Abstract
Digital technology offers scalable, real-time interventions for mental health promotion and treatment. This systematic review explores the opportunities and challenges associated with the use of digital technology in mental health, with a focus on informing mental health system strengthening interventions in the United Arab Emirates (UAE). Following PRISMA guidelines, a systematic search of databases was conducted up to August 2023 and identified a total of 8479 citations of which 114 studies were included in the qualitative analysis. The included studies encompass diverse digital interventions, platforms, and modalities used across various mental health conditions. The review identifies feasible, acceptable, and efficacious interventions, ranging from telehealth and mobile apps to virtual reality and machine learning models. Opportunities for improving access to care, reducing patients’ transfers, and utilizing real-world interaction data for symptom monitoring are highlighted. However, challenges such as digital exclusion, privacy concerns, and potential service replacement caution policymakers. This study serves as a valuable evidence base for policymakers and mental health stakeholders in the UAE to navigate the integration of digital technology in mental health services effectively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Digital technology has emerged as a sustainable and scalable tool for real-time interventions in mental health promotion and care [1]. It can reduce the prevalence of diseases and enhance mental health in communities by collecting, analyzing, and using data from a range of digital gadgets [2]. In the United Arab Emirates (UAE), the adoption of digital technologies in healthcare has been growing rapidly, especially during the COVID-19 pandemic [3, 4]. According to the Philips Health Trends Research for the UAE, there is high acceptance of digital health technologies, with 95% of respondents believing that technology can play an important role in managing their health more efficiently. Additionally, 72% of participants believe that virtual discussions with their doctors are as effective as face-to-face examinations [5].
Digital interventions are technology-driven, self-help, supervised, or unsupervised interventions focused on offering support for physical and mental health [6]. Various concepts such as mobile health (mHealth) and internet-based (eHealth) therapies powered by digital technologies are gaining ground to provide effective treatments for mental illnesses [7]. These interventions come in various forms, including telepsychiatry and mobile apps, which are being increasingly implemented in the UAE to enhance mental health services [8]. In Abu Dhabi, for example, mental health services were remodeled during the COVID-19 pandemic and tele-assessment mental health visits comprised 60% of all visits during April–May, 2020 [9].
Numerous research studies suggest that digital interventions are equally as effective as face-to-face therapy and more successful than standard care in the case of common anxiety disorder, depression, and cancer-related distress [10, 11]. Also, past systematic studies have found that videoconferencing-based counseling and psychotherapy can be effective and useful for a variety of age groups, urban and rural contexts, and mental health conditions such as anxiety [12]. Many studies have been carried out throughout the world to pinpoint possible factors that can promote and hinder the adoption of digital mental health such as reach, engagement (intervention) uptake, and outcome optimization [13,14,15]. It has been established that virtual reality (VR) technology is suitable, secure, and effective for both physical and psychological rehabilitation [16, 17]. On the contrary, some critics have claimed that the use of digital technology for mental health is a “one size fits all” approach, however, each case deserves a distinct intervention multidisciplinary diagnosis, and treatment [18].
A recent study found that nearly 60% of Portuguese psychologists perceived the techniques for remote psychological evaluation as inaccurate, increasing the risk of misdiagnosis, citing inadequate training and lack of experience as factors contributing to negative attitudes [19]. In addition, 30% of respondents in another study deemed digital evaluation to be precarious, primarily when assessing patients who were at significant risk of suicide [20]. However, evidence showed that the risk assessment of suicide can be obtained effectively via videoconference and in-home messaging devices as equally as it could be done in person [21]. Similarly, some studies have suggested that using digital technology will improve the current collaboration and prompt access to mental health services [7]. Nonetheless, several studies have transversally shown that many medical professionals lack training and expertise in digital mental health, which is why digital interventions end up in trial and error [22]. Moreover, several barriers to implementation are commonly quoted as the lack of ethical, legal, and regulatory frameworks for providing web-based mental health care [23], and potential security and confidentiality issues with digital systems [19]. Understanding the opportunities and challenges associated with the integration of digital technology in mental health services is vital for informed policymaking and the strengthening of mental health systems. The goal of this study was to consolidate the opportunities and challenges in leveraging digital technology for mental health system strengthening, to provide evidence-based to guide policymakers and mental health stakeholders in leveraging digital technology to strengthen mental health interventions in the UAE.
Methods
This study was conducted according to the Preferred Reporting Items of Systematic Reviews and Meta-Analysis (PRISMA) guidelines [24]. The protocol for the study was registered in the International Prospective Register of Systematic Reviews (PROSPERO 2023 CRD42023472455).
Data sources and search strategy
Databases including PubMed, EMBASE, PsycINFO, CINAHL, and the Cochrane Database were searched up to August 2023. Searches were limited to open access, English-language publications, and no other search restrictions were applied. Additional studies were identified by scanning the bibliographies of relevant reviews and eligible articles. An example of search terms used in different platforms is available in Supporting File 1.
Stud selection and inclusion
All studies self-identified as qualitative, quantitative, or mixed-methods original research reporting opportunities and/or challenges for the use of digital technology-specific mental health conditions were included. We excluded non-English language publications, opinion papers, editorials, commentaries, systematic reviews, and meta-analyses.
Data extraction (selection and coding)
All potentially eligible records were imported into Covidence systematic review management software and duplicate references were eliminated [25]. Two reviewers independently screened titles and abstracts using the predefined inclusion criteria, and a third reviewer resolved any detected conflicts. Two reviewers have independently assessed full texts against the inclusion criteria, with any remaining disagreements resolved through discussion with the project team. The data were extracted to include all details specific to the review question, including (i) authors, publication date, and study setting; (ii) sample characteristics, design, and data collection methods; and (iii) study findings.
Risk of bias (quality) assessment
The risk of bias in the included studies was assessed independently by two reviewers, with discrepancies resolved by the corresponding author. All eligible studies were assessed for quality, but no study was excluded on the grounds of quality. Quality assessment was assessed using the Newcastle-Ottawa Scale for quality assessment of observational studies, and it’s customized version for non-randomized trails [26], while randomized controlled trials were using Cochrane guidelines for quality assessment of RCTs [27]. The quality assessment of included studies is available in Supporting File 2.
Results
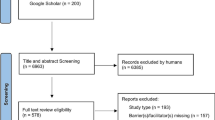
The initial search generated a total of 8479 citations where 1975 duplicates have been identified and removed by Convivence software or manually. Following the title and abstract screening for 6504 articles, 5174 were not relevant and from 1329 full-text articles retrieved and screened against the inclusion criteria, a total of 114 were included in the qualitative analysis (Fig. 1).
The included studies comprised a diverse range of perspectives from patients, healthcare workers, or both. Digital mental health interventions have been evaluated using different study designs and across various patient populations including traumatized children [28], individuals with social [29], generalized anxiety disorder (GAD) [30,31,32,33] and related disorders [34], depressive symptoms including late-life, post-partum, antenatal and postnatal depression [35,36,37,38,39,40,41,42,43,44], obsessive-compulsive disorder [45,46,47,48,49,50], schizophrenia [51,52,53,54], autism spectrum disorder [55], bipolar disorder [56], post-traumatic stress disorder (PTSD) [57,58,59,60,61,62], attention deficit hyperactivity disorder (ADHD) [63], substance use disorder [64, 65], panic disorder [66, 67], social phobia [68] and interventions for multiple mental health conditions [69,70,71,72,73,74,75,76,77,78]. A detailed summary of the included studies is available in Supporting File 3.
Digital mental health interventions, platforms, and modalities
Digital mental health interventions in the included studies span a broad array of technology platforms and telemental health modalities. These include utilizing platforms such as Zoom and other video platforms [79, 80], technology-supported mindfulness-based interventions [48, 81], VR technology [55], telemedicine mobile technologies [53, 82,83,84], and app-based interventions [76, 85,86,87,88], wearable devices [52, 56] and interventions utilizing cognitive control through entertainment software [38]. In addition to telephone-delivered interventions, spanning from telephone Cognitive behavioral therapy (CBT) [35] to nurse-delivered interpersonal psychotherapy (CNM-IPT) [89], and text messages [90]. Collaborative care models such as Telepsychiatry Collaborative Care (TCC) and Telepsychiatry/telepsychology Enhanced Referral (TER) integrate videoconferencing and digital platforms to enhance mental health support [91].
Opportunities for the use of digital technology in mental health
Feasibility, acceptance, and efficacy of digital interventions increase access to care
Patients and practitioners expressed a preference for continuing the use of telemental health including telephone-based and video-based services, as a sustainable mode of service delivery [45, 79, 92, 93] particularly valuable in rural areas, addressing the issue of limited access to mental health care [94,95,96]. Internet-guided self-help, individualized e-mail therapy, scenario-based CBT, mobile phones, and computer-aided telephone support were identified as feasible, acceptable, and efficacious mediums for service delivery [76, 97, 98], highlighting the diverse approaches available to practitioners and patients to overcoming barriers to access, particularly for patients with severe mental illness and chronic psychiatric disorders [51, 99,100,101]. The delivery of PowerPoint e-CBT modules via email was found to be a viable method for delivering CBT to individuals with GAD and a simple method for overcoming language, cultural, and travel barriers to accessing mental health resources [102].
Concerning specialized populations and conditions, digital health interventions were found to be acceptable, empowering individuals to take ownership of their healthcare needs [103]. Telepsychiatry in clinically unsupervised settings was considered feasible and as effective as standard care for depressed outpatients in terms of clinical outcomes, patient satisfaction, therapeutic relationship, and medication compliance [104]. Psychotherapy via telehealth for psychogenic nonepileptic seizures (PNES) was recognized as a viable option, eliminating barriers to access to mental health care [105], and online mental health treatment showed significant reductions in anxiety and depression in migrants [106]. Tele-delivered Problem-Solving Therapy (PST) for low-income homebound older adults was identified as an efficacious and economically viable treatment [107], and telepsychiatry was reported to be effective in treating posttraumatic stress symptoms, even in unstable and insecure settings [59], emphasizing the capability of digital interventions for reducing barriers to mental care.
Utilization of real-world patient interaction data for monitoring symptoms
Mobile health interventions, particularly those utilizing apps, were acknowledged as potential tools for mood tracking and assessment in youth with mental health problems [108]. Real-world interaction data from smartphones can be utilized as an early warning system detecting mood instability and changes and Ecological Momentary Assessment (EMA) approaches connect different forms of pervasive technology interaction (smartphones, wearables, social robots) to track everyday health status [56]. Another study of machine-learning models reported that patients’ social media activity captures objective linguistic and behavioral markers of psychotic relapse in young individuals with recent onset psychosis, and that machine-learning models were capable of making personalized predictions of imminent relapse hospitalizations at the patient-specific level using Facebook social media platform data [109]. Moreover, a study demonstrated the potential of smartphones with behavioral-sensing-installed data to identify behavioral patterns linked to symptomatic decline, enabling inferential modeling of sensor stream features to understand critical behavioral patterns [110].
Improving clinical outcomes and reducing patient transfer
Telehealth interventions, such as a one-time brief telephone intervention, were effective in engaging service members in PTSD treatment earlier, leading to immediate symptom reduction [58]. Other interventions, such as Tele-CBT and internet-based CBT, and other web-based self-help tools were effective in improving psychological distress and disordered eating [82, 111,112,113,114]. Also, scenario-based CBT apps demonstrated efficacy in reducing symptoms and improving mental health outcomes [85, 93].
Moreover, telepsychiatry showed significant effects on anxiety, with positive trends observed for depression [115,116,117,118,119], and other platforms demonstrated to positively influence the clinical condition of individuals with paranoid schizophrenia and related conditions [53, 120]. Similarly, patients with psychogenic nonepileptic seizures treated remotely with manual-based seizure therapy decreased seizure frequency and comorbid symptoms and improved functioning using telehealth [105]. Mobile phone-based assessments were recognized for their potential benefits in clinical care [90] and patient engagement with mobile apps was associated with improved outcomes [121]. The Strongest Families intervention, delivered remotely proved more effective than usual care in treating mild to moderate pediatric mental health disorders remotely using nonprofessionals [122].
Transdiagnostic and antidepressant interventions delivered via telehealth platforms, including decision support, proved effective in detecting and reducing suicidal ideation [123,124,125]. Additionally, nurse/midwife-delivered telephone Interpersonal Psychotherapy (IPT) was identified as an effective treatment for postpartum depression and anxiety [44, 89]. The ability for psychiatrists to see mental health patients via videoconferencing reduces the probability of patient transfers, aligning with patient preferences to remain in their communities [126].
Challenges to the use of digital technology in mental health
Extant barriers and concerns in digital mental health utilization
Despite the overall acceptability of digital mental health interventions due to their empowering nature for self-management, concerns including the potential for digital exclusion, privacy, and confidentiality were identified especially among older people [103, 127]. Additionally, there were fears that digital health interventions might be perceived as a complete replacement for all mental health services, raising caution regarding their comprehensive effectiveness [103].
Barriers to digital health utilization were reported as individuals with lower educational attainment faced challenges in using telehealth interventions indicating the need for targeted outreach and programming to enhance telehealth utilization [128]. Barriers included discomfort with tele-mental health, difficulties in connecting with providers, perceptions of decreased session numbers, technological challenges, and concerns about the effectiveness of phone-based interactions [129]. Despite the growth in telemental health use, it was reported to be insufficient in eliminating overall rural-urban differences in specialty care utilization [95], indicating persistent challenges in bridging the gap in access to mental health services between rural and urban populations. Also, mHealth transitions of care intervention (Mobile After-Care Support) for adults with schizophrenia-spectrum disorders immediately following a psychiatric hospitalization, are not routinely utilized in real-world clinical settings due to barriers related to feasibility, cost, and access [130].
Technology/modality -specific challenges and barriers
While app-based CBT demonstrated some clinical benefits, a study identified a range of barriers to engagement and emphasized caution in interpreting findings related to app effectiveness and careful consideration of the challenges associated with widespread adoption [131]. Also, the use of certified nurse-midwife telephone-administered Interpersonal Psychotherapy (CNM-IPT) presented challenges related to availability, highlighting the critical need for a careful assessment of intervention feasibility, and more research is still needed to evaluate the translation of such interventions into practice [89]. Although the addition of videoconferencing to regular care had a positive effect on patient satisfaction, overall, its impact was reported to be limited, and it might not offer significant added value to standard care for severe mental illness [132]. Finally, a study comparing in-person and home-based teletherapy for PTSD highlighted the need for increased doses (more sessions) to achieve therapeutic outcomes in home-based telehealth [61].
Mixed satisfaction with technology-mediated interactions
A study reported variability in satisfaction levels and reluctance with digital mental health as some individuals expressed satisfaction with technology-mediated interactions, while others were less content and remained hesitant about future use of digital mental health [133], prompting the need for more evidence on preferences and experiences with technology-mediated mental health interactions. Another study reports that youth at clinically high risk for psychosis or in the early stages exhibited communication patterns and perceptions in digital contexts that significantly differed from community controls such as reductions in the quality and quantity of social interactions [134].
Discussion
This study lays a robust foundation for informing mental health system strengthening interventions in the UAE, offering both promising opportunities and challenges to address in the integration of digital technology in mental healthcare provision. The current study identified a diverse range of digital mental health interventions, platforms, and modalities, including teletherapy, mobile apps, virtual reality therapy, and wearable devices. These technologies offer promise in increasing access to care, improving clinical outcomes, and empowering individuals to manage their mental well-being effectively.
The study reveals the potential of real-world interaction data from smartphones for monitoring symptoms, offering a proactive approach through early warning systems and ecological momentary assessments. Machine learning models, tapping into patients’ social media activity, demonstrate a groundbreaking capacity to predict psychotic relapses, showcasing the transformative power of technology in predictive and preventive mental health care. Moreover, digital interventions in the current study prove effective across a spectrum of mental health conditions, including PTSD, schizophrenia, and anxiety disorders. From Tele-CBT to nurse-delivered interpersonal psychotherapy, the diverse modalities cater to specialized populations, emphasizing the versatility of digital technology in mental health care. Furthermore, Innovative platforms like virtual reality technology and machine learning-driven models align with global trends, showing the potential to revolutionize mental health care. This study also reveals the effectiveness of smartphone behavioral-sensing-installed data, paving the way for personalized and patient-specific interventions. Policymakers can utilize this evidence to design tailored mental health programs that address the unique needs of different populations within the UAE.
The recent inauguration of the ‘Mindspire’ app at the UAE Innovates event at Expo by the Dubai Health Authority exemplifies the country’s commitment to leveraging technology to enhance mental health services [135]. By employing non-intrusive analysis and machine learning algorithms, the app offers personalized support and interventions for individuals suffering from depression. In addition, various other digital mental health technologies and platforms have emerged such as mobile applications, teletherapy platforms, wearable devices, and online counseling services. Platforms like Ayadi, Bright Shift, and LifeWorks offer online therapy sessions, providing individuals with convenient access to mental health support from qualified professionals [136].
The UAE’s digital health landscape also encompasses innovative approaches such as mindfulness-based interventions, virtual reality therapy, and machine learning algorithms for mood tracking and personalized recommendations. These technologies leverage artificial intelligence and data analytics to provide tailored interventions and support individuals in managing their mental well-being effectively [137]. However. Despite the proliferation of mental health, there remains a dearth of formal evaluations, highlighting the need for robust assessment frameworks to ensure efficacy and safety.
Challenges and considerations for policymakers
Despite the opportunities presented by digital mental health interventions, this systematic review emphasizes the challenge of potential digital exclusion. Policymakers in the UAE need to address this concern by implementing strategies that ensure equitable access to technology and digital literacy using initiatives focused on bridging the digital divide, especially among vulnerable populations [138].
The review highlights concerns related to privacy and confidentiality in the use of digital mental health services. Fortunately, the UAE government has already issued standards for telehealth services in the country to ensure the quality, safety, and effectiveness of telehealth interventions [139, 140]. These standards delineate key areas of telehealth, including teleconsultation, telediagnosis, telemonitoring, mHealth, telerobotics, and telepharmacy. New innovative digital mental health services should be developed with robust data protection regulations to safeguard users’ privacy and align with the existing guidelines and standards.
User acceptance and resistance to technology-mediated interactions are significant challenges identified in the review. Incorporating user-centric design principles in the development and implementation of digital mental health interventions is recommended as user feedback mechanisms, ongoing education, and awareness campaigns can contribute to fostering positive attitudes towards technology-enabled mental healthcare [141]. An essential consideration for policymakers is the integration of digital mental health services with traditional in-person services. Hybrid models that seamlessly blend technology-enabled interventions with existing mental health infrastructure could be explored [142].
Recommendations for policymakers and stakeholders
Policymakers should consider adopting and scaling the digital mental health platforms and modalities identified as effective in this review. Also, the integration of digital mental health services with existing in-person care is essential. Hybrid models that blend digital and traditional services should be explored to provide comprehensive mental health support. Such models can address varying patient needs and preferences, ensuring that no population is left underserved. Addressing the digital divide is crucial for the equitable implementation of digital mental health interventions. Initiatives focused on improving digital literacy, particularly among vulnerable and underserved populations, should be prioritized. Given the sensitive nature of mental health data, it is imperative that new digital health services are developed in compliance with robust data protection regulations. Policymakers should ensure that all digital interventions align with existing telehealth standards in the UAE, safeguarding patient privacy and maintaining the integrity of mental health services. More importantly, to maintain the efficacy and safety of digital mental health interventions, ongoing evaluation and research are necessary.
Limitations
One of the strengths of this study is the comprehensive approach to reviewing a wide array of digital mental health interventions across various platforms and patient populations, which lays a robust foundation for informing mental health system strengthening interventions. However, there are several limitations to consider; the study is limited by restricting the review to English-language publications, which may exclude relevant studies published in other languages. Moreover, there is a potential publication bias as the review primarily included open-access articles. Furthermore, the rapid evolution of digital technologies means that some of the reviewed interventions may become outdated quickly, necessitating ongoing research to keep up with technological advancements.
Conclusion
This systematic review provides a valuable evidence base for policymakers and mental health stakeholders in the UAE to navigate the landscape of digital mental health interventions. By capitalizing on the identified opportunities, addressing challenges, and implementing targeted recommendations, policymakers can contribute to the strengthening of the mental health system in the UAE. The integration of digital technology has the potential to revolutionize mental health care delivery, making it more accessible, flexible, and responsive to the diverse needs of the population. Through strategic and informed decision-making, the UAE can position itself at the forefront of leveraging digital innovation for mental health system development.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Bell IH, Thompson A, Valentine L, Adams S, Alvarez-Jimenez M, Nicholas J, Ownership. Use of, and Interest in Digital Mental Health Technologies among clinicians and Young People across a spectrum of Clinical Care Needs: cross-sectional survey. JMIR Ment Heal. 2022;9. https://doi.org/10.2196/30716.
Taylor CB, Ruzek JI, Fitzsimmons-Craft EE, Sadeh-Sharvit S, Topooco N, Weissman RS, et al. Using Digital Technology to reduce the prevalence of Mental Health disorders in populations: time for a New Approach. J Med Internet Res. 2020;22. https://doi.org/10.2196/17493.
Alnakhi WK, Mamdouh H, Hussain HY, Mudawi MS, Ibrahim GM, Al Balushi AJ, et al. Doctor for Every Citizen: Telehealth visits at Dubai Health Authority during COVID-19 pandemic in Dubai, United Arab Emirates. Healthcare. 2023;11. https://doi.org/10.3390/HEALTHCARE11030294.
Al Meslamani AZ, Aldulaymi R, El Sharu H, Alwarawrah Z, Ibrahim OM, Al Mazrouei N. The patterns and determinants of telemedicine use during the COVID-19 crisis: a nationwide study. J Am Pharm Assoc. 2022;62:1778. https://doi.org/10.1016/J.JAPH.2022.05.020.
Censuswide, UAE residents are using technology to take control of their health says Philips Health Trends Research - News | Philips. 2022. https://www.philips.ae/a-w/about/news/archive/standard/news/press/2023/20230309-uae-residents-are-using-technology-to-take-control-of-their-health-says-philips-health-trends-research.html. Accessed 29 Jun 2024.
Andersson G, Carlbring P, Titov N, Lindefors N. Internet interventions for adults with anxiety and Mood disorders: a Narrative Umbrella Review of recent Meta-analyses. Can J Psychiatry. 2019;64:465–70. https://doi.org/10.1177/0706743719839381.
Kemp J, Zhang T, Inglis F, Wiljer D, Sockalingam S, Crawford A, et al. Delivery of Compassionate Mental Health Care in a Digital Technology-Driven Age: scoping review. J Med Internet Res. 2020;22. https://doi.org/10.2196/16263.
Dias V, Mushtaha AS. Digital transformation: how has telemedicine impacted UAE’s healthcare sector during the Covid-19 pandemic? Int Conf Electr Comput Commun Mechatronics Eng ICECCME 2023. 2023.
Al Garhy M, Al Dhufairi A, Abdulrahman H, Al Maskari B, Ahmed N, Al Khamashi S, et al. Mental Health Services during the COVID-19 pandemic in Abu Dhabi, UAE. Prog Neurol Psychiatry. 2021;25:38–41. https://doi.org/10.1002/PNP.720.
Carlbring P, Andersson G, Cuijpers P, Riper H, Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn Behav Ther. 2018;47:1–18. https://doi.org/10.1080/16506073.2017.1401115.
Carl JR, Miller CB, Henry AL, Davis ML, Stott R, Smits JAJ, et al. Efficacy of digital cognitive behavioral therapy for moderate-to-severe symptoms of generalized anxiety disorder: a randomized controlled trial. Depress Anxiety. 2020;37:1168–78. https://doi.org/10.1002/DA.23079.
Berryhill MB, Halli-Tierney A, Culmer N, Williams N, Betancourt A, King M, et al. Videoconferencing psychological therapy and anxiety: a systematic review. Fam Pract. 2019;36:53–63. https://doi.org/10.1093/FAMPRA/CMY072.
Borghouts J, Pretorius C, Ayobi A, Abdullah S, Eikey EV. Factors influencing user engagement with digital mental health interventions. Front Digit Heal. 2023;5.
Gan DZQ, McGillivray L, Han J, Christensen H, Torok M. Effect of Engagement with Digital Interventions on Mental Health Outcomes: a systematic review and Meta-analysis. Front Digit Heal. 2021;3:764079.
Saleem M, Kühne L, de Santis KK, Christianson L, Brand T, Busse H. Understanding Engagement strategies in Digital Interventions for Mental Health Promotion: scoping review. JMIR Ment Heal. 2021;8. https://doi.org/10.2196/30000.
Pourmand A, Davis S, Lee D, Barber S, Sikka N. Emerging utility of virtual reality as a Multidisciplinary Tool in Clinical Medicine. Games Health J. 2017;6:263–70.
Qian J, McDonough DJ, Gao Z. The effectiveness of virtual reality Exercise on Individual’s physiological, psychological and rehabilitative outcomes: a systematic review. Int J Environ Res Public Health. 2020;17:1–17. https://doi.org/10.3390/IJERPH17114133.
Spadaro B, Martin-Key NA, Bahn S. Building the digital mental health ecosystem: opportunities and challenges for mobile health innovators. J Med Internet Res. 2021;23.
Mendes-Santos C, Weiderpass E, Santana R, Andersson G. Portuguese Psychologists’ Attitudes Toward Internet Interventions: Exploratory Cross-Sectional Study. JMIR Ment Heal. 2020;7(4)e16817 https//mental.jmir.org/2020/4/e16817. 2020;7:e16817. https://doi.org/10.2196/16817
Gilmore AK, Ward-Ciesielski EF. Perceived risks and use of psychotherapy via telemedicine for patients at risk for suicide. J Telemed Telecare. 2019;25:59–63. https://doi.org/10.1177/1357633X17735559.
Godleski L, Nieves JE, Darkins A, Lehmann L. VA telemental health: suicide assessment. Behav Sci Law. 2008;26:271–86. https://doi.org/10.1002/BSL.811.
Glueckauf RL, Maheu MM, Drude KP, Wells BA, Wang Y, Gustafson DJ, et al. Survey of psychologists’ telebehavioral health practices: technology use, ethical issues, and training needs. Prof Psychol Res Pract. 2018;49:205–19.
Feijt MA, De Kort YAW, Bongers IMB, IJsselsteijn WA. Perceived drivers and barriers to the adoption of eMental Health by psychologists: the construction of the levels of adoption of eMental Health Model. J Med Internet Res. 2018;20. https://doi.org/10.2196/JMIR.9485.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:332–6.
Covidence systematic review software. Veritas Health Innovation, Melbourne, Australia. https://support.covidence.org. Accessed 29 Jul 2023.
Wells G, Wells G, Shea B, Shea B, O’Connell D, Peterson J et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2014.
Higgins JP, Savovic J, Page MJ, Elbers RG, Sterne JA. Chapter 8: Assessing risk of bias in a randomized trial | Cochrane Training. https://training.cochrane.org/handbook/current/chapter-08. Accessed 29 Jan 2024.
Baker AJL, Konigsberg M, Brown E, Adkins KL. Successes, challenges, and opportunities in providing evidence-based teletherapy to children who have experienced trauma as a response to Covid-19: a national survey of clinicians. Child Youth Serv Rev. 2023;146:106819.
Nordh M, Wahlund T, Jolstedt M, Sahlin H, Bjureberg J, Ahlen J, et al. Therapist-guided internet-delivered cognitive behavioral therapy vs internet-delivered supportive therapy for children and adolescents with social anxiety disorder. JAMA Psychiatry. 2021;78:705.
Brenes GA, Danhauer SC, Lyles MF, Hogan PE, Miller ME. Telephone-delivered cognitive behavioral therapy and telephone-delivered nondirective supportive therapy for rural older adults with generalized anxiety disorder. JAMA Psychiatry. 2015;72:1012.
Brenes GA, Miller ME, Williamson JD, McCall WV, Knudson M, Stanley MA. A randomized controlled trial of telephone-delivered cognitive-behavioral therapy for late-life anxiety disorders. Am J Geriatr Psychiatry. 2012;20:707–16.
Brenes GA, Danhauer SC, Lyles MF, Anderson A, Miller ME. Long-Term effects of Telephone-Delivered psychotherapy for late-life GAD. Am J Geriatr Psychiatry. 2017;25:1249–57.
Oser M, Wallace ML, Solano F, Szigethy EM. Guided digital cognitive behavioral program for anxiety in primary care: propensity-matched controlled trial. JMIR Ment Heal. 2019;6:e11981.
Milosevic I, Cameron DH, Milanovic M, McCabe RE, Rowa K. Face-to-face versus video teleconference group cognitive behavioural therapy for anxiety and related disorders: a preliminary comparison. Can J Psychiatry. 2022;67:391–402.
Ngai F-W, Wong PW-C, Leung K-Y, Chau P-H, Chung K-F. The Effect of Telephone-based cognitive-behavioral therapy on postnatal depression: a Randomized Controlled Trial. Psychother Psychosom. 2015;84:294–303.
Corruble E, Swartz HA, Bottai T, Vaiva G, Bayle F, Llorca P-M, et al. Telephone-administered psychotherapy in combination with antidepressant medication for the acute treatment of major depressive disorder. J Affect Disord. 2016;190:6–11.
Barrera TL, Cummings JP, Armento M, Cully JA, Bush Amspoker A, Wilson NL, et al. Telephone-delivered cognitive-behavioral therapy for older, rural veterans with depression and anxiety in Home-based primary care. Clin Gerontol. 2017;40:114–23.
Anguera JA, Gunning FM, Areán PA. Improving late life depression and cognitive control through the use of therapeutic video game technology: a proof-of-concept randomized trial. Depress Anxiety. 2017;34:508–17.
Forsell E, Bendix M, Holländare F, von Szymanska B, Nasiell J, Blomdahl-Wetterholm M, et al. Internet delivered cognitive behavior therapy for antenatal depression: a randomised controlled trial. J Affect Disord. 2017;221:56–64.
Chokshi S, Senathirajah Y, Yadav V, Winsberg M, O’Callaghan E, Sullivan S et al. A comparative evaluation of measurement-based Psychiatric Care Delivered via Specialized Telemental Health platform Versus Treatment as Usual: a retrospective analysis. Cureus. 2022.
Farrer L, Christensen H, Griffiths KM, Mackinnon A. Web-based cognitive behavior therapy for Depression with and without Telephone Tracking in a National Helpline: secondary outcomes from a Randomized Controlled Trial. J Med Internet Res. 2012;14:e68.
Kok G, Burger H, Riper H, Cuijpers P, Dekker J, van Marwijk H, et al. The three-Month Effect of Mobile Internet-based cognitive therapy on the course of depressive symptoms in remitted recurrently depressed patients: results of a Randomized Controlled Trial. Psychother Psychosom. 2015;84:90–9.
Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN et al. Effect of Telephone-Administered vs Face-to-face cognitive behavioral therapy on adherence to Therapy and Depression outcomes among Primary Care patients. JAMA. 2012;307.
Dennis C-L, Grigoriadis S, Zupancic J, Kiss A, Ravitz P. Telephone-based nurse-delivered interpersonal psychotherapy for postpartum depression: nationwide randomised controlled trial. Br J Psychiatry. 2020;216:189–96.
Tie H, Krebs G, Lang K, Shearer J, Turner C, Mataix-Cols D, et al. Cost-effectiveness analysis of telephone cognitive–behaviour therapy for adolescents with obsessive–compulsive disorder. BJPsych Open. 2019;5:e7.
Pinciotti CM, Bulkes NZ, Horvath G, Riemann BC. Efficacy of intensive CBT telehealth for obsessive-compulsive disorder during the COVID-19 pandemic. J Obsessive Compuls Relat Disord. 2022;32:100705.
Lovell K, Cox D, Haddock G, Jones C, Raines D, Garvey R, et al. Telephone administered cognitive behaviour therapy for treatment of obsessive compulsive disorder: randomised controlled non-inferiority trial. BMJ. 2006;333:883.
Hawley LL, Rector NA, DaSilva A, Laposa JM, Richter MA. Technology supported mindfulness for obsessive compulsive disorder: self-reported mindfulness and EEG correlates of mind wandering. Behav Res Ther. 2021;136:103757.
Nair A, Turner C, Heyman I, Mataix-Cols D, Lovell K, Krebs G, et al. Moderators and predictors of outcomes in telephone delivered compared to face-to-face cognitive behaviour therapy for paediatric obsessive–compulsive disorder: preliminary evidence from a non-inferiority RCT. Cogn Behav Ther. 2019;48:353–68.
Cerea S, Ghisi M, Bottesi G, Carraro E, Broggio D, Doron G. Reaching reliable change using short, daily, cognitive training exercises delivered on a mobile application: the case of relationship obsessive compulsive disorder (ROCD) symptoms and cognitions in a subclinical cohort. J Affect Disord. 2020;276:775–87.
Lewis S, Ainsworth J, Sanders C, Stockton-Powdrell C, Machin M, Whelan P, et al. Smartphone-enhanced Symptom Management in psychosis: Open, Randomized Controlled Trial. J Med Internet Res. 2020;22:e17019.
Cella M, Okruszek Ł, Lawrence M, Zarlenga V, He Z, Wykes T. Using wearable technology to detect the autonomic signature of illness severity in schizophrenia. Schizophr Res. 2018;195:537–42.
Krzystanek M, Borkowski M, Skałacka K, Krysta K. A telemedicine platform to improve clinical parameters in paranoid schizophrenia patients: results of a one-year randomized study. Schizophr Res. 2019;204:389–96.
Ainsworth J, Palmier-Claus JE, Machin M, Barrowclough C, Dunn G, Rogers A, et al. A comparison of two delivery modalities of a Mobile phone-based Assessment for Serious Mental illness: native smartphone application vs text-Messaging only implementations. J Med Internet Res. 2013;15:e60.
Zhao J, Zhang X, Lu Y, Wu X, Zhou F, Yang S et al. Virtual reality technology enhances the cognitive and social communication of children with autism spectrum disorder. Front Public Heal. 2022;10.
Bennett CC, Ross MK, Baek E, Kim D, Leow AD. Predicting clinically relevant changes in bipolar disorder outside the clinic walls based on pervasive technology interactions via smartphone typing dynamics. Pervasive Mob Comput. 2022;83:101598.
Acierno R, Gros DF, Ruggiero KJ, Hernandez-Tejada MA, Knapp RG, Lejuez CW, Behavioral activation and therapeutic exposure for posttraumatic stress disorder, et al. A noninferiority trial of treatment delivered in person versus home-based telehealth. Depress Anxiety. 2016;33:415–23.
Stecker T, McHugo G, Xie H, Whyman K, Jones M. RCT of a brief phone-based CBT intervention to improve PTSD Treatment utilization by returning Service members. Psychiatr Serv. 2014;65:1232–7.
Knaevelsrud C, Brand J, Lange A, Ruwaard J, Wagner B. Web-based psychotherapy for posttraumatic stress disorder in war-traumatized arab patients: Randomized controlled trial. J Med Internet Res. 2015;17.
Ashwick R, Turgoose D, Murphy D. Exploring the acceptability of delivering Cognitive Processing Therapy (CPT) to UK veterans with PTSD over Skype: a qualitative study. Eur J Psychotraumatol. 2019;10.
Acierno R, Jaffe AE, Gilmore AK, Birks A, Denier C, Muzzy W, et al. A randomized clinical trial of in-person vs. home-based telemedicine delivery of prolonged exposure for PTSD in military sexual trauma survivors. J Anxiety Disord. 2021;83:102461.
Peterson AL, Mintz J, Moring JC, Straud CL, Young-McCaughan S, McGeary CA, et al. In-office, in-home, and telehealth cognitive processing therapy for posttraumatic stress disorder in veterans: a randomized clinical trial. BMC Psychiatry. 2022;22:41.
Myers K, Vander Stoep A, Zhou C, McCarty CA, Katon W. Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: a community-based randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2015;54:263–74.
Zanjani F, Miller B, Turiano N, Ross J, Oslin D. Effectiveness of telephone-based referral care management, a brief intervention to improve psychiatric treatment engagement. Psychiatr Serv. 2008;59:776–81. https://doi.org/10.1176/PS.2008.59.7.776/ASSET/IMAGES/LARGE/JJ14T1.JPEG.
Chermack ST, Bonar EE, Goldstick JE, Winters J, Blow FC, Friday S, et al. A randomized controlled trial for aggression and substance use involvement among veterans: impact of combining motivational interviewing, cognitive behavioral treatment and telephone-based Continuing Care. J Subst Abuse Treat. 2019;98:78–88.
Carlbring P, Bohman S, Brunt S, Buhrman M, Westling BE, Ekselius L, et al. Remote treatment of panic disorder: a randomized trial of internet-based cognitive behavior therapy supplemented with telephone calls. Am J Psychiatry. 2006;163:2119–25.
Oh J, Jang S, Kim H, Kim J-J. Efficacy of mobile app-based interactive cognitive behavioral therapy using a chatbot for panic disorder. Int J Med Inf. 2020;140:104171.
Carlbring P, Gunnarsdóttir M, Hedensjö L, Andersson G, Ekselius L, Furmark T. Treatment of social phobia: randomised trial of internet-delivered cognitive-behavioural therapy with telephone support. Br J Psychiatry. 2007;190:123–8.
Ebert D, Tarnowski T, Gollwitzer M, Sieland B, Berking M. A transdiagnostic internet-based maintenance treatment enhances the Stability of Outcome after Inpatient cognitive behavioral therapy: a Randomized Controlled Trial. Psychother Psychosom. 2013;82:246–56.
Andrews B, Klein B, Van Nguyen H, Corboy D, McLaren S, Watson S. Efficacy of a Digital Mental Health Biopsychosocial Transdiagnostic Intervention with or without therapist assistance for adults with anxiety and depression: adaptive randomized controlled trial. J Med Internet Res. 2023;25:e45135.
Dallinger VC, Krishnamoorthy G, du Plessis C, Pillai-Sasidharan A, Ayres A, Waters L, et al. Utilisation of Digital Applications for Personal Recovery Amongst Youth with Mental Health concerns. Int J Environ Res Public Health. 2022;19:16818.
Hohman JA, Martinez KA, Anand A, Rood M, Martyn T, Rose S, et al. Use of Direct-to-consumer telemedicine to Access Mental Health Services. J Gen Intern Med. 2022;37:2759–67.
Lawn S, Huang N, Zabeen S, Smith D, Battersby M, Redpath P, et al. Outcomes of telephone-delivered low-intensity cognitive behaviour therapy (LiCBT) to community dwelling australians with a recent hospital admission due to depression or anxiety: MindStep™. BMC Psychiatry. 2019;19:2.
Wu MS, Wickham RE, Chen S-Y, Chen C, Lungu A. Examining the Impact of Digital Components Across Different Phases of Treatment in a blended care cognitive behavioral therapy intervention for depression and anxiety: pragmatic retrospective study. JMIR Form Res. 2021;5:e33452.
Strid C, Andersson C, Forsell Y, Öjehagen A, Lundh L. Internet-based cognitive behaviour therapy and physical exercise – effects studied by automated telephone assessments in mental ill‐health patients; a randomized controlled trial. Br J Clin Psychol. 2016;55:414–28.
Moberg C, Niles A, Beermann D. Guided self-help works: Randomized Waitlist Controlled Trial of Pacifica, a Mobile App integrating cognitive behavioral therapy and mindfulness for stress, anxiety, and Depression. J Med Internet Res. 2019;21:e12556.
Ben-Zeev D, Brian RM, Jonathan G, Razzano L, Pashka N, Carpenter-Song E, et al. Mobile health (mHealth) versus clinic-based group intervention for people with serious mental illness: a randomized controlled trial. Psychiatr Serv. 2018;69:978–85.
Phang YS, Heaukulani C, Martanto W, Morris R, Tong MM, Ho R. Perceptions of a Digital Mental Health platform among participants with depressive disorder, anxiety disorder, and other clinically diagnosed Mental disorders in Singapore: usability and acceptability study. JMIR Hum Factors. 2023;10:e42167.
Buckman JEJ, Saunders R, Leibowitz J, Minton R. The barriers, benefits and training needs of clinicians delivering psychological therapy via video. Behav Cogn Psychother. 2021;49:696–720.
Zimmerman M, D’Avanzato C, King BT. Telehealth treatment of patients with major depressive disorder during the COVID-19 pandemic: comparative safety, patient satisfaction, and effectiveness to prepandemic in-person treatment. J Affect Disord. 2023;323:624–30.
Ritvo P, Knyahnytska Y, Pirbaglou M, Wang W, Tomlinson G, Zhao H, et al. Online mindfulness-based cognitive behavioral therapy intervention for Youth with Major Depressive disorders: Randomized Controlled Trial. J Med Internet Res. 2021;23:e24380.
Kim Y-R, Cardi V, Lee GY, An S, Kim J, Kwon G, et al. Mobile Self-Help interventions as Augmentation Therapy for patients with Anorexia Nervosa. Telemed e-Health. 2019;25:740–7.
Depp CA, Perivoliotis D, Holden J, Dorr J, Granholm EL. Single-Session Mobile-Augmented intervention in Serious Mental illness: A Three-Arm Randomized Controlled Trial. Schizophr Bull. 2019;45:752–62.
Elbogen EB, Dennis PA, Van Voorhees EE, Blakey SM, Johnson JL, Johnson SC, et al. Cognitive Rehabilitation with Mobile Technology and Social Support for Veterans with TBI and PTSD: a Randomized Clinical Trial. J Head Trauma Rehabil. 2019;34:1–10.
Hur J-W, Kim B, Park D, Choi S-WA, Scenario-Based. Cognitive behavioral therapy Mobile App to reduce dysfunctional beliefs in individuals with Depression: a Randomized Controlled Trial. Telemed e-Health. 2018;24:710–6.
Austin SF, Jansen JE, Petersen CJ, Jensen R, Simonsen E. Mobile App Integration into Dialectical Behavior Therapy for persons with Borderline personality disorder: qualitative and quantitative study. JMIR Ment Heal. 2020;7:e14913.
Christoforou M, Sáez Fonseca JA, Tsakanikos E. Two novel cognitive behavioral therapy–based mobile apps for Agoraphobia: Randomized Controlled Trial. J Med Internet Res. 2017;19:e398.
Bonet L, Torous J, Arce D, Blanquer I, Sanjuan J. ReMindCare App for early psychosis: pragmatic real world intervention and usability study. JMIR mHealth uHealth. 2020;8:e22997.
Posmontier B, Neugebauer R, Stuart S, Chittams J, Shaughnessy R. Telephone-administered interpersonal psychotherapy by nurse‐midwives for Postpartum Depression. J Midwifery Womens Health. 2016;61:456–66.
Palmier-Claus JE. RAAJMMBCLLBEKSWTLSW. Integrating mobile-phone based assessment for psychosis. BMC Psychiatry. 2013;13.
Hall JD, Danna MN, Hoeft TJ, Solberg LI, Takamine LH, Fortney JC et al. Patient and clinician perspectives on two telemedicine approaches for treating patients with mental health disorders in underserved areas. Am Board Fam Med. https://doi.org/10.3122/jabfm.2022.03.210377
Lal S, Abdel-Baki A, Lee H. Telepsychiatry services during < scp > COVID ‐19: A < scp > cross‐sectional survey on the experiences and perspectives of young adults with < scp > first‐episode psychosis. Early Interv Psychiatry. 2023;17:368–77.
Lynch DA, Stefancic A, Cabassa LJ, Medalia A. Client, clinician, and administrator factors associated with the successful acceptance of a telehealth comprehensive recovery service: a mixed methods study. Psychiatry Res. 2021;300:113871.
Grady B, Singleton M. Telepsychiatry Coverage to a rural Inpatient Psychiatric Unit. Telemed e-Health. 2011;17:603–8.
Patel SY, Huskamp HA, Busch AB, Mehrotra A. Telemental Health and US rural–urban differences in Specialty Mental Health Use, 2010–2017. Am J Public Health. 2020;110:1308–14.
Dong F, Jumper MBE, Becker-Haimes EM, Vatza C, Miao L, Conroy C, et al. Tele-Mental Health Transitions for Pennsylvania Coordinated Specialty Care Programs for early psychosis during the COVID-19 pandemic. Psychiatr Q. 2023;94:89–102.
Zaheer S, Garofalo V, Rodie D, Perivolaris A, Chum J, Crawford A, et al. Computer-aided telephone support for primary care patients with common Mental Health conditions: Randomized Controlled Trial. JMIR Ment Heal. 2018;5:e10224.
Vernmark K, Lenndin J, Bjärehed J, Carlsson M, Karlsson J, Öberg J, et al. Internet administered guided self-help versus individualized e-mail therapy: a randomized trial of two versions of CBT for major depression. Behav Res Ther. 2010;48:368–76.
Shakeri A, Chu C, Stamenova V, Fang J, Barker LC, Vigod SN et al. Comparison of Healthcare utilization between Telemedicine and Standard Care: a propensity-score matched Cohort Study among individuals with Chronic Psychotic disorders in Ontario, Canada. Schizophr Bull Open. 2022;3.
Carpenter-Song E, Jonathan G, Brian R, Ben-Zeev D. Perspectives on Mobile Health Versus Clinic-Based Group interventions for people with Serious Mental illnesses: a qualitative study. Psychiatr Serv. 2020;71:49–56.
Sreejith G, Menon V. Mobile Phones as a Medium of Mental Health Care Service Delivery: perspectives and barriers among patients with severe Mental illness. Indian J Psychol Med. 2019;41:428–33.
ALAVI N. The efficacy of PowerPoint-based CBT delivered through email: breaking the barriers to treatment for generalized anxiety disorder. J Psychiatr Pract. 2020;26:89–100.
Berry N, Lobban F, Bucci S. A qualitative exploration of service user views about using digital health interventions for self-management in severe mental health problems. BMC Psychiatry. 2019;19:35.
Hungerbuehler I, Valiengo L, Loch AA, Rössler W, Gattaz WF. Home-Based Psychiatric Outpatient Care through Videoconferencing for Depression: a Randomized Controlled Follow-Up trial. JMIR Ment Heal. 2016;3:e36.
LaFrance WC, Ho WLN, Bhatla A, Baird GL, Altalib HH, Godleski L. Treatment of psychogenic nonepileptic seizures (PNES) using video telehealth. Epilepsia. 2020;61:2572–82.
Kayrouz R, Karin E, Staples LG, Nielssen O, Dear BF, Titov N. A comparison of the characteristics and treatment outcomes of migrant and Australian-born users of a national digital mental health service. BMC Psychiatry. 2020;20:111.
Choi NG, Marti CN, Bruce ML, Hegel MT, Wilson NL, Kunik ME, Six-month postintervention depression, and disability outcomes of in-home telehealth problem-solving therapy for depressed, low-income homebound older adults. Depress Anxiety. 2014;31:653–61.
Dubad M, Elahi F, Marwaha S. The clinical impacts of Mobile Mood-Monitoring in Young People with Mental Health problems: the MeMO study. Front Psychiatry. 2021;12.
Birnbaum ML, Ernala SK, Rizvi AF, Arenare E, Van Meter R, De Choudhury A. Detecting relapse in youth with psychotic disorders utilizing patient-generated and patient-contributed digital data from Facebook. Npj Schizophr. 2019;5:17.
Ben-Zeev D, Brian R, Wang R, Wang W, Campbell AT, Aung MSH, et al. CrossCheck: integrating self-report, behavioral sensing, and smartphone use to identify digital indicators of psychotic relapse. Psychiatr Rehabil J. 2017;40:266–75.
Aardoom JJ, Dingemans AE, Spinhoven P, van Ginkel JR, de Rooij M, van Furth EF. Web-based fully automated self-help with different levels of therapist support for individuals with eating disorder symptoms: a Randomized Controlled Trial. J Med Internet Res. 2016;18:e159.
Mitchell JE, Crosby RD, Wonderlich SA, Crow S, Lancaster K, Simonich H, et al. A randomized trial comparing the efficacy of cognitive–behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav Res Ther. 2008;46:581–92.
Wagner B, Nagl M, Dölemeyer R, Klinitzke G, Steinig J, Hilbert A, et al. Randomized Controlled Trial of an internet-based cognitive-behavioral treatment program for binge-eating disorder. Behav Ther. 2016;47:500–14.
Sockalingam S, Leung SE, Ma C, Hawa R, Wnuk S, Dash S, et al. The impact of telephone-based cognitive behavioral therapy on Mental Health Distress and Disordered Eating among bariatric surgery patients during COVID-19: preliminary results from a Multisite Randomized Controlled Trial. Obes Surg. 2022;32:1884–94.
Graham AK, Kwasny MJ, Lattie EG, Greene CJ, Gupta NV, Reddy M, et al. Targeting subjective engagement in experimental therapeutics for digital mental health interventions. Internet Interv. 2021;25:100403.
Gellatly J, Chisnall L, Seccombe N, Ragan K, Lidbetter N, Cavanagh K. @Home eTherapy Service for people with common Mental health problems: an evaluation. Behav Cogn Psychother. 2018;46:115–20.
Bolier L, Haverman M, Kramer J, Westerhof GJ, Riper H, Walburg JA, et al. An internet-based intervention to promote Mental Fitness for mildly depressed adults: Randomized Controlled Trial. J Med Internet Res. 2013;15:e200.
Venkatesan A, Rahimi L, Kaur M, Mosunic C. Digital Cognitive Behavior Therapy intervention for depression and anxiety: Retrospective Study. JMIR Ment Heal. 2020;7:e21304.
Van Den Berg N, Grabe H-J, Baumeister SE, Freyberger HJ, Hoffmann W. A telephone-and text message-based telemedicine concept for patients with mental health disorders: results of a randomized controlled trial. Karger com. 2015. https://doi.org/10.1159/000369468.
Abel EA, Shimada SL, Wang K, Ramsey C, Skanderson M, Erdos J, et al. Dual use of a patient Portal and Clinical Video Telehealth by Veterans with Mental Health diagnoses: Retrospective, cross-sectional analysis. J Med Internet Res. 2018;20:e11350.
Venkatesan A, Forster B, Rao P, Miller M, Scahill M. Improvements in Depression outcomes following a Digital Cognitive Behavioral Therapy Intervention in a Polychronic Population: Retrospective Study. JMIR Form Res. 2022;6:e38005.
McGrath PJ, Lingley-Pottie P, Thurston C, MacLean C, Cunningham C, Waschbusch DA, et al. Telephone-based mental health interventions for child disruptive behavior or anxiety disorders: randomized trials and overall analysis. J Am Acad Child Adolesc Psychiatry. 2011;50:1162–72.
AL-Asadi AM, Klein B, Meyer D. Multiple comorbidities of 21 psychological disorders and relationships with Psychosocial variables: a study of the Online Assessment and Diagnostic System within a web-based Population. J Med Internet Res. 2015;17:e55.
Bidargaddi N, Bastiampillai T, Allison S, Jones GM, Furber G, Battersby M, et al. Telephone-based low intensity therapy after crisis presentations to the emergency department is associated with improved outcomes. J Telemed Telecare. 2015;21:385–91.
O’Callaghan E, Mahrer N, Belanger HG, Sullivan S, Lee C, Gupta CT, et al. Telehealth-supported decision-making Psychiatric Care for suicidal ideation: longitudinal observational study. JMIR Form Res. 2022;6:e37746.
Buckley D, Weisser S. Videoconferencing could reduce the number of mental health patients transferred from outlying facilities to a regional mental health unit. Aust N Z J Public Health. 2012;36:478–82.
Watson A, Mellotte H, Hardy A, Peters E, Keen N, Kane F. The digital divide: factors impacting on uptake of remote therapy in a South London psychological therapy service for people with psychosis. J Ment Heal. 2022;31:825–32.
Andersen JA, Rowland B, Gloster E, McElfish PA. Telehealth utilization during COVID-19 among people with diagnosed Mental Health conditions. Telemed e-Health. 2022;28:743–6.
Costa M, Reis G, Pavlo A, Bellamy C, Ponte K, Davidson L. Tele-Mental Health utilization among people with Mental illness to Access Care during the COVID-19 pandemic. Community Ment Health J. 2021;57:720–6.
Moitra E, Park HS, Gaudiano BA. Development and initial testing of an mHealth transitions of care intervention for adults with Schizophrenia-Spectrum disorders immediately following a Psychiatric hospitalization. Psychiatr Q. 2021;92:259–72.
Badesha K, Wilde S, Dawson DL. Mental health mobile application self-help for adolescents exhibiting psychological distress: a single case experimental design. Psychol Psychother Theory Res Pract. 2023;96:223–48.
Hulsbosch AM, Nugter MA, Tamis P, Kroon H. Videoconferencing in a mental health service in the Netherlands: a randomized controlled trial on patient satisfaction and clinical outcomes for outpatients with severe mental illness. J Telemed Telecare. 2017;23:513–20.
Feijt M, de Kort Y, Westerink J, Bierbooms J, Bongers I, IJsselsteijn W. Integrating technology in mental healthcare practice: a repeated cross-sectional survey study on professionals’ adoption of Digital Mental Health before and during COVID-19. Front Psychiatry. 2023;13.
Grossman MJ, Woolridge S, Lichtenstein S, McLaughlin D, Auther AM, Carrión RE, et al. Patterns and perceptions of face-to-face and digital communication in the clinical high risk and early stages of psychosis. Psychiatry Res. 2020;284:112667.
Gulf News. UAE Health - Dubai to unveil new mental health app that uses artificial intelligence. https://gulfnews.com/uae/health/dubai-to-unveil-new-mental-health-app-that-uses-artificial-intelligence-1.85704754. Accessed 8 Feb 2024.
Mental Health Online Platforms - AE. https://mentalhealth.ae/online-platforms/. Accessed 8 Feb 2024.
Telemedicine | The Official Portal of the UAE Government. https://u.ae/en/information-and-services/health-and-fitness/telemedicine. Accessed 8 Feb 2024.
Chang BL, Bakken S, Brown SS, Houston TK, Kreps GL, Kukafka R, et al. Bridging the Digital divide: reaching vulnerable populations. J Am Med Inf Assoc. 2004;11:448. https://doi.org/10.1197/JAMIA.M1535.
Health Policies and Standards Department- ealth Regulation Sector. Standards for Telehealth Services. Dubai; 2021. https://www.dha.gov.ae/uploads/012023/Standards for Telehealth Services2023158613.pdf.
Department of Health - Abu Dhabi. DOH Standard on Tele-medicine. Abu Dhabi. 2020. https://www.doh.gov.ae/-/media/0272CB2B824D41D6B4A2A5C78EBD94F9.ashx
Latha K, Meena KS, Pravitha MR, Dasgupta M, Chaturvedi SK. Effective use of social media platforms for promotion of mental health awareness. J Educ Health Promot. 2020;9. https://doi.org/10.4103/JEHP.JEHP_90_20.
Knapp AA, Cohen K, Nicholas J, Mohr DC, Carlo AD, Skerl JJ, et al. Integration of Digital Tools Into Community Mental Health Care Settings that serve Young people: Focus Group Study. JMIR Ment Heal. 2021;8. https://doi.org/10.2196/27379.
Acknowledgements
We acknowledge Basil Ibrahim for assistance in the database search, Nihal Khunaijir, Tarig Alshiekh, Tarteel Mohamed, Yusra Mohamed, Khadija Mansour, Abrar Elamin, Raghda Mohamed Ahmed, Atika Ellfaki, for their contribution to the current study.
Funding
This project was funded by Abu Dhabi University College of Health Sciences.
Author information
Authors and Affiliations
Contributions
RA conceptualized the study and consensus on methodology and registration was done by RA and YAME. Defining keywords for the search was done by BI, YAME, and RA. Database search was done by BI and YAME. The first tier of title and abstract screening was done by YAME, HS, RK, and RA second tier of title and abstract screening was done by DE, NSS, TM, and NK. Full-text screening and checking eligibility criteria were done by YAME, HS, NK, TM, AO, and KM. Data extraction was done by YAME, NSS, RK, AE and reassessed by RA, TM. Qualitative analysis was done by YAME. Data analysis and quality appraisal were done by YAME, TM, NK, TA and reviewed by RA. The introduction, methodology, discussion, and conclusion were drafted by YAME and RA. RA, RK, NSS, DE and YAME have reviewed the article and provided input. All co-authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Al Dweik, R., Ajaj, R., Kotb, R. et al. Opportunities and challenges in leveraging digital technology for mental health system strengthening: a systematic review to inform interventions in the United Arab Emirates. BMC Public Health 24, 2592 (2024). https://doi.org/10.1186/s12889-024-19980-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19980-y