Abstract
Background
Many people with Whiplash Associated Disorders (WAD) report problems with vision, some of which may be due to impaired eye movements. Better understanding of such impaired eye movements could improve diagnostics and treatment strategies.
This systematic review surveys the current evidence on changes in eye movements of patients with WAD and explains how the oculomotor system is tested.
Methods
Nine electronic data bases were searched for relevant articles from inception until September 2015. All studies which investigated eye movements in patients with WAD and included a healthy control group were screened for inclusion. Qualifying studies were retrieved and independently assessed for methodological quality using the Methodology Checklists provided by the Scottish Intercollegiate Guidelines Network.
Results
Fourteen studies out of 833 unique hits were included. Ten studies reported impaired eye movements in patients with WAD and in four studies no differences compared to healthy controls were found. Different methods of eye movement examination were used in the ten studies: in five studies, the smooth pursuit neck torsion test was positive, in two more the velocity and stability of head movements during eye-coordination tasks were decreased, and in another three studies the cervico-ocular reflex was elevated.
Conclusions
Overall the reviewed studies show deficits in eye movement in patients with WAD, but studies and results are varied. When comparing the results of the 14 relevant publications, one should realise that there are significant differences in test set-up and patient population. In the majority of studies patients show altered compensatory eye movements and smooth pursuit movements which may impair the coordination of head and eyes.
Similar content being viewed by others
Background
People who suffer from chronic ‘Whiplash Associated Disorders’ (WAD) exhibit very distinct complaints [1]. Seventy percent of patients complain of pain, dizziness and unsteadiness [2], while 50 % report problems with vision [3]. These problems with vision comprise concentration problems during reading, sensitivity to light, visual fatigue and eye strain [3]. The severity of problems with vision is higher in traumatic neck pain patients than in non-traumatic neck pain patients [3]. Problems in vision could be due to malfunction of the oculomotor system that is meant to keep the eye on a target [4, 5]. Such oculomotor problems in WAD patients could be related to cervical sensorimotor disorders. The knowledge of cervical induced oculomotor system disorders is still limited [6]. This may be because of the complexity of the cervico-oculomotor system, that includes not only the central nervous system but also the proprioceptive system of the cervical spine (for review see e.g. [7]).
Eye movement control depends on eye position in the head and on the position of the head in space [8]. Head position is determined by integration of several sub-systems such as the vestibular system, visual information and proprioceptive system of the cervical spine [8, 9]. Disturbed afferent cervical information is related to nystagmus, dizziness and deficits in balance [10, 11].
The principal source of cervical afferent information is formed by mechanoreceptors in the upper cervical spine. Specifically in the deep upper cervical muscles (i.e. m. obliquus capitis superior and inferior, m. longus colli), the density of muscle spindles is extremely high compared to other muscles in the body [12, 13]. Muscle spindles are part of the sensorimotor system [14]. In patients with WAD sensorimotor control is disturbed [14–17].
In attempts to reveal the complex relation between cervical sensorimotor disorders and visual problems several studies regarding oculomotor problems in patients with WAD have been published [3, 18–23]. In all studies one of three distinct eye movement types were used to assess oculomotor problems in patients with WAD: eye stabilization reflexes, smooth pursuit eye movements and head-eye coordination.
Eye stabilisation reflexes
Eye stabilization reflexes preserve stable vision on the retina during head movement. At least three eye stabilization reflexes can be distinguished based on their sensory input: the cervico-ocular reflex (COR), the vestibulo-ocular reflex (VOR) and the optokinetic reflex (OKR). These three complementary reflexes have distinct characteristics and receive input from the cervical spine, the vestibulum and the eyes, respectively. The COR receives input from muscle spindles in the cervical spine, especially from the deep upper cervical muscles and joint capsules of C1 to C3 [24]. The central pathways of the VOR and the COR are the same; both reflexes converge at the vestibular nuclei [24]. The OKR pathways, however, are quite distinct from the COR and VOR pathways [25].
Smooth pursuit eye movements
Accurate smooth pursuit is essential to look at a moving object by keeping the retinal image steady within the foveal area. Ideally, smooth pursuit velocity matches the velocity of the moving object. Performing smooth pursuit eye movements properly requires the integration of visual, vestibular and cervical information [26].
Head-eye coordination
Head-eye coordination is the overall result of all systems in control of the visual system. During these tasks, the compensatory eye movements and the motor control of the neck co-operate, requiring integration of saccades, the COR, VOR, OKR and active neck movements.
This systematic review provides an overview of existing evidence on oculomotor system changes in patients with WAD and how this evidence was perceived. We aim to address the question of what is known about changed eye movements in patients with WAD. To our knowledge no reviews of the literature concerning oculomotor problems in patients with WAD have previously been published. Therefore, we present a comprehensive, systematic overview of the literature concerning changed eye movements in patients with WAD compared to healthy controls.
Methods
The PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) were employed in this systematic literature review [27].
Information sources and search parameters
To be as comprehensive as possible, the following databases have been searched until September 2015: Embase, Medline (OvidSP), Web of Science, Scopus, Cinahl, SportDiscus, Cochrane, Pubmed Publisher and Google scholar. Keywords were derived from the research question and transformed to associated and free text words. The search strategy in Embase was based on the following combination of terms: ‘cornea reflex’/exp OR ‘eye movement’/exp OR ‘eye movement disorder’/de OR ‘oculomotor system’/de OR ‘extraocular muscle’/de OR (((cornea* OR eye* OR ocular* OR cervicoocul* OR visual*) NEAR/6 (reflex* OR movement* OR pursuit* OR motilit* OR track*)) OR oculomotor* OR ((extraocular* OR ocular* OR eye*) NEAR/3 muscle*) OR ‘smooth pursuit’ OR (tracking NEAR/3 (perform* OR task*))):ab,ti) AND (‘neck pain’/de OR ‘neck injury’/de OR ‘whiplash injury’/exp OR (((neck OR cervic* OR colli OR collum*) NEAR/6 (pain* OR hyperextension* OR ache OR injur* OR disorder* OR trauma* OR lesion* OR bruise*)) OR neckache* OR Cervicalgia* OR Cervicodynia* OR whiplash):ab,ti).
In addition, Medline (OvidSP), Web of Science, Scopus, Cinahl, SportDiscus, Cochrane, Pubmed Publisher and Google scholar were similarly searched with their own thesaurus used for indexing articles and free entries.
Study selection
For inclusion in the systematic review the following criteria had to be met: (1) participants in the study had to be 18 years or older; (2) patients had to have Whiplash Associated Disorders; (3) one of the outcome measures in the study had to be eye movements; (4) control subjects were healthy individuals; (5) the article was written in English, Dutch or German; (6) the original article was available in full text.
Data items and collection
Information was extracted from the included articles and presented in the evidence table (Table 1), regarding (1) study, (2) sample size, (3) characteristics of the patients, (4) testing device for eye movements, (5) eye movements testing protocol, (6) results and (7) possible bias.
Risk of bias in individual studies
The validity and risk of bias of the included articles was checked by using the “Methodology Checklist 4: Case–control studies” version 2.0 and “Methodology Checklist 3: Cohort studies” version 3.0 provided by the Scottish Intercollegiate Guidelines Network (SIGN). The risk of bias table is presented in Table 2. The appraisal of the articles was based on the description of the internal validity, i.e. the selection of subjects, exclusion of selection bias, clear definition of outcomes, blinding of assessors, reliable assessment of exposure, identification of potential confounders and provision of confidence intervals. For the studies the grading score has been set from “Low quality” (0), “Acceptable” (+) or “High quality” (++). In the present review, only articles graded as “Acceptable” or “High quality” were included. This criterion was set a priori.
Methodological quality of the included articles was assessed blindly and independently by authors BI and JV. After both researchers appraised the selected articles, results were compared and any differences discussed after screening the article a second time.
Results
Study selection
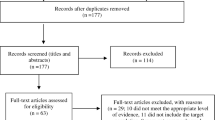
A total of 833 studies were identified. As shown in Fig. 1, 14 studies remained after two screening phases.
In the first phase all articles were screened on relevance of the title and abstract. Twenty-one of the included studies remained after the first screening. These studies met the inclusion criteria, according to the title and abstract. After the first full-text reading, two researchers agreed on 19 of the 21 studies. Seven of these 19 studies were excluded because they did not fulfil the inclusion criteria, regarding the participants [28–30] or the outcome parameter [3, 18, 31, 32].
In two studies, the reviewers disagreed on the validity of the measurement protocol [33, 34]. After a second reading and comparison of the differences, the researchers reached consensus. Both studies were included, resulting in 14 included studies.
The methodological quality of all of the included studies was “acceptable” (+) according to the SIGN criteria checklist. This implies some weaknesses in the study, with an associated risk of bias. Most studies used rather small and heterogeneous populations (e.g. the time after accident of the patients varied from 1 month to 7 years [33, 35]). There was also limited information concerning raw data, possible confounders and patient characteristics (e.g. pain, anxiety and disability).
Study characteristics
The characteristics of the data that were extracted from the included studies (study, sample size, characteristics of the patients, eye movement testing instrument, testing protocol, results, and possible bias) are presented in Table 1.
Thirteen studies were case control studies and one was a cohort study [20].
Nine studies used the classification of the Quebec Task Force on Whiplash Associated Disorders (WAD) [16, 20–23, 34–37]. In these studies patients were included with WAD grade 1 (complaints of neck pain, stiffness or tenderness only without physical signs that are noted by an examining physician), grade 2 (complaints of neck pain and musculoskeletal signs, such as a decreased range of motion and point tenderness in the neck) or grade 3 (includes additional signs such as decreased or absent deep tendon reflexes, weakness, and sensory deficits) [38].
All 14 studies included a healthy control group.
Outcome measures
The principal outcome measure of the current review was eye movements, being the main subject of investigation in all included studies. However, different tests for eye movements were used among the included studies. The different tests were: (1) tests for head-eye coordination, integrating compensatory eye movements and neck movement tests; (2) smooth pursuit tests and (3) compensatory eye movement tests, including the VOR and the COR. Also for these three different tests, two different eye movement measurement techniques were used: electro-oculography and video-oculography.
Head-eye coordination
In two studies several parameters concerning the head-eye coordination were tested using two different tests [19, 39]. One of the tests was gaze stability during active head rotation. The other test was the sequential head and eye movement (SHEM) test. During the gaze stability test, the subject has to keep the eyes focussed on a point straight ahead while rotating the neck actively. During the SHEM test, the subject has to move the eyes first to one side, followed by an active head motion. Subsequently the subject first moves the eyes and then the head back to the starting position. During these tasks the compensatory eye movements and the motor control of the neck co-operate, requiring integration of saccades, the COR, VOR, OKR and active neck movements. In both tasks the patients executed the head movements slower compared to controls. During the gaze stability test, head range of motion was smaller in patients.
Smooth pursuit eye movements
Nine studies used smooth pursuit eye movements with a large variety in patient selection and study set-up (for details see Table 1) [16, 20, 33–37, 40, 41]. This variety complicates proper comparison of the studies. In addition, in some studies set-up information is incomplete. The evidence table (Table 1) shows possible bias of each selected study.
One study tested the smooth pursuit eye movements in neutral position only and not in a torsioned neck position. However they used two different velocities [20]. When tested with 20°/s only two, and with 30°/s five of the 26 patients were classified with dysfunctional gain (i.e. the ratio between the movement of the eyes and the movement of the stimulus).
In all other studies, using varying velocities between 18°/s and 37°/s, in contrast to the first study, the influence of a relative rotated cervical spine (head stationary, trunk turned) on the smooth pursuit eye movement was tested (smooth pursuit neck torsion (SPNT) test) [16, 33–37, 40, 41].
In four of the eight studies the primary outcome parameter (‘SPNTdiff’ the difference between the gain in neutral and in relatively rotated position) was significantly higher in patients compared to healthy controls (WAD 0.14/0.11/0.08/0.12, controls 0.02/0.01/0.02/0.02) [34, 37, 40, 41]. All four mentioned studies manually analysed the data and excluded all blinks and square waves [34, 37, 41] and saccades [40]. Three other studies did not find any differences between cases and controls [33, 35, 36]. In the later three studies the data was analysed fully-automated [33, 36] and one study does not provide information about the analysis [34].
Another study provided only the number of patients with an altered SPNTdiff compared to controls, but did not provide the median values of the smooth pursuit gain [16]. In one study with a semi-automated analysis the SPNT difference of patients with WAD was larger for predictably moving targets compared to unpredictably moving targets. This difference was not seen in healthy controls and patients with non-traumatic neck pain [40].
Eye stabilization reflexes
In three studies the COR and the VOR were measured [21–23]. These eye stabilization reflexes were tested in a custom setting with an infrared eye tracking device in a darkened room (further description of the measurement method in [42]). All studies reported a significantly higher COR gain in patients with WAD. One study described that both the COR and VOR gain could adapt in healthy controls, but not in patients [22].
In summary, as shown in Table 1, ten of the fourteen studies reported differences between patients with WAD and healthy controls [16, 19, 21–23, 34, 37, 39–41]. Velocity of eye movements is decreased and eye movements are less coordinated in patients than in healthy controls. In five of the eight studies which used the SPNT test, the smooth pursuit movements in the neck-rotated position were slower in the patient group compared to the healthy controls [16, 34, 37, 40, 41]. In all five studies which used the tests for eye stabilization reflexes and the head-eye coordination tests, the WAD group performed worse than the healthy control group [19, 21–23, 39]. In the discussion section we will discuss extensively the variety of outcome parameters in the tests for oculomotor deficits. Generally, patients with WAD had an elevated COR and had more problems in stabilizing the head and gaze during stability tasks and sequential movement tasks.
The differences and possible shortcomings of all studies are summarized in Tables 1 and 2. Four studies did not find differences between patients and healthy controls [20, 33, 35, 36]. All four studies analyzed smooth pursuit movements. In these studies the way of data analysis varied (two times fully automated, one time semi-automated and one time not specified), which was mentioned in one study as possible reason [36]. It is also noteworthy that the studied population was very heterogeneous or insufficiently described. Two studies mentioned this differences in symptom severity of the patient group and also attentional deficits of the patients as possible reasons [33, 35]. Heikkilä et al. found differences in patients after a whole battery of oculomotor tests, but no differences in the smooth pursuit test alone [20]. In general, most studied studies lack details in the description of patient characteristics [16, 20–23, 33–35, 39–41]. Heterogeneity in patient population may be an important factor in confounding the results of eye movement tests.
Discussion
The current review provides an overview of present knowledge on altered eye movements in WAD patients. The majority of studies in this review confirm the possibility of eye movement impairments in WAD patients. This underlines the necessity to include an examination of eye movement impairments in the diagnostic process of patients with WAD. There are various methods that address different aspects of eye movement. The 14 studies included in this review are evaluated by the specific aspect of oculomotor problems that are tested, their clinical applicability and test validity.
Head-eye coordination
Two studies used a series of tests to analyse the head-eye coordination [19, 39]. The purpose of this method is to evaluate over-all head-eye coordination disturbances. This method does not allow discrimination as to which part of the system is causing the actual disturbance. The head-eye coordination tests were developed for clinical use, are well described and relatively easy to execute. However, due to the requirement of active cervical movements and the combination of cervical, vestibular and visual input, it is not possible to draw specific conclusions about eye movements in isolation. The studies included in this review did not provide substantial information on the validity of this method. However, in another study that was excluded from this review as it was not performed on WAD patients the discriminative validity and reliability were considered sufficient when three out of five test scored positive [43].
Smooth pursuit eye movements
Eight studies focused on smooth pursuit eye movements by using the SPNT test [16, 33–37, 40, 41]. The SPNT test is developed for clinical use and eye movements are measured with electro-oculography. One point of concern is the diversity in analysing the recordings. The accuracy, reliability and non-standardized interpretation is a source of bias [36, 44, 45]. In this review the four studies that did not find differences between patients with WAD and healthy subject were all SPNT test studies. This leads to the conclusion that the used analysis of the SPNT test is possibly not optimal and has to be developed. Until then the SPNT test should be used with care in the clinical setting.
In addition, as in the head-eye coordination method, it remains unclear what exactly is causing the recorded disturbance. In a recent study on the SPNT test the question was raised whether confounding factors such as pain experience or impaired cognitive functioning may affect test outcomes [40]. However, Treleaven et al. found no association to SPNT with pain, anxiety, medication, level of disability and time since injury [37]. More research seems to be required into the effect of patient characteristics on eye movements.
Eye stabilization reflexes
Solitary cervical induced eye movements were investigated in three studies. These studies focused on eye stabilization reflexes and measured the COR in isolation. COR gain was measured without influence of visual, vestibular or cervical motor information [21–23]. Therefore it is impossible to influence COR gain deliberately, which makes the COR an objective outcome measure of oculomotor function. However, the experimental setup for the COR test is complex and it is necessary to perform the test in a completely darkened room.
A future challenge would be the conversion of the existing test into a less expensive and easy to perform test, suitable for the clinical practice. Recording of eye stabilization reflexes is relatively new. The present studies provide little information on validity of the test.
In general, comparing all three methods in one patient group may clarify which methods are most applicable to evaluate oculomotor problems in patients with WAD. At present head-eye coordination measurements seem the most suitable for clinical use. Particularly when training head-eye disturbances is used as therapeutic intervention. When a test comprises multiple (sub-) systems, it remains difficult to determine the most important factor in the observed change. However, this knowledge is necessary for successful treatment of the patient. To enhance therapeutic interventions, more insight in aetiological relations between WAD and oculomotor dysfunction is essential. At present, eye stabilization reflexes, more than the smooth pursuit method, may enhance our comprehension of the complex interaction between the cervico-oculomotor system and the coherence of neck pain symptoms. The used methodology of the SPNT test varies widely. Before using the smooth pursuit neck torsion test, more research is required into the methodology and specifically the method of analysis. In general, the SPNT test has the best potential for differential diagnosis compared to eye head coordination.
Conclusion
In the majority of studies included in this review, patients show altered eye reflexes and smooth pursuit movements which may impair the coordination of head and eyes.
In this review three methods of eye movement examination are found. The used methods and the patient populations significantly differ. At present there is not one single test that provides the required information. A specific combination of tests may be more suitable to properly determine eye motion.
At the present time, the head-eye coordination tests may be the most suitable method for clinical use. Further studies of eye stabilization reflexes can help to clarify the aetiology of oculomotor problems in patients with WAD. More research into the methodology of the SPNT test is required to evaluate the clinical value.
Abbreviations
- COR:
-
Cervico-ocular reflex
- OKR:
-
Optokinetic reflex
- SHEM:
-
Sequential head and eye movement
- SIGN:
-
Scottish Intercollegiate Guidelines Network
- SPNT:
-
Smooth pursuit neck torsion
- SPNTdiff:
-
The difference between the gain in neutral and in relatively rotated position
- VOR:
-
Vestibulo-ocular reflex
- WAD:
-
Whiplash associated disorders
References
Curatolo M, Bogduk N, Ivancic PC, McLean SA, Siegmund GP, Winkelstein BA. The role of tissue damage in whiplash-associated disorders: discussion paper 1. Spine (Phila Pa 1976). 2011;36(25 Suppl):S309–15.
Treleaven J, Jull G, Sterling M. Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. J Rehabil Med. 2003;35:36–43.
Treleaven J, Takasaki H. Characteristics of visual disturbances reported by subjects with neck pain. Man Ther. 2014;19:203–7.
Hülse. Klinik der Funktionsstörungen des Kopfgelenkbereiches. In: Hülse M, Neuhuber WL WH, editors. Der kranio-zervikale Übergang. Berlin: Sprin; 1998. p. 43–97.
Wolff H. Störungen des kraniozervikalen Übergang (Kopfgelenkbereich). In: Wolff H, editor. Neurophysiologische Aspekte des Bewegungssystems. Berlin: Springer; 1996.
Westergren H, Freeman MD, Malmström E-M. The whiplash enigma: still searching for answers. Scand J Pain. 2014;5:226–8.
Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther. 2008;13:2–11.
Corneil BD. The neural base of gaze shifts. In: Liversedge S, Gilchrist I, Everling S, editors. Oxford Handbook on Eye Movements; 2011:1–35.
Treleaven J, LowChoy N, Darnell R, Panizza B. Comparison of sensorimotor disturbance between subjects with persistent whiplash-associated disorder and subjects with vestibular pathology associated with …. Arch Phys … 2008;89:522–30.
Cohen L. Role of eye and neck proprioceptive mechanisms in body orientation and motor coordination. J Neurophysiol. 1961;24:1–11.
Biemond A, Jong JMBVDE. On cervical nystagmus and related disorders. Brain. 1969;92:437–58.
Boyd-Clark LC, Briggs CA, Galea MP. Muscle spindle distribution, morphology, and density in longus colli and multifidus muscles of the cervical spine. Spine (Phila Pa 1976). 2002;27:694–701.
Kulkarni V, Chandy MJ, Babu KS. Quantitative study of muscle spindles in suboccipital muscles of human foetuses. 2001. p. 355–9 (December).
Falla D, Farina D. Neural and muscular factors associated with motor impairment in neck pain. Curr Rheumatol Rep. 2007;9:497–502.
Hodges PW. Pain and motor control: from the laboratory to rehabilitation. J Electromyogr Kinesiol. 2011;21:220–8.
Treleaven J, Jull G, LowChoy N. The relationship of cervical joint position error to balance and eye movement disturbances in persistent whiplash. Man Ther. 2006;11:99–106.
Kristjansson E, Treleaven J. Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009;39:364–377.
Storaci R, Manelli A, Schiavone N, Mangia L. Whiplash injury and oculomotor dysfunctions: clinical–posturographic correlations. Eur Spine … 2006;15:1811–6.
Treleaven J, Jull G, Grip H. Head eye co-ordination and gaze stability in subjects with persistent whiplash associated disorders. Man Ther. 2011;16:252–7.
Heikkilä HV, Wenngren BI. Cervicocephalic kinesthetic sensibility, active range of cervical motion, and oculomotor function in patients with whiplash injury. Arch Phys Med Rehabil. 1998;79:1089–94.
Montfoort I, Kelders WPA, Van Der Geest JN, Schipper IB, Feenstra L, De Zeeuw CI, Frens MA. Interaction between ocular stabilization reflexes in patients with whiplash injury. Invest Ophthalmol Vis Sci. 2006;47:2881–4.
Montfoort I, Van Der Geest JN, Slijper HP, De Zeeuw CI, Frens MA. Adaptation of the cervico- and vestibulo-ocular reflex in whiplash injury patients. J Neurotrauma. 2008;25:687–93.
Kelders WPA, Kleinrensink GJ, van der Geest JN, Schipper IB, Feenstra L, De Zeeuw CI, Frens MA. The cervico-ocular reflex is increased in whiplash injury patients. J Neurotrauma. 2005;22:133–7.
Hikosaka O, Maeda M. Cervical effects on abducens motoneurons and their interaction with vestibulo-ocular reflex. Exp Brain Res. 1973;18:512–30.
Van Die GC, Collewijn H. Control of human optokinetic nystagmus by the central and peripheral retina: effects of partial visual field masking, scotopic vision and central retinal scotomata. Brain Res. 1986;383:185–94.
Lencer R, Trillenberg P. Neurophysiology and neuroanatomy of smooth pursuit in humans. Brain Cogn. 2008;68:219–28.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Mergner T, Schweigart G, Botti F, Lehmann A. Eye movements evoked by proprioceptive stimulation along the body axis in humans. Exp Brain Res. 1998;120:450–60.
Kongsted A, Jorgensen LV, Leboeuf-Yde C, Qerama E, Korsholm L, Bendix T. Are altered smooth pursuit eye movements related to chronic pain and disability following whiplash injuries? A prospective trial with one-year follow-up. Clin Rehabil. 2008;22:469–79.
Treleaven J, Clamaron-Cheers C, Jull G. Does the region of pain influence the presence of sensorimotor disturbances in neck pain disorders? Man Ther. 2011;16:636–40.
Freitag P, Greenlee MW, Wachter K, Ettlin Th M, Radue EW. fMRI response during visual motion stimulation in patients with late whiplash syndrome. Neurorehabil Neural Repair. 2001;15:31–7.
Bexander CSM, Hodges PW. Cervico-ocular coordination during neck rotation is distorted in people with whiplash-associated disorders. Exp Brain Res. 2012;217:67–77.
Dispenza F, Gargano R, Mathur N, Saraniti C, Gallina S. Analysis of visually guided eye movements in subjects after whiplash injury. Auris Nasus Larynx. 2011;38:185–9.
Tjell C, Rosenhall U. Smooth pursuit neck torsion test: a specific test for cervical dizziness. Am J Otol. 1998;19:76–81.
Prushansky T, Dvir Z, Pevzner E, Gordon CR. Electro-oculographic measures in patients with chronic whiplash and healthy subjects: a comparative study. J Neurol Neurosurg Psychiatry. 2004;75:1642–4.
Kongsted A, Jørgensen LV, Bendix T, Korsholm L, Leboeuf-Yde C. Are smooth pursuit eye movements altered in chronic whiplash-associated disorders? A cross-sectional study. Clin Rehabil. 2007;21:1038–49.
Treleaven J, Jull G, LowChoy N. Smooth pursuit neck torsion test in whiplash-associated disorders: relationship to self-reports of neck pain and disability, dizziness and anxiety. J Rehabil Med. 2005;37:219–23.
Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau JSS. Scientific monograph of the quebec task force on whiplash-associated disorders: redefining “whiplash” and its management. Spine (Phila Pa 1976). 1995;20:1S–73S.
Grip H, Jull G, Treleaven J. Head eye co-ordination using simultaneous measurement of eye in head and head in space movements: potential for use in subjects with a whiplash injury. J Clin Monit Comput. 2009;23:31–40.
Janssen M, Ischebeck BK, de Vries J, Kleinrensink G-J, Frens MA, van der Geest JN: Smooth Pursuit Eye Movement Deficits in Patients With Whiplash and Neck Pain are Modulated by Target Predictability. Spine (Phila Pa 1976). 2015;40:E1052–E1057.
Treleaven J, LowChoy N, Darnell R, Panizza B, Brown-Rothwell D, Jull G. Comparison of sensorimotor disturbance between subjects with persistent whiplash-associated disorder and subjects with vestibular pathology associated with acoustic neuroma. Arch Phys Med Rehabil. 2008;89:522–30.
Kelders WPA, Kleinrensink GJ, van der Geest JN, Feenstra L, de Zeeuw CI, Frens MA. Compensatory increase of the cervico-ocular reflex with age in healthy humans. J Physiol. 2003;553(Pt 1):311–7.
Della Casa E, Affolter Helbling J, Meichtry A, Luomajoki H, Kool J. Head-Eye movement control tests in patients with chronic neck pain; inter-observer reliability and discriminative validity. BMC Musculoskelet Disord. 2014;15:16.
Collewijn H. Eye movement recording. In: JG R, editor. Vision research, a practical guide to laboratory methods. 1st edition. Oxford: Oxford University Press; 1999. p. 245–185
Hess CW, Muri R, Meienberg O. Recording of horizontal saccadic eye movements: methodological comparison between electro-oculography and infrared reflection oculography. Neuro Ophthalmol. 1986;6:189–97.
Acknowledgements
The authors wish to thank Wichor Bramer, biomedical information specialist at Erasmus MC, for the support with the literature search.
Funding
We are grateful for the financial support of TC2N (EU Interreg; MF & JG), and Stichting Coolsingel (MF).
Availability of data and materials
This is a review paper and the results and conclusions are made from studies which are all referenced in the manuscript.
Authors’ contributions
BI has been substantially involved in the whole process of conception, design, acquisition and interpretation of the data and writing of the article. JV has made substantial contributions to conception and design, acquisition of data and interpretation of data. JV read all articles and assessed the methodological quality. JG participated in the design of the study and has been involved in drafting the manuscript and revising it critically for important intellectual content. MJ has been involved in drafting the manuscript and revising it critically for important intellectual content. JW has been involved in drafting the manuscript and revising it critically for important intellectual content. GJ participated in the design of the study and helped to draft the manuscript. MF has been involved in drafting the manuscript and revising it critically for important intellectual content. MF has given final approval of the version to be published. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethical approval and consent to participate
Not applicable since this was a systematic literature review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ischebeck, B.K., de Vries, J., Van der Geest, J.N. et al. Eye movements in patients with Whiplash Associated Disorders: a systematic review. BMC Musculoskelet Disord 17, 441 (2016). https://doi.org/10.1186/s12891-016-1284-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-016-1284-4