Abstract
Chronic obstructive pulmonary disease and asthma are the most frequent chronic respiratory diseases that affect the general population. For a long period of time these two conditions were considered to be separate diseases. However, it became evident that some patients share symptoms and clinical findings from both diseases. These patients are considered to represent a distinct phenotype, called asthma-COPD overlap syndrome (ACOS). However, since approximately the one third of the asthmatics smoke the ACOS may primarily define those patients. This is a relatively newly defined clinical syndrome whose underlying mechanisms and most appropriate management remain to be confirmed. In this review, we summarize current knowledge on this syndrome, aiming to update clinicians and help their daily practice.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) and asthma are frequent chronic diseases, which pose a significant burden to health status, quality of life and –in the case of COPD- survival of the patients [1]. The reported prevalence of COPD ranged from 0.2% in Japan to 37% in the USA, but this varied widely across countries and populations, by diagnostic criteria, and by age group analyzed [2]. COPD is one of the leading causes of death [3]; it is estimated that in 2020 it will be the third leading cause of death worldwide and fifth leading cause of years lost through early mortality or handicap (disability-adjusted life years). COPD a disease of the elderly is usually associated with a number of significant comorbidities [4].
Asthma also is a serious global health problem affecting all age groups, with global prevalence ranging from 1 to 21% in adults [5]. Thus, asthma is also a common condition, responsible for considerable morbidity, healthcare utilization and costs, which include those costs caused by the days off work and decrease productivity of patients with uncontrolled asthma [6, 7]. Asthma is also characterized by the presence of comorbidities which substantially affect the quality of life and the number of exacerbations [8].
Review
In 1961, during the first Bronchitis Symposium held in Groningen, the Netherlands, Orie and colleagues hypothesized that the various forms of airway obstruction, such as asthma, chronic bronchitis, and emphysema, should be considered not as separate diseases but as different expressions of one disease entity, which they named chronic nonspecific lung disease [9]. Later on in 1969 this hypothesis was termed the Dutch hypothesis [10]. The Dutch hypothesis is in contrast to the “British hypothesis”, where asthma and chronic obstructive pulmonary disease (COPD) are seen as distinct entities generated by different mechanisms [11].
In recent years, it became clear that some patients share clinical characteristics of both asthma and COPD. This presentation could be another phenotype of airway disease called asthma-COPD overlap syndrome (ACOS). The frequency of emergency room visits and intensive care unit admissions are higher among those patients with overlap syndrome compared to those with COPD but not asthma [12]. In addition, overall healthcare expenditure for patients with co-existent asthma and COPD is almost twice the expenditure for patients with asthma but not COPD [13].
Unfortunately, distinguishing asthma from COPD is challenging, especially in elderly patients [14, 15]. Quite often the diagnosis can change during life and more authors report about cases of unclassified airflow limitation [16]. Moreover, it has been suggested that ACOS may include not one but several heterogeneous phenotypes with different underlying mechanisms and since these patients were previously excluded from clinical trials we have limited data of this condition [17, 18]. Thus, a significant phenotype of COPD could be the smoking Asthmatic [19].
Definitions
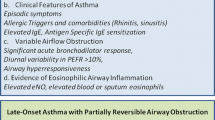
Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness and cough that vary over time and in intensity, together with variable expiratory airflow limitation according to the 2016 Global Initiative for Asthma (GINA) guidelines [20].
In the 2017 Global Strategy for Diagnosis, Management, and Prevention of COPD (GOLD) guidelines, defined COPD as a common, preventable and treatable disease, that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases [21].
ACOS is characterized by persistent airflow limitation with several features usually associated with asthma and several features usually associated with COPD. ACOS is therefore identified by the features that it shares with both asthma and COPD [22]. The prevalence of this syndrome among patients with obstructive pulmonary disease varies depending on the diagnostic criteria and country from 2.1 to 55% [22,23,24]. Several specialists in obstructive lung disease state that since there is limited data to this subject a more specific definition of ACOS till now cannot be developed and others challenge its existence. Therefore ACOS is a new clinical syndrome that recently appeared in respiratory medicine and till now is poorly defined and poorly understood.
Another theory is that asthma, COPD, and ACOS do not represent separate diseases but a continuum, consisting of several endotypes and phenotypes. ACOS allows a more simple approach to therapy which on the other hand hinders progression towards the concept of personalized medicine [25, 26]. It is also accurately stated that ACOS term may lead to clinical confusion and potential inappropriate use of resources [27].
The terms asthma and COPD are based on “Oslerian paradigm” which was introduced by Sir William Osler more than 100 years ago on the basis of the principal organ system in which symptoms and signs are attributed [28]. However, classical Oslerian approach is not taking in consideration new genetic, molecular and imagistic data, it can be sometimes efficient in “stereotypical” cases and not so good in patients with combination of asthma and COPD [26]. In the post-genomic era it has been recognized that both terms represent “umbrella” terms that include distinct groups of patients. In recent years, we have identified several phenotypes, which are subgroups of patients defined by different clinical characteristics, which have different prognosis or respond differently to treatments. More importantly, we have managed to divide some of these phenotypes to endotypes by identifying the underlying molecular pathways (typical example – a1 antitrypsin deficiency) [29, 30]. Recently Agusti et al. proposed a new holistic approach to the assessment and management of chronic airway disease, which is based exclusively on treatable traits in each patient [26]. Treatable traits are classified in multiple domains, which can coexist: airflow limitation, eosinophilic airway inflammation, chronic bronchitis, airway bacterial colonisation, bronchiectasis, cough reflex hypersensitivity, pre-capillary pulmonary hypertension, chronic respiratory failure, deconditioning, etc. Patients with airway disease could present with any combination of the above mentioned traits and their management should be guided accordingly.
All in all, there is still significant ongoing disagreement on the use of the term ACOS and characterization of these patients with intermediate clinical characteristics. While treatable traits and personalized medicine lead to a more overall management of all patients with chronic airway disease, the concept of ACOS also serve in the understanding of the underlying mechanisms and simplification of the management of these patients by non-specialists [31].
Pathogenesis and pathophysiology
Pathophysiology and underlying immunological pathways of asthma and COPD differ significantly. Similarly the clinical presentation, pathophysiology of ACOS receives several characteristics from both asthma and COPD.
The inflammation in asthma patients is usually caused by eosinophils which release pro-inflammatory mediators and basic proteins that may damage epithelial cells and cause airway remodeling [32]. Mast cells are also considered to play an important role in asthma and contribute to inflammation with bronchoconstriction mediators [33, 34]. Furthermore, other cells such as lymphocytes, dendritic cells, macrophages are abundantly present and contribute to inflammation [35]. On the other hand, in non-eosinophilic asthma, neutrophils appear to be the predominant inflammatory cells [36, 37]. Neutrophilic inflammation can be present in severe or late-onset asthma, chronic infections or in smokers [38]. Particularly bronchial infiltrate of CD8(+) T cells and CD68(+) macrophages, and epithelial remodeling resembling COPD-like features can be present in smokers with asthma [39].
COPD is characterized by a specific pattern of inflammation involving increased numbers of CD8+ (cytotoxic) Tc1 lymphocytes present only in smokers that develop the disease [40]. The inflamed airways of COPD patients contain also macrophages, T lymphocytes, and dendritic cells [41]. Still there are reports of eosinophilic airway inflammation in patients with severe COPD exacerbations which further complicates the pathogenesis and pathophysiology of an already complicated disease [42]. The Evaluation of COPD Longitudinally to Identify Predictive Surrogate End-points (ECLIPSE) cohort also demonstrated that 37.4% of patients with stable COPD had eosinophil counts persistently ≥ 2% at all visits, 13.6% had eosinophil counts persistently < 2% at all visits, and an intermittent group of 49% subjects had variable eosinophil counts that oscillated above and below 2% [43].
Oxidative stress plays an important role in the pathogenesis and pathophysiology of COPD but not asthma. Shortage of antioxidant nutrients, especially of ascorbic acid and lycopene, as well as reduced glutathione can be found in some of COPD patients but not those with bronchial asthma [44]. It had been shown that there were significant differences in the CD83(+) dendritic and B cells in smoking asthmatics render those patients less responsive to corticosteroids and more susceptible to infections [31].
In addition asthma cytotoxic immune response is represented by granzyme A and B, whereas in smoking asthmatic perforin and 8-OHdG are additionally involved, resembling the immune response of COPD [45]. Those markers could be used to identify ACOS patients in the future.
Mitochondrial dysfunction due to oxidative stress -normally a characteristic of COPD- also contributes to the pathogenesis of ACOS [46].
Finally, genetic factors can also play an important role and there are genetic variants associated with ACOS reported in the literature such as single nucleotide polymorphisms in the genes CSMD1 and GPR65 [47].
Risks factors
Ageing is associated with a marked decrease in the prevalence of diagnosed asthma and with a marked increase in the prevalence of COPD. The prevalence of the overlap of asthma and COPD is also increased with ageing [48, 49]. Kiljander and colleagues suggested that age more than 60 years and smoking for more than 20 pack-years are the best predictors of ACOS. COPD is six times more prevalent among patients who meet these two criteria, compared to patients who do not fulfill any of them (odds ratio 6.08 [2.11, 17.49]) [50].
Moreover, patients with ACOS have lower cumulative smoking, suffer more from obesity and atopic diseases and used more asthma treatments compared to COPD patients. The authors stated that the dyspnea, quality of life, exacerbations, comorbidities and mortality are not different from COPD patients [51]. Data on sex predominance of ACOS is conflicting [24, 52].
Finally, ACOS shares risk factors with asthma [53]. Subjects who developed asthma before the age of 40 years may be at higher risk for ACOS [24].
Diagnosis
Spanish Respiratory Society proposed diagnostic criteria for ACOS in 2012. Diagnosis is confirmed when 2 major and 2 minor criteria are met (Table 1) [54].
However, globally consensus is still lacking on the existence of ACOS as a separate syndrome, and on its diagnostic criteria [55].
According to GOLD/GINA recommendations normal FEV1/FVC pre- or post bronchodilatator test is not compatible with ACOS unless there is other evidence of chronic airflow limitation. FEV1 more or equal to 80% predicted is compatible with diagnosis of mild form of ACOS. FEV1 less than 80% is an indicator of severity and possible complications in the future. Post bronchodilatator increase in FEV1 more or equal to 12% and 200 ml from baseline is common in ACOS if FEV1 is low. Moreover an increase in FEV1 more than 15% and 400 ml is also compatible with ACOS diagnosis [22].
Other methods such as the assessment of fractional exhaled nitric oxide (FENO) and immunoglobulin E (IgE) in COPD patients were also used in the diagnosis of ACOS. When the cutoff value of FENO was 35 ppb the prevalence rate of ACOS was 16.3% in COPD group. But if both FENO and IgE were assessed, the high-FENO/high-IgE group was 7.8% among patients with COPD. This indicates both asthma-like airway inflammation and the presence of atopy in COPD patients [56].
Future studies may demonstrate other markers and criteria for diagnosing ACOS. A recent study demonstrates that inflammatory cytokines IL-4, IL-8, IL-10, and TNF-α are different among control, asthma, COPD with exacerbation and ACOS groups and might be useful in assessing the development of these diseases [57].
Radiology investigations
It has been suggested that ACOS has radiological features similar to COPD. However, recent studies suggested patients with ACOS have less emphysema, that is differently distributed; they also have greater post-bronchodilatation variations in air trapping, compared to patients with COPD, suggesting a different CT densitometry between the two clinical entities [58]. Interstitial changes in ACOS patients are associated with age and smoking history and can be found in up to 23.3%. ACOS with interstitial changes tend to have a higher rate of fungal sensitization [59].
The percentage of total cross-sectional area of pulmonary vessels less than 5 mm2 is also higher in ACOS rather than COPD patients [60]. On the other hand nearly half of the patients with asthma and fixed airflow limitations in elderly asthma patients show coexisting COPD components [61].
Nevertheless current data is too limited to confirm the possibility of characteristic or pathognomonic radiological features in ACOS.
Assessment
There is still debatable whether ACOS represents a more severe disease than asthma or COPD. Several studies concluded that COPD patients have a more pronounced rate of decline in FEV1, SGRQ and 6MWD compared to asthma and ACOS patients [62]. However, others found that ACOS is more likely to be associated with low lung function, low socioeconomic status, short education duration, lower self-rated health, and past diagnosis of pulmonary tuberculosis or bronchiectasis. Multiple logistic regression analysis revealed that both overlap syndrome and asthma groups were independently associated with lower self-rated health after adjustment for age, sex, socioeconomic status, education level, smoking status, comorbidities, and lung function [63]. ACOS appears to be associated with the poorest health-related quality of life (HRQL) [64].
Compared to the COPD cohort, ACOS patients had a 1.13-fold adjusted incidence rate ratio of pneumonia and a 2.58-fold adjusted incidence rate ratio of acute exacerbation [65]. Past medical history of tuberculosis was more frequent among patients with ACOS. Within the ACOS cohort, the adjusted hazard ratio for tuberculosis was higher among patients receiving short acting beta agonists and short acting muscarinic antagonists (3.06), long acting beta agonists and long acting muscarinic antagonists (3.68), and inhaled corticosteroids (2.79, all p < 0.05). Also, patients with more than 15 outpatient visits and hospitalizations per year demonstrated the highest adjusted hazard ratio for tuberculosis (8.09; 95% CI, 6.85-9.56) [66]. Pulmonary embolism appears to be more frequent among patients with ACOS, compared to COPD alone. The risk of pulmonary embolism also increases with the number of outpatient visits and hospitalizations [67]. On the other hand ACOS patients appear to have less emphysema [47].
In general subjects with ACOS were more likely to have respiratory symptoms, physical impairment, and to report hospital admissions compared to asthma or COPD alone [24, 48, 68, 69].. On the other hand, ACOS patients have a better one-year prognosis than clinically similar COPD patients with no ACOS criteria [52]. Finally, 15-year mortality rate showed that long-term prognosis of ACOS is similar to COPD, and worse than asthma and healthy controls [70].
In adjusted analyses, allergic rhinitis, anxiety, gastroesophageal reflux disease, and osteoporosis were more frequent in ACOS than COPD. Chronic kidney disease and ischemic heart disease were less frequent. Still, in patients with ACOS, cardiovascular diseases showed the strongest prognosis for hospitalization [71]. The ACOS group was more likely to have at least one comorbidity than the COPD group [72].
Vitamin D deficiency is present in ACOS patients and circulating 25(OH)D level may be of prognostic significance, since a positive correlation was found between 25(OH)D level and FEV1, forced vital capacity, forced expiratory flow between 25 and 75% of FVC, and peak expiratory flow [73].
Management
Until now only limited data exist on the management of ACOS, mainly because ACOS patients were excluded by most COPD or asthma trials. The management should include smoking cessation, oxygen supplementation, pulmonary rehabilitation, vaccines and management of comorbidities since all of these are well justified clinically [74, 75].
There is consensus that first-line treatment for ACOS is the combination of a long-acting β2-agonist and inhaled steroid, and this combination can be used with a long-acting antimuscarinic agent (triple therapy) for severe ACOS [55].
As mentioned, very limited data are available from randomised controlled trials. A 12-week, randomized, open-label cross-over study was conducted in 16 patients with ACOS compared the effectiveness of once-daily fluticasone furoate/vilanterol vs. twice-daily fluticasone propionate/salmeterol. Furoate/vilanterol was found to provide substantial improvement in lung function, indicating that this combination should be considered for the treatment of ACOS [76]. Another study which included 40 stable ACOS patients and 100 stable COPD patients with no differences between groups for sex, age, smoking history, body mass index, FEV1%predicted, vital capacity results and their ratios of residual volume to total lung capacity demonstrated that compared to baseline, budesonide/formoterol treatment significantly increased the FEV1 and decreased the degree of airway wall thickness as well as pulmonary microvascular density (% cross-sectional area < 5) in ACOS patients [60].
While inhaled corticosteroids are recommended in the management of patients with ACOS, its effectiveness is controversial. In a observational 12-year retrospective cohort study involving 125 patients by Lim and coworkers, ICS treatment was not associated with significant improvements in the annual rate of decrease in FEV1, the incidence of severe exacerbations or the overall mortality compared with the non-ICS treatment group [77]. Thus individualized management is probably the best option at present. Among the predictors for ICS response may be high sputum eosinophil counts and bronchial wall thickening on chest high-resolution computed tomography [78].
Montelukast administration showed good results in asthma patients who smoke suggesting that leukotrienes may play an important role in this particular case. More studies are required to determine whether leukotriene modifiers can be recommended for the manageent of ACOS patients [79].
Multiple studies suggested that phospodiasteraze 4 inhibitors (PDEI) such as roflumilast can significantly improve pre-bronchodilator FEV1 and reduce the rate of moderate to severe exacerbations [80, 81]. Evidence show that asthma patient can also benefit from treatment with roflumilast since it decreases airway inflammation, remodeling and hyperresponsiveness [82, 83]. The results are better when combined with montelukast or ICS [82, 84]. It also enhances efficacy of the concomitant ICS/LABA/LAMA therapy [85]. Therefore, it is logical to presume that roflumilast may be helpful in the treatment of ACOS. However, it should be used cautiously and only in severe cases, not controlled with other medications, given its frequent and significant adverse events.
Recently, several reports demonstrated that anti-IgE therapy (omalizumab) may be an effective and safe therapy for patients with ACOS [86]. The efficacy was demonstrated in a 12 months study, in a small group (10 patients) treated with omalizumab. After the treatment patients had a decreased IgE, FENO, eosinophil, neutrophils, macrophages, eosinophil cationic peptide and serum IL-4 levels. They also had decreased dyspnea, wheezing, bronchial hyper-responsiveness) and migraine attacks [87] (Table 2).
Conclusion
ACOS represent a relatively new syndrome in the literature of pulmonary medicine and its definition, etiology, pathophysiology, management and treatment are not clear yet. Therefore, there are still very limited recommendations and guidelines.
There is a critical need to better define the management of this syndrome that we believe it refers primarily to the smoking asthmatic. Large, well conducted trials are urgently required to inform the diagnosis and management of ACOS. Unfortunately, clinicians have to manage this syndrome empirically at present.
Abbreviations
- 6MWD:
-
Six-minute walk test
- ACOS:
-
Asthma-COPD overlap syndrome
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computer tomography
- FENO:
-
Fractional exhaled nitric oxide
- FEV1:
-
Forced expiratory volume
- FEV1:
-
Forced expiratory volume in 1 second
- FVC:
-
Forced vital capacity
- GINA:
-
Global initiative for asthma
- GOLD:
-
Global strategy for diagnosis, management, and prevention of COPD
- HRQL:
-
Health-related quality of life
- ICS:
-
Inhailed corticosteroids
- IgE:
-
Immunoglobulin E
- IL:
-
Interleukin
- LABA:
-
Long acting beta agonists
- LAMA:
-
Long acting muscarinic agents
- PDEI:
-
Phospodiasteraze 4 inhibitors
- SAMA:
-
Short acting muscarinic agent
- SGRQ:
-
St George’s respiratory questionnaire
- TNF-α:
-
Tumor necrosis factor α
References
Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007. doi:10.1164/rccm.200703-456SO.
Rycroft CE, Heyes A, Lanza L, Becker K. Epidemiology of chronic obstructive pulmonary disease: a literature review. Int J Chron Obstruct Pulmon Dis. 2012. doi:10.2147/COPD.S32330.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006. doi:10.1371/journal.pmed.0030442.
Miłkowska-Dymanowska J, Białas AJ, Zalewska-Janowska A, Górski P, Piotrowski WJ. Underrecognized comorbidities of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015. doi:10.2147/copd.s82420.
To T, Stanojevic S, Moores G, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012. doi:10.1186/1471-2458-12-204.
Mukherjee M, Stoddart A, Gupta RP, et al. The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: analyses of standalone and linked national databases. BMC Med. 2016. doi:10.1186/s12916-016-0657-8.
Ehteshami-Afshar S, FitzGerald JM, Carlsten C, et al. The impact of comorbidities on productivity loss in asthma patients. Respir Res. 2016. doi:10.1186/s12931-016-0421-9.
Tay TR, Radhakrishna N, Hore-Lacy F, et al. Comorbidities in difficult asthma are independent risk factors for frequent exacerbations, poor control and diminished quality of life. Respirology (Carlton, Vic). 2016. doi:10.1111/resp.12838.
Orie NGM, Sluiter HJ, de Vries K, et al. The host factor in bronchitis. In: Orie NGM, Sluiter HJ, editors. Bronchitis: an international symposium. Assen: Royal van Gorcum; 1961.
Orie NGM, van der Lende R, editors. Bronchitis III: Third international symposium on bronchitis. Assen: Royal van Gorcum; 1970. p. 115.
Barnes PJ. Against the Dutch hypothesis: asthma and chronic obstructive pulmonary disease are distinct diseases. Am J Respir Crit Care Med. 2006. doi:10.1164/rccm.2604008.
Rhee CK, Yoon HK, Yoo KH, et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. Copd. 2014. doi:10.3109/15412555.2013.831061.
Gerhardsson de Verdier M, Andersson M, Kern DM, Zhou S, Tunceli O. Asthma and chronic obstructive pulmonary disease overlap syndrome: doubled costs compared with patients with asthma alone. Value Health. 2015. doi:10.1016/j.jval.2015.04.010.
Kraft M. Asthma and chronic obstructive pulmonary disease exhibit common origins in any country! Am J Respir Crit Care Med. 2006. doi:10.1164/rccm.2604007.
Tzortzaki EG, Proklou A, Siafakas NM. Asthma in the elderly: can we distinguish it from COPD? J Allergy (Cairo). 2011. doi:10.1155/2011/843543.
Al-Kassimi FA, Abba AA, Al-Hajjaj MS, et al. Asthma masquerading as chronic obstructive pulmonary disease: a study of smokers fulfilling the GOLD definition of chronic obstructive pulmonary disease. Respiration. 2011. doi:10.1159/000323075.
Reddel HK. Treatment of overlapping asthma-chronic obstructive pulmonary disease: can guidelines contribute in an evidence-free zone? J Allergy Clin Immunol. 2015. doi:10.1016/j.jaci.2015.06.043.
Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009. doi:10.1136/thx.2008.108027.
Chatkin JM, Dullius CR. The management of asthmatic smokers. Asthma Res Pract. 2016. doi:10.1186/s40733-016-0025-7.
Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2016. Available from: http://www.ginasthma.org/.
Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017. Available from: http://www.goldcopd.org
A joint project of GINA and GOLD. Diagnosis of Diseases of Chronic Airflow Limitation: Asthma, COPD, and Asthma-COPD Overlap Syndrome. 2015.
Guerriero M, Caminati M, Paiano S, et al. The prevalence of asthma–chronic obstructive pulmonary disease overlap syndrome (ACOS) in a Northern Italy general population sample. Eur Respir J. 2015. doi:10.1183/13993003.congress-2015.PA4064.
Barrecheguren M, Roman-Rodriguez M, Miravitlles M. Is a previous diagnosis of asthma a reliable criterion for asthma-COPD overlap syndrome in a patient with COPD? Int J Chron obstruct Pulmon Dis. 2015. doi:10.2147/copd.s87025.
Cazzola M, Rogliani P. Do we really need asthma-chronic obstructive pulmonary disease overlap syndrome? J Allergy Clin Immunol. 2016. doi:10.1016/j.jaci.2016.04.028.
Agusti A, Bel E, Thomas M, et al. Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J. 2016. doi:10.1183/13993003.01359-2015.
Kostikas K, Clemens A, Patalano F. The asthma-COPD overlap syndrome: do we really need another syndrome in the already complex matrix of airway disease? Int J Chron Obstruct Pulmon Dis. 2016. doi:10.2147/copd.s107307.
Vanfleteren LEGW, Kocks JWH, Stone IS, et al. Moving from the Oslerian paradigm to the post-genomic era: are asthma and COPD outdated terms? Thorax. 2014. doi:10.1136/thoraxjnl-2013-203602.
Agusti A, Anto JM, Auffray C, et al. Personalized respiratory medicine: exploring the horizon, addressing the issues. Summary of a BRN-AJRCCM workshop held in Barcelona on June 12, 2014. Am J Respir Crit Care Med. 2015. doi:10.1164/rccm.201410-1935PP.
Ritchie MD, de Andrade M, Kuivaniemi H. The foundation of precision medicine: integration of electronic health records with genomics through basic, clinical, and translational research. Front Genet. 2015. doi:10.3389/fgene.2015.00104.
Tsoumakidou M, Elston W, Zhu J, et al. Cigarette smoking alters bronchial mucosal immunity in asthma. Am J Respir Crit Care Med. 2007. doi:10.1164/rccm.200607-908OC.
Kay AB, Phipps S, Robinson DS. A role for eosinophils in airway remodelling in asthma. Trends Immunol. 2004. doi:10.1016/j.it.2004.07.006.
Virk H, Arthur G, Bradding P. Mast cells and their activation in lung disease. Transl Res. 2016. doi:10.1016/j.trsl.2016.01.005.
Robinson DS. The role of the mast cell in asthma: induction of airway hyperresponsiveness by interaction with smooth muscle? J Allergy Clin Immunol. 2004. doi:10.1016/j.jaci.2004.03.034.
Cukic V, Lovre V, Dragisic D, Ustamujic A. Asthma and chronic obstructive pulmonary disease (COPD) – differences and similarities. Materia Socio-Medica. 2012. doi:10.5455/msm.2012.24.100-105.
Lee YJ, Kim KW, Choi BS, Sohn MH, Kim KE. Clinical characteristics of eosinophilic and noneosinophilic asthma in children. Acta paediatrica (Oslo, Norway : 1992). 2013. doi:10.1111/apa.12046.
Brooks CR, van Dalen CJ, Zacharasiewicz A, et al. Absence of airway inflammation in a large proportion of adolescents with asthma. Respirology (Carlton, Vic). 2015. doi:10.1111/resp.12701.
Mauad T, Dolhnikoff M. Pathologic similarities and differences between asthma and chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2008. doi:10.1097/MCP.0b013e3282f19846.
Ravensberg AJ, Slats AM, van Wetering S, et al. CD8(+) T cells characterize early smoking-related airway pathology in patients with asthma. Respir Med. 2013. doi:10.1016/j.rmed.2013.03.018.
Barnes PJ, Shapiro SD, Pauwels RA. Chronic obstructive pulmonary disease: molecular and cellular mechanisms. Eur Respir J. 2003;22(4):672–88.
Givi ME, Peck MJ, Boon L, Mortaz E. The role of dendritic cells in the pathogenesis of cigarette smoke-induced emphysema in mice. Eur J Pharmacol. 2013. doi:10.1016/j.ejphar.2013.09.027.
Siva R, Green RH, Brightling CE, et al. Eosinophilic airway inflammation and exacerbations of COPD: a randomised controlled trial. Eur Respir J. 2007. doi:10.1183/09031936.00146306.
Singh D, Kolsum U, Brightling CE, et al. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J. 2014. doi:10.1183/09031936.00162414.
Kodama Y, Kishimoto Y, Muramatsu Y, et al. Antioxidant nutrients in plasma of Japanese patients with chronic obstructive pulmonary disease (COPD), asthma-COPD overlap syndrome, and bronchial asthma. Clin Respir J. 2015. doi:10.1111/crj.12436.
Proklou A, Soulitzis N, Neofytou E, et al. Granule cytotoxic activity and oxidative DNA damage in smoking and nonsmoking patients with asthma. Chest. 2013. doi:10.1378/chest.13-0367.
Carpagnano GE, Lacedonia D, Malerba M, et al. Analysis of mitochondrial DNA alteration in new phenotype ACOS. BMC Pulmon Med. 2016. doi:10.1186/s12890-016-0192-6.
Hardin M, Cho M, McDonald ML, et al. The clinical and genetic features of COPD-asthma overlap syndrome. Eur Respir J. 2014. doi:10.1183/09031936.00216013.
de Marco R, Pesce G, Marcon A, et al. The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PLoS One. 2013. doi:10.1371/journal.pone.0062985.
Zeki AA, Schivo M, Chan A, Albertson TE, Louie S. The asthma-COPD overlap syndrome: a common clinical problem in the elderly. J Allergy. 2011. doi:10.1155/2011/861926.
Kiljander T, Helin T, Venho K, Jaakkola A, Lehtimaki L. Prevalence of asthma-COPD overlap syndrome among primary care asthmatics with a smoking history: a cross-sectional study. NPJ Prim Care Respir Med. 2015. doi:10.1038/npjpcrm.2015.47.
Caillaud D, Chanez P, Escamilla R, et al. Asthma-COPD overlap syndrome (acos) versus “pure” copd: a distinct phenotype? Allergy. 2016. doi:10.1111/all.13004.
Cosio BG, Soriano JB, Lopez-Campos JL, et al. Defining the Asthma-COPD overlap syndrome in a COPD cohort. Chest. 2015. doi:10.1378/chest.15-1055.
de Marco R, Marcon A, Rossi A, et al. Asthma, COPD and overlap syndrome: a longitudinal study in young European adults. Eur Respir J. 2015. doi:10.1183/09031936.00008615.
Soler-Cataluna JJ, Cosio B, Izquierdo JL, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol. 2012. doi:10.1016/j.arbres.2011.12.009.
Miravitlles M, Alcazar B, Alvarez FJ, et al. What pulmonologists think about the asthma-COPD overlap syndrome. Int J Chron Obstruct Pulmon Dis. 2015. doi:10.2147/copd.s88667.
Tamada T, Sugiura H, Takahashi T, et al. Biomarker-based detection of asthma-COPD overlap syndrome in COPD populations. Int J Chron Obstruct Pulmon Dis. 2015. doi:10.2147/copd.s88274.
Huang AX, Lu LW, Liu WJ, Huang M. Plasma inflammatory cytokine IL-4, IL-8, IL-10, and TNF-alpha levels correlate with pulmonary function in patients with asthma-chronic obstructive pulmonary disease (COPD) overlap syndrome. Med Sci Monit. 2016;22:2800–8.
Gao Y, Zhai X, Li K, et al. Asthma COPD overlap syndrome on CT densitometry: a distinct phenotype from COPD. Copd. 2016. doi:10.3109/15412555.2015.1102874.
Chiba S, Tsuchiya K, Nukui Y, et al. Interstitial changes in asthma-COPD overlap syndrome (ACOS). Clin Respir J. 2016. doi:10.1111/crj.12461.
Suzuki T, Tada Y, Kawata N, et al. Clinical, physiological, and radiological features of asthma-chronic obstructive pulmonary disease overlap syndrome. Int J Chron Obstruct Pulmon Dis. 2015. doi:10.2147/copd.s80022.
Tamada T, Sugiura H, Takahashi T, et al. Coexisting COPD in elderly asthma with fixed airflow limitation: assessment by DLco %predicted and HRCT. J Asthma. 2016. doi:10.1080/02770903.2016.1247168.
Fu JJ, Gibson PG, Simpson JL, McDonald VM. Longitudinal changes in clinical outcomes in older patients with asthma, COPD and asthma-COPD overlap syndrome. Respiration. 2014. doi:10.1159/000352053.
Chung JW, Kong KA, Lee JH, et al. Characteristics and self-rated health of overlap syndrome. Int J Chron Obstruct Pulmon Dis. 2014. doi:10.2147/copd.s61093.
Kauppi P, Kupiainen H, Lindqvist A, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011. doi:10.3109/02770903.2011.555576.
Chung WS, Lin CL, Kao CH. Comparison of acute respiratory events between asthma-COPD overlap syndrome and COPD patients: a population-based cohort study. Medicine. 2015. doi:10.1097/md.0000000000000755.
Yeh JJ, Wang YC, Kao CH. Asthma-chronic obstructive pulmonary diseases overlap syndrome increases the risk of incident tuberculosis: a national cohort study. PLoS One. 2016. doi:10.1371/journal.pone.0159012.
Yeh JJ, Wang YC, Kao CH. Asthma-chronic obstructive pulmonary disease overlap syndrome associated with risk of pulmonary embolism. PLoS One. 2016. doi:10.1371/journal.pone.0162483.
Miravitlles M, Soriano JB, Ancochea J, et al. Characterisation of the overlap COPD-asthma phenotype. Focus on physical activity and health status. Respir Med. 2013. doi:10.1016/j.rmed.2013.03.007.
Alshabanat A, Zafari Z, Albanyan O, Dairi M, FitzGerald JM. Asthma and COPD overlap syndrome (ACOS): a systematic review and meta analysis. PLoS One. 2015. doi:10.1371/journal.pone.0136065.
Sorino C, Pedone C, Scichilone N. Fifteen-year mortality of patients with asthma-COPD overlap syndrome. Eur J Intern Med. 2016. doi:10.1016/j.ejim.2016.06.020.
van Boven JF, Roman-Rodriguez M, Palmer JF, et al. Comorbidome, pattern, and impact of asthma-COPD overlap syndrome in real life. Chest. 2016. doi:10.1016/j.chest.2015.12.002.
Kumbhare S, Pleasants R, Ohar JA, Strange C. Characteristics and prevalence of asthma/chronic obstructive pulmonary disease overlap in the United States. Ann Am Thorac Soc. 2016. doi:10.1513/AnnalsATS.201508-554OC.
Odler B, Ivancso I, Somogyi V, et al. Vitamin D deficiency is associated with impaired disease control in asthma-COPD overlap syndrome patients. Int J Chron Obstruct Pulmon Dis. 2015. doi:10.2147/copd.s91654.
Corlateanu A, Pripa V, Montanari G, Botnaru V. Overlap syndrome in respiratory medicine: asthma and chronic obstructive pulmonary disease. J Cardiothorac Med. 2014;2(1):109–12.
Corlateanu A, Montanari G, Mathioudakis AG, Botnaru V, Siafakas N. Management of stable COPD: an update. Curr Respir Med Rev. 2013;9:352–9.
Ishiura Y, Fujimura M, Shiba Y, et al. A comparison of the efficacy of once-daily fluticasone furoate/vilanterole with twice-daily fluticasone propionate/salmeterol in asthma-COPD overlap syndrome. Pulm Pharmacol Ther. 2015. doi:10.1016/j.pupt.2015.10.005.
Lim HS, Choi SM, Lee J, et al. Responsiveness to inhaled corticosteroid treatment in patients with asthma-chronic obstructive pulmonary disease overlap syndrome. Ann Allergy Asthma Immunol. 2014. doi:10.1016/j.anai.2014.08.021.
Kitaguchi Y, Komatsu Y, Fujimoto K, Hanaoka M, Kubo K. Sputum eosinophilia can predict responsiveness to inhaled corticosteroid treatment in patients with overlap syndrome of COPD and asthma. Int J Chron Obstruct Pulmon Dis. 2012. doi:10.2147/copd.s30651.
Lazarus SC, Chinchilli VM, Rollings NJ, et al. Smoking affects response to inhaled corticosteroids or leukotriene receptor antagonists in asthma. Am J Respir Crit Care Med. 2007. doi:10.1164/rccm.200511-1746OC.
Calverley PM, Rabe KF, Goehring UM, et al. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet (London, England). 2009. doi:10.1016/s0140-6736(09)61255-1.
Wedzicha JA, Rabe KF, Martinez FJ, et al. Efficacy of roflumilast in the COPD frequent exacerbator phenotype. Chest. 2013. doi:10.1378/chest.12-1489.
Bateman ED, Goehring UM, Richard F, Watz H. Roflumilast combined with montelukast versus montelukast alone as add-on treatment in patients with moderate-to-severe asthma. J Allergy Clin Immunol. 2016. doi:10.1016/j.jaci.2015.11.035.
Kim SW, Kim JH, Park CK, et al. Effect of roflumilast on airway remodeling in a murine model of chronic asthma. Clin Exp Allergy. 2015. doi:10.1111/cea.12670.
Meltzer EO, Chervinsky P, Busse W, et al. Roflumilast for asthma: efficacy findings in placebo-controlled studies. Pulm Pharmacol Ther. 2015. doi:10.1016/j.pupt.2015.10.006.
Vos W, Hajian B, De Backer J, et al. Functional respiratory imaging to assess the interaction between systemic roflumilast and inhaled ICS/LABA/LAMA. Int J Chron Obstruct Pulmon Dis. 2016. doi:10.2147/copd.s93830.
Tat TS, Cilli A. Omalizumab treatment in asthma-COPD overlap syndrome. J Asthma. 2016. doi:10.1080/02770903.2016.1178281.
Yalcin AD, Celik B, Yalcin AN. Omalizumab (anti-IgE) therapy in the asthma-COPD overlap syndrome (ACOS) and its effects on circulating cytokine levels. Immunopharmacol Immunotoxicol. 2016. doi:10.3109/08923973.2016.1173057.
Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016. Available from: http://www.goldcopd.org.
Hoonhorst SJ, ten Hacken NH, Vonk JM, et al. Steroid resistance in COPD? Overlap and differential anti-inflammatory effects in smokers and ex-smokers. PLoS One. 2014. doi:10.1371/journal.pone.0087443.
Li H, Yang T, Ning Q, et al. Cigarette smoke extract-treated mast cells promote alveolar macrophage infiltration and polarization in experimental chronic obstructive pulmonary disease. Inhal Toxicol. 2015. doi:10.3109/08958378.2015.1116644.
Barnes PJ. Immunology of asthma and chronic obstructive pulmonary disease. Nat Rev Immunol. 2008. doi:10.1038/nri2254.
Peters SP, Kunselman SJ, Icitovic N, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med. 2010. doi:10.1056/NEJMoa1008770.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Authors’ contributions
AC, SC, AM: drafted and revised the manuscript. VB, NS: revised the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Corlateanu, A., Covantev, S., Mathioudakis, A.G. et al. Ashtma-Chronic obstructive pulmonary disease overlap syndrome (ACOS): current evidence and future research directions. COPD Res Pract 3, 6 (2017). https://doi.org/10.1186/s40749-017-0025-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40749-017-0025-x