Abstract
Background
Chronic respiratory diseases, such as chronic obstructive pulmonary disease (COPD) and bronchiectasis, present significant threats to global health. Recent studies have revealed the crucial role of the lung microbiome in the development of these diseases. Pathogens have evolved complex strategies to evade the immune response, with the manipulation of host cellular epigenetic mechanisms playing a pivotal role. There is existing evidence regarding the effects of Pseudomonas on epigenetic modifications and their association with pulmonary diseases. Therefore, this study aims to directly assess the connection between Pseudomonas abundance and chronic respiratory diseases. We hope that our findings will shed light on the molecular mechanisms behind lung pathogen infections.
Methods
We analyzed data from 366 participants, including individuals with COPD, acute exacerbations of COPD (AECOPD), bronchiectasis, and healthy individuals. Previous studies have given limited attention to the impact of Pseudomonas on these groups and their comparison with healthy individuals. Two independent datasets from different ethnic backgrounds were used for external validation. Each dataset separately analyzed bacteria at the genus level.
Results
The study reveals that Pseudomonas, a bacterium, was consistently found in high concentrations in all chronic lung disease datasets but it was present in very low abundance in the healthy datasets. This suggests that Pseudomonas may influence cellular mechanisms through epigenetics, contributing to the development and progression of chronic respiratory diseases.
Conclusions
This study emphasizes the importance of understanding the relationship between the lung microbiome, epigenetics, and the onset of chronic pulmonary disease. Enhanced recognition of molecular mechanisms and the impact of the microbiome on cellular functions, along with a better understanding of these concepts, can lead to improved diagnosis and treatment.
Similar content being viewed by others
Background
The microbiome refers to the collection of microorganisms that live within and on the human body, and it has been shown to have a significant impact on human health and disease [1]. Examining lung diseases from a microbiome perspective is crucial as the human lung is home to a diverse population of microorganisms, collectively known as the lung microbiome [2]. Recent studies have shown that an imbalance in the lung microbiome, known as dysbiosis, can contribute to the development and progression of diseases [3].
By examining the lung microbiome, researchers can identify new targets for therapeutic interventions and gain insight into the complex interactions between the microorganisms, host, and environment that contribute to health and disease [4, 5]. The field of probiotic applications is expanding rapidly, with a focus on their use in managing respiratory tract infections. In a study conducted by Giovanna Batoni and her colleagues, they identified Lactobacillus acidophilus as a promising candidate for further investigation in the development of potential treatments for controlling Pseudomonas aeruginosa infections [6]. Scientists explored the effectiveness of supplementing patients with COPD using Lactobacillus casei Shirota. The findings revealed enhancements in both lung function and quality of life, indicating a possible beneficial role for probiotics in managing COPD [7, 8]. A study by Huang et al. explored the impact of dietary prebiotics, on asthma control. Consumption of prebiotic-rich foods was associated with reduced airway inflammation in asthmatic individuals, highlighting the potential of dietary interventions in asthma management [9].
Fecal microbiota transplantation (FMT) and a high-fiber diet resulted in reduced local and systemic inflammation while also offering protection against alveolar destruction and cellular apoptosis [10]. A deeper understanding of the lung microbiome has the potential to improve our ability to diagnose and treat lung diseases, leading to better outcomes for patients [11]. This is achieved through fecal transplantation from donors whose microbial diversity is well-suited for this purpose. Long Wen et al. found that Pseudomonas aeruginosa leads to a reduction in both the diversity and quantity of gut microbiota in mice with pneumonia, resulting in metabolic imbalances. When fecal microbiota transplantation (FMT) was administered, this situation improved in mice with pneumonia. That helped restore the balance between Treg and Th17 cells, consequently alleviating lung inflammation and injury in mice infected with Pseudomonas aeruginosa pneumonia by regulating gut microbiota and addressing metabolic dysfunction [12].
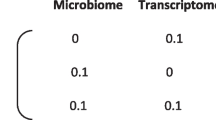
Epigenetics encompasses heritable changes in gene function that occur independently of alterations in the DNA sequence [13, 14]. Types of epigenetic changes include DNA methylation, histone modification, and miRNA regulation [15,16,17]. Epigenetics plays a crucial role in the relationship between the microbiome and lung disease [18, 19]. The microbiome in the lungs is involved in regulating various biological processes such as cell proliferation, differentiation, stress response, and pathogenesis. Studies have shown that certain microRNAs are dysregulated in chronic lung diseases such as COPD, IPF, and CF and may contribute to the development and progression of these diseases by regulating inflammation, cell proliferation, tissue remodeling, and the immune response to infection [14, 17, 18, 20].
In the context of the lung microbiome, epigenetic changes can impact the balance of microorganisms within the lung and lead to dysbiosis, which can contribute to the development and progression of lung diseases. The interplay between the microbiome and the epigenome is intricate and mutually influential [13]. A better understanding of the role of epigenetics in the microbiome-lung disease relationship has the potential to provide new insights into the development and progression of lung diseases, as well as new targets for therapeutic interventions [21].
Pseudomonas is a type of bacteria that can cause respiratory infections and disease in individuals with weakened immune systems, such as those with cystic fibrosis, chronic obstructive pulmonary disease (COPD), or severe asthma [22]. Pseudomonas aeruginosa (P. aeruginosa) infection represents a significant danger to individuals with cystic fibrosis (CF). Within the context of this infection, P. aeruginosa typically inhabits the thickened mucus lining the airways. This mucus not only offers a supportive structure and a nutrient-rich habitat for the bacterium to thrive but also rarely comes into direct contact with the underlying airway epithelial cells [23]. The presence of Pseudomonas in the respiratory tract can disrupt the composition of the respiratory microbiome, resulting in alterations to its typical functions and an elevated susceptibility to respiratory infections [18, 24]. Studies have also shown that Pseudomonas can impact the epigenetic regulation of host cells. These changes in gene expression can contribute to the development and progression of respiratory disease [25].
Aforementioned, the mechanism of pathogens interplay with the lung cells are in the question yet, the role of the epigenetics and the connection of Pseudomonas and epigenetic have been mentioned on the previous studies. Our main goal is to directly investigate the effect of the Pseudomonas pathogen on the COPD as a chronic lung disease. Thus, we compared the composition of the lung microbiome in healthy, COPD, AECOPD, and bronchiectasis subjects using metagenomic data. We categorized the bacteria with high prevalence in each disease and found that the prevalence of the Pseudomonas genus is common in all chronic lung diseases and not in the healthy dataset. Our results beside the previous study could propose the epigenetic changes as the cellular mechanism of Pseudomonas infection however this idea needs more investigations.
Methods
Data acquisition
We carried out a comprehensive screening process of existing datasets on chronic lung diseases using biological samples. The datasets were then grouped based on the V region of the 16s rRNA gene. The results of the screening process led to the selection of the lung sputum biological sample and the V4 region for further analysis. Additionally, a control dataset in healthy individuals for lung sputum samples was also selected for comparison. We selected a total of 820 samples from 366 patients. All the data used in the study was obtained from EBI databases, a reliable source of biological information. The selection of these datasets and the careful screening process were important in ensuring the validity and accuracy of the results of the study.
Data preprocessing
The process of preparing the data involved several crucial steps to ensure the accuracy and quality of the results. The first step was demultiplexing, which involved separating the different samples present in the dataset based on the single-end or paired-end sequence information. This step was performed using QIIME2 version 2020.6, a widely used software for microbial analysis [26]. After demultiplexing, the samples were denoised to remove any noise present in the data. The DADA2 technique was utilized for this step, which allowed for an evaluation of the quality of the denoised reads [27]. Finally, the filtered raw sequencing data were subjected to a thorough cleaning process to eliminate any samples with fewer than 5000 reads. This step was taken to ensure that the final results were based on high-quality data and to minimize the potential for errors. In conclusion, the data preparation process was crucial to the success of the study and involved several important steps to ensure the accuracy and reliability of the results.
Taxonomic analysis
The process of taxonomic analysis in QIIME2 version 2020.6 involves a series of crucial steps to obtain meaningful results. The first step involves the clustering of Operational Taxonomic Units (OTUs) based on their similarity, which is determined by a similarity of over 97%. This can be achieved through the use of two methods, the Denovo and closed reference clustering methods [28]. The next step involves the classification of the 16S rRNA gene sequences using a Scikit-Learn naive Bayes machine-learning classifier that is based on the GreenGenes database.
Alpha and beta diversity
The data obtained from the above steps is then evaluated using various indices, including the Shannon index, which is used to determine alpha diversity, the weighted UniFrac, which is used to evaluate beta diversity, and the primary coordinate analysis (PCoA).
The taxonomic data is analyzed at the genus level. The relative abundances of each genus in each sample are calculated for each dataset individually. This step helps to provide a comprehensive understanding of the taxonomic composition of the data, which can be useful in various applications, such as environmental monitoring, and disease diagnosis among others. The use of clustering methods, machine-learning classifiers, and various indices helps to provide a comprehensive understanding of the taxonomic composition of the data, which can be useful in various applications.
External validation data
In order to corroborate the findings from the preceding stages, we repeated the analyses detailed in the prior step using two distinct datasets: one comprising data from healthy subjects and the other containing data from patients with COPD (refer to Table 1).
Results
Data acquisition
As depicted in Table 1, the analysis of 16 s rRNA genes in lung sputum was carried out using five distinct datasets, including patients with pulmonary disease and healthy individuals. In the “Availability of data and materials” section, the link to the data obtained from the EBI database is mentioned. The filtered samples consisted of those whose sequence length was less than 5000.
Data and taxonomic analysis
Alpha-rarefaction separations that were shown in Fig. 1 are done to account for differences in sequencing depth and to ensure that rare species are not missed. Phylogenetically, the diversity of microbial communities was evaluated using four metrics: mean-nearest-taxon-distance (MNTD), nearest-taxon-index (NTI), mean phylogenetic distance (MPD), and net-relatedness index (NRI). The comparison between each sample pair was made using a distance calculation, such as Bray–Curtis or UniFrac, which produced a matrix of pairwise distances. We determined the relative abundance of bacteria at the genus level in three databases for chronic lung diseases, including bronchiectasis, COPD, AECOPD, and a healthy database. The bacteria that showed a high relative abundance in each illness are considered potential candidates. As illustrated in Fig. 2, Pseudomonas bacteria (which are highlighted in red) were detected in all patients with chronic lung diseases, whereas it was absent in healthy individuals.
Rothia was found to have a significant relative frequency in all datasets except in bronchiectasis. Actinomyces was found to have a significant relative frequency in the mentioned diseases, while its relative frequency in the healthy dataset was not significant. Prevotella, Streptococcus, Veillonella, Neisseria, and Haemophilus were found to have a significant frequency in chronic lung disease and healthy individuals and were considered as “housekeeping genes” in the lung microbiome.
The following genera of bacteria were found to have low abundance only in healthy individuals: Bacteroides, Butyrivibrio, Peptococcus, Filifactor, Peptostreptococcus, Bulleidia, Cardiobacterium, and Mycoplasma. Tannerella and Catonella were observed to have low abundance in all datasets except AECOPD. Porphyromonas was found to have low abundance in all three disease datasets but was not observed in healthy individuals. Bifidobacterium and Scardovia were only seen with low abundance in COPD and AECOPD. Leptotrichia, Ochrobactrum, and Actinobacillus were only seen with low abundance in bronchiectasis. Acinetobacter was only seen with low abundance in AECOPD and Turicibacter, Blautia, Oscillospira, Schwartzia, and Clostridium were only seen with low abundance in COPD.
Leptotrichia was found to be in significant abundance in COPD and AECOPD and had a lower abundance in the healthy and bronchiectasis datasets. Lactobacillus was significantly abundant in COPD and AECOPD but was absent in the healthy and bronchiectasis datasets. It appears that the high abundance of these two bacteria is related to COPD. Moraxella was found in COPD but was not present in other datasets. Actinobacillus was found to have the highest relative abundance in healthy individuals and low relative abundance in bronchiectasis and was not present in COPD and AECOPD. It appears that its abundance has an inverse relationship with respiratory disease.
In the examination of AECOPD, there was no substantial difference observed in the microbiome between males and females. As the metadata in other datasets lacked information regarding sex, it was impossible to determine the variations in the microbiome based on gender. Our results showed negative correlations based on their relative abundance, which were found between Pseudomonas and Prevotella, Veillonella, Streptococcus, and Capnocytophaga in bronchiectasis whereas there was not any significant correlation between Pseudomonas and other genera in chronic lung disease. These findings indicate that the relationship between Pseudomonas and other genera may differ among respiratory diseases.
External validation data
We conducted the same analyses mentioned in the previous steps on two distinct datasets concerning healthy individuals and patients with COPD (Table 1). In the dataset related to healthy individuals, Pseudomonas was not observed, while in the COPD dataset, Pseudomonas was observed with a significant frequency.
Statistical analysis
In this section, we conducted Chi-Square and Mann–Whitney statistical analyses to assess the presence and abundance of Pseudomonas bacteria in various chronic lung diseases compared to the healthy state. Based on the results obtained in Table 2, a significant difference in the abundance of this bacterium was observed between the diseased and healthy states.
Discussion
In this study, we conducted a comparison of the respiratory microbiome among individuals with chronic lung diseases, including Chronic Obstructive Pulmonary Disease (COPD), Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD), non-cystic fibrosis bronchiectasis, and healthy controls. This comparison was based on sputum samples obtained from the V4 area, and we analyzed a total of 820 samples from 366 patients. We found that Pseudomonas was present in significant frequencies across all disease datasets, while its abundance was markedly lower in the dataset of healthy individuals. Validation results using independent data have further confirmed our findings. Thus, we are investigating the impact of this pathogen on the epigenetics of chronic lung diseases.
In study by Faure et al., it has been suggested that the presence of Pseudomonas is harmless in healthy people [29]. However, our study has explored this issue and found a substantial and distinct difference between healthy individuals and those with COPD, bronchiectasis, and ACOPD. This difference is quite pronounced.
The observed negative correlation between Pseudomonas and Bacteroidetes/Firmicutes in bronchiectasis (Fig. 3) is likely due to their competition for shared resources and the production of antimicrobial compounds that hinder the growth of competing bacterial groups [30].
Correlation between Pseudomonas and other genera in bronchiectasis based on their relative abundance. The colors of nodes represent bacteria at the phylum level. Blue represents Firmicutes, gray represents Bacteroidetes, and orange represents Proteobacteria. Edges show a negative correlation above 0.4 in bacteria abundance. The thickness of the edges in the network represents the strength of the connections between bacteria
Pseudomonas. aeruginosa, a gram-negative bacterium, which is commonly found in the respiratory tract, can modulate epigenetic mechanisms in host cells to promote its own survival and colonization [31]. Overall, research suggests that Pseudomonas may play an important role in shaping the epigenetic landscape of the respiratory microbiome, which can have implications for respiratory health and disease.
DNA methylation is a process by which methyl groups are added to the DNA molecule. This can lead to changes in gene expression by blocking the access of the transcription machinery to the DNA. Pseudomonas can modulate host gene expression by changing host ncRNA expression or host DNA methylation pattern in a way that benefits the bacteria [25, 32, 33].
Pseudomonas is known to modulate the expression of a wide range of host genes to establish and maintain chronic infections [33]. Some examples of host genes that are affected by Pseudomonas include:
-
Genes involved in inflammation: Pseudomonas’ ability to upregulate pro-inflammatory genes, like TNF-alpha and IL-8, fosters a pro-inflammatory environment conducive to bacterial growth. Furthermore, TNF-alpha and IL-8, known for their roles in infection-related immune responses and their implication in chronic lung diseases such as COPD and bronchiectasis, are suggested to be influenced by the presence of Pseudomonas in the respiratory microbiome, potentially affecting the development and progression of chronic lung diseases [34].
-
Genes involved in host defense: Pseudomonas can downregulate the expression of host defense genes, such as those encoding antimicrobial peptides, to evade the host’s defenses. The downregulation of these genes may result in a weakened immune response and increased susceptibility to infections and inflammation [35]. This can contribute to the progression of the disease and make it more difficult to treat. Genes involved in the innate immune response, such as toll-like receptors (TLRs) and nucleotide-binding oligomerization domain-like receptors (NLRs), have been implicated in the pathogenesis of chronic obstructive pulmonary disease (COPD) and other respiratory disorders [36]. Similarly, changes in the expression of genes involved in adaptive immune responses, such as T-cell receptors and immunoglobulin genes, have been observed in individuals with these conditions [37]. Alterations in host defense genes can result in a weakened immune response, leading to increased susceptibility to infections and inflammation. In other cases, changes in these genes may result in an overactive immune response, leading to tissue damage.
-
Genes involved in cell signaling: Pseudomonas can modulate the expression of host genes involved in cell signaling pathways, such as those encoding receptor tyrosine kinases, to alter host cell behavior in a manner that favors their survival, enabling them to evade the host’s immune defenses [31,32,33]. In the context of respiratory diseases, the expression and activation of RTKs may play a crucial role in the development and progression of the disease [38]. Dysregulation of RTK signaling has been implicated in several respiratory diseases, including IPF, Asthma, chronic obstructive pulmonary disease (COPD), and lung cancer.
-
Genes involved in apoptosis: Pseudomonas can modulate the expression of host genes involved in programmed cell death (apoptosis), to prevent host cells from dying and releasing antimicrobial molecules [39]. Alterations in the expression or activity of genes involved in the apoptosis pathway, such as Bcl-2, caspases, and P53, have been observed in individuals with chronic obstructive pulmonary disease (COPD), lung cancer, and other respiratory disorders [40]. In some cases, changes in these genes may lead to an impaired ability of the cells in the respiratory system to undergo apoptosis, resulting in increased cell survival and contributing to the development of disease [41]. In other cases, alterations in the apoptosis pathway may result in increased cell death, leading to inflammation and scarring.
-
MicroRNA: Research indicates a bidirectional relationship between microbiome composition and host miRNA expression, with potential implications for chronic lung diseases. In COPD, for example, changes in the lung microbiome have been linked to alterations in miRNA expression, which can lead to inflammation and exacerbation of the disease [42]. Additionally, some miRNAs have been shown to directly target bacterial genes, suggesting a direct link between host miRNA expression and microbiome [43]. This highlights the importance of understanding the interplay between the host miRNA expression and the lung microbiome in the development and progression of chronic lung diseases.
The above are examples of host genes affected by Pseudomonas, but this bacterium can modulate many other genes depending on the context of infection. Understanding the specific genes and pathways affected by Pseudomonas in different types of infections may help to develop new treatments for these infections.
Conclusion
In this study, we analyzed multiple datasets from individuals with chronic lung diseases and a healthy control group to compare the respiratory microbiome between the two. The results revealed that the genus Pseudomonas is abundant and significant in the respiratory microbiome of individuals with chronic lung diseases. Our study also demonstrated that the pathogen Pseudomonas can cause epigenetic changes that perpetuate airway inflammation and worsen lung damage. Further investigation is required to fully comprehend the specific mechanisms through which Pseudomonas induces these changes and to determine if targeting these changes may offer a promising therapeutic approach for individuals with chronic lung diseases.
Availability of data and materials
The public datasets analyzed during the current study are available in
https://www.ebi.ac.uk/ena/browser/view/PRJNA491749?show=reads
https://www.ebi.ac.uk/ena/browser/view/PRJEB14304?show=reads
https://www.ebi.ac.uk/ena/browser/view/PRJNA377739?show=reads
https://www.ebi.ac.uk/ena/browser/view/PRJEB9607?show=reads
https://www.ebi.ac.uk/ena/browser/view/PRJNA491861?show=reads
https://www.ebi.ac.uk/ena/browser/view/PRJNA299077?show=reads
Abbreviations
- COPD:
-
Chronic Obstructive Pulmonary Disease
- AECOPD:
-
Acute Exacerbation Chronic Obstructive Pulmonary Disease
- OTU:
-
Operational Taxonomic Unit
- PCoA:
-
Principal Coordinate Analysis
- IPF:
-
Idiopathic Pulmonary Fibrosis
- CF:
-
Cystic Fibrosis
- MNTD:
-
Mean-Nearest-Taxon-Distance
- NTI:
-
Nearest-Taxon-Index
- MPD:
-
Mean Phylogenetic Distance
- NRI:
-
Net-Relatedness Index
- P. aeruginosa :
-
Pseudomonas aeruginosa
- FMT:
-
Fecal microbiota transplantation
- ncRNA:
-
Non-coding RNA
References
Hou K, Wu Z-X, Chen X-Y, Wang J-Q, Zhang D, Xiao C, et al. Microbiota in health and diseases. Signal Transduct Target Ther. 2022;7:135.
Natalini JG, Singh S, Segal LN. The dynamic lung microbiome in health and disease. Nat Rev Microbiol. 2023;21:222–35.
Chen J, Li T, Ye C, Zhong J, Huang J-D, Ke Y, et al. The lung microbiome: a new frontier for lung and brain disease. Int J Mol Sci. 2023;24:2170.
Zheng D, Liwinski T, Elinav E. Interaction between microbiota and immunity in health and disease. Cell Res. 2020;30:492–506.
Kavianfar A, Taherkhani H, Salimi M. Impact of perioperative management on ocular microbiota composition and diversity: a study of intravitreal injection patients with 16S rRNA sequencing. J Ophthalmic Optom Sci. 2021;5(4):14–29.
Batoni G, Kaya E, Catelli E, Quinti S, Botti M, De Carli A, et al. Lactobacillus probiotic strains differ in their ability to adhere to human lung epithelial cells and to prevent adhesion of clinical isolates of Pseudomonas aeruginosa from cystic fibrosis lung. Microorganisms. 2023;11:1707.
Carvalho JL, Miranda M, Fialho AK, Castro-Faria-Neto H, Anatriello E, Keller AC, et al. Oral feeding with probiotic Lactobacillus rhamnosus attenuates cigarette smoke-induced COPD in C57Bl/6 mice: relevance to inflammatory markers in human bronchial epithelial cells. PLoS One. 2020;15:e0225560.
Mortaz E, Adcock IM, Folkerts G, Barnes PJ, Paul Vos A, Garssen J. Probiotics in the management of lung diseases. Mediators Inflamm. 2013;2013:751068.
Huang L, Guo J, Li W, Jiang M, Wang F, Kang J, et al. Probiotics, prebiotics, and synbiotics for the treatment of asthma: protocol for a systematic review. Medicine (Baltimore). 2019;98:e17840.
Jang YO, Lee SH, Choi JJ, Kim D-H, Choi J-M, Kang M-J, et al. Fecal microbial transplantation and a high fiber diet attenuates emphysema development by suppressing inflammation and apoptosis. Exp Mol Med. 2020;52:1128–39.
O’Shaughnessy M, Sheils O, Baird A-M. The lung microbiome in COPD and lung cancer: exploring the potential of metal-based drugs. Int J Mol Sci. 2023;24:12296.
Wen L, Shi L, Kong X-L, Li K-Y, Li H, Jiang D-X, et al. Gut microbiota protected against Pseudomonas aeruginosa pneumonia via restoring Treg/Th17 balance and metabolism. Front Cell Infect Microbiol. 2022;12:856633.
Khan FH, Bhat BA, Sheikh BA, Tariq L, Padmanabhan R, Verma JP, et al. Microbiome dysbiosis and epigenetic modulations in lung cancer: From pathogenesis to therapy. Semin Cancer Biol. 2022;86:732–42.
McCauley KE, Flynn K, Calatroni A, DiMassa V, LaMere B, Fadrosh DW, et al. Seasonal airway microbiome and transcriptome interactions promote childhood asthma exacerbations. J Allergy Clin Immunol. 2022;150:204–13.
Woo V, Alenghat T. Epigenetic regulation by gut microbiota. Gut Microbes. 2022;14:2022407.
Gallardo VJ, Vila-Pueyo M, Pozo-Rosich P. The impact of epigenetic mechanisms in migraine: current knowledge and future directions. Cephalalgia. 2023;43:03331024221145916.
Ebrahimi V, Soleimanian A, Ebrahimi T, Azargun R, Yazdani P, Eyvazi S, et al. Epigenetic modifications in gastric cancer: focus on DNA methylation. Gene. 2020;742:144577.
Bradic M, Taleb S, Thomas B, Chidiac O, Robay A, Hassan N, et al. DNA methylation predicts the outcome of COVID-19 patients with acute respiratory distress syndrome. J Transl Med. 2022;20:526.
Wang H, Hu J, Wu J, Ji P, Shang A, Li D. The function and molecular mechanism of commensal microbiome in promoting malignant progression of lung cancer. Cancers. 2022;14:5394.
Izzo LT, Affronti HC, Wellen KE. The bidirectional relationship between cancer epigenetics and metabolism. Annu Rev Cancer Biol. 2021;5:235–57.
Haque S, Raina R, Afroze N, Hussain A, Alsulimani A, Singh V, et al. Microbial dysbiosis and epigenetics modulation in cancer development – a chemopreventive approach. Semin Cancer Biol. 2022;86:666–81.
Stölting H, Lloyd CM. Pseudomonas aeruginosa: a pathogen making itself at home. Trends Immunol. 2022;43:497–9.
Greenwald MA, Wolfgang MC. The changing landscape of the cystic fibrosis lung environment: from the perspective of Pseudomonas aeruginosa. Curr Opin Pharmacol. 2022;65:102262.
Bernardy EE, Raghuram V, Goldberg JB. Staphylococcus aureus and Pseudomonas aeruginosa isolates from the same cystic fibrosis respiratory sample coexist in coculture. Microbiol Spectr. 2022;10:e0097622.
Kyung Lee M, Armstrong DA, Hazlett HF, Dessaint JA, Mellinger DL, Aridgides DS, et al. Exposure to extracellular vesicles from Pseudomonas aeruginosa result in loss of DNA methylation at enhancer and DNase hypersensitive site regions in lung macrophages. Epigenetics. 2021;16:1187–200.
Bolyen E, Rideout JR, Dillon MR, Bokulich NA, Abnet CC, Al-Ghalith GA, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol. 2019;37:852–7.
Callahan BJ, Mcmurdie PJ, Rosen MJ, Han AW, Johnson AJA, Holmes SP. DADA2: High-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13:581–3.
Westcott SL, Schloss PD. De novo clustering methods outperform reference-based methods for assigning 16S rRNA gene sequences to operational taxonomic units. PeerJ. 2015;3:e1487.
Faure E, Kwong K, Nguyen D. Pseudomonas aeruginosa in chronic lung infections: how to adapt within the host? Front Immunol. 2018;9:2416.
Wang W-W, Mao B, Liu Y, Gu S-Y, Lu H-W, Bai J-W, et al. Altered fecal microbiome and metabolome in adult patients with non-cystic fibrosis bronchiectasis. Respir Res. 2022;23:317.
Qin S, Xiao W, Zhou C, Pu Q, Deng X, Lan L, et al. Pseudomonas aeruginosa: pathogenesis, virulence factors, antibiotic resistance, interaction with host, technology advances and emerging therapeutics. Signal Transduct Target Ther. 2022;7:199.
Lin J, Cheng J, Wang Y, Shen X. The Pseudomonas Quinolone Signal (PQS): not just for quorum sensing anymore. Front Cell Infect Microbiol. 2018;8:230.
Duan K, Dammel C, Stein J, Rabin H, Surette MG. Modulation of Pseudomonas aeruginosa gene expression by host microflora through interspecies communication. Mol Microbiol. 2003;50:1477–91.
Kany S, Vollrath JT, Relja B. Cytokines in inflammatory disease. Int J Mol Sci. 2019;20:6008.
Apidianakis Y, Mindrinos MN, Xiao W, Lau GW, Baldini RL, Davis RW, et al. Profiling early infection responses: Pseudomonas aeruginosa eludes host defenses by suppressing antimicrobial peptide gene expression. Proc Natl Acad Sci U S A. 2005;102:2573–8.
Chaput C, Sander LE, Suttorp N, Opitz B. NOD-like receptors in lung diseases. Front Immunol. 2013;4:393.
Kałużna A, Olczyk P, Komosińska-Vassev K. The Role of innate and adaptive immune cells in the pathogenesis and development of the inflammatory response in ulcerative colitis. J Clin Med. 2022;11:400.
Grimminger F, Günther A, Vancheri C. The role of tyrosine kinases in the pathogenesis of idiopathic pulmonary fibrosis. Eur Respir J. 2015;45:1426–33.
Wood SJ, Goldufsky JW, Seu MY, Dorafshar AH, Shafikhani SH. Pseudomonas aeruginosa cytotoxins: mechanisms of cytotoxicity and impact on inflammatory responses. Cells. 2023;12:195.
Zeng H, Kong X, Peng H, Chen Y, Cai S, Luo H, et al. Apoptosis and Bcl-2 family proteins, taken to chronic obstructive pulmonary disease. Eur Rev Med Pharmacol Sci. 2012;16:711–27.
Uddin MA, Barabutis N. P53 in the impaired lungs. DNA Repair (Amst). 2020;95:102952.
Casciaro M, Di Salvo E, Pioggia G, Gangemi S. Microbiota and microRNAs in lung diseases: mutual influence and role insights. Eur Rev Med Pharmacol Sci. 2020;24:13000–8.
Riahi Rad Z, Riahi Rad Z, Goudarzi H, Goudarzi M, Mahmoudi M, Yasbolaghi Sharahi J, et al. MicroRNAs in the interaction between host-bacterial pathogens: a new perspective. J Cell Physiol. 2021;236:6249–70.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
A.MN and AA proposed the idea. AK and HT performed the data analysis and wrote the first draft of the manuscript. A.MN, MS and AA conceived and supervised and edited the final draft of the work. MS and HL helped with the biological discussion. HL participated in writing and edited the final version. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
KavianFar, A., Taherkhani, H., Ahmadi, A. et al. Restoring the epigenetic landscape of lung microbiome: potential therapeutic approach for chronic respiratory diseases. BMC Pulm Med 24, 2 (2024). https://doi.org/10.1186/s12890-023-02789-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02789-7