Abstract
Purpose
Following posterior cruciate ligament (PCL) rupture, autografts and allografts are routinely used for its reconstruction. This study investigated the efficacy and safety of allografts for primary PCL reconstruction, comparing them to autografts in terms of patient-reported outcome measures (PROMs), functional tests, and complications.
Methods
This study followed the PRISMA guidelines. PubMed, Web of Science, Google Scholar, Embase, and Scopus were accessed in October 2022. All the clinical studies investigating the outcomes of primary PCL reconstruction using allografts, or comparing the outcomes of allografts versus autografts, were accessed. The outcomes of interests were: instrumental laxity, range of motion (ROM), Telos stress radiography, drawer test, International Knee Documentation Committee (IKDC), Tegner Activity Scale, and the Lysholm Knee Scoring Scale. Data on complications were also recorded.
Results
A total of 445 patients were included. The mean follow-up was 45.2 ± 23.8 months. The mean age of the patients was 30.6 ± 2.2 years. The time span between the injury and surgical intervention was 12.9 ± 10 months. Overall, 28% (125 of 445 patients) were women. Good baseline comparability was found between the two cohorts. No difference was found in terms of Lysholm Score, ROM, Tegner Scale, IKDC, arthrometer laxity, drawer test, and Telos stress radiography. No difference was found in the rates of anterior knee pain and revision.
Conclusion
Allografts can be considered a suitable alternative to autografts for PCL reconstruction.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The posterior cruciate ligament (PCL) provides primary stabilization for posterior tibial translation over the femur [7, 36, 46, 58]. The PCL is typically injured by a high-energy trauma directed posteriorly to the proximal tibia with the flexed knee, an event which typically occurs in traffic accidents or contact sports practice [37, 55]. Sport-specific PCL injuries incidence ranges from 1 to 4% [3]. The PCL has better healing capability and greater strength than the anterior cruciate ligament [17, 60]. Indeed, PCL tears can be managed conservatively when up to 10 mm of posterior knee translation is present [1]. However, surgical PCL reconstruction may be necessary in patients with greater laxity associated with instability [38, 54]. Both autografts and allografts have been employed for PCL reconstruction [4, 46, 53]. In 2018, Belk et al. [4] performed a systematic review including five studies [2, 27, 31, 52] comparing allografts versus autografts for PCL reconstruction. Since then, further available studies have not yet been considered for systematic reviews [13, 21, 33, 47, 48, 56, 57, 59, 60].
The present study investigated the role of allografts for primary PCL reconstruction, comparing them to autografts in terms of patient-reported outcome measures (PROMs) and functional tests. It was hypothesized that allografts and autografts achieve similar outcome following reconstruction of the PCL.
Materials and methods
Search strategy
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA checklist [40]. The PICOT algorithm was primarily developed:
-
P (Population): PCL tears;
-
I (Intervention): PCL reconstruction;
-
C (Comparison): allograft versus autograft;
-
O (Outcomes): joint instability, PROMs.
-
T (Timing): minimum 12 months follow-up.
Data source and extraction
Two authors (F.M. and A.P.) independently performed the literature search in October 2022. PubMed and Web of Science were accessed. Subsequently, Google Scholar, Embase, and Scopus were accessed to identify further articles. The following keywords were used in combination: knee, posterior cruciate ligament, PCL, tears, injury, surgery, reconstruction, allograft, autograft, instability, BPTB, Achilles, hamstring, tibialis anterior, quadriceps, laxity, patient-reported outcome measures, PROMs, laxity, stability, complication, anterior knee pain, failure, revision. The same authors independently performed the initial screening of the resulting titles. If title and abstract matched, the article full-text was accessed. The bibliographies of the full-text articles were also screened. Disagreements were solved by a third author (N.M.).
Eligibility criteria
All the clinical studies investigating the outcomes of primary PCL reconstruction using allografts, or comparing the outcomes of allografts versus autografts, were accessed. Given the authors’ language capabilities, articles in English, German, Italian, French, and Spanish were included. Studies of level I–IV of evidence, according to Oxford Centre of Evidence-Based Medicine [23], were considered. Editorials, cohort studies, reviews, technical notes, narrative reviews, expert opinion, and letters were excluded. Animal, biomechanics, and cadaveric studies were also excluded. Articles combining PCL reconstruction with ACL reconstruction were excluded. Articles reporting data on revision settings were not considered. Only articles reporting quantitative data under the outcomes of interest were considered for inclusion.
Data extraction
Two authors (F.M. and A.P.) independently performed data extraction. Study generalities (author, year, journal, type of study) and patient baseline demographic information (number of samples with related gender and mean age, time span between the injury and the index surgery, length of the follow-up) were collected. The following data were retrieved at last follow-up for both grafts: (1) functional tests: instrumental laxity, range of motion (ROM), Telos stress radiography, drawer test; (2) PROMs: International Knee Documentation Committee (IKDC), Tegner Activity Scale, Lysholm Knee Scoring Scale; (3) complications. The instrumental laxity was evaluated using the arthrometers KT-1000 or KT-2000 (MEDmetric Corp, San Diego, California). Both these devices applied a posterior translation force of 134 N on the tibial plateau over the femur condyles.
Methodology quality assessment
For the methodological quality assessment, the Coleman Methodology Score (CMS) was used. The CMS is widely used to evaluate the methodological quality of scientific articles for systematic reviews and meta-analyses [12]. This score analyses the included papers under several items, including study size, length of the follow-up, surgical approach, type of study, and the description of diagnosis, surgical technique, and rehabilitation. Additionally, outcome criteria assessment, procedures for assessing outcomes, and the subject selection process are also evaluated. The CMS rates articles with values comprised between 0 (poor) and 100 (excellent). A mean value greater than 60 points is considered satisfactory.
Statistical analysis
All statistical analyses were performed by the main author (F.M.). All the studies reporting the outcomes of PCL reconstruction using allografts were compared to autografts. Data from autografts were obtained from the included studies which compared between the two grafts. Continuous variables were analysed using the mean difference (MD) effect measure. The Student t test was performed, with values of P < 0.05 considered statistically significant. The odds ratio (OR) effect measure was used to investigate the rate of complications, with values of the \(\chi\)2 test < 0.05 considered statistically significant. Studies that directly compared allografts versus autografts which also reported measure of data dispersion (standard deviation or confidence interval) were included in the meta-analysis. The meta-analyses were performed using the Review Manager Software 5.3 (The Nordic Cochrane Collaboration, Copenhagen). The inverse variance was adopted for continuous variables, with MD effect measure. Dichotomous data were evaluated through a Mantel–Haenszel analysis, with OR effect measure. The comparisons were performed with a fixed model effect as set up. Heterogeneity was assessed through the Higgins-I2 test. If I2 test > 50%, high heterogeneity was detected. In cases of heterogeneity, a random model effect was used. The confidence intervals (CI) were set at 95% in all comparisons. The overall effect was considered statistically significant if P < 0.05. The funnel plot of the most commonly reported outcome was performed to assess the risk of publication bias. Egger’s linear regression was performed through the STATA MP Software version 16 (StataCorp, College Station, USA) to assess funnel plot asymmetry, with values of P < 0.05 indicating statistically significant asymmetry.
Results
Search result
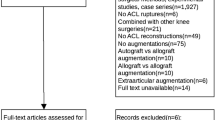
The literature search identified 122 articles comparing allografts versus autografts for primary posterior cruciate ligament reconstruction. Of these, 30 duplicates were excluded. An additional 67 articles were excluded because of the following reasons: revision setting (n = 4), type of study (N = 50), combined with ACL reconstruction (N = 7), combined allografts and allografts (N = 6). An additional 15 articles were excluded because they lacked quantitative data under the outcomes of interest. This left 10 comparative studies for inclusion: 7 retrospective studies, and three prospective studies (Fig. 1).
Methodological quality assessment
The CMS identified some limitations and strengths in the present study. The study size and the length of the follow-up were adequate in most of studies. Surgical approach, diagnosis, and rehabilitation protocols were generally well described. Outcome measures and timing of assessment were often well defined, providing moderate reliability. The procedures for assessing outcomes and subject selection were often biased and not satisfactorily described. Concluding, the CMS for the articles was 66 points, attesting the acceptable quality of the methodological quality assessment.
Risk of publication bias
The funnel plot of the most reported outcome was performed (Fig. 2). The graph evidenced minimal asymmetry in the referral point disposition. However, the Egger’s test did not evidence any statistically significant asymmetry (P = n.s.). In conclusion, the risk of publication bias was low to moderate.
Patient demographics
A total of 445 patients were included. The mean follow-up was 45.2 ± 23.8 months. The mean age of the patients was 30.6 ± 2.2 years. The time span between the injury and surgery was 12.9 ± 10 months. Overall, 28% (125 of 445 patients) were women. Good baseline comparability was found between the two cohorts in terms of mean age, length of the follow-up, time span between the injury and the surgical intervention. The demographics of the included studies is shown in Table 1.
Outcomes of interest
No difference was found between allografts and autografts in Lysholm Score, ROM, Tegner Activity Scale, IKDC, arthrometer laxity, drawer test, and Telos stress radiography. These results are shown in greater detail in Table 2.
Complications
No difference was found in the rate of anterior knee pain and revision. These results are shown in greater detail in Table 3.
Meta-analyses
Five studies [2, 31, 52, 56, 59] compared directly allografts versus autografts and were included in the meta-analysis. No difference was found in Lysholm Score, ROM mean, Tegner Activity Scale, and arthrometer laxity. The forest plots of the comparisons included in the meta-analysis are shown in Fig. 3.
Discussion
The main finding of the present study is that allografts demonstrated similar outcome to autografts for PCL reconstruction. No differences were observed in functional tests (arthrometer laxity, ROM, Telos stress, drawer test), PROMs (IKDC, Lysholm Knee Scoring Scale) and activity levels according to the Tegner Activity Scale. Only one revision over 445 procedures was reported (0.2%). The PCL is the strongest of the knee ligaments, approximately twice as strong as the ACL [26], and revision procedures following its reconstruction are rare. Future clinical studies providing longer follow-up are required to investigate possible difference in graft survivorship.
Semitendinosus, gracilis, bone–patellar tendon–bone (BPTB), and quadriceps autografts are commonly used for PCL reconstruction [5, 8,9,10,11, 14,15,16, 18, 20, 24, 35, 42, 44, 51, 62]. Among allografts, given its length and thickness, the Achilles tendon is commonly employed for PCL reconstruction [31]. Hamstring, tibialis anterior, and BPTB allografts have also been used [29, 39, 43, 50, 61]. Advantages of allografts include a shorter surgical duration, no donor site morbidity, and the choice of desired graft length and thickness. On the other hand, allografts have high costs, potential risk of disease transmission, the possibility of graft versus host reaction, and potential early deterioration deriving from sterilization methods [29, 39, 43, 50, 61]. After implantation, autografts undergo incorporation and remodelling, developing characteristics similar to the native ligament [34, 45]. This process of “ligamentization” is minimal or absent in allografts [30]. A recent systematic review investigated factors influencing the biomechanical properties of allografts [28]. High-dose irradiation for sterilization purposes decreased tensile strength and stiffness compared to low-dose protocols [28]. Further, prolonged freezing impaired the load to failure, ultimate stress and ultimate strain of grafts. Several chemical sterilization measures also negatively affect the biomechanical properties [28]. Surgeons must be aware of the processes that allografts underwent, to better adapt the PCL reconstruction to individual patients.
A recent systematic review including five studies (132 patients) compared allografts versus autografts for PCL reconstruction [4]. They found greater anteroposterior knee laxity in the allograft group with similar Lysholm, IKDC, and Tegner scores, concluding that probably both grafts provide similar outcomes [4]. To date, there is no consensus with regard to the graft choice for primary PCL reconstruction, and the graft source relates to the surgeon preferences. Different autografts have been used for PCL reconstruction [5, 8,9,10,11, 14,15,16, 18, 20, 24, 35, 42, 44, 51, 62]. Setyawan et al. [51] described PCL reconstruction using peroneus longus tendon autograft with good functional outcomes and preservation of ankle function at 2 years follow-up. Recently, Rhatomy et al. [49] compared peroneus longus versus hamstring autografts, reporting excellent postoperative knee functional outcome scores for both groups. The maximum strength of hamstring tendon autograft is comparable to the biomechanical proprieties of patellar tendon autograft [22]. However, some concerns have been reported with the use of BPTB, including anterior knee pain, kneeling pain, risks of patellar fracture and weakening of the extensor mechanism, which acts as a synergist to the PCL [22]. Lin et al. [32] found that both hamstring and BPTB autografts achieved similar good clinical outcome; however, the latter evidenced greater rates of kneeling, squatting, and anterior knee pain [32]. Achilles tendon, tibialis anterior and posterior, BTPB, and hamstring tendons are commonly used as allografts [29, 31, 39, 43, 50, 61]. Achilles tendon allografts are expensive and not always available [6, 41]. Quadriceps allograft could be also considered a good alternative to the Achilles allograft for PCL reconstruction [25]. Achilles and quadriceps allografts for PCL reconstruction demonstrated similar clinical outcomes [25]. In a biomechanical study, Achilles allografts showed more similar biomechanical characteristics of a native PCL compared to quadriceps allografts [19].
The findings of the present study must be interpreted with some limitations. The relatively small number of studies available for inclusion represents an important limitation. Further, 76% (10 of 13 included studies) were retrospective, increasing the risk of selection bias. Moreover, the analyses were conducted irrespective of the source and the strands of the grafts. The current literature lacks prospective analyses with blinding or sample randomization. The eligibility criteria and the procedure protocols were often biased and small between-study differences were evidenced. Allografts must be increased for revision PCL reconstruction, but there is no evidence yet to recommend allografts compared to autograft for primary PCL reconstruction.
Conclusion
Allografts are an effective and safe alternative to autografts in PCL reconstruction.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
Abbreviations
- PCL:
-
Posterior cruciate ligament
- PROMs:
-
Patient-reported outcome measures
- ROM:
-
Range of motion
- IKDC:
-
International Knee Documentation Committee
References
Agolley D, Gabr A, Benjamin-Laing H, Haddad FS (2017) Successful return to sports in athletes following non-operative management of acute isolated posterior cruciate ligament injuries: medium-term follow-up. Bone Jt J 99-B:774–778
Ahn JH, Yoo JC, Wang JH (2005) Posterior cruciate ligament reconstruction: double-loop hamstring tendon autograft versus Achilles tendon allograft–clinical results of a minimum 2-year follow-up. Arthroscopy 21:965–969
Bedi A, Musahl V, Cowan JB (2016) Management of posterior cruciate ligament injuries: an evidence-based review. J Am Acad Orthop Surg 24:277–289
Belk JW, Kraeutler MJ, Purcell JM, McCarty EC (2018) Autograft versus allograft for posterior cruciate ligament reconstruction: an updated systematic review and meta-analysis. Am J Sports Med 46:1752–1757
Boutefnouchet T, Bentayeb M, Qadri Q, Ali S (2013) Long-term outcomes following single-bundle transtibial arthroscopic posterior cruciate ligament reconstruction. Int Orthop 37:337–343
Bullis DW, Paulos LE (1994) Reconstruction of the posterior cruciate ligament with allograft. Clin Sports Med 13:581–597
Chahla J, Williams BT, LaPrade RF (2020) Posterior cruciate ligament. Arthroscopy 36:333–335
Chan YS, Yang SC, Chang CH, Chen AC, Yuan LJ, Hsu KY et al (2006) Arthroscopic reconstruction of the posterior cruciate ligament with use of a quadruple hamstring tendon graft with 3- to 5-year follow-up. Arthroscopy 22:762–770
Chen CH, Chen WJ, Shih CH (1999) Arthroscopic posterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arch Orthop Trauma Surg 119:86–88
Chen CH, Chen WJ, Shih CH, Chou SW (2004) Arthroscopic posterior cruciate ligament reconstruction with quadriceps tendon autograft: minimal 3 years follow-up. Am J Sports Med 32:361–368
Chen CH, Chuang TY, Wang KC, Chen WJ, Shih CH (2006) Arthroscopic posterior cruciate ligament reconstruction with hamstring tendon autograft: results with a minimum 4-year follow-up. Knee Surg Sports Traumatol Arthrosc 14:1045–1054
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 10:2–11
Cooper DE, Stewart D (2004) Posterior cruciate ligament reconstruction using single-bundle patella tendon graft with tibial inlay fixation: 2- to 10-year follow-up. Am J Sports Med 32:346–360
Cury Rde P, Mestriner MB, Kaleka CC, Severino NR, de Oliveira VM, Camargo OP (2014) Double-bundle PCL reconstruction using autogenous quadriceps tendon and semitendinous graft: surgical technique with 2-year follow-up clinical results. Knee 21:763–768
Cury RP, Castro Filho RN, Sadatsune DA, do Prado DR, Goncalves RJ, Mestriner MB (2017) Double-bundle PCL reconstruction using autologous hamstring tendons: outcome with a minimum 2-year follow-up. Rev Bras Ortop 52:203–209
Deehan DJ, Salmon LJ, Russell VJ, Pinczewski LA (2003) Endoscopic single-bundle posterior cruciate ligament reconstruction: results at minimum 2-year follow-up. Arthroscopy 19:955–962
Deng Z, Li Y, Lin Z, Zhu Y, Zhao R (2017) The biomechanical and histological effects of posterior cruciate ligament rupture on the medial tibial plateau. J Orthop Surg Res 12:48
Fanelli GC, Edson CJ (2004) Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2- to 10-year follow-up. Arthroscopy 20:339–345
Forsythe B, Haro MS, Bogunovic L, Collins MJ, Arns TA, Trella KJ et al (2016) Biomechanical evaluation of posterior cruciate ligament reconstruction with quadriceps versus achilles tendon bone block allograft. Orthop J Sports Med 4:2325967116660068
Garofalo R, Jolles BM, Moretti B, Siegrist O (2006) Double-bundle transtibial posterior cruciate ligament reconstruction with a tendon-patellar bone-semitendinosus tendon autograft: clinical results with a minimum of 2 years’ follow-up. Arthroscopy 22(1331–1338):e1331
Hermans S, Corten K, Bellemans J (2009) Long-term results of isolated anterolateral bundle reconstructions of the posterior cruciate ligament: a 6- to 12-year follow-up study. Am J Sports Med 37:1499–1507
Hoher J, Scheffler S, Weiler A (2003) Graft choice and graft fixation in PCL reconstruction. Knee Surg Sports Traumatol Arthrosc 11:297–306
Howick J CI, Glasziou P, Greenhalgh T, Carl Heneghan, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford CEBM Levels of Evidence. Oxford Centre for Evidence-Based Medicine. Available at https://www.cebm.net/index.aspx?o=5653
Jackson WF, van der Tempel WM, Salmon LJ, Williams HA, Pinczewski LA (2008) Endoscopically-assisted single-bundle posterior cruciate ligament reconstruction: results at minimum ten-year follow-up. J Bone Joint Surg Br 90:1328–1333
Kang SH, Sohn KM, Lee DK, Lee BH, Yang SW, Wang JH (2020) Arthroscopic posterior cruciate ligament reconstruction: the achilles tendon allograft versus the quadriceps tendon allograft. J Knee Surg 33:553–559
Kannus P, Bergfeld J, Jarvinen M, Johnson RJ, Pope M, Renstrom P et al (1991) Injuries to the posterior cruciate ligament of the knee. Sports Med 12:110–131
Kim SJ, Kim HK, Kim HJ (1999) Arthroscopic posterior cruciate ligament reconstruction using a one-incision technique. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199902000-00017156-166
Lansdown DA, Riff AJ, Meadows M, Yanke AB, Bach BR Jr (2017) What factors influence the biomechanical properties of allograft tissue for ACL reconstruction? A systematic review. Clin Orthop Relat Res 475:2412–2426
LaPrade RF, Cinque ME, Dornan GJ, DePhillipo NN, Geeslin AG, Moatshe G et al (2018) Double-bundle posterior cruciate ligament reconstruction in 100 patients at a mean 3 years’ follow-up: outcomes were comparable to anterior cruciate ligament reconstructions. Am J Sports Med 46:1809–1818
Levitt RL, Malinin T, Posada A, Michalow A (1994) Reconstruction of anterior cruciate ligaments with bone-patellar tendon-bone and achilles tendon allografts. Clin Orthop Relat Res 303:67–78
Li B, Wang JS, He M, Wang GB, Shen P, Bai LH (2015) Comparison of hamstring tendon autograft and tibialis anterior allograft in arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 23:3077–3084
Lin YC, Chen SK, Liu TH, Cheng YM, Chou PP (2013) Arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction using patellar tendon graft compared with hamstring tendon graft. Arch Orthop Trauma Surg 133:523–530
MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF (2006) Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy 22:320–328
Malinin TI, Levitt RL, Bashore C, Temple HT, Mnaymneh W (2002) A study of retrieved allografts used to replace anterior cruciate ligaments. Arthroscopy 18:163–170
Matthews IT (2002) Antibodies for neoplastic disease solid tumors. Mol Biotechnol 21:91–97
Migliorini F, Pintore A, Spiezia F, Oliva F, Hildebrand F, Maffulli N (2022) Single versus double bundle in posterior cruciate ligament (PCL) reconstruction: a meta-analysis. Sci Rep 12:4160
Migliorini F, Pintore A, Vecchio G, Oliva F, Hildebrand F, Maffulli N (2022) Hamstring, bone-patellar tendon-bone, quadriceps and peroneus longus tendon autografts for primary isolated posterior cruciate ligament reconstruction: a systematic review. Br Med Bull 142:23–33
Migliorini F, Pintore A, Vecchio G, Oliva F, Hildebrand F, Maffulli N (2022) Ligament advanced reinforcement system (LARS) synthetic graft for PCL reconstruction: systematic review and meta-analysis. Br Med Bull 143:57–68
Min BH, Lee YS, Lee YS, Jin CZ, Son KH (2011) Evaluation of transtibial double-bundle posterior cruciate ligament reconstruction using a single-sling method with a tibialis anterior allograft. Am J Sports Med 39:374–379
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Nemzek JA, Arnoczky SP, Swenson CL (1996) Retroviral transmission in bone allotransplantation. The effects of tissue processing. Clin Orthop Relat Res 324:275–282
Norbakhsh ST, Zafarani Z, Najafi A, Aslani H (2014) Arthroscopic posterior cruciate ligament reconstruction by using hamstring tendon autograft and transosseous screw fixation: minimal 3 years follow-up. Arch Orthop Trauma Surg 134:1723–1730
Nyland J, Hester P, Caborn DN (2002) Double-bundle posterior cruciate ligament reconstruction with allograft tissue: 2-year postoperative outcomes. Knee Surg Sports Traumatol Arthrosc 10:274–279
Ochiai S, Hagino T, Senga S, Yamashita T, Haro H (2019) Treatment outcome of reconstruction for isolated posterior cruciate injury: subjective and objective evaluations. J Knee Surg 32:506–512
Panni AS, Milano G, Lucania L, Fabbriciani C (1997) Graft healing after anterior cruciate ligament reconstruction in rabbits. Clin Orthop Relat Res 343:203–212
Park HG, Ham HJ (2020) Effect of posteromedial corner injury on stability and second-look arthroscopic findings after posterior cruciate ligament reconstruction using allograft. J Orthop 22:104–108
Rauck RC, Nwachukwu BU, Allen AA, Warren RF, Altchek DW, Williams RJ (2019) Outcome of isolated posterior cruciate ligament reconstruction at mean 6.3-year follow up: a consecutive case series. Phys Sportsmed 47:60–64
Razi M, Ghaffari S, Askari A, Arasteh P, Ziabari EZ, Dadgostar H (2020) An evaluation of posterior cruciate ligament reconstruction surgery. BMC Musculoskelet Disord 21:526
Rhatomy S, Abadi MBT, Setyawan R, Asikin AIZ, Soekarno NR, Imelda LG et al (2020) Posterior cruciate ligament reconstruction with peroneus longus tendon versus hamstring tendon: a comparison of functional outcome and donor site morbidity. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06077-3
Sekiya JK, West RV, Ong BC, Irrgang JJ, Fu FH, Harner CD (2005) Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction. Arthroscopy 21:1042–1050
Setyawan R, Soekarno NR, Asikin AIZ, Rhatomy S (2019) Posterior Cruciate Ligament reconstruction with peroneus longus tendon graft: 2-Years follow-up. Ann Med Surg (Lond) 43:38–43
Sun X, Zhang J, Qu X, Zheng Y (2015) Arthroscopic posterior cruciate ligament reconstruction with allograft versus autograft. Arch Med Sci 11:395–401
Tian P, Hu WQ, Li ZJ, Sun XL, Ma XL (2017) Comparison of autograft and allograft tendons in posterior cruciate ligament reconstruction: a meta-analysis. Medicine (Baltimore) 96:e7434
Vaquero-Picado A, Rodriguez-Merchan EC (2017) Isolated posterior cruciate ligament tears: an update of management. EFORT Open Rev 2:89–96
Vermeijden HD, van der List JP, DiFelice GS (2020) Arthroscopic posterior cruciate ligament primary repair. Sports Med Arthrosc Rev 28:23–29
Wang CJ, Chan YS, Weng LH, Yuan LJ, Chen HS (2004) Comparison of autogenous and allogenous posterior cruciate ligament reconstructions of the knee. Injury 35:1279–1285
Wang R, Xu B, Wu L, Xu H (2018) Long-term outcomes after arthroscopic single-bundle reconstruction of the posterior cruciate ligament: a 7-year follow-up study. J Int Med Res 46:865–872
Xie WQ, He M, He YQ, Yu DJ, Jin HF, Yu F et al (2021) The effects of posterior cruciate ligament rupture on the biomechanical and histological characteristics of the medial collateral ligament: an animal study. J Orthop Surg Res 16:330
Xu M, Zhang Q, Dai S, Teng X, Liu Y, Ma Z (2019) Double bundle versus single bundle reconstruction in the treatment of posterior cruciate ligament injury: a prospective comparative study. Indian J Orthop 53:297–303
Yang JH, Yoon JR, Jeong HI, Hwang DH, Woo SJ, Kwon JH et al (2012) Second-look arthroscopic assessment of arthroscopic single-bundle posterior cruciate ligament reconstruction: comparison of mixed graft versus achilles tendon allograft. Am J Sports Med 40:2052–2060
Yoon KH, Bae DK, Song SJ, Lim CT (2005) Arthroscopic double-bundle augmentation of posterior cruciate ligament using split Achilles allograft. Arthroscopy 21:1436–1442
Zayni R, Hager JP, Archbold P, Fournier Y, Quelard B, Chambat P et al (2011) Activity level recovery after arthroscopic PCL reconstruction: a series of 21 patients with a mean follow-up of 29 months. Knee 18:392–395
Acknowledgements
None.
Funding
Open Access funding enabled and organized by Projekt DEAL. No external source of funding was used.
Author information
Authors and Affiliations
Contributions
AP, FM: literature search, data extraction, methodological quality assessment, writing. FM: statistics. NM, AB, FO, JE: supervision, revision. All the authors approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Migliorini, F., Pintore, A., Oliva, F. et al. Allografts as alternative to autografts in primary posterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 31, 2852–2860 (2023). https://doi.org/10.1007/s00167-022-07258-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07258-y