Abstract
Background
The diagnostic criteria for asthma-chronic obstructive pulmonary disease overlap have not been unified. Different studies have used different criteria, and this has led to diagnostic inconsistencies.
Methods
We collected data of patients who were older than 40 years and hospitalised because of chronic bronchial diseases. One hundred and seventy-one patients were included in this study. We compared seven different diagnostic criteria, examined their consistency, and analysed differences among groups classified with each set.
Results
The prevalence of ACO ranged between 7.02 and 27.49% depending on the criteria applied. The patients who met the Soler-Cataluna et al. criteria also met the GesEPOC criteria. Rhee has proposed the strictest diagnostic criteria; hence, the number of patients who met these criteria was the smallest, and those patients also met the diagnostic criteria proposed by the other studies. We found that applying the different sets of criteria did not lead to the selection of the same population, while there were no statistical differences in age, disease duration, allergens, and inflammatory markers.
Conclusions
The diagnostic criteria of ACO have not been unified, which hinders the design and progress of clinical studies that would investigate the ACO phenotypes and underlying mechanisms.
Similar content being viewed by others
Background
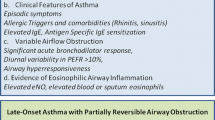
Chronic obstructive pulmonary disease (COPD) is preventable, common, and treatable and is characterised by persistent respiratory symptoms and airflow limitation [1]. Asthma is a common, chronic respiratory disease, characterised by variable symptoms of wheezing, shortness of breath, chest tightness and/or cough, and by variable expiratory airflow limitation [2]. In some patients, chronic asthma cannot be clearly distinguished from COPD using currently available tests and techniques, and in those patients, it is assumed that asthma and COPD coexist. Asthma-COPD overlap syndrome [3] has been coined to acknowledge that this represents an overlap of common disorders causing chronic airflow limitation rather than being a distinct syndrome [4]. To avoid the impression that this is a single disease, the term ACOS is no longer advised; the descriptive term asthma-COPD overlap (ACO) may be more appropriate [2]. The prevalence rates of ACO range from 15 to 55%, with variation depending on sex and age [5,6,7]. The wide range may be due to the different criteria used by different investigators. The prognosis of ACO is often worse than that of asthma or COPD alone [8], but the evidence for ACO treatment is very limited as few pharmacotherapy studies have examined this population. The different diagnostic criteria used in various regions and by different investigators might also limit the progress of ACO clinical studies. The diagnostic criteria of ACO have not been unified. Previous studies have used their own respective standards, so there was a lack of evaluation among the ACO patients screened by each standard. Our study compared the consistency among seven different sets of ACO diagnostic criteria proposed by previous studies to examine the clinical characteristics of patients screened by different standards, aiming to provide more clinical evidence for ACO diagnosis.
Materials and methods
Subjects
We collected data of patients who were older than 40 years and hospitalised because of chronic bronchial diseases (asthma or COPD) in Xinhua Hospital, from January 2017 to April 2018. The inclusion and exclusion criteria are shown in Table 1. One hundred and seventy-one patients were included in this study. The study was approved by the ethics committee of Xinhua Hospital, and informed consent was secured from the participating patients.
Data collection
Clinical data included general information (name, sex, age, age at onset, family history, smoking history), laboratory tests (routine blood test, eosinophilia in sputum, immunoglobulin E, arterial blood gas, allergen detection, and inflammatory factors), pulmonary function tests, disease condition in the past year, and medication use.High IgE meaned IgE > 100 IU/ml, high FeNO meaned FeNO > 25 ppb, elevated sputum eosinophil meaned eosinophil > 1.01% [9]. In order not to omit COPD patients, we equated exposures of noxious particles or gases over 10 years, such as tobacco smoke, air pollution, and occupational exposures to smoking history.
Diagnostic criteria
Our study compared the consistency among seven different sets of ACO diagnostic criteria proposed by previous studies, including the GOLD in 2016 [10], Spanish COPD Guidelines (GesEPOC) [11], Soler-Cataluna et al. [12], Marsh et al. [6], Kauppi et al. [5], Louie et al. [13], and Rhee [14] (Table 2) .
Statistical analysis
SPSS was used for statistical analysis. To compare differences among groups, analysis of variance, chi-square tests, and the Kruskal-Wallis test were used for parametric continuous, categorical, and nonparametric continuous variables, respectively. P < 0.05 was considered statistically significant. Diagnostic consistency was calculated by kappa testing, and kappa coefficients were assessed as follows: 0.01–0.40: slight agreement; 0.41–0.70: moderate agreement; 0.71–0.99: high agreement.
Results
The data of 171 participants were analysed. The sample was 68.4% male and had a mean age of 67.5 years. In total, 115 cases (67.3%) had a history of smoking. Full details are shown in Table 3.
Seven sets of ACO diagnostic criteria
The prevalence of ACO in chronic airway diseases ranged from 7.02 to 27.49% (Table 4). The patients who met the Soler-Cataluna et al. criteria also met the GesEPOC criteria. Rhee has proposed the strictest diagnostic criteria; hence, the number of patients who met these criteria was the smallest, and those patients also met the diagnostic criteria proposed by the other studies (Fig. 1).
Consistency comparison among the seven sets of ACO diagnostic criteria
The GesEPOC diagnostic criteria were most consistent with those proposed by Soler-Cataluna et al. (Kappa = 0.84, P < 0.0001). The Marsh et al. criteria were moderately consistent with the other sets of diagnostic criteria, while the criteria proposed by Rhee were poorly consistent with those proposed by the other studies (Kappa < 0.4 in all but one case) (Table 5).
Clinical characteristics of the patients with ACO based on the seven sets of diagnostic criteria
There were significant differences in sex, smoking history, and lung function (increase in forced expiratory volume in one second (FEV1) and FEV1% after bronchodilation) among the diagnostic criteria. However, we found no statistical differences in age, disease duration, positive results of allergens, and inflammatory markers (such as interleukin (IL)-2, IL-6, IL-8, tumour necrosis factor, and fractional exhaled nitric oxide) (Table 6).
Discussion
Most previous studies of airways diseases have excluded patients with ACO [15, 16]. We collected data of 171 patients who were older than 40 years and had chronic bronchial diseases. After comparing seven sets of diagnostic criteria, examining their consistency, and analysing differences among groups, we found that the different sets did not lead to the selection of the same population.
Based on the lung function test definition of ACO alone, many patients with asthma or COPD could be considered to have ACO. Thus, a narrower and more accurate definition of ACO is needed in clinical practice. Some experts have suggested a definition of ACO based on both lung function and on clinical features [12]. However, a specific definition for ACO cannot be confirmed until more evidence becomes available regarding its clinical phenotypes and underlying mechanisms.
According to GOLD [10], clinicians should diagnose chronic airways disease first, estimate the syndromic diagnosis of asthma, COPD, and ACO; perform spirometry testing, and then commence therapy to estimate the therapeutic effect and confirm the diagnosis; additional specialised investigations should be performed if necessary. There is no specific numerical standard in GOLD, and it relies more on clinical symptoms and clinical judgment. Therefore, the GOLD are more descriptive of ACO. GOLD highlights the significance that the therapeutic effect has for diagnosis and does not rely on a single medical record, while the therapeutic effect was rarely mentioned in the other studies [5, 6, 11,12,13,14]. This renders this method more comprehensive, but it may also require a greater degree of subjective clinician input, leading to diagnostic inconsistencies and hence, it cannot be readily established as a standard.
The GesEPOC [11] and Soler-Cataluna et al. [12] criteria shared the most similarities. The GesEPOC criteria are relatively broad, and thus the patients who met the Soler-Cataluna et al. criteria also met the GesEPOC criteria. The common feature of these two sets of criteria are the high requirements regarding the bronchodilator test. Both sets of criteria require a very positive bronchodilator test (major criterion; increase in FEV1 ≥ 15% and ≥ 400 ml) and positive bronchodilator tests on two or more occasions (minor criterion; increase in FEV1 ≥ 12% and ≥ 200 ml). While the criteria proposed by the other studies mostly require one positive bronchodilator test. This might be the reason why these two sets had poor consistency with the criteria proposed by the other studies.
The Marsh et al. [6] and Kauppi et al. [5] diagnostic criteria are both based on a definitive diagnosis of COPD first, and then, to be diagnosed with ACO, the patients should have certain asthma characteristics. The asthma characteristics included in the Kauppi et al. study were only focused on lung function, while Marsh et al. also included physician diagnosis of asthma and inhaler use. Therefore, the Marsh et al. assessment is more comprehensive, and this might explain why the Marsh et al. diagnostic criteria, compared to the Kauppi et al. criteria, were generally more consistent with those proposed by the other studies.
The Rhee diagnostic criteria are the most stringent, stating that the patients should meet the spirometric and clinical criteria for asthma and the spirometric and clinical criteria for COPD [14]; the criteria proposed by the other studies only required patients to meet some of these to receive an ACO diagnosis. Consequently, the fewest patients were diagnosed with ACO based on the Rhee criteria, which led to the worst consistency between this set and the other sets of criteria. However, the patients who meet the Rhee criteria might be considered to have true ACO. Without a firm definition of ACO, it is not possible to perform high-quality clinical trials. Thus, Rhee contested that a narrow definition of ACO, which includes both asthma and COPD diagnoses, was needed.
In order to delineate the clinical characteristics of the patients selected by each diagnostic method, we statistically compared the groups. It was found that there was a significant difference in lung function, especially in increase in FEV1% and in FEV1. This might be in line with the GesEPOC [11] and Soler-Cataluna et al. [12] criteria, which require a very positive bronchodilator test. In addition, sex and smoking history were also statistically different among the groups. Some diagnostic criteria used smoking history as a major criterion while others as a minor criterion, and most of the smokers in the sample were male, which may have led to the significant differences. No differences were found in inflammatory factors and other biomarkers. Differences in biomarkers may be related to underlying mechanisms and phenotypes [17,18,19]. The diagnostic criteria examined here can only be used to diagnose ACO, and at present, there are no methods to diagnose the ACO phenotypes; further research is needed to this end [2].
The small sample and our single-center design limited the results of our study. We enrolled only patients with hospitalization. Many stable chronic airway disease patients without history of hospitalization were not included. This is indeed one of the shortcomings of our research. At the beginning of the study design, we also considered to include stable chronic airway disease patients of outpatient department into our study. However, most of those patients have incomplete examination data, and it is difficult to be included in the statistics. So finally we decided to enroll only patients with hospitalization. Additionally, our study was cross sectional and it did not involve follow-up observation of the clinical characteristics and treatment effects in our patients. Our team plans to follow up the patients in a prospective study, aiming to advance the search for the most appropriate diagnostic criteria for ACO and its phenotypes.
Conclusions
The diagnostic criteria of ACO have not been unified, and the diagnostic methods used in different studies lead to diagnostic inconsistencies. Furthermore, these methods cannot be used to diagnose the ACO phenotypes and to study the underlying mechanisms. As a future research direction, our team plans to follow up on the clinical characteristics and treatment effects in these patients in a prospective study to propose some potential solutions.
Availability of data and materials
Please contact Wenjing Ye.
Abbreviations
- ACOS:
-
Asthma-COPD overlap syndrome
- COPD:
-
Chronic obstructive pulmonary disease
- FEV1:
-
Forced expiratory volume in one second
- IL:
-
Interleukin
References
Muneswarao J, Verma AK, Hassali MAA. Global initiative for chronic obstructive lung disease (GOLD) 2018 report: highlighting an incorrect information. Pulm Pharmacol Ther. 2018;49:10.
Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, JM FG, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31:143–78.
Cosio BG, pérez de llano l, lopez viña a, Torrego a, Lopez-Campos JL, Soriano JB, et al. Th-2 signature in chronic airway diseases: towards the extinction of asthma-COPD overlap syndrome? Eur Respir J. 2017;49:1602397.
Vogelmeier CF, Criner GJ, Martínez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J. 2017;49:1750214.
Kauppi P, Kupiainen H, Lindqvist A, Tammilehto L, Kilpeläinen M, Kinnula VL, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011;48:279–85.
Marsh SE, Travers J, Weatherall M, Williams MV, Aldington S, Shirtcliffe PM, et al. Proportional classifications of COPD phenotypes. Thorax. 2008;63:761–7.
Weatherall M, Travers J, Shirtcliffe PM, Marsh SE, Williams MV, Nowitz MR, et al. Distinct clinical phenotypes of airways disease defined by cluster analysis. Eur Respir J. 2009;34:812–8.
Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009;64:728–35.
Simpson JL, Scott R, Boyle MJ, Gibson PG. Inflammatory subtypes in asthma: assessment and identification using induced sputum. Respirology. 2006;11:54–61.
Lu M, Yao WZ. Interpretation of global strategy for the diagnosis, management and prevention of chronic obstructive lung disease (GOLD) 2016. Zhonghua Yi Xue Za Zhi. 2016;96:2689–91.
Miravitlles M, Soler-Cataluña JJ, Calle M, Molina J, Almagro P, Quintano JA, et al. Spanish COPD guidelines (GesEPOC)66: pharmacological treatment of stable COPD. Spanish society of pulmonology and thoracic surgery. Arch Bronconeumol. 2012;48:247–57.
Soler-Cataluna JJ, Cosío B, Izquierdo JL, López-Campos JL, Marín JM, Agüero R, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol. 2012;48:331–7.
Louie S, Zeki AA, Schivo M, Chan AL, Yoneda KY, Avdalovic M, et al. The asthma-chronic obstructive pulmonary disease overlap syndrome: pharmacotherapeutic considerations. Expert Rev Clin Pharmacol. 2013;6:197–219.
Rhee CK. Phenotype of asthma-chronic obstructive pulmonary disease overlap syndrome. Korean J Intern Med. 2015;30:443–9.
Petersen MK, Andersen KV, Andersen NT, Søballe K. "to whom do the results of this trial apply?" external validity of a randomized controlled trial involving 130 patients scheduled for primary total hip replacement. Acta Orthop. 2007;78:12–8.
Travers J, Marsh S, Caldwell B, Williams M, Aldington S, Weatherall M, et al. External validity of randomized controlled trials in COPD. Respir Med. 2007;101:1313–20.
Hardin M, Cho M, McDonald ML, Beaty T, Ramsdell J, Bhatt S, et al. The clinical and genetic features of COPD-asthma overlap syndrome. Eur Respir J. 2014;44:341–50.
Wardlaw AJ, Silverman M, Siva R, Pavord ID, Green R. Multi-dimensional phenotyping: towards a new taxonomy for airway disease. Clin Exp Allergy. 2005;35:1254–62.
Carolan BJ, Sutherland ER. Clinical phenotypes of chronic obstructive pulmonary disease and asthma: recent advances. J Allergy Clin Immunol. 2013;131:627–34 quiz 635.
Acknowledgements
N/A
Funding
No funding.
Author information
Authors and Affiliations
Contributions
WJY conceived the study and participated in its design and performance, the statistical analysis, and in drafting and revising the manuscript. XML participated in the study design and performance, statistical analysis, and in drafting and revising the manuscript. WG conceived the study and participated in its design and coordination and in revising the manuscript. XJG conceived the study and participated in its design and coordination and in revising the manuscript. FFH conceived the study and participated in its design and performance. LS participated in the study design and performance, statistical analysis. All authors have read and approved the manuscript, and ensured that this is the case.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of Xinhua Hospital. It was a retrospective study, and verbal informed consent was obtained from all of the participants, the method of which was approved by the ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declared no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ye, W., Li, X., Gu, W. et al. A comparison of diagnostic consistency for asthma-chronic obstructive pulmonary disease overlap and clinical characteristics study. BMC Pulm Med 19, 249 (2019). https://doi.org/10.1186/s12890-019-1024-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-019-1024-2