Newcastle-Ottawa scale
- OR:
-
Odds ratio
- PGA-Dacron:
-
polyglycolic acid Dacron
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT:
-
Randomized controlled trial
References
Chalmers PN, Mall NA, Moric M, Sherman SL, Paletta GP, Cole BJ, et al. Does ACL reconstruction alter natural history?: a systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96(4):292–300.
Mascarenhas R, MacDonald PB. Anterior cruciate ligament reconstruction: a look at prosthetics--past, present and possible future. Mcgill J Med. 2008;11(1):29–37.
Kim HS, Seon JK, Jo AR. Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2013;25(4):165–73.
Shelton WR, Fagan BC. Autografts commonly used in anterior cruciate ligament reconstruction. The Journal of the American Academy of Orthopaedic Surgeons. 2011;19(5):259–64.
Vaishya R, Agarwal AK, Ingole S, Vijay V. Current trends in anterior cruciate ligament reconstruction: a review. Cureus. 2015;7(11):e378.
Glezos CM, Waller A, Bourke HE, Salmon LJ, Pinczewski LA. Disabling synovitis associated with LARS artificial ligament use in anterior cruciate ligament reconstruction: a case report. Am J Sports Med. 2012;40(5):1167–71.
Tiefenboeck TM, Thurmaier E, Tiefenboeck MM, Ostermann RC, Joestl J, Winnisch M, et al. Clinical and functional outcome after anterior cruciate ligament reconstruction using the LARS system at a minimum follow-up of 10 years. Knee. 2015;22(6):565–8.
Iliadis DP, Bourlos DN, Mastrokalos DS, Chronopoulos E, Babis GC. LARS artificial ligament versus ABC purely polyester ligament for anterior cruciate ligament reconstruction. Orthop. J Sports Med. 2016;4(6):2325967116653359.
Shaerf DA, Pastides PS, Sarraf KM, Willis-Owen CA. Anterior cruciate ligament reconstruction best practice: a review of graft choice. World J Orthop. 2014;5(1):23–9.
Sherman OH, Banffy MB. Anterior cruciate ligament reconstruction: which graft is best? Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2004;20(9):974–80.
Duchman KR, Lynch TS, Spindler KP. Graft selection in anterior cruciate ligament surgery: who gets what and why. Clin Sports Med. 2017;36(1):25–33.
Miller SL, Gladstone JN. Graft selection in anterior cruciate ligament reconstruction. The Orthopedic clinics of North America. 2002;33(4):675–83.
Kraeutler MJ, Bravman JT, McCarty EC. Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med. 2013;41(10):2439–48.
Yao LW, Wang Q, Zhang L, Zhang C, Zhang B, Zhang YJ, et al. Patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2015;25(2):355–65.
Carey JL, Dunn WR, Dahm DL, Zeger SL, Spindler KP. A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. J Bone Joint Surg Am. 2009;91(9):2242–50.
Zeng C, Gao SG, Li H, Yang T, Luo W, Li YS, et al. Autograft versus allograft in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials and systematic review of overlapping systematic reviews. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2016;32(1):153–63. e18
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS med. 2009;6(7):e1000100.
Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85-A(1):1–3.
Cota GF, de Sousa MR, Fereguetti TO, Rabello A. Efficacy of anti-leishmania therapy in visceral leishmaniasis among HIV infected patients: a systematic review with indirect comparison. PLoS Negl Trop Dis. 2013;7(5):e2195.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials. 1996;17(1):1–12.
Engstrom B, Wredmark T, Westblad P. Patellar tendon or Leeds-Keio graft in the surgical treatment of anterior cruciate ligament ruptures. Intermediate results. Clin Orthop Relat Res. 1993;295:190–7.
Nau T, Lavoie P, Duval N. A new generation of artificial ligaments in reconstruction of the anterior cruciate ligament. Two-year follow-up of a randomised trial. J Bone Joint Surg Br. 2002;84(3):356–60.
Ghalayini SR, Helm AT, Bonshahi AY, Lavender A, Johnson DS, Smith RB. Arthroscopic anterior cruciate ligament surgery: results of autogenous patellar tendon graft versus the Leeds-Keio synthetic graft five year follow-up of a prospective randomised controlled trial. Knee. 2010;17(5):334–9.
Grontvedt T, Engebretsen L. Comparison between two techniques for surgical repair of the acutely torn anterior cruciate ligament. A prospective, randomized follow-up study of 48 patients. Scand J Med Sci Sports. 1995;5(6):358–63.
Liu ZT, Zhang XL, Jiang Y, Zeng BF. Four-strand hamstring tendon autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Int Orthop. 2010;34(1):45–9.
Pritchett JW. Assisted reproduction of the anterior cruciate ligament. J Knee Surg. 2009;22(4):325–30.
Pan X, Wen H, Wang L, Ge T. Bone-patellar tendon-bone autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. European journal of orthopaedic surgery & traumatology : orthopedie traumatologie. 2013;23(7):819–23.
Fujikawa K, Iseki F, Seedhom BB. Arthroscopy after anterior cruciate reconstruction with the Leeds-Keio ligament. J Bone Joint Surg Br. 1989;71(4):566–70.
Kennedy JC, Roth JH, Mendenhall HV, Sanford JB. Presidential address. Intraarticular replacement in the anterior cruciate ligament-deficient knee. Am J Sports Med. 1980;8(1):1–8.
Murray AW, Macnicol MF. 10-16 year results of Leeds-Keio anterior cruciate ligament reconstruction. Knee. 2004;11(1):9–14.
Riel KA. Augmented anterior cruciate ligament replacement with the Kennedy-LAD (ligament augmentation device)--long term outcome. Zentralbl Chir. 1998;123(9):1014–8.
Denti M, Bigoni M, Dodaro G, Monteleone M, Arosio A. Long-term results of the Leeds-Keio anterior cruciate ligament reconstruction. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 1995;3(2):75–7.
Kumar K, Maffulli N. The ligament augmentation device: an historical perspective. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 1999;15(4):422–32.
Chen J, Gu A, Jiang H, Zhang W, Yu X. A comparison of acute and chronic anterior cruciate ligament reconstruction using LARS artificial ligaments: a randomized prospective study with a 5-year follow-up. Arch Orthop Trauma Surg. 2015;135(1):95–102.
Dericks G. Ligament advanced reinforcement system anterior cruciate ligament reconstruction. Op Tech Sports Med. 1995;3:187–205.
Parchi PD, Gianluca C, Dolfi L, Baluganti A, Nicola P, Chiellini F, et al. Anterior cruciate ligament reconstruction with LARS artificial ligament results at a mean follow-up of eight years. Int Orthop. 2013;37(8):1567–74.
Gao K, Chen S, Wang L, Zhang W, Kang Y, Dong Q, et al. Anterior cruciate ligament reconstruction with LARS artificial ligament: a multicenter study with 3- to 5-year follow-up. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2010;26(4):515–23.
Lavoie P, Fletcher J, Duval N. Patient satisfaction needs as related to knee stability and objective findings after ACL reconstruction using the LARS artificial ligament. Knee. 2000;7(3):157–63.
Cha J, Choi SH, Kwon JW, Lee SH, Ahn JH. Analysis of cyclops lesions after different anterior cruciate ligament reconstructions: a comparison of the single-bundle and remnant bundle preservation techniques. Skelet Radiol. 2012;41(8):997–1002.
van der List JP, Zuiderbaan HA, Nawabi DH, Pearle AD. Impingement following anterior cruciate ligament reconstruction: comparing the direct versus indirect femoral tunnel position. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA: p. 2015;
Udagawa K, Niki Y, Enomoto H, Toyama Y, Suda Y. Factors influencing graft impingement on the wall of the intercondylar notch after anatomic double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(9):2219–25.
Nikolic O, Vanhoenacker FM, Petrovic K, Vandenberk R. Cyclops lesion of the knee. JBR-BTR. 2012;95(5):336.
Hyder N, Bollen SR, Sefton G, Swann AC. Correlation between Arthrometric evaluation of knees using KT 1000 and telos stress radiography and functional outcome following ACL reconstruction. Knee. 1997;4(3):121–4.
Acknowledgments
The corresponding author wishes to thank all the co-authors for their contributions.
Funding
Scholar Fund of Second Military Medical University (2016JS24).
Tengfei Project (16 T016).
Zonghe Project (2016JS24).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
JZ and ZC searched the databases and performed data extraction and quality assessment; JZ, HX and XW designed the study; JZ, ZC, CS, XC and LT analyzed the data and wrote the manuscript. JZ, ZC and CS revised the manuscript. All authors read and approved the final content of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. There is no need for ethical approval and informed consents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Jia, ZY., Zhang, C., Cao, Sq. et al. Comparison of artificial graft versus autograft in anterior cruciate ligament reconstruction: a meta-analysis. BMC Musculoskelet Disord 18, 309 (2017). https://doi.org/10.1186/s12891-017-1672-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-017-1672-4