Abstract
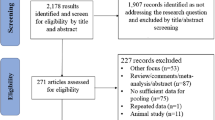
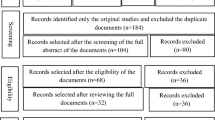
Many researchers have studied the role of air pollutants on cognitive function, changes in brain structure, and occurrence of dementia. Due to the wide range of studies and often contradictory results, the present systematic review was conducted to try and clarify the relationship between air pollutants and dementia. To identify studies for this review, a systematic search was conducted in Scopus, PubMed, and Web of Science databases (without historical restrictions) until May 22, 2023. The PECO statement was created to clarify the research question, and articles that did not meet the criteria of this statement were excluded. In this review, animal studies, laboratory studies, books, review articles, conference papers and letters to the editors were avoided. Also, studies focused on the effect of air pollutants on cellular and biochemical changes (without investigating dementia) were also excluded. A quality assessment was done according to the type of design of each article, using the checklist developed by the Joanna Briggs Institute (JBI). Finally, selected studies were reviewed and discussed in terms of Alzheimer's dementia and non-Alzheimer's dementia. We identified 14,924 articles through a systematic search in databases, and after comprehensive reviews, 53 articles were found to be eligible for inclusion in the current systematic review. The results showed that chronic exposure to higher levels of air pollutants was associated with adverse effects on cognitive abilities and the presence of dementia. Studies strongly supported the negative effects of PM2.5 and then NO2 on the brain and the development of neurodegenerative disorders in old age. Because the onset of brain structural changes due to dementia begins decades before the onset of disease symptoms, and that exposure to air pollution is considered a modifiable risk factor, taking preventive measures to reduce air pollution and introducing behavioral interventions to reduce people's exposure to pollutants is advisable.
Similar content being viewed by others
Introduction
Technological development and the rapid expansion of mechanization during the last few decades have led to an increase in life expectancy in various societies, especially in developed countries [1]. An increase in the life expectancy can lead to the growth of neurological disorders [2]. According to statistics published worldwide, neurological disorders, including Parkinson's (PD), cognitive dysfunction, Alzheimer's (AD) and dementia, are a leading cause of disability and death [3, 4]. Cognitive function also diminishes with age [5] and therefore, elderly people are disproportionately affected by cognitive disorders and, finally, dementia [6, 7] which imposes a significant burden on health care systems. According to statistics published by the World Health Organization (WHO), approximately 55 million people worldwide suffered from dementia in 2019, which is estimated to more than double in 2050 [8]. Dementia is the cause of 2.4 million deaths and 28.8 million disability-adjusted life years (DALYs) in 2016 and is known as the third cause of neurological DALYs [3, 9].
Various factors are involved in dementia, including anthropometric parameters (for example, body mass index), the APOE Ɛ4 allele [10], lack of weight [11], inactivity [12], non-Mediterranean diet [13], and the lack of specific micronutrients and macronutrients [14]. In addition, many epidemiological studies have shown that exposure to air pollution can also contribute to neuropathology through oxidative stress, hyperactivation of microglia, disruption of the blood–brain barrier (BBB) and neuroinflammation [15, 16] and cause adverse effects on the brain, accelerate cognitive aging and even increase the occurrence of AD and other forms of dementia [17,18,19]. The 2020 Lancet Commission on dementia prevention, intervention and care, considered air pollution as a new modifiable risk factor for dementia, accounting for about 2% of cases worldwide [20]. Studies conducted in the United Kingdom showed that an increase of 1 µg/m3 PM2.5 (particles with a diameter of 2.5 µm or less) increases the risk of dementia by 6% and the risk of AD by 10% [21]. Mortamais et al. (2021) found that an increase of 5µg/m3 in PM2.5 level, increases 20% the risk for all-cause dementia, 20% for AD and 33% for Vascular Dementia (VaD) in elderly people over 70 years [22]. However, the adverse effects of air pollution on cognitive function are not limited to old age. Recent epidemiological studies support the hypothesis that public exposure to air pollutants can cause structural and functional changes in children's brains [23, 24] and by causing negative effects on neuropsychological development, make them susceptible to neurological disorders in middle and old age [25, 26].
Therefore, prevention of exposure to air pollution is a potentially correctable risk factor in the occurrence of cognitive decline and dementia in the elderly. The present systematic review was conducted to critically examine the published scientific literature related to the impact of exposure to air pollution on dementia. Specifically, the objectives were: (1) to evaluate the type and concentration of air pollutants including PM10 (particles with a diameter of 10 µm or less), PM2.5, NO2, O3, black carbon (BC), polycyclic aromatic hydrocarbons (PAHs), benzene, toluene, ethylbenzene and xylenes (BTEX), formaldehyde (FA) in geographic areas and (2) to assess the risk of dementia in adults with chronic respiratory exposure to the mentioned pollutants.
Methods
Protocol
This systematic review was guided by the PRISMA statement (Preferred Reporting Items for Systematic Review and Meta-analyses) and fully complied with the protocol registered in the International Prospective Register of Systematic Reviews (PROSPERO, CRD42023413916).
PECO statement
In this study, the PECO (population, exposure, comparator, and outcome) [27] statement was used to develop the research question, search terms, and inclusion and exclusion criteria of the systematic review. Table 1 shows the PECO statement for understanding the adverse effects of respiratory exposure to pollutants PM10, PM2.5, NO2, O3, BC, PAHs, BTEX, and FA on dementia.
Search strategy and selection of studies
According to our knowledge, this is the first systematic review that investigated the effect of respiratory exposure to pollutants i.e. PM10, PM2.5, NO2, O3, BC, PAHs, BTEX, and FA on dementia. To obtain all published studies in this field, a systematic search was conducted in Scopus, PubMed, and Web of Science databases, without a date limit until May 22, 2023. The keywords used in this study include the following (the details of the search strategy used for the systematic search in the databases are shown in Appendix A1):
-
Exposure to pollutants: “air pollution”, “PM10”, “PM2.5”, “nitrogen dioxide”, “ozone”, “black carbon”, “diesel”, “diesel exhaust”, “PAH*”, “BTEX”, “toluene”, “ethylbenzene”, “xylene”, “benzene”, “formaldehyde”, “formal”, “formalin”, “methanol”, “methylene oxide”
-
Outcomes of exposure: “Alzheimer's disease”, “Neuromarker”, “Neuroinflammation”, “Dementia”, “Vascular dementia”, “Frontotemporal dementia”, “Frontotemporal lobar degeneration”, “Lewy body disease”, “Lewy body dementia”
The mentioned keywords were extracted by (M.M and A.H.Kh) and systematically searched by (A.H.Kh) in Title/Abstract and Mesh (if any). After merging the studies in EndNote X20 software, all duplicates were removed and the data were independently screened and extracted by two researchers (M.M and A.H.Kh). More contradictions and ambiguities were resolved with the intervention of the third author (J.G). In addition, to obtain additional studies that meet the inclusion criteria, additional to the hand searching, the reference list of selected studies was also systematically searched in parallel.
Criteria of entering and extracting studies
In this review, we excluded studies focused on the effects of exposure to air pollutants on neurological and biochemical changes (without examining dementia) and studies that investigated exposure to air pollutants as a dependent variable. Animal studies, laboratory studies, books, review articles, conference papers, and letters to the editors were also excluded. In this systematic review, only original peer-reviewed articles in English were reviewed.
Finally, the following information was extracted from the selected articles:
Authors, the year of publication, study design, country, the number of sample people, the age range of people, gender, the type of pollutant, the mean concentration of pollutant, diagnosis tool, and the type of dementia.
Quality control
The quality of the selected studies was checked by two researchers (M.M and A.H.Kh) using the Joanna Briggs Institute (JBI) checklist for cohort studies, case–control studies and analytical cross-sectional studies, independently. This checklist evaluates the risk of bias in studies by asking 2 questions from each of the sample areas including selection criteria, exposure assessment, confounding factors and results and appropriate statistical analysis. The defined answers for each question can be one of the options (yes, no, unclear, or not applicable). According to the total selection percentage of each of the 4 mentioned answers, the quality of articles is determined in the following 3 levels:
-
High-quality level and low risk of bias (Q1) (Yes ≥ 50–75%).
-
Moderate quality level and unclear risk of bias (Q2) (unclear ≥ 50–75%).
-
Low-quality and high risk of bias (Q3) (No ≥ 50–75%) [28].
All the articles that were of adequate quality were included in the study.
Result synthesis
Due to heterogeneity in study design, exposure (occupational/environmental) and the age of subjects, quantitative synthesis of studies in the form of meta-analysis was not possible. Therefore, the results obtained from the selected studies, which included the type of dementia, the age of the subjects, gender, the type of air pollutants, mean concentration, the instrument for detecting pollutants, and the diagnosis of dementia, and the outcome of exposure (Appendix A2), were narratively combined. This synthesis was done in two steps. The first stage included the initial synthesis using the general grouping of studies based on Alzheimer's and non-Alzheimer's dementia; therefore, the results of articles were carefully studied, and considered which of the types of Alzheimer's dementia (AD) (Appendix A2) and non-Alzheimer's dementia (VaD, FTD and PD) (Appendix A3) have been investigated. In the second step, the relationship between the type and concentration of each pollutant in dementia was investigated.
Figure 1 shows the process of conducting the present systematic review by the members of the research team, which includes six general steps:
Topic selection, systematic search, screening and data extraction, quality control, resolving contradictions and ambiguities, and synthesis of results.
Results and Discussion
Selection process and characteristics of articles
In this review, 14,924 articles were obtained through a systematic search in databases, of which 4532 studies were retrieved from PubMed, 5878 from Scopus, and 4514 from Web of Science. After entering the articles into EndNote X20 software, 6546 duplicates were removed and 8378 studies were screened for title and abstract. At this stage, 8289 articles were excluded and the entry and exit criteria and quality assessment were done for 88 full texts. Finally, after conducting additional reviews, 36 studies were excluded for the following reasons:
Nine studies were review articles, two studies only investigated brain volume, in twelve articles the type of air pollutant was not specified, five studies investigated the effect of other pollutants on dementia, five studies were excluded due to the high risk of bias and access to three full texts was not possible.
In addition, hand searching and systematic search of the selected articles' reference lists were also conducted to identify additional studies eligible for inclusion, which led to the identification of two studies through reference checking. Therefore, the total number of studies included in this systematic review increased to 53 articles (Fig. 2).
The studies in this systematic review included 6 case–control [29,30,31,32,33,34], 7 cross-sectional [19, 35,36,37,38,39,40], and 40 cohort studies [1, 2, 18, 21, 22, 41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75]. Specifically, selected studies have been conducted in 17 countries around the world:
19 in the United States of America, 7 in Sweden, 7 in Taiwan, 4 in Canada, 3 in France, 2 in Australia, 2 in Germany, 2 in Hong Kong, 2 in Mexico, 2 in the United Kingdom, 1 in each country of Netherlands, Spain, China, Denmark, England, Italy, and the Republic of Korea.
In total, 173,698,774 subjects were contained in the studies examined in this systematic review. The characteristics of the reviewed studies are shown in Table 2.
Diagnostic methods in the types of dementia
When we examined the 53 selected studies, 39 diagnostic tools and methods for AD and other types of dementia had been used (Appendix A2 and A3); of these, 21 diagnostic tools were used for Alzheimer's dementia and 28 methods for non-Alzheimer's dementia. According to the investigations carried out in studies related to Alzheimer's dementia, the methods of medical records (N = 11) and Mini-Mental Status Examination (MMSE) (N = 8) were the most prevalent. Five studies also used medical imaging (such as MRI and CT scan) to investigate the changes made in brain structures, which indicate the onset of Alzheimer's disease. In addition, the most common diagnostic tools for non-Alzheimer's dementia were included medical reports (N = 4), MMSE (N = 10), Medical imaging (N = 4), Clinical Dementia Rating Sum of Box (CDR-SB) (N = 4), and the Montreal Cognitive Assessment (MoCA) (N = 3).
MMSE and MoCA are among the most important reliable screening tools that are widely used for clinical and research purposes [76, 77]. These tools have received a lot of attention due to the need for little training, ease of implementation, and the ability to differentiate dementia patients from healthy people [78,79,80]. MMSE is also widely used to describe a wide range of cognitive functions, including attention, memory, verbal ability, and visual-spatial cognitive function [81], and its total score is related to disease progression [82]. However, it has been found that the MMSE may be less reliable than the MoCA in the diagnosis of mild cognitive impairment (MCI) because this instrument had lower sensitivity among multiple study settings [83,84,85,86,87]. In addition, the MoCA can show differences in the cognitive profile of people diagnosed with MMSE in the normal range, which makes the MoCA a powerful, concise, and useful tool [77, 88, 89].
Although the use of questionnaire methods is a standard requirement for dementia researchers, the importance of medical imaging methods in diagnosing dementia types with high certainty should not be neglected to investigate the changes made in the brain structure and the speed of disease progression. Among the most important diagnostic imaging tools for dementia are PET imaging with 2-deoxy-positron emission tomography (PiB-PET), 2 [18F] fluoro-D-glucose tracer (FDG-PET) and Structural and Functional Magnetic Resonance Imaging (MRI) [90]. The first PET technique used to diagnose neurodegenerative disorders was 18F-fluorodeoxyglucose (18F-FDG) metabolic imaging, which is a measure of neuronal or synaptic integrity [91, 92]. More recent advances using PET includes the detection of specific neural ligands, such as specific ligands for fibrillar Aβ [93], paired-helical filament tau [94, 95], and synaptic vesicle protein 2A [96]. The PET technique, however, is only available in specialized centers due to its high cost.
In our systematic review, the main neuroimaging technique used was MRI. This tool can measure brain atrophy, especially in the mesial-temporal structures, and detect it even before appearing the first clinical symptoms [97, 98]. This method is included in both the diagnostic criteria presented by Dubois [99] and NIA-AA [100] and has been used as a reliable diagnostic tool by many researchers [101,102,103]. The sensitivity of this method as an AD marker has been reported to be more than 85% [97], which is more than PiB-PET (70%) [104] and FDG-PET (80%) [105, 106].
Atrophy in the medial temporal lobe, especially the hippocampus, and a decrease in the thickness of the cerebral cortex in vulnerable areas of AD are among the first signs detectable by MRI in the early stages of the disease [107,108,109]. This tool can show hippocampal volume reduction 2 to 3 years before the onset of dementia in asymptomatic carriers of APP mutations [110] and in elderly people up to 6 years before that [103, 107]. In addition, entorhinal cortex volume reduction, which progresses up to four years before cognitive decline, can be detected by MRI up to 90% [107].
Alzheimer’s dementia
The characteristics and results extracted from the articles related to Alzheimer's dementia are shown in Appendix A2. Thirty-one studies investigated the effect of pollutants i.e. PM10, PM2.5, NO2, O3, BC, PAHs, BTEX, and FA on the occurrence of Alzheimer's dementia. These studies were published from 1995–2023, and most were since 2018, indicating the novelty of the subject under discussion. More than 80% of the studies investigated the incidence of Alzheimer's in people over 60 years old, but some studies included younger people, comprising Haisu Zhang (2023) [40], Lilian Calderón-Garcidueñas (2022) [38, 39], Marta Crous-Bou (2020) [1], Anna Oudin (2019 and 2016) [44, 53], and Ruo-Ling Li (2019) [51].
The results showed that chronic exposure to air pollutants, especially particulate matter (PMs), increases the number of hospitalizations due to the exacerbation of neurocognitive disorders caused by Alzheimer's dementia or related diseases. This finding is compatible with previous studies on the role of exposure to air pollutants on the development of this neurological disorder [18, 74, 75]. Results from human and animal studies have shown that air pollution is associated with atherosclerosis, increased blood inflammatory biomarkers, and oxidative stress, which may accelerate hospitalization for several neurological diseases [111, 112]. In the United Kingdom, the results of a population-based cohort study showed that the risk of AD was associated with exposure to PM2.5 (adjusted hazard ratio—HR 1.10, 95% CI 1.02–1.18) and NO2 (1.23, 1.07–1.43) increases significantly so that an increase of 1 µg/m3 PM2.5 is associated with a 10% increase in the risk of AD. Exposure to O3 reduced this risk [21]. Also Cerza et al. (2019) in a cohort study in Italy concluded that a positive association between exposure to O3 and NOx and dementia hospitalizations, (O3: HR = 1.06; 95% CI: 1.04–1.09 per 10 μg/m3; NOx: HR = 1.01; 95% CI: 1.00–1.02 per 20 μg/m3) [52]. This study showed that exposure to NOx, NO2, PM2.5, and PM10, except for O3, has a significant negative relationship with AD [52].
He et al. (2022) also demonstrated in a population-based cohort study in China that exposure to PM2.5, PM10, and CO pollutants was significantly associated with an increased risk of AD, but there is no significant relationship between exposure to NO and SO2 with the occurrence of this disorder. This study also showed an inverse relationship between O3 exposure and AD [69]. Meanwhile, Jung et al. (2015) concluded that for an increase of 9.63 ppb in O3 concentration, the risk of AD increases 1.06 times in the elderly ≥ 65 years (adjusted HR 1.06, 1.00–1.12) [43]. The difference between the results of these studies can be caused by different characteristics in the study population, study design, sample size, setting, and different measurements of exposure to air pollutants.
In addition, the researchers found evidence of the adverse effect of exposure to air pollutants on episodic memory. Several animal studies showed that exposure to inhaled PM2.5 can impair neural systems that underlie episodic memory processes [113,114,115]. So far, limited longitudinal epidemiological studies have been conducted about PM2.5 and episodic memory in humans [116,117,118]. The results of a prospective study on 998 elderly women aged 73 to 87 years old in the US showed that chronic exposure to PM2.5 in residential environments was associated with a rapid decline in episodic memory, especially in measures of immediate recall and learning of new material [68]. A decrease in verbal episodic memory (such as the ability to remember details, with context, from daily and distant experiences) is prominent in AD and can be detected in the preclinical stage [119, 120]. For example, impaired episodic memory is one of the main criteria for the classic diagnosis of AD by Dubois et al. (2007), which appears early in the course of the disease [99]. Studies have proven that the rapid decline of this memory is somewhat associated with an increase in the Alzheimer's disease pattern similarity (AD-PS) score [68]. AD-PS is a brain MRI-based structural biomarker that reflects high-dimensional gray matter atrophies in brain regions vulnerable to AD neuropathology [68]. In addition to exposure to environmental factors, natural aging can also lead to a decrease in episodic memory, which is related to the decrease in the volume of the hippocampus and other structures of the medial temporal lobe [121]. The medial temporal lobe and its structural components, especially the hippocampus, play an important role in encoding (learning, recalling) and retrieving (recalling) the details of events that make up episodic memories [121].
Zhao et al. (2019) showed in a human imaging study that atrophy in hippocampal subfields can impose a wide range of effects on measures of episodic memory (immediate recalls, delayed-recalls, and recognition) [122]. Although so far the relative roles of hippocampal subfields (e.g. cornu ammonis (CA, CA2-3), CA4-denate gyrus, presubiculum, subiculum) have not been determined in the processes related to encoding and retrieval, animal studies have proven the adverse effects of PMs on the morphology and functional changes in hippocampal subfields. Also, we can mention the decrease in apical dendritic spine density and dendritic branches in the CA1 and CA3 regions [123], decrease in synaptic function in CA1 neurons [114, 124], decrease in basic protein in white matter, and increase in atrophy of neurites in the CA1 region [125]. Based on the studies, encoding is done by CA2, CA3, and dentate gyrus, while CA1 and subiculum are involved in retrieval [126]. According to the results obtained by Younan et al. (2020), it seems that the significant reduction of episodic memory processes (immediate recall/new learning) caused by exposure to PM2.5 is more due to the adverse effects of this pollutant on hippocampal subfields associated with encoding, such as CA2, CA3, and dentate gyrus [68]. These neurotoxicological results indicate that some hippocampal subfields may be more sensitive to the adverse effects of particulate matter than other subfields.
So far, many studies have proven the existence of an inverse relationship between exposure to air pollutants and white matter volume, gray matter volume, and cerebral cortex thickness in brain areas affected by AD [127,128,129,130]. Wilker et al. (2015) showed in a study that with increasing PM2.5 concentration, brain volume decreases by 0.32% [131], which was consistent with the results obtained by Chen et al. (2015) regarding the reduction of white matter volume and the volume of the whole brain due to exposure to high concentrations of this pollutant [128]. The results of the study by Crous-Bou et al. (2020) showed that chronic exposure to air pollutants, especially NO2 and PM10, is associated with a decrease in the thickness of the cerebral cortex in brain areas affected by AD [1], which is consistent with the results of study done by Casanova et al. (2016) [127]. In a voxel-based morphometry study, they examined the local brain structure related to PMs in elderly women and concluded that exposure to PM2.5 has an inverse relationship with the reduction of the frontal cortex [127]. Furthermore, Cho et al. (2023) showed that a 10 µg/m3 increase in (β = -1.13; 95% CI, − 1.73 to − 0.53) PM10 and a 10 ppb increase in (β = -1.09; 95% CI, − 1.40 to − 0.78) NO2 are significantly associated with decreasing MoCA score. Also, these two pollutants were significantly associated with an increase in AD-like cortical atrophy scores and a decrease in the thickness of the cerebral cortex [129].
PET ligand studies indicate that gray matter atrophy of the brain can be caused by tau neuropathological processes, which can lead to cognitive decline in patients [132,133,134]. Several plausible biological mechanisms explain the rapid development or onset of neurological diseases caused by exposure to air pollution. After inhalation, air pollutants can pass through the BBB and enter the brain through the olfactory bulb or systemic circulation [135] causing oxidative stress and systemic inflammatory responses, disruption of the blood–brain barrier, deposition of peptides beta-amyloid (Aβ) and activation of microglia and as a result may exacerbate the disease progression of AD [136, 137]. In addition, it has been reported that NO2 is associated with inflammatory responses and markers such as increased serum concentration of systemic interleukin IL-6 [138]. Recent studies have shown that exposure to air pollutants can be effective in causing neurological and cognitive disorders by contributing to AD pathologies such as brain Aβ and tau burden [139, 140]. Researchers use the levels of Aβ, total tau (t-tau) and phospho-tau (p-tau) in CSF as specific biomarkers for the clinical diagnosis of probable AD [99]. Some studies have proven that CSF Aβ, as the first marker of AD, shows abnormal levels several years before the appearance of impaired memory [141, 142]. Diagnosis of early AD in patients with mild cognitive impairment (MCI) can be done by detecting low levels of Aβ and high levels of p-tau and t-tau in CSF [143].
Reports show that living in areas with high air pollution can lead to the accumulation of Aβ in neurons and astrocytes [144]. Also, the results obtained from the study of Fu et al. (2022) indicate that the increase in the concentration of each unit of ln-transformed Ʃ-OH PAHs in the urine of coke oven workers was associated with an increase of 9.416 units of P-Tau231 in plasma and a decrease of 0.281 in visuospatial/executive function [145]. Tau is a microtubule-associated protein that contributes to the stability of axonal microtubules in the brain [146]. The presence of hyperphosphorylated tau leads to the formation of neurofibrillary tangles, which is considered a pathological characteristic of AD [147]. Some researchers have reported changes in the concentration of phosphorylated tau as a possible sign of the progression of some neurological diseases [148, 149]. This is consistent with the results of Nie et al.'s (2013) study, which showed that benzo[a]pyrene (B[a]P) leads to tau 231 hyperphosphorylation [150].
Non-Alzheimer’s dementia
Among the 53 selected articles, 41 studies investigated the effect of air pollutants on the incidence of non-Alzheimer's dementia (Appendix A3), which were published during the years 2014–2023. Except for the studies of Anna Oudin (2016) [44], Anna Oudin (2018) [49], Iain M Carey (2018) [21], Anna Oudin (2019) [53], Han-Wei Zhang (2019) [54], Zorana J. Andersen (2022) [67], Lilian Calderón-Garcidueñas (2022) [38, 39], and Haisu Zhang (2023) [40], the rest of the articles included people over the age of 60 years old.
Non-Alzheimer's dementia accounts for almost half of dementia cases [151]. The most common non-Alzheimer's neurological disorders include vascular dementia (VaD) [152, 153], Parkinson's disease (PD) [154], Fronto-Temporal Dementia (FTD) [155] and Dementia with Lewy Bodies (DLB) [92], which are characterized by the accumulation of natural proteins in the CNS, as proteinopathies [156].
Vascular Dementia
The present study showed that exposure to air pollutants may have a direct effect on the incidence and progression of VaD. In a longitudinal study, Oudin et al. (2016) concluded that the probability of VaD diagnosis, with HR = 1.43, was higher among citizens with the highest exposure to traffic-related air pollution than those with low exposure [44]. These results were consistent with the study conducted by Cerza et al. (2019) [52]. In a longitudinal study on elderly men and women in Italy, they reported that chronic exposure to NOx, NO2, PM10 and PM2.5 has a positive relationship with VaD. In addition, a direct relationship between exposure to O3 and NOx with dementia hospitalization was also observed (O3: HR = 1.06 per 10 μg/m3; NOx: HR = 1.01; per 20 μg/m3) [52].
According to the studies, chronic exposure to air pollutants can cause vascular damage caused by large vessel atherosclerosis and small vessel arteriosclerosis and cause cortical and subcortical infarcts, sub-infarct ischemic lesions, and large and small cerebral hemorrhages [153, 157]. Researchers identify these factors as responsible for the initiation of VaD [153]. Moreover, dysfunction and degeneration of the neurovascular unit, which consists of a network of pericytes, myocytes, astrocytes, neurons, oligodendrocytes, endothelial cells and cerebral microvessels, aggravate the pathogenesis of VaD by disrupting the BBB [158]; which require hospital care to treat and prevent further side effects.
Also, the results obtained from a case–control study in Taiwan indicate that exposure to high levels of NO2 significantly increases the risk of developing VaD [31]. According to the studies, some researchers showed that for an increase of 5 μg/m3 NO2, the risk of VaD increases by 1.62 [74]. However, some studies have reached contradictory results. A cohort study conducted in England estimated the prevalence of VaD among men and women aged 50–79 years old at 29%, but found little evidence of the effect of air pollution on this neurological disorder [21]. Differences in results could be due to differences in instruments used, study design, and sample population characteristics.
VaD is a pathological condition in the elderly characterized by progressive cognitive dysfunction and is the second most common form of dementia, after AD [159]. This disorder is manifested by the loss of rationality, judgment skills, and especially cognitive functions and memory, and patients usually survive only 5–7 years after its onset [160]. Multifactorial etiopathology, diverse clinical manifestations, and numerous clinical subgroups are among the characteristics of VaD [152]. Chronic reduction in cerebral blood flow is one of the main characteristics of this neurological disorder [161], which results in the departure of brain blood vessels from regulation. This causes functional damage to capillaries, arteries and venules and damage to myelinated axons, and by creating a lesion in the white matter, it starts the pathophysiological process of VaD [162]. Small vessel disease (leukoaraiosis and lacunar infarcts), microinfarcts, microhemorrhages, cerebral amyloid angiopathy, and mixed vascular lesions are among the most important debilitating lesions of VaD [163, 164]. In addition, chronic cerebral hypoperfusion (CCH) has been reported as the main cause of this type of dementia [163, 165]. The results obtained from the studies indicate that CCH is associated with both neurodegeneration and dementia [166, 167]. Studies have shown that exposure to PMs can increase CCH-induced white matter neurotoxicity by enhancing pathophysiology [168, 169]. In a recent epidemiological study, Chen et al. (2015) showed that exposure to PM2.5 was associated with a decrease in regional white matter volume in the corpus callosum and frontal/temporal lobes of elderly women [128], which is consistent with the results of the study by Erickson et al. (2020) was matched [170]. In addition, experimental data obtained from animal studies showed that exposure to air pollutants, especially PMs, causes changes in myelin in the CA1 area of the hippocampus in rodents [171], which can increase the risk of developing neurological disorders and types of dementia.
Dementia due to Parkinson’s disease
The results of the studies retrieved in this systematic review showed that dementia due to PD, a dementia that begins 1 year or more after well-established Parkinson's disease [92], can be considered as one of the adverse effects of exposure to air pollutants, especially PMs. Shi et al. (2020) in a national cohort study in the USA showed that for an annual increase of 5 μg/m3 PM2.5, the probability of the first hospital admission due to PD and other related dementias will increase by 1.13 times for the American Medicare population (HR = 1.13) [75]. In this regard, Yuchi et al. (2020) also obtained similar results [32]. In a population-based cohort study in Canada, they proved that exposure to air pollutants increases the risk of PD (HR for PMs = 1.09, HR for BC = 1.03, HR for NO2 = 1.12), but no relationship was observed on the occurrence of AD [32]. These results were consistent with those obtained from the studies of Rhew et al. (2021) [33], Yitshak-Sade et al. (2021) [61] and Calderón-Garcidueñas et al. [39].
The studies have demonstrated that over 80% of individuals with Parkinson's disease develop dementia [172]. Generally, the point prevalence of dementia in patients with Parkinson's has been determined to be approximately 25%, which has a higher prevalence in men than in women [173]. Researchers have proven that the risk of dementia increased as the duration of the disease increased, so that this probability reached 50% 10 years after the diagnosis of Parkinson's [91]. Research indicates that dementia occurs in patients who survive for more than 10 years [93].
PD, containing Lewy bodies and Lewy neurites, is one of the common brain disorders associated with aging and is characterized by the accumulation of α-synuclein in intracellular inclusions [154]. The main pathological characteristic of PD is the progressive loss of nigrostriatal dopaminergic neurons in the substantia nigra pars compacta, which causes Parkinsonism in PD patients [174]. Parkinsonism is a clinical syndrome characterized by rest tremor, rigidity, bradykinesia and gait dysfunction with postural instability [174]. Neurological disorders such as progressive supranuclear palsy (PSP), corticobasal syndrome (CBS), or FTD may overlap in their symptoms with PD [156]. Reports show that a significant number of people with PD suffer from cognitive impairment and PD dementia during their disease [172, 175]. In some cases, co-existing pathology of TDP-43 can also be detected in PD patients [176]. TDP-43 is a protein biomarker whose accumulation can diagnose and classify neurological disorders [177]. The available evidence indicates that exposure to air pollutants plays a role in the accumulation of this protein [178]. Neuropathological examination of 44 children (average age 12.89 ± 4.9 years old) and 159 young adults (average age 29.2 ± 6.8 years old) living in Mexico City showed that exposure to PM2.5 and O3 pollutants can cause AD and PD in 23% of people. Furthermore, it causes TDP-43 pathology in 18.7% of cases [179, 180], which is in line with the results of the present systematic review.
Fronto-Temporal Dementia
FTD is a group of neurodegenerative disorders and although clinically and pathologically heterogeneous, they mainly affect the frontal and/or temporal lobes of the brain [156, 181]. This type of dementia is usually characterized by predominant frontal or temporal atrophy, and atrophy in the fronto-polar region is considered a special symptom of FTD [182]. The main clinical manifestations of FTD include two types of behavioral variant (bvFTD) and primary progressive aphasia (PPA). BvFTD mainly leads to personality changes and behavioral problems; While PPA causes gradual deterioration in speech/language and has a lower prevalence than bvFTD [183]. Primary Parkinsonism is observed in more than 20% of patients with FTD, mostly in bvFTD patients, and then non-fluent variant primary progressive aphasia occurs [184]. Each of the mentioned stages can have an effective role in reducing people's lives and increasing the economic burden for health systems by creating FTD.
In the current review, only two studies investigated FTD. Parra et al. (2022) concluded in a national cohort in the UK that there was a strong association between exposure to PM2.5, NO2, and NOx with the incidence of AD and VaD but not with FTD [73]. Meanwhile, Calderón-Garcidueñas et al. (2022) obtained completely contradictory results in the study of neurological disorders caused by exposure to PM2.5 in young adults living in the metropolis of Mexico City [39]. They showed that chronic exposure to PM2.5 higher than the values recommended by US-EPA causes a significant reduction of gray matter in higher-order cortical areas, which is usually associated with AD, PD and FTD in educated Mexicans [39]. The discrepancy in the results of these two studies can be explained by the difference in the number of cases, the age range of the cases, and the country under study.
Strengths and limitations of the study
Although several review studies related to exposure to air pollutants and the incidence of dementia have been published in recent years [135, 185,186,187], the present systematic review has several notable strengths that distinguish our study from other review studies. First, this study is the most up-to-date systematic review published related to the role of chronic exposure to air pollutants on dementia (Alzheimer's/Non-Alzheimer's).
Second, unlike other studies, we did not impose any restrictions on publication time [135], study design [185,186,187], and geographic scope [185] in the systematic search, which allowed us to find more studies and more comprehensive results. In addition, we tried to perform a systematic search in the largest and the most reliable databases to ensure the inclusion of all eligible studies. This resulted in the extraction of 53 related studies that met the inclusion criteria for the present review. However, our investigations showed that none of the recent review articles discussed the current number of studies [135, 185,186,187].
Third, due to the inclusion of an acceptable number of articles in the present systematic review, the results obtained from examining a substantial population of subjects, 173,698,774 people, were presented, which indicates the comprehensiveness and generalizability of the results of the present study.
Fourth, our study included types of dementia, such as Alzheimer's and non-Alzheimer's, and related dementias. This will help researchers to understand the impact of air pollution on each type of dementia and the action mechanism of pollutants in creating structural changes in the brain.
Fifth, in this study, in addition to criterion pollutants, other common and dangerous air pollutants, including FA, BTEX, and PAHs, were also investigated; these pollutants were not investigated in any of the published reviews.
However, the lack of access to the full texts of some studies and the examination of a limited number of pollutants were among the inevitable limitations of this systematic review.
Gaps and Recommendations
An in-depth review of published studies indicates the existence of some gaps in this important health field, including the lack of sufficient studies related to the role of air pollutants on FTD. As mentioned earlier, we could find only two studies related to the effect of exposure to PM2.5, PM10, NO2, and NOx on FTD [39, 73], which makes it impossible to compare the results with each other. Therefore, it is recommended that more researchers investigate the impact of exposure to different pollutants in diverse populations on FTD, to cover this important gap.
Moreover, the presence of various confounding factors can also be effective in achieving contradictory results in studies. Researchers believe that factors such as aging, early retirement, smoking, body mass index (BMI), alcohol consumption, and physical inactivity are among the confounding factors that can accelerate the process of dementia [66]. Also, studies have proven that co-morbidities, such as cardiovascular diseases, cerebrovascular disease, diabetes and mental health, environmental tobacco smoke (ETS), chronic exposure to noise, insufficient sleep, and unhealthy diet can also play an effective role in occurring or developing dementia at an older age [188]. Research has identified several potential socioeconomic factors that can influence the relationship between air pollution exposure and neurological outcomes at the individual and regional levels. Based on this, living in deprived neighborhoods and on the outskirts of cities increases the possibility of exposure to high levels of air pollution [189]. Studies have also shown that lower levels of education, and poor access to socioeconomic benefits, such as health care, are associated with an increased risk of dementia in the future [190, 191]. Therefore, it is necessary to consider strategies to control the impact of confounding factors to achieve more accurate results.
Also, due to the limited number of studies related to occupational exposure to pollutants in dementia, it is recommended to conduct more research to investigate occupational exposure in workers of different occupations and compare and analyze their results.
Since it has been proven that prenatal exposure is effective in the occurrence of some diseases in the future; therefore, it is recommended that cohort studies be designed and implemented to investigate the role of prenatal exposure to air pollutants and dementia at older ages.
Conclusion
The results of this systematic review showed that chronic exposure to air pollutants, especially PM2.5 and NO2, could have a potential role in the development and progression of AD and non-Alzheimer's dementia in old age. The review of selected studies indicates that the relationship between exposure to PM2.5 and then NO2 and O3 and suffering from dementia has been the focus of researchers in the last 5 years. No study was found that investigated the effect of FA on dementia and met the inclusion criteria for this study. In addition, BTEX and PAHs have been neglected by researchers, which is surprising due to the widespread presence of these pollutants in the environment and industries. Therefore, conducting more studies on the impact of other air pollutants, including FA, BTEX and PAHs, on the incidence of dementia and cognitive disorders is highly recommended. We believe that the identification and prevention of modifiable risk factors, such as exposure to toxic air in conjunction with behavioral interventions, can help prevent or delay the progression of neurodegenerative disorders and significantly reduce the burden of those disorders on society.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Code availability
Not applicable.
Abbreviations
- AD:
-
Alzheimer's dementia
- BBB:
-
Blood-brain barrier
- BC:
-
Black carbon
- BTEX:
-
Benzene, Toluene, Ethylbenzene, and Xylenes
- CCH:
-
Chronic cerebral hypoperfusion
- DLB:
-
Dementia with Lewy Bodies
- DALYs:
-
Disability-adjusted life years
- FA:
-
Formaldehyde
- FTD:
-
Fronto-Temporal Dementia
- PD :
-
Parkinson Disease
- PM:
-
Particulate Matter
- PM10 :
-
Particles with a diameter of 10 µm or less
- PM2.5 :
-
Particles with a diameter of 2.5 µm or less
- PAH:
-
Polycyclic Aromatic Hydrocarbons
- MoCA:
-
The Montreal Cognitive Assessment
- VaD:
-
Vascular Dementia
- WHO:
-
World Health Organization
References
Crous-Bou M, Gascon M, Gispert JD, Cirach M, Sánchez-Benavides G, Falcon C, et al. Impact of urban environmental exposures on cognitive performance and brain structure of healthy individuals at risk for Alzheimer’s dementia. Environ Int. 2020;138:105546.
Shi L, Wu X, Danesh Yazdi M, Braun D, Abu Awad Y, Wei Y, et al. Long-term effects of PM2·5 on neurological disorders in the American Medicare population: a longitudinal cohort study. Lancet Planet Health. 2020;4(12):e557–65.
Feigin VL, Nichols E, Alam T, Bannick MS, Beghi E, Blake N, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):459–80.
Maragakis NJ, Rothstein JD. Mechanisms of Disease: astrocytes in neurodegenerative disease. Nat Clin Pract Neurol. 2006;2(12):679–89.
Lipnicki DM, Crawford JD, Dutta R, Thalamuthu A, Kochan NA, Andrews G, et al. Age-related cognitive decline and associations with sex, education and apolipoprotein E genotype across ethnocultural groups and geographic regions: a collaborative cohort study. PLoS Med. 2017;14(3):e1002261.
Gao Q, Zang E, Bi J, Dubrow R, Lowe SR, Chen H, et al. Long-term ozone exposure and cognitive impairment among Chinese older adults: A cohort study. Environ Int. 2022;160:107072.
Jia L, Quan M, Fu Y, Zhao T, Li Y, Wei C, et al. Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurol. 2020;19(1):81–92.
WHO. Global status report on the public health response to dementia 2021 [Available from: https://www.who.int/publications/i/item/9789240033245.
Nichols E, Szoeke CE, Vollset SE, Abbasi N, Abd-Allah F, Abdela J, et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(1):88–106.
Gachupin F, Romero MD, Ortega WJ, Jojola R, Hendrie H, Torres EP, et al. Cognition, Depressive Symptoms and Vascular Factors among Southwest Tribal Elders. Ethn Dis. 2016;26(2):235–44.
Park KM, Sung JM, Kim WJ, An SK, Namkoong K, Lee E, et al. Population-based dementia prediction model using Korean public health examination data: A cohort study. PLoS ONE. 2019;14(2):e0211957.
Ran J, Zhang Y, Han L, Sun S, Zhao S, Shen C, et al. The joint association of physical activity and fine particulate matter exposure with incident dementia in elderly Hong Kong residents. Environ Int. 2021;156.
Aridi Y S, Walker J L, Wright ORL. The Association between the Mediterranean Dietary Pattern and Cognitive Health: A Systematic Review. Nutrients [Internet]. 2017;9(7):674.
Solfrizzi V, Custodero C, Lozupone M, Imbimbo BP, Valiani V, Agosti P, et al. Relationships of Dietary Patterns, Foods, and Micro- and Macronutrients with Alzheimer’s Disease and Late-Life Cognitive Disorders: A Systematic Review. J Alzheimer’s Dis. 2017;59:815–49.
Block ML, Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32(9):506–16.
Calderón-Garcidueñas L, Azzarelli B, Acuna H, Garcia R, Gambling TM, Osnaya N, et al. Air pollution and brain damage. Toxicol Pathol. 2002;30(3):373–89.
Jeremy W. Air pollution and brain health: an emerging issue. Lancet. 2017;390:1345–422.
Mork D, Braun D, Zanobetti A. Time-lagged relationships between a decade of air pollution exposure and first hospitalization with Alzheimer’s disease and related dementias. Environ Int. 2023;171.
Li Z, Christensen GM, Lah JJ, Marcus M, Russell AG, Ebelt S, et al. Neighborhood characteristics as confounders and effect modifiers for the association between air pollution exposure and subjective cognitive functioning. Environ Res. 2022;212.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–46.
Carey IM, Anderson HR, Atkinson RW, Beevers SD, Cook DG, Strachan DP, et al. Are noise and air pollution related to the incidence of dementia? A cohort study in London, England. BMJ Open. 2018;8(9).
Mortamais M, Gutierrez L-A, de Hoogh K, Chen J, Vienneau D, Carrière I, et al. Long-term exposure to ambient air pollution and risk of dementia: Results of the prospective Three-City Study. Environ Int. 2021;148.
Guxens M, Lubczyńska MJ, Muetzel RL, Dalmau-Bueno A, Jaddoe VWV, Hoek G, et al. Air Pollution Exposure During Fetal Life, Brain Morphology, and Cognitive Function in School-Age Children. Biol Psychiatry. 2018;84(4):295–303.
Pujol J, Martínez-Vilavella G, Macià D, Fenoll R, Alvarez-Pedrerol M, Rivas I, et al. Traffic pollution exposure is associated with altered brain connectivity in school children. Neuroimage. 2016;129:175–84.
Forns J, Dadvand P, Foraster M, Alvarez-Pedrerol M, Rivas I, López-Vicente M, et al. Traffic-Related Air Pollution, Noise at School, and Behavioral Problems in Barcelona Schoolchildren: A Cross-Sectional Study. Environ Health Perspect. 2016;124(4):529–35.
Suades-González E, Gascon M, Guxens M, Sunyer J. Air Pollution and Neuropsychological Development: A Review of the Latest Evidence. Endocrinology. 2015;156(10):3473–82.
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev. 2021;10(1):39.
Santos WMd, Secoli SR, Püschel VAdA. The Joanna Briggs Institute approach for systematic reviews. Revista latino-americana de enfermagem. 2018;26:3074.
Kukull WA, Larson EB, Bowen JD, McCormick WC, Teri L, Pfanschmidt ML, et al. Solvent Exposure as a Risk Factor for Alzheimer’s Disease: A Case-Control Study. Am J Epidemiol. 1995;141(11):1059–71.
Wu Y-C, Lin Y-C, Yu H-L, Chen J-H, Chen T-F, Sun Y, et al. Association between air pollutants and dementia risk in the elderly. Alzheimer’s Dement. Diagn Assess Dis Monit. 2015;1(2):220–8.
Li C-Y, Li C-H, Martini S, Hou W-H. Association between air pollution and risk of vascular dementia: A multipollutant analysis in Taiwan. Environ Int. 2019;133: 105233.
Yuchi W, Sbihi H, Davies H, Tamburic L, Brauer M. Road proximity, air pollution, noise, green space and neurologic disease incidence: a population-based cohort study. Environ Health. 2020;19(1):8.
Rhew SH, Kravchenko J, Lyerly HK. Exposure to low-dose ambient fine particulate matter PM2.5 and Alzheimer’s disease, non-Alzheimer’s dementia, and Parkinson’s disease in North Carolina. PLOS ONE. 2021;16(7):e0253253.
Lin FC, Chen CY, Lin CW, Wu MT, Chen HY, Huang P. Air Pollution Is Associated with Cognitive Deterioration of Alzheimer’s Disease. Gerontology. 2021;68(1):53–61.
Tan J, Li N, Wang X, Chen G, Yan L, Wang L, et al. Associations of particulate matter with dementia and mild cognitive impairment in China: A multicenter cross-sectional study. The Innovation. 2021;2(3).
Petkus AJ, Younan D, Wang X, Beavers DP, Espeland MA, Gatz M, et al. Associations Between Air Pollution Exposure and Empirically Derived Profiles of Cognitive Performance in Older Women. J Alzheimer’s Dis. 2021;84:1691–707.
Semmens EO, Leary CS, Fitzpatrick AL, Ilango SD, Park C, Adam CE, et al. Air pollution and dementia in older adults in the Ginkgo Evaluation of Memory Study. Alzheimers Dement. 2023;19(2):549–59.
Calderón-Garcidueñas L, Chávez-Franco DA, Luévano-Castro SC, Macías-Escobedo E, Hernández-Castillo A, Carlos-Hernández E, et al. Metals, Nanoparticles, Particulate Matter, and Cognitive Decline. Front neurol. 2022;12:794071.
Calderón-Garcidueñas L, Hernández-Luna J, Mukherjee P S, Styner M, Chávez-Franco D A, Luévano-Castro S C, et al. Hemispheric Cortical, Cerebellar and Caudate Atrophy Associated to Cognitive Impairment in Metropolitan Mexico City Young Adults Exposed to Fine Particulate Matter Air Pollution. Toxics [Internet]. 2022;10(4):156.
Zhang H, Shi L, Ebelt S T, D’Souza R R, Schwartz J D, Scovronick N, et al. Short-term associations between ambient air pollution and emergency department visits for Alzheimer’s disease and related dementias. Environmental Epidemiology. 2022;7(1):e237.
Ranft U, Schikowski T, Sugiri D, Krutmann J, Krämer U. Long-term exposure to traffic-related particulate matter impairs cognitive function in the elderly. Environ Res. 2009;109(8):1004–11.
Chang K-H, Chang M-Y, Muo C-H, Wu T-N, Chen C-Y, Kao C-H. Increased Risk of Dementia in Patients Exposed to Nitrogen Dioxide and Carbon Monoxide: A Population-Based Retrospective Cohort Study. PLoS ONE. 2014;9(8): e103078.
Jung C-R, Lin Y-T, Hwang B-F. Ozone, Particulate Matter, and Newly Diagnosed Alzheimer’s Disease: A Population-Based Cohort Study in Taiwan. J Alzheimer’s Dis. 2015;44:573–84.
Oudin A, Forsberg B, Adolfsson Annelie N, Lind N, Modig L, Nordin M, et al. Traffic-Related Air Pollution and Dementia Incidence in Northern Sweden: A Longitudinal Study. Environ Health Perspect. 2016;124(3):306–12.
Chen H, Kwong JC, Copes R, Hystad P, van Donkelaar A, Tu K, et al. Exposure to ambient air pollution and the incidence of dementia: A population-based cohort study. Environ Int. 2017;108:271–7.
Culqui DR, Linares C, Ortiz C, Carmona R, Díaz J. Association between environmental factors and emergency hospital admissions due to Alzheimer’s disease in Madrid. Sci Total Environ. 2017;592:451–7.
Chen J-C, Wang X, Serre M. Particulate Air Pollutants, Brain Structure, and Neurocognitive Disorders in Older Women. Res Rep Health Eff Inst. 2017;2017(193):1–65.
Andersson J, Oudin A, Sundström A, Forsberg B, Adolfsson R, Nordin M. Road traffic noise, air pollution, and risk of dementia – results from the Betula project. Environ Res. 2018;166:334–9.
Oudin A, Segersson D, Adolfsson R, Forsberg B. Association between air pollution from residential wood burning and dementia incidence in a longitudinal study in Northern Sweden. PLoS ONE. 2018;13(6):e0198283.
Lee H, Kang JM, Myung W, Choi J, Lee C, Na DL, et al. Exposure to ambient fine particles and neuropsychiatric symptoms in cognitive disorder: A repeated measure analysis from the CREDOS (Clinical Research Center for Dementia of South Korea) study. Sci Total Environ. 2019;668:411–8.
Li R-L, Ho Y-C, Luo C-W, Lee S-S, Kuan Y-H. Influence of PM2.5 Exposure Level on the Association between Alzheimer’s Disease and Allergic Rhinitis: A National Population-Based Cohort Study. Int J Environ Res Public Health [Internet]. 2019;16(18):3357.
Cerza F, Renzi M, Gariazzo C, Davoli M, Michelozzi P, Forastiere F, et al. Long-term exposure to air pollution and hospitalization for dementia in the Rome longitudinal study. Environ Health. 2019;18(1):72.
Oudin A, Andersson J, Sundström A, Nordin Adolfsson A, Oudin Åström D, Adolfsson R, et al. Traffic-related air pollution as a risk factor for dementia: no clear modifying effects of APOE ɛ4 in the Betula cohort. J Alzheimer’s Dis. 2019;71(3):733–40.
Zhang H-W, Kok VC, Chuang S-C, Tseng C-H, Lin C-T, Li T-C, et al. Long-Term Exposure to Ambient Hydrocarbons Increases Dementia Risk in People Aged 50 Years and above in Taiwan. Curr Alzheimer Res. 2019;16(14):1276–89.
Smargiassi A, Sidi EAL, Robert L-E, Plante C, Haddad M, Gamache P, et al. Exposure to ambient air pollutants and the onset of dementia in Québec. Canada Environ Res. 2020;190:109870.
Ilango SD, Chen H, Hystad P, van Donkelaar A, Kwong JC, Tu K, et al. The role of cardiovascular disease in the relationship between air pollution and incident dementia: a population-based cohort study. Int J Epidemiol. 2020;49(1):36–44.
Paul KC, Haan M, Yu Y, Inoue K, Mayeda ER, Dang K, et al. Traffic-related air pollution and incident dementia: direct and indirect pathways through metabolic dysfunction. J Alzheimer’s Dis. 2020;76(4):1477–91.
Ran J, Schooling CM, Han L, Sun S, Zhao S, Zhang X, et al. Long-term exposure to fine particulate matter and dementia incidence: A cohort study in Hong Kong. Environ Pollut. 2021;271:116303.
Shaffer Rachel M, Blanco Magali N, Li G, Adar Sara D, Carone M, Szpiro Adam A, et al. Fine Particulate Matter and Dementia Incidence in the Adult Changes in Thought Study. Environ Health Perspect. 2021;129(8):087001.
Diana Y, Xinhui W, Ramon C, Ryan B, Sarah AG, Santiago S, et al. PM<sub>2.5</sub> Associated With Gray Matter Atrophy Reflecting Increased Alzheimer Risk in Older Women. Neurology. 2021;96(8):e1190.
Yitshak-Sade M, Nethery R, Schwartz J D, Mealli F, Dominici F, Di Q, et al. PM2.5 and hospital admissions among Medicare enrollees with chronic debilitating brain disorders. Sci Total Environ. 2021;755:142524.
Shaffer RM, Li G, Adar SD, Dirk Keene C, Latimer CS, Crane PK, et al. Fine Particulate Matter and Markers of Alzheimer’s Disease Neuropathology at Autopsy in a Community-Based Cohort. J Alzheimer’s Dis. 2021;79:1761–73.
Sullivan KJ, Ran X, Wu F, Chang C-CH, Sharma R, Jacobsen E, et al. Ambient fine particulate matter exposure and incident mild cognitive impairment and dementia. J Am Geriatr Soc. 2021;69(8):2185–94.
Kriit HK, Forsberg B, Åström DO, Oudin A. Annual dementia incidence and monetary burden attributable to fine particulate matter (PM2.5) exposure in Sweden. Environmental Health. 2021;20(1):65.
Shi L, Steenland K, Li H, Liu P, Zhang Y, Lyles RH, et al. A national cohort study (2000–2018) of long-term air pollution exposure and incident dementia in older adults in the United States. Nat Commun. 2021;12(1):6754.
Wu J, Grande G, Stafoggia M, Ljungman P, Laukka EJ, Eneroth K, et al. Air pollution as a risk factor for Cognitive Impairment no Dementia (CIND) and its progression to dementia: A longitudinal study. Environ Int. 2022;160: 107067.
Andersen ZJ, Zhang J, Jørgensen JT, Samoli E, Liu S, Chen J, et al. Long-term exposure to air pollution and mortality from dementia, psychiatric disorders, and suicide in a large pooled European cohort: ELAPSE study. Environ Int. 2022;170:107581.
Younan D, Wang X, Gruenewald T, Gatz M, Serre ML, Vizuete W, et al. Racial/Ethnic Disparities in Alzheimer’s Disease Risk: Role of Exposure to Ambient Fine Particles. The Journals of Gerontology: Series A. 2022;77(5):977–85.
He F, Tang J, Zhang T, Lin J, Li F, Gu X, et al. Impact of air pollution exposure on the risk of Alzheimer’s disease in China: A community-based cohort study. Environ Res. 2022;205:112318.
Wood D, Evangelopoulos D, Beevers S, Kitwiroon N, Katsouyanni K. Exposure to Ambient Air Pollution and the Incidence of Dementia in the Elderly of England: The ELSA Cohort. Int J Environ Res Public Health [Internet]. 2022;19(23):15889.
Chen C, Whitsel EA, Espeland MA, Snetselaar L, Hayden KM, Lamichhane AP, et al. B vitamin intakes modify the association between particulate air pollutants and incidence of all-cause dementia: Findings from the Women’s Health Initiative Memory Study. Alzheimers Dement. 2022;18(11):2188–98.
Letellier N, Gutierrez L-A, Duchesne J, Chen C, Ilango S, Helmer C, et al. Air quality improvement and incident dementia: Effects of observed and hypothetical reductions in air pollutant using parametric g-computation. Alzheimers Dement. 2022;18(12):2509–17.
Parra KL, Alexander GE, Raichlen DA, Klimentidis YC, Furlong MA. Exposure to air pollution and risk of incident dementia in the UK Biobank. Environ Res. 2022;209: 112895.
Trevenen ML, Heyworth J, Almeida OP, Yeap BB, Hankey GJ, Golledge J, et al. Ambient air pollution and risk of incident dementia in older men living in a region with relatively low concentrations of pollutants: The Health in Men Study. Environ Res. 2022;215.
Shi L, Zhu Q, Wang Y, Hao H, Zhang H, Schwartz J, et al. Incident dementia and long-term exposure to constituents of fine particle air pollution: A national cohort study in the United States. Proc Natl Acad Sci. 2023;120(1).
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool For Mild Cognitive Impairment. J Am Geriatr Soc. 2005;53(4):695–9.
Damian AM, Jacobson SA, Hentz JG, Belden CM, Shill HA, Sabbagh MN, et al. The Montreal Cognitive Assessment and the Mini-Mental State Examination as Screening Instruments for Cognitive Impairment: Item Analyses and Threshold Scores. Dement Geriatr Cogn Disord. 2011;31(2):126–31.
Freitas S, Simões MR, Alves L, Santana I. Montreal cognitive assessment: validation study for mild cognitive impairment and Alzheimer disease. Alzheimer Dis Assoc Disord. 2013;27(1):37–43.
Fasnacht JS, Wueest AS, Berres M, Thomann AE, Krumm S, Gutbrod K, et al. Conversion between the Montreal Cognitive Assessment and the Mini-Mental Status Examination. J Am Geriatr Soc. 2023;71(3):869–79.
Khachiyants N, Kim k. Mini-mental status examination mapping to the corresponding brain areas in dementia. Appl technol innov. 2012;12(3):60–3.
Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: A Comprehensive Review. J Am Geriatr Soc. 1992;40(9):922–35.
Ciesielska N, Sokołowski R, Mazur E, Podhorecka M, Polak-Szabela A, Kędziora-Kornatowska K. Is the Montreal Cognitive Assessment (MoCA) test better suited than the Mini-Mental State Examination (MMSE) in mild cognitive impairment (MCI) detection among people aged over 60? Meta-analysis Psychiatr Pol. 2016;50(5):1039–52.
Dong Y, Lee WY, Basri NA, Collinson SL, Merchant RA, Venketasubramanian N, et al. The Montreal Cognitive Assessment is superior to the Mini-Mental State Examination in detecting patients at higher risk of dementia. Int Psychogeriatr. 2012;24(11):1749–55.
Larner AJ. Screening utility of the Montreal Cognitive Assessment (MoCA): in place of – or as well as – the MMSE? Int Psychogeriatr. 2012;24(3):391–6.
Breton A, Casey D, Arnaoutoglou NA. Cognitive tests for the detection of mild cognitive impairment (MCI), the prodromal stage of dementia: Meta-analysis of diagnostic accuracy studies. Int J Geriatr Psychiatry. 2019;34(2):233–42.
Pinto TC, Machado L, Bulgacov TM, Rodrigues-Júnior AL, Costa ML, Ximenes RC, et al. Is the Montreal Cognitive Assessment (MoCA) screening superior to the Mini-Mental State Examination (MMSE) in the detection of mild cognitive impairment (MCI) and Alzheimer’s Disease (AD) in the elderly? Int Psychogeriatr. 2019;31(4):491–504.
Pendlebury ST, Markwick A, de Jager CA, Zamboni G, Wilcock GK, Rothwell PM. Differences in Cognitive Profile between TIA, Stroke and Elderly Memory Research Subjects: A Comparison of the MMSE and MoCA. Cerebrovasc Dis. 2012;34(1):48–54.
Siqueira GSA, Hagemann PdMS, Coelho DdS, Santos FHD, Bertolucci PHF. Can MoCA and MMSE Be Interchangeable Cognitive Screening Tools? A Systematic Review. Gerontol. 2019;59(6):e743–63.
Lloret A, Esteve D, Lloret M-A, Cervera-Ferri A, Lopez B, Nepomuceno M, et al. When Does Alzheimer′s Disease Really Start? The Role of Biomarkers. Int J Mol Sci. 2019;20(22):5536.
Williams-Gray CH, Mason SL, Evans JR, Foltynie T, Brayne C, Robbins TW, et al. The CamPaIGN study of Parkinson’s disease: 10-year outlook in an incident population-based cohort. J Neurol Neurosurg Psychiatry. 2013;84(11):1258–64.
Walker Z, Possin KL, Boeve BF, Aarsland D. Lewy body dementias. Lancet. 2015;386(10004):1683–97.
Svenningsson P, Westman E, Ballard C, Aarsland D. Cognitive impairment in patients with Parkinson’s disease: diagnosis, biomarkers, and treatment. Lancet Neurol. 2012;11(8):697–707.
Pedersen KF, Larsen JP, Tysnes O-B, Alves G. Prognosis of Mild Cognitive Impairment in Early Parkinson Disease: The Norwegian ParkWest Study. JAMA Neurol. 2013;70(5):580–6.
Williams-Gray CH, Evans JR, Goris A, Foltynie T, Ban M, Robbins TW, et al. The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the CamPaIGN cohort. Brain. 2009;132(11):2958–69.
Aarsland D, Kvaløy JT, Andersen K, Larsen JP, Tang MX, Lolk A, et al. The effect of age of onset of PD on risk of dementia. J Neurol. 2007;254(1):38–45.
Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E. Alzheimer’s disease. Lancet. 2011;377(9770):1019–31.
Bobinski M, de Leon MJ, Wegiel J, DeSanti S, Convit A, Saint Louis LA, et al. The histological validation of post mortem magnetic resonance imaging-determined hippocampal volume in Alzheimer’s disease. Neuroscience. 1999;95(3):721–5.
Dubois B, Feldman HH, Jacova C, DeKosky ST, Barberger-Gateau P, Cummings J, et al. Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS–ADRDA criteria. Lancet Neurol. 2007;6(8):734–46.
Jack CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9(1):119–28.
Scheltens P, Blennow K, Breteler MMB, de Strooper B, Frisoni GB, Salloway S, et al. Alzheimer’s disease. Lancet. 2016;388(10043):505–17.
Frisoni GB, Fox NC, Jack CR, Scheltens P, Thompson PM. The clinical use of structural MRI in Alzheimer disease. Nat Rev Neurol. 2010;6(2):67–77.
Fiandaca MS, Mapstone ME, Cheema AK, Federoff HJ. The critical need for defining preclinical biomarkers in Alzheimer’s disease. Alzheimers Dement. 2014;10(3S):S196–212.
Val JL, Bradley JK, Clifford R, Jack Jr, Matthew S, Stephen W, Maria S, et al. Comparison of 18F-FDG and PiB PET in Cognitive Impairment. J Nucl Med. 2009;50(6):878.
Toledo JB, Xie SX, Trojanowski JQ, Shaw LM. Longitudinal change in CSF Tau and Aβ biomarkers for up to 48 months in ADNI. Acta Neuropathol. 2013;126(5):659–70.
Ewers M, Brendel M, Rizk-Jackson A, Rominger A, Bartenstein P, Schuff N, et al. Reduced FDG-PET brain metabolism and executive function predict clinical progression in elderly healthy subjects. Neuroimage Clin. 2014;4:45–52.
Martin SB, Smith CD, Collins HR, Schmitt FA, Gold BT. Evidence that volume of anterior medial temporal lobe is reduced in seniors destined for mild cognitive impairment. Neurobiol Aging. 2010;31(7):1099–106.
Dickerson BC, Stoub TR, Shah RC, Sperling RA, Killiany RJ, Albert MS, et al. Alzheimer-signature MRI biomarker predicts AD dementia in cognitively normal adults. Neurology. 2011;76(16):1395.
Bradford CD, David AW. MRI cortical thickness biomarker predicts AD-like CSF and cognitive decline in normal adults. Neurology. 2012;78(2):84.
Fox NC, Crum WR, Scahill RI, Stevens JM, Janssen JC, Rossor MN. Imaging of onset and progression of Alzheimer’s disease with voxel-compression mapping of serial magnetic resonance images. Lancet. 2001;358(9277):201–5.
Jayaraj RL, Rodriguez EA, Wang Y, Block ML. Outdoor Ambient Air Pollution and Neurodegenerative Diseases: the Neuroinflammation Hypothesis. Curr Environ Health Rep. 2017;4(2):166–79.
Araujo JA, Barajas B, Kleinman M, Wang X, Bennett BJ, Gong KW, et al. Ambient Particulate Pollutants in the Ultrafine Range Promote Early Atherosclerosis and Systemic Oxidative Stress. Circ Res. 2008;102(5):589–96.
Cheng L, Lau WKW, Fung TKH, Lau BWM, Chau BKH, Liang Y, et al. PM2.5 Exposure Suppresses Dendritic Maturation in Subgranular Zone in Aged Rats. Neurotox Res. 2017;32(1):50–7.
Ku T, Li B, Gao R, Zhang Y, Yan W, Ji X, et al. NF-κB-regulated microRNA-574-5p underlies synaptic and cognitive impairment in response to atmospheric PM2.5 aspiration. Part Fibre Toxicol. 2017;14(1):34.
Liu X, Qian X, Xing J, Wang J, Sun Y, Wang Qg, et al. Particulate Matter Triggers Depressive-Like Response Associated With Modulation of Inflammatory Cytokine Homeostasis and Brain-Derived Neurotrophic Factor Signaling Pathway in Mice. Toxicol Sci. 2018;164(1):278–88.
Weuve J, Puett RC, Schwartz J, Yanosky JD, Laden F, Grodstein F. Exposure to Particulate Air Pollution and Cognitive Decline in Older Women. Arch Intern Med. 2012;172(3):219–27.
Tonne C, Elbaz A, Beevers S, Singh-Manoux A. Traffic-related air pollution in relation to cognitive function in older adults. Epidemiology. 2014;25(5):674–81.
Wurth R, Kioumourtzoglou MA, Tucker KL, Griffith J, Manjourides J, Suh H. Fine Particle Sources and Cognitive Function in An Older Puerto Rican Cohort in Greater Boston. Environ Epidemiol. 2018;2(3): e022.
Gallagher M, Koh MT. Episodic memory on the path to Alzheimer’s disease. Curr Opin Neurobiol. 2011;21(6):929–34.
Aisen PS, Cummings J, Jack CR, Morris JC, Sperling R, Frölich L, et al. On the path to 2025: understanding the Alzheimer’s disease continuum. Alzheimers Res Ther. 2017;9(1):60.
Dickerson BC, Eichenbaum H. The Episodic Memory System: Neurocircuitry and Disorders. Neuropsychopharmacology. 2010;35(1):86–104.
Zhao W, W, Wang X, X, Yin C, He M, Li S, Han Y. Trajectories of the Hippocampal Subfields Atrophy in the Alzheimer’s Disease: A Structural Imaging Study. Front Neuroinform. 2019;13:13.
Fonken LK, Xu X, Weil ZM, Chen G, Sun Q, Rajagopalan S, et al. Air pollution impairs cognition, provokes depressive-like behaviors and alters hippocampal cytokine expression and morphology. Mol Psychiatry. 2011;16(10):987–95.
Davis DA, Akopian G, Walsh JP, Sioutas C, Morgan TE, Finch CE. Urban air pollutants reduce synaptic function of CA1 neurons via an NMDA/NȮ pathway in vitro. J Neurochem. 2013;127(4):509–19.
Woodward NC, Pakbin P, Saffari A, Shirmohammadi F, Haghani A, Sioutas C, et al. Traffic-related air pollution impact on mouse brain accelerates myelin and neuritic aging changes with specificity for CA1 neurons. Neurobiol Aging. 2017;53:48–58.
Zammit AR, Ezzati A, Zimmerman ME, Lipton RB, Lipton ML, Katz MJ. Roles of hippocampal subfields in verbal and visual episodic memory. Behav Brain Res. 2017;317:157–62.
Casanova R, Wang X, Reyes J, Akita Y, Serre ML, Vizuete W, et al. A Voxel-Based Morphometry Study Reveals Local Brain Structural Alterations Associated with Ambient Fine Particles in Older Women. Front Hum Neurosci. 2016;10:495.
Chen J-C, Wang X, Wellenius GA, Serre ML, Driscoll I, Casanova R, et al. Ambient air pollution and neurotoxicity on brain structure: Evidence from women’s health initiative memory study. Ann Neurol. 2015;78(3):466–76.
Cho J, Noh Y, Kim SY, Sohn J, Noh J, Kim W, et al. Long-term ambient air pollution exposures and brain imaging markers in Korean adults: the Environmental Pollution-Induced Neurological EFfects (EPINEF) study. Environ Health Perspect. 2020;128(11).
Power MC, Lamichhane AP, Liao D, Xu X, Jack CR, Gottesman RF, et al. The association of long-term exposure to particulate matter air pollution with brain MRI findings: the ARIC study. Environ Health Perspect. 2018;126(2): 027009.
Wilker EH, Preis SR, Beiser AS, Wolf PA, Au R, Kloog I, et al. Long-term exposure to fine particulate matter, residential proximity to major roads and measures of brain structure. Stroke. 2015;46(5):1161–6.
Bejanin A, Schonhaut DR, La Joie R, Kramer JH, Baker SL, Sosa N, et al. Tau pathology and neurodegeneration contribute to cognitive impairment in Alzheimer’s disease. Brain. 2017;140(12):3286–300.
Jagust W. Imaging the evolution and pathophysiology of Alzheimer disease. Nat Rev Neurosci. 2018;19(11):687–700.
Harrison TM, La Joie R, Maass A, Baker SL, Swinnerton K, Fenton L, et al. Longitudinal tau accumulation and atrophy in aging and alzheimer disease. Ann Neurol. 2019;85(2):229–40.
Power MC, Adar SD, Yanosky JD, Weuve J. Exposure to air pollution as a potential contributor to cognitive function, cognitive decline, brain imaging, and dementia: A systematic review of epidemiologic research. Neurotoxicology. 2016;56:235–53.
Schwartz M, Deczkowska A. Neurological Disease as a Failure of Brain-Immune Crosstalk: The Multiple Faces of Neuroinflammation. Trends Immunol. 2016;37(10):668–79.
Zhu X, Raina AK, Lee H-g, Casadesus G, Smith MA, Perry G. Oxidative stress signalling in Alzheimer’s disease. Brain Res. 2004;1000(1–2):32–9.
Gruzieva O, Merid SK, Gref A, Gajulapuri A, Lemonnier N, Ballereau S, et al. Exposure to traffic-related air pollution and serum inflammatory cytokines in children. Environ Health Perspect. 2017;125(6).
Alemany S, Crous-Bou M, Vilor-Tejedor N, Milà-Alomà M, Suárez-Calvet M, Salvadó G, et al. Associations between air pollution and biomarkers of Alzheimer’s disease in cognitively unimpaired individuals. Environ Int. 2021;157.
Ma Y-H, Chen H-S, Liu C, Feng Q-S, Feng L, Zhang Y-R, et al. Association of Long-term Exposure to Ambient Air Pollution With Cognitive Decline and Alzheimer’s Disease-Related Amyloidosis. Biol Psychiatry. 2023;93(9):780–9.
Jack CR, Holtzman DM. Biomarker modeling of Alzheimer’s disease. Neuron. 2013;80(6):1347–58.
Dubois B, Hampel H, Feldman HH, Scheltens P, Aisen P, Andrieu S, et al. Preclinical Alzheimer’s disease: Definition, natural history, and diagnostic criteria. Alzheimers Dement. 2016;12(3):292–323.
Buchhave P, Minthon L, Zetterberg H, Wallin ÅK, Blennow K, Hansson O. Cerebrospinal Fluid Levels ofβ-Amyloid 1–42, but Not of Tau, Are Fully Changed Already 5 to 10 Years Before the Onset of Alzheimer Dementia. Arch Gen Psychiatry. 2012;69(1):98–106.
Calderón-Garcidueñas L, Solt AC, Henríquez-Roldán C, Torres-Jardón R, Nuse B, Herritt L, et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid β-42 and α-synuclein in children and young adults. Toxicol Pathol. 2008;36(2):289–310.
Fu M, Wang H, Bai Q, Du J, Niu Q, Nie J. Urinary polycyclic aromatic hydrocarbon metabolites, plasma p-tau231 and mild cognitive impairment in coke oven workers. Chemosphere. 2022;307.
Cleveland DW, Hwo S-Y, Kirschner MW. Physical and chemical properties of purified tau factor and the role of tau in microtubule assembly. J Mol Biol. 1977;116(2):227–47.
Medeiros R, Baglietto-Vargas D, LaFerla FM. The Role of Tau in Alzheimer’s Disease and Related Disorders. CNS Neurosci Ther. 2011;17(5):514–24.
Suárez-Calvet M, Karikari TK, Ashton NJ, Lantero Rodriguez J, Milà-Alomà M, Gispert JD, et al. Novel tau biomarkers phosphorylated at T181, T217 or T231 rise in the initial stages of the preclinical Alzheimer’s continuum when only subtle changes in Aβ pathology are detected. EMBO Mol Med. 2020;12(12).
Baek MS, Lee MJ, Kim H-K, Lyoo CH. Temporal trajectory of biofluid markers in Parkinson’s disease. Sci Rep. 2021;11(1):14820.
Nie J, Duan L, Yan Z, Niu Q. Tau Hyperphosphorylation is Associated with Spatial Learning and Memory After Exposure to Benzo[a]pyrene in SD Rats. Neurotox Res. 2013;24(4):461–71.
Isaksen JL, Ghouse J, Skov MW, Olesen MS, Holst AG, Pietersen A, et al. Associations between primary care electrocardiography and non-Alzheimer dementia. Journal of Stroke and Cerebrovasc Dis. 2022;31(9).
Kuang H, Zhou ZF, Zhu YG, Wan ZK, Yang MW, Hong FF, et al. Pharmacological Treatment of Vascular Dementia: A Molecular Mechanism Perspective. Aging Dis. 2021;12(1):308–26.
O’Brien JT, Thomas A. Vascular dementia. Lancet. 2015;386(10004):1698–706.
Aarsland D, Creese B, Politis M, Chaudhuri KR, ffytche DH, Weintraub D, et al. Cognitive decline in Parkinson disease. Nat Rev Neurol. 2AD;13(4):217–31.
Bang J, Spina S, Miller BL. Frontotemporal dementia. Lancet. 2015;386(10004):1672–82.
Ashton NJ, Hye A, Rajkumar AP, Leuzy A, Snowden S, Suárez-Calvet M, et al. An update on blood-based biomarkers for non-Alzheimer neurodegenerative disorders. Nat Rev Neurol. 2020;16(5):265–84.
Künzli N, Jerrett M, Mack Wendy J, Beckerman B, LaBree L, Gilliland F, et al. Ambient Air Pollution and Atherosclerosis in Los Angeles. Environ Health Perspect. 2005;113(2):201–6.
Sweeney MD, Ayyadurai S, Zlokovic BV. Pericytes of the neurovascular unit: key functions and signaling pathways. Nat Neurosci. 2016;19(6):771–83.
Pandey T, Abubacker S. Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy: An Imaging Mimic of Multiple Sclerosis. Med Princ Pract. 2006;15(5):391–5.
Romay MC, Toro C, Iruela-Arispe ML. Emerging molecular mechanisms of vascular dementia. Curr Opin Hematol. 2019;26(3):199–206.
Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 2019;18(7):684–96.
Kalaria RN. Neuropathological diagnosis of vascular cognitive impairment and vascular dementia with implications for Alzheimer’s disease. Acta Neuropathol. 2016;131(5):659–85.
Iadecola C. The Pathobiology of Vascular Dementia. Neuron. 2013;80(4):844–66.
Kalaria RN. The pathology and pathophysiology of vascular dementia. Neuropharmacology. 2018;134:226–39.
Du S-Q, Wang X-R, Xiao L-Y, Tu J-F, Zhu W, He T, et al. Molecular Mechanisms of Vascular Dementia: What Can Be Learned from Animal Models of Chronic Cerebral Hypoperfusion? Mol Neurobiol. 2017;54(5):3670–82.
Wolters FJ, Zonneveld HI, Hofman A, Van Der Lugt A, Koudstaal PJ, Vernooij MW, et al. Cerebral perfusion and the risk of dementia: a population-based study. Circulation. 2017;136(8):719–28.
Benedictus MR, Binnewijzend MAA, Kuijer JPA, Steenwijk MD, Versteeg A, Vrenken H, et al. Brain volume and white matter hyperintensities as determinants of cerebral blood flow in Alzheimer’s disease. Neurobiol Aging. 2014;35(12):2665–70.
Babadjouni R, Patel A, Liu Q, Shkirkova K, Lamorie-Foote K, Connor M, et al. Nanoparticulate matter exposure results in neuroinflammatory changes in the corpus callosum. PLoS ONE. 2018;13(11).
Liu Q, Radwanski R, Babadjouni R, Patel A, Hodis DM, Baumbacher P, et al. Experimental chronic cerebral hypoperfusion results in decreased pericyte coverage and increased blood–brain barrier permeability in the corpus callosum. J Cereb Blood Flow Metab. 2019;39(2):240–50.
Erickson LD, L D, Gale S D, Anderson J E, Brown B L, Hedges D W. Association between Exposure to Air Pollution and Total Gray Matter and Total White Matter Volumes in Adults: A Cross-Sectional Study. Brain Sci [Internet]. 2020;10(3):164.
Woodward NC, Levine MC, Haghani A, Shirmohammadi F, Saffari A, Sioutas C, et al. Toll-like receptor 4 in glial inflammatory responses to air pollution in vitro and in vivo. J Neuroinflammation. 2017;14(1):84.
Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord. 2007;22(12):1689–707.
Aarsland D, Zaccai J, Brayne C. A systematic review of prevalence studies of dementia in Parkinson’s disease. Mov Disord. 2005;20(10):1255–63.
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30(12):1591–601.
Goetz CG, Emre M, Dubois B. Parkinson’s disease dementia: Definitions, guidelines, and research perspectives in diagnosis. Ann Neurol. 2008;64(S2):S81–92.
Elobeid A, Libard S, Leino M, Popova SN, Alafuzoff I. Altered Proteins in the Aging Brain. J Neuropathol Exp Neurol. 2016;75(4):316–25.
Kovacs G G. Molecular Pathological Classification of Neurodegenerative Diseases: Turning towards Precision Medicine. Int J Mol Sci [Internet]. 2016;17(2):189.
Calderón-Garcidueñas L, Ayala A. Air Pollution, Ultrafine Particles, and Your Brain: Are Combustion Nanoparticle Emissions and Engineered Nanoparticles Causing Preventable Fatal Neurodegenerative Diseases and Common Neuropsychiatric Outcomes? Environ Sci Technol. 2022;56(11):6847–56.
Calderón-Garcidueñas L, Gónzalez-Maciel A, Reynoso-Robles R, Delgado-Chávez R, Mukherjee PS, Kulesza RJ, et al. Calderón-Garcidueñas L, Gónzalez-Maciel A, Reynoso-Robles R, Delgado-Chávez R, Mukherjee PS, Kulesza RJ, et al. Hallmarks of Alzheimer disease are evolving relentlessly in Metropolitan Mexico City infants, children and young adults. APOE4 carriers have higher suicide risk and higher odds of reaching NFT stage V at ≤ 40 years of age. Environ Res. 2018;164:475–87. Environ Res. 2018;164:475–87.
Calderón-Garcidueñas L, González-Maciel A, Reynoso-Robles R, Hammond J, Kulesza R, Lachmann I, et al. Quadruple abnormal protein aggregates in brainstem pathology and exogenous metal-rich magnetic nanoparticles (and engineered Ti-rich nanorods). The substantia nigrae is a very early target in young urbanites and the gastrointestinal tract a key brainstem portal. Environ Res. 2020;191:110139.
Fiondella L, Mattioli I, Salemme S, Carbone C, Vinceti G, Tondelli M, et al. The brain correlates of behavioral disturbances in frontotemporal dementia. Alzheimers Dement. 2021;17(S6).
Rosen HJ, Gorno-Tempini ML, Goldman WP, Perry RJ, Schuff N, Weiner M, et al. Patterns of brain atrophy in frontotemporal dementia and semantic dementia. Neurology. 2002;58(2):198.
Woollacott IOC, Rohrer JD. The clinical spectrum of sporadic and familial forms of frontotemporal dementia. J Neurochem. 2016;138(S1):6–31.
Ber IL, Guedj E, Gabelle A, Verpillat P, Volteau M, Thomas-Anterion C, et al. Demographic, neurological and behavioural characteristics and brain perfusion SPECT in frontal variant of frontotemporal dementia. Brain. 2006;129(11):3051–65.
Tang J, Chen A, He F, Shipley M, Nevill A, Coe H, et al. Association of air pollution with dementia: a systematic review with meta-analysis including new cohort data from China. Environ Res. 2023;223.
Abolhasani E, Hachinski V, Ghazaleh N, Azarpazhooh MR, Mokhber N, Martin J. Air Pollution and Incidence of Dementia. Neurology. 2023;100(2):e242–54.
Peters R, Ee N, Peters J, Booth A, Mudway I, Anstey KJ. Air pollution and dementia: a systematic review. J Alzheimer’s Dis. 2019;70(s1):S145–63.
Delgado-Saborit JM, Guercio V, Gowers AM, Shaddick G, Fox NC, Love S. A critical review of the epidemiological evidence of effects of air pollution on dementia, cognitive function and cognitive decline in adult population. Sci Total Environ. 2021;757.
Xu X, Ha SU, Basnet R. Basnet R. A Review of Epidemiological Research on Adverse Neurological Effects of Exposure to Ambient Air Pollution. Front Public Health. 2016;4:157.
Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012;11(11):1006–12.
Xu H, Dupre ME, Gu D, Wu B. The impact of residential status on cognitive decline among older adults in China: Results from a longitudinal study. BMC Geriatr. 2017;17(1):107.
Acknowledgements
Not applicable.
Funding
No funding was secured for this study.
Author information
Authors and Affiliations
Contributions
M.M and A.H. Kh conceptualized the study and were involved in screening and data extraction. All authors were involved in the interpretation of the findings. M.M wrote the first draft. All authors were involved in the scientific processes leading up to the writing of the manuscript and contributed to the interpretation of the findings and the critical evaluation of the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mohammadzadeh, M., Khoshakhlagh, A.H. & Grafman, J. Air pollution: a latent key driving force of dementia. BMC Public Health 24, 2370 (2024). https://doi.org/10.1186/s12889-024-19918-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19918-4