Abstract
Background
Preterm birth (PTB) is an important predictor of perinatal morbidity and mortality. Previous researches have reported a correlation between air pollution and an increased risk of preterm birth. However, the specific relationship between short-term and long-term exposure to carbon monoxide (CO) and preterm birth remains less explored.
Methods
A population-based study was conducted among 515,498 pregnant women in Chongqing, China, to assess short-term and long-term effects of CO on preterm and very preterm births. Generalized additive models (GAM) were applied to evaluate short-term effects, and exposure-response correlation curves were plotted after adjusting for confounding factors. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated using COX proportional hazard models to estimate the long-term effect.
Results
The daily incidence of preterm and very preterm birth was 5.99% and 0.41%, respectively. A positive association between a 100 µg/m³ increase in CO and PTB was observed at lag 0–3 days and 12–21 days, with a maximum relative risk (RR) of 1.021(95%CI: 1.001–1.043). The exposure-response curves (lag 0 day) revealed a rapid increase in PTB due to CO. Regarding long-term exposure, positive associations were found between a 100 µg/m3 CO increase for each trimester(Model 2 for trimester 1: HR = 1.054, 95%CI: 1.048–1.060; Model 2 for trimester 2: HR = 1.066, 95%CI: 1.060–1.073; Model 2 for trimester 3: HR = 1.007, 95%CI: 1.001–1.013; Model 2 for entire pregnancy: HR = 1.080, 95%CI: 1.073–1.088) and higher HRs of very preterm birth. Multiplicative interactions between air pollution and CO on the risk of preterm and very preterm birth were detected (P- interaction<0.05).
Conclusions
Our findings suggest that short-term exposure to low levels of CO may have protective effects against preterm birth, while long-term exposure to low concentrations of CO may reduce the risk of both preterm and very preterm birth. Moreover, our study indicated that very preterm birth is more susceptible to the influence of long-term exposure to CO during pregnancy, with acute CO exposure exhibiting a greater impact on preterm birth. It is imperative for pregnant women to minimize exposure to ambient air pollutants.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
According to the definition provided by the World Health Organization (WHO), preterm birth refers to the delivery of a live baby before completing 37 weeks of gestation, with subcategories including very preterm birth (VPTB, < 32 weeks gestation) [1]. Numerous studies have demonstrated that preterm birth (PTB) serves as a crucial predictor of perinatal morbidity and mortality [2, 3]. Infants born before 25 weeks of gestation face a 40% likelihood of mortality before discharge [4]. By 34 weeks, only 50% of preterm infants exhibit a survival rate, and at the age of 2 years old, approximately 4% manifest cerebral palsy, while 8% experience neurological delays [4,5,6]. Furthermore, preterm birth affects 5 to 11% of newborns globally, varying by ethnicity, country, or other factors [7].
Air pollution has emerged as a significant environmental hazard to human health. The 2017 Global Burden of Diseases (GBD) Study revealed that over 4.9 million preterm births worldwide could be attributable to ambient air pollution, with 1.2 million occurring in China alone [8]. Our prior investigations delved into the correlation between exposure to ambient air pollutants and adverse birth outcomes [9,10,11,12]. The exposure assessment relied on measurements obtained from 17 ground monitoring stations located in Chongqing. Our research found that elevated levels of PM2.5 and PM10 were linked to higher risk of spontaneous abortion for short-term effects [12]. Additionally, we reported that maternal exposure to high levels of PM2.5 and PM10 during pregnancy may increase risk for preterm birth at late stage of pregnancy. There was important to note that exposure to CO significantly increased the risk of preterm birth during each trimester and entire pregnancy [11].
CO, a colorless, odorless gas resulting from the incomplete combustion of fossil fuels, has been the focus of epidemiological literature linking environmental fine particulate matter to an elevated risk of preterm birth [13,14,15,16]. A prospective birth cohort study found 15% increases in risk of PTB with 100 µg/m3 increase in CO mean concentrations [17]. However, a research from Southern California suggests that increased concentrations of CO in the environment may (to a lesser extent) contribute to the occurrence of preterm birth [18].
Few researchers have specifically explored the relationship between CO and preterm birth, particularly very preterm birth. The present study concentrates specifically on evaluating the impact of carbon monoxide (CO) on preterm birth. This investigation not only expands upon the earlier analysis of preterm birth but also introduces results about very preterm birth and maternal age stratification to calculate the hazard risk (HR). Consequently, our focus in this research is to explore and assess both short-term and long-term effects of ambient CO on preterm birth.
Materials and methods
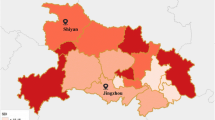
Study area
Chongqing is a large municipality located in southwest China, under the direct control of the national government. It is situated between longitudes 28°10′ N-32°13′ N and latitudes 105°11′ E -110°11′ E. It covers an area of 82,400 square kilometers. Moreover, Chongqing is nicknamed “Fog City” due to its basin topography and meteorological conditions that hinder the diffusion of air pollutants. According to the seventh population census of China, the resident population of Chongqing is 32.12 million. The research area of this paper was the main urban area of Chongqing, including nine closely connected districts: Yubei, Jiulongpo, Jiangbei, Yuzhong, Dadukou, Shapingba, Nanan, Banan and Beibei.
Study population
This is a retrospective cohort study using 5-year daily data. The birth outcome data was obtained from the Chongqing Birth Certificate System, including the gestational age, date of birth, maternal address, etc. After excluding those who lacked gestational age and non-urban residents, we obtained 515,498 pregnant women living in the main urban area of Chongqing from 2016 to 2020. After delivery, the baby’s birth information was filled in the neonatal care record system by the health care worker or midwife. The information was then verified and uploaded to the system. Parents and healthcare boards confirm this information before issuing a birth certificate.
Exposure assessment and outcomes
During the research period, daily 24-hour monitor data of PM2.5, PM10, SO2, NO2, CO and O3 (8 h maximum value) were collected from 17 ground-based monitoring stations in Chongqing via the Chinese National Urban Air Quality Monitoring Platform (https://zhb.gov.cn). Daily average relative humidity and temperature were available from the China Greenhouse Data Sharing Platform (http://data.sheshiyuanyi.com, accessed on 2 April 2021).
For short-term effect of pollutants, we took the number of preterm and very preterm births per day as the independent variable, and the average daily concentrations of pollutants and meteorological factors as the covariate from the perspective of population.
For long-term exposure to pollutants, each pregnant woman’s exposure to air pollutants and meteorological factors was calculated for each day from fertilization to delivery. Specifically, maternal addresses were geocoded to x and y coordinates with Python through Amap key. Then, we used inverse distance weighting (IDW) to assess each pregnancy woman’s exposure to six pollutants, temperature and relative humidity by ArcGIS during each day of pregnancy. Finally, we averaged the pollutants and meteorological factors of each woman in each trimester and the entire pregnancy period.
Outcomes
Gestational age at the time of delivery was calculated in weeks from the first day of the last menstrual period. Based on gestational age, preterm birth was defined as a live birth that occurs before 37 completed weeks of gestation [19]. Very preterm birth was defined as a delivery prior to 32 completed weeks of gestation. Full term birth was defined as a birth occurs at 37 or more weeks of gestation.
Data analysis
Previous researches have shown that the relationship between preterm birth and very preterm birth are small probability events, and have a non-linear relationship with air pollution.
Thus, for short-term effects, we used distributed lag nonlinear model (DLNM) with quasi-Poisson GAM to estimate effect of CO on preterm birth. The equation was as follows:
Where \({Y}_{t}\) is the observed daily preterm birth counts at day t; \(\propto\) is the model intercept; \({Pollution}_{t}\) stands for the pollutant concentration at day \(t\), \({Temp}_{t}\) represents the temperature on day \(t\), \({RH}_{t}\) represents the relative humidity on day \(t\); \(cb\left({Temp}_{t},lag\right)\), \(cb\left({RH}_{t},lag\right)\) indicates the matrix of temperature and relative humidity. \(s\left({CO}_{t},{Pollution}_{t}\right)\) is the interaction effect of CO and air pollution. Then we use the DLNMs by the definition of a “cross-basis” function, a two dimensional function space expressing the influence of the predictor range and in its lag dimension. \({Time}_{t}\) is time trend, and ns() denotes a natural cubic smooth spline function that eliminates unobserved long-term and seasonal patterns from the dataset of time series. \({DOW}_{t}\) was the day of week; \({holiday}_{t}\) represent dummy variable (0 indicates non-holiday, and 1 indicates a holiday).
For the long-term effects, we used Cox proportional hazards models to assess the hazard ratios (HRs) of preterm birth with CO exposure in each trimester and entire pregnancy period, respectively. The time scale used gestational age which allows for better control of association of preterm birth risk and gestational age. More importantly, the Cox model provides a more straightforward interpretation that translates HRs into “risk” compared to the ratio of the odds from logistic regression. We fitted three models for each exposure time window: an unadjusted model (Model 1); a model adjusted for temperature and relative humidity (Model 2); a model adjusted for interaction term (exposure of CO and other each air pollutant), temperature and relative humidity (Model 3). In model 3, we used a multiplicative interaction term to explore the interactions between CO and other air pollutants (PM2.5, PM10, NO2, SO2, O3), and p < 0.05 of the product term indicates a multiplicative interaction.
To assess potential effect modification by maternal age, we performed analysis stratified by age (≤ 21 years, 22–34 years, and ≥ 35 years), and obtained HRs and 95% confidence intervals (CIs). Furthermore, we employed a restricted cubic spline (RCS) with four knots (ascertained by using the Akaike information criterion) to construct exposure-response curves for the association between long-term CO exposure and risk of incident preterm and very preterm birth. The nonlinearity was assessed using ANOVA F statistic, while the findings were visually presented through a line plot.
In addition to the main analyses, we performed several sensitivity analyses to confirm the robustness of our estimates by: (1) excluding the mothers whose residential address was more than 10 km away from the nearest monitoring station; (2)plotting the exposure-response curves of CO for incident preterm and very preterm birth risk; (3)further adjusting temperature, relative humidity and multiplicative interaction. (4)building a multi-trimester model including CO exposure in first, second and third trimester to check the robustness of the estimated associations. R software (version 4.1.3, R Foundation for Statistical Computing, Vienna, Austria) was used for all analyses, with “mgcv”, “spline” and“dlnm” packages. A probability value of<0.05 was considered statistically significant for all statistical tests.
Results
Descriptive statistics of the research objects
We summarized the demographic characteristics of live births in urban of Chongqing, China (Table 1). From January 1 st, 2016 to December 31 st, 2020, a total of 515.498 live births were identified from the birth register system. Among these, 30,884 live births were preterm (5.99%), 2120 were very preterm births (0.41%), and 484,614 were full-term births (94.01%). The incidence of both preterm birth and very preterm birth increases with advanced maternal age, particularly when the mother was 35 years old or older. Notably, both preterm and very preterm births exhibited higher average concentrations of CO during each trimester and throughout the entire pregnancy compared to full-term births. Throughout the entire pregnancy, very preterm births had the highest average level of CO compared to full-term and preterm births.
Supplementary Fig. 1 illustrates the time-series trends of ambient air pollution, daily preterm births and very preterm births from 2013 to 2019. The concentrations of PM2.5, PM10, SO2, NO2 and CO exhibited seasonal variations, with higher levels observed during winter months and lower levels during summer. The daily incidence of preterm birth was 16.923, while that of very preterm birth was 1.162. Over the five-year period, the average concentration of PM2.5, PM10, SO2, NO2, O3, and CO was 40.735 µg/m3, 64.003 µg/m3, 9.376 µg/m3, 40.249 µg/m3, 42.368 µg/m3 and 886.521 µg/m3, respectively. Additionally, the average daily relative humidity was 75.105%, and the mean temperature was 19.972℃ (Supplementary Table 1).
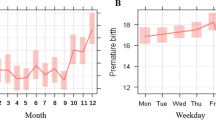
Short-term effect
We conducted a risk assessment to evaluate the potential acute impact of CO on the rates of preterm and very preterm births, as depicted in Fig. 1. Our findings indicate that pregnant mothers exposed to CO may have an increased likelihood of giving birth prematurely, particularly when exposed during lag 0–3 days and 12–21 days. The maximum RR was 1.021, with a 95% confidence interval ranging from 1.001 to 1.043. However, no significant association with CO was observed for very preterm births. To further elucidate the relationship between the concentrations of CO and preterm and very preterm birth, exposure-response correlation curves were plotted at lag 0 day, as shown in Fig. 2. Notably, the response curve for CO exposure exhibited a protective effect on preterm birth at relatively low levels. Conversely, at higher concentrations, CO posed a risk factor for preterm birth, with a positive correlation between concentration and log(RR) value. No evidence was found for a relationship between CO concentrations and very preterm births on the current day.
Long-term effect
Tables 2 and 3 present the unadjusted and adjusted hazard risk of preterm and very preterm birth linked to CO exposure during each trimester and the entire pregnancy. Model 2, accounting for temperature and humidity, revealed that CO exposure during the first trimester, second trimester, and entire pregnancy had a greater impact on preterm birth compared to Model 1. Each 100 µg/m3 increase in CO concentration before conception was significantly associated with preterm birth (Model 2 for trimester 1: HR = 1.054, 95%CI: 1.048–1.060; Model 2 for trimester 2: HR = 1.066, 95%CI: 1.060–1.073; Model 2 for trimester 3: HR = 1.007, 95%CI: 1.001–1.013; Model 2 for entire pregnancy: HR = 1.080, 95%CI: 1.073–1.088). The strongest effect for preterm birth was observed in the second trimester for CO, while for very preterm birth it was in the first trimester.
Significantly multiplicative interactions were identified between air pollutants (PM2.5, PM10, NO2 and SO2) and CO on the risk of preterm birth and very preterm birth (Tables 2 and 3). The largest HR (95% CI) for preterm birth was associated with the combination of CO and PM2.5 in trimester 2 (HR = 1.162, 95%CI: 1.150–1.174). In addition, the combined effect of O3 and CO on preterm birth was diminished due to their multiplicative interactions. The adjusted HR (Model 2) for preterm birth with every 100 µg/m3 increase in CO was 1.054 (95%CI: 1.048, 1.060), and the HR value for the interaction between CO and O3 during early pregnancy was 1.151 (95%CI: 1.045–1.157). Similar significantly multiplicative interactions were found between individual air pollutants and CO on the risk of very preterm birth. Moreover, the effect of CO on very preterm birth was higher than that on preterm birth at the same time and model. Interestingly, the impact of CO in the third trimester, whether on preterm or very preterm birth, was found to be minimal.
In the stratified analyses, the risk of preterm and very preterm birth associated with long-term CO exposure varied by maternal age ( Figs. 3 and 4). In model 2, mothers aged over 35 exhibited the highest risk of preterm birth when exposed to CO compared to those aged ≤ 21 and 22–34 in the 1st trimester (HR = 1.071, 95%CI: 1.056–1.086), 2nd trimester (HR = 1.061, 95%CI: 1.045–1.077) and entire pregnancy (HR = 1.074, 95%CI: 1.056–1.093). An intriguing result in the 3rd trimester indicated a protective effect of CO against preterm birth in mothers aged ≤ 21 (HR = 0.959, 95%CI: 0.931–0.987) and ≥ 35 (HR = 0.976, 95%CI: 0.962–0.990). Notably, in the group of mothers aged ≤ 21 (HR = 0.782, 95%CI: 0.706–0.866), CO exposure in the 3rd trimester exhibited a protective effect against very preterm birth, suggesting a potential risk reduction for pregnant women in this age group.
The results of restricted cubic spline (RCS) models, presented in Fig. 5, further confirmed the non-linear dose-response association between ambient CO exposure and the risk of preterm and very preterm births during the entire pregnancy. Elevated CO concentrations above thresholds were positively associated with an increased risk of preterm and very preterm births. HRs for preterm and very preterm birth at the 95th percentile of CO, compared to the thresholds, were 1.150 (95%CI: 1.105–1.196) and 1.345 (95%CI: 1.169–1.548), respectively. However, HRs for preterm and very preterm birth at the 25th percentile of CO, compared to the thresholds, were 0.928 (95%CI: 0.914–0.942) and 0.806 (95%CI: 0.760–0.855), respectively.
Dose-response associations (smoothing by RCS function with five knots) of preterm and very preterm with ambient CO exposure during the entire pregnancy, with the mean of CO exposure serving as the reference value. Models were adjusted for temperature and relative humidity. Hazard risk was represented by a bold line, and the 95% confidence interval was represented by the shaded area
Discussion
To our knowledge, this study represents the first extensive population-based investigation addressing both acute and chronic effects of ambient carbon monoxide (CO) on preterm and very preterm birth. Our results indicated that exposure to ambient CO has an acute effect on preterm birth at lag 0–3 and lag 12–21 days, with no significant impact on very preterm birth. Notably, a protective effect on preterm birth was observed at lag 0 day for CO concentrations below the threshold. Concerning long-term effects, increased CO concentrations during each trimester and throughout the entire pregnancy were associated with an elevated risk of both preterm and very preterm birth.
Despite CO being widely recognized as a common cause of poisoning and a routinely monitored air pollutant, our threshold analyses reveal that both acute and chronic exposure to low-level CO was associated with a reduced risk of preterm birth, with long-term low-dose exposure being protective against very preterm birth. This suggests that the effects of CO may vary at different exposure levels. Ritz et al. reported a negative association between entire pregnancy CO exposure and preterm birth (0.59–0.91 ppm carbon monoxide: OR = 0.76, 95%CI: 0.62–0.97) [20]. Furthermore, existing research indicates that the inhalation of CO at a concentration of 125 ppm for 2 h per day over 4 days did not exceed a 4.5% increase in carboxyhemoglobin (CO-Hb) level [21]. The adverse effects associated with CO exposure are typically observed only when the CO-Hb level reaches approximately 20%. Furthermore, it has been found that expectant mothers exposed to ambient CO levels independently exhibit a decreased risk of developing pre-eclampsia. Several studies suggest that the underlying biological mechanism through which low concentrations of CO protective effects against preterm birth [22]. Olgun NS et al. reported that ET-1 is associated with preterm birth [23]. Peltier MR et al. found that the introduction of a low, non-toxic level of 250 ppm CO can prevent the production of 1 L-1β in placental explants stimulated by bacteria, as well as TNFα in fetal membranes. Both of these substances are known to induce ET-1 [24, 25]. Other studies have also demonstrated the impact of CO on reducing the activity of the ET axis in various systems [26, 27], such as mitigating the increase in ET-1 production caused by an infection in the human placenta through the administration of low doses of CO [26].
Moreover, a threshold value of air pollutant effect is usually expected to protect population health by keeping the pollutant below this level. Higher levels of CO exposure throughout pregnancy were found to be associated with an increased likelihood of preterm and very preterm birth. For short-term effect, the log(RR) of preterm birth was 0.160 (95%CI: 0.115–0.205) at the 95th percentile of CO compared to the thresholds. For long-term effect, the hazard risk of preterm birth was 1.150 (95%CI: 1.105–1.196) at the 95th percentile of CO compared to the thresholds, while the risk of very preterm birth was 1.345 (95%CI: 1.169–1.548). This aligns with a study in Brisbane that associated increased CO concentrations above 162.5 ppb with an increased risk of preterm birth [28]. While our study reveals a protective effect of low-dose CO exposure on preterm and very preterm birth, it is essential to note that short-term exposure to CO increases the risk of preterm birth but not very preterm birth. Additionally, long-term exposure to CO further elevates the risk of preterm and very preterm birth when considering the overall CO exposure dose.
Our findings align with some previous research in confirming the acute association between CO exposure and the risk of preterm birth. Discrepancies between our study and others may arise from variations in exposure time-frame and effect estimates. For instance, a time-series study in Ningbo found that the largest excess risks (ERs) were at lag 4 for CO (ERs = 3.36, 95%CI: 0.5–6.3) [29]. In our study, preterm birth was associated with CO when exposure lagged 0–3 days and 12–21 days, while very preterm birth did not exhibit a similar pattern. Regarding the long-term impact of CO, our study establishes a correlation between CO exposure and each trimester of preterm and very preterm birth. In addition, we found the hazard risk of both preterm and very preterm increased from low-to-mean concentrations of CO, followed by a continued increase from mean-to-high concentrations (Fig. 5). However, existing literature on the relationship between CO, preterm, and very preterm birth offers mixed results. Gong et al. demonstrated that exclusive exposure to CO during the third trimester significantly increases the risk of preterm birth [30]. A prospective birth cohort study found a 15% (OR = 1.15, 95%CI: 1.11, 1.19) increase in the risk of preterm birth with 100 µg/m3 increase in CO concentration during the entire pregnancy, with the strongest effect in the second trimester for CO [17]. The results of a study in the U.S. State of Georgia suggest that there is an association between carbon monoxide (CO) exposure and preterm birth. The odds ratios for inter-quartile range increases in CO during the first, second, and third trimesters as well as throughout the entire pregnancy were found to be 1.005 (95%CI: 1.001–1.009), 1.007 (95%CI: 1.002–1.011), and 1.011 (95%CI: 1.006–1.017), respectively [31]. However, among about 3509 women delivering between 1996 and 2006, Rudra et al. found no evidence that CO influences the risk of preterm delivery in western Washington [32]. Similarly, Ju et al. reported no significant association between CO exposure and increased risk of very preterm birth (RR = 0.930, 95%CI: 0.847–1.022) [33].
Our findings further suggest that air pollutants (PM2.5, PM10, NO2, SO2, O3) may partially increase the effect of CO exposure on the risk of both preterm and very preterm birth. The multiplicative interaction of air pollutants and CO contributes to the risk of preterm and very preterm birth. This may be attributed to air pollution, particularly PM2.5 and PM10, inducing oxidative stress and inflammation in the body, thereby augmenting the risk of CO exposure during pregnancy. The effects of CO on preterm birth appeared to be stronger for older women in the first trimester. To further evaluate the impact of CO exposure throughout pregnancy, subgroup analysis by maternal age should be conducted.
Despite offering new insights into the short-term and long-term effects of CO on preterm and very preterm birth, our study has several limitations. Firstly, due to data unavailability, we are unable to account for more detailed demographic information (e.g., family income, occupation and education level) [16, 34] and other behavioral risk factors related to preterm and very preterm birth outcomes (e.g., parental smoking, diet habits) [35]. We didn’t use multiple exposure methods to analyze the effects of CO and other air pollutants exposure on preterm birth. However, the population-based nature of our study minimizes participant selection bias, and the large population and extended study period enhance the accuracy of the estimated impact. Secondly, the presence of indoor air pollution resulting from cooking practices and traditional heating methods in rural regions could potentially emerge as a noteworthy environmental element [36]. Moreover, CO concentrations were measured based on monitor station rather than individual exposure, and we were unable to accurately calculate the exposure of pregnant women to activity trajectories, work, etc. Nevertheless, we employed the inverse distance weighting technique to estimate the various long-term exposure periods for each pregnant woman based on registered addresses. This encompassed different time intervals and the cumulative average concentration of CO throughout the follow-up duration.
Conclusion
In summary, our findings suggest that short-term exposure to low levels of CO may have protective effects against preterm birth, while long-term exposure to low concentrations of CO may reduce the risk of both preterm and very preterm birth. Moreover, our study provides evidence indicating that very preterm birth is more susceptible to the influence of long-term exposure to CO during pregnancy, with acute CO exposure exhibiting a greater impact on preterm birth. Despite the comprehensive nature of our large population-based study, the assertion regarding the protective effect of low-dose CO exposure on preterm and very preterm birth necessitates careful consideration. Further investigations into the underlying biological mechanisms are imperative to substantiate this conclusion. It is imperative for pregnant women to minimize exposure to ambient air pollutants.
Data availability
The data sets generated and analysed during the current study are not publicly available due property rights protection but are available from the correspinding author on resonable request.
References
WHO. Recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta Obstet Gynecol Scand. 1977;56(3):247–53.
Walani SR. Global burden of preterm birth. Int J Gynaecol Obstet. 2020;150(1):31–3.
Larroque B, Ancel PY, Marret S, Marchand L, Andre M, Arnaud C, Pierrat V, Roze JC, Messer J, Thiriez G, et al. Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): a longitudinal cohort study. Lancet. 2008;371(9615):813–20.
Ancel PY, Goffinet F, Group E-W, Kuhn P, Langer B, Matis J, Hernandorena X, Chabanier P, Joly-Pedespan L, Lecomte B, et al. Survival and morbidity of preterm children born at 22 through 34 weeks’ gestation in France in 2011: results of the EPIPAGE-2 cohort study. JAMA Pediatr. 2015;169(3):230–8.
Wu Y, Ye H, Yuan Y, Kong C, Jing W, Liu J, Liu M. Association between season of conception, month of conception with preterm birth in China: a population-based retrospective cohort study. Reprod Health. 2023;20(1):88.
Liu J, Zhang S, Liu M, Wang Q, Shen H, Zhang Y. Maternal pre-pregnancy infection with hepatitis B virus and the risk of preterm birth: a population-based cohort study. Lancet Glob Health. 2017;5(6):e624–32.
Bretelle F, Loubiere S, Desbriere R, Loundou A, Blanc J, Heckenroth H, Schmitz T, Benachi A, Haddad B, Mauviel F et al. Effectiveness and costs of molecular screening and Treatment for Bacterial Vaginosis to prevent Preterm Birth: the AuTop Randomized Clinical Trial. JAMA Pediatr 2023.
Collaborators GBDRF. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1923–94.
Zhou W, Ming X, Yang Y, Hu Y, He Z, Chen H, Li Y, Cheng J, Zhou X. Associations between maternal exposure to ambient air pollution and very low birth weight: a birth cohort study in Chongqing, China. Front Public Health. 2023;11:1123594.
Ming X, He Z, Li Y, Hu Y, Yang Y, Chen H, Chen Q, Yang H, Zhou W. The short-term effects of air pollution exposure on preterm births in Chongqing, China: 2015–2020. Environ Sci Pollut Res Int. 2023;30(18):51679–91.
Zhou W, Ming X, Yang Y, Hu Y, He Z, Chen H, Li Y, Zhou X, Yin P. Association between maternal exposure to Ambient Air Pollution and the risk of Preterm Birth: a birth cohort study in Chongqing, China, 2015–2020. Int J Environ Res Public Health 2022, 19(4).
Zhou W, Ming X, Chen Q, Liu X, Yin P. The acute effect and lag effect analysis between exposures to ambient air pollutants and spontaneous abortion: a case-crossover study in China, 2017–2019. Environ Sci Pollut Res Int. 2022;29(44):67380–9.
Zhang Y, Ye T, Yu P, Xu R, Chen G, Yu W, Song J, Guo Y, Li S. Preterm birth and term low birth weight associated with wildfire-specific PM(2.5): a cohort study in New South Wales, Australia during 2016–2019. Environ Int. 2023;174:107879.
Zhang H, Zhang X, Feng D, Gao Z, Gong Y, Zhang J, Song S, Yu Z, Huang C. Interaction effects of night-time temperature and PM(2.5) on preterm birth in Huai River Basin, China. Environ Int. 2023;171:107729.
Qiu Z, Li W, Qiu Y, Chen Z, Yang F, Xu W, Gao Y, Liu Z, Li Q, Jiang M, et al. Third trimester as the susceptibility window for maternal PM(2.5) exposure and preterm birth: a nationwide surveillance-based association study in China. Sci Total Environ. 2023;880:163274.
Liu XX, Fan SJ, Luo YN, Hu LX, Li CC, Zhang YD, Li JX, Qiu HL, Dong GH, Yang BY. Global, regional, and national burden of preterm birth attributable to ambient and household PM(2.5) from 1990 to 2019: worsening or improving? Sci Total Environ. 2023;871:161975.
Qian Z, Liang S, Yang S, Trevathan E, Huang Z, Yang R, Wang J, Hu K, Zhang Y, Vaughn M, et al. Ambient air pollution and preterm birth: a prospective birth cohort study in Wuhan, China. Int J Hyg Environ Health. 2016;219(2):195–203.
Ritz B, Yu F, Chapa G, Fruin S. Effect of air pollution on preterm birth among children born in Southern California between 1989 and 1993. Epidemiology. 2000;11(5):502–11.
Warren JL, Kong W, Luben TJ, Chang HH. Critical window variable selection: estimating the impact of air pollution on very preterm birth. Biostatistics. 2020;21(4):790–806.
Ritz B, Wilhelm M, Hoggatt KJ, Ghosh JK. Ambient air pollution and preterm birth in the environment and pregnancy outcomes study at the University of California, Los Angeles. Am J Epidemiol. 2007;166(9):1045–52.
Bathoorn E, Slebos DJ, Postma DS, Koeter GH, van Oosterhout AJ, van der Toorn M, Boezen HM, Kerstjens HA. Anti-inflammatory effects of inhaled carbon monoxide in patients with COPD: a pilot study. Eur Respir J. 2007;30(6):1131–7.
Zhai D, Guo Y, Smith G, Krewski D, Walker M, Wen SW. Maternal exposure to moderate ambient carbon monoxide is associated with decreased risk of preeclampsia. Am J Obstet Gynecol 2012, 207(1):57 e51-59.
Olgun NS, Patel HJ, Stephani R, Lengyel I, Reznik SE. Blockade of endothelin-1 with a novel series of 1,3,6-trisubstituted-2-carboxy-quinol-4-ones controls infection-associated preterm birth. Am J Pathol. 2010;177(4):1929–35.
Wort SJ, Ito M, Chou PC, Mc Master SK, Badiger R, Jazrawi E, de Souza P, Evans TW, Mitchell JA, Pinhu L, et al. Synergistic induction of endothelin-1 by tumor necrosis factor alpha and interferon gamma is due to enhanced NF-kappaB binding and histone acetylation at specific kappaB sites. J Biol Chem. 2009;284(36):24297–305.
Kotani T, Iwase A, Tsuda H, Mano Y, Yamamoto E, Nakano T, Hasegawa Y, Li H, Sumigama S, Itakura A, et al. Altered expression of enzymes regulating the activity of endothelin-1 in the lower segment of the human amnion during labor. Biol Reprod. 2013;89(3):52.
Olgun NS, Arita Y, Hanna M, Murthy A, Tristan S, Peltier MR, Hanna N. Carbon monoxide attenuates bacteria-induced Endothelin-1 expression in second trimester placental explants. Placenta. 2014;35(6):351–8.
Stanford SJ, Walters MJ, Mitchell JA. Carbon monoxide inhibits endothelin-1 release by human pulmonary artery smooth muscle cells. Eur J Pharmacol. 2004;486(3):349–52.
Li S, Guo Y, Williams G. Acute Impact of Hourly Ambient Air Pollution on Preterm Birth. Environ Health Perspect. 2016;124(10):1623–9.
Liu WY, Yu ZB, Qiu HY, Wang JB, Chen XY, Chen K. Association between ambient air pollutants and preterm birth in Ningbo, China: a time-series study. BMC Pediatr. 2018;18(1):305.
Gong Y, Sun P, Fu X, Jiang L, Yang M, Zhang J, Li Q, Chai J, He Y, Shi C et al. The type of previous abortion modifies the association between air pollution and the risk of preterm birth. Environ Res 2022, 212(Pt A):113166.
Hao H, Chang HH, Holmes HA, Mulholland JA, Klein M, Darrow LA, Strickland MJ. Air Pollution and Preterm Birth in the U.S. state of Georgia (2002–2006): associations with concentrations of 11 Ambient Air pollutants estimated by combining Community Multiscale Air Quality Model (CMAQ) simulations with stationary monitor measurements. Environ Health Perspect. 2016;124(6):875–80.
Rudra CB, Williams MA, Sheppard L, Koenig JQ, Schiff MA. Ambient carbon monoxide and fine particulate matter in relation to preeclampsia and preterm delivery in western Washington State. Environ Health Perspect. 2011;119(6):886–92.
Ju L, Li C, Yang M, Sun S, Zhang Q, Cao J, Ding R. Maternal air pollution exposure increases the risk of preterm birth: evidence from the meta-analysis of cohort studies. Environ Res. 2021;202:111654.
Liu Y, Xu J, Chen D, Sun P, Ma X. The association between air pollution and preterm birth and low birth weight in Guangdong, China. BMC Public Health. 2019;19(1):3.
Jardel H, Martin CL, Hoyo C, Rappazzo KM. Interplay of gestational parent exposure to ambient air pollution and diet characteristics on preterm birth. BMC Public Health. 2023;23(1):822.
Zhou G, Wu J, Yang M, Sun P, Gong Y, Chai J, Zhang J, Afrim FK, Dong W, Sun R, et al. Prenatal exposure to air pollution and the risk of preterm birth in rural population of Henan Province. Chemosphere. 2022;286(Pt 2):131833.
Acknowledgements
Not Applicable.
Funding
This study was supported by the Chongqing Science and Technology Commission Project [grant number: cstc2018jscx-mszdX0021] and the Chongqing Research Center for Prevention & Control of Maternal and Child Diseases and Public Health [CQFYSJ01003].
Author information
Authors and Affiliations
Contributions
Xin Ming: Formal analysis, Writing-original draft. Wenzheng Zhou: Conceptualization, Methodology, Writing-review & editing; Founding acquisition. Jin Cheng: Methodology, Writing-review & editing; Yunping Yang: Data curation, Supervision. Yannan Li: Data curation, software. Ziyi He: Conceptualization, Data curation. Xiaoqin Tian: Data curation, methodology. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The research protocol was approved by the Institutional Ethical Committee Board of the Chongqing Health Center for Women and Children. All daily surveillance data were aggregated at the city level, not linked to any person ally identifying data, such as participant name, identity information, address, or telephone number. This study only reviewed secondary aggregated data and analyzed them at the aggregate level. thus, a waiver of written informed consent was taken by the Institutional Ethical Committee Board of the Chongqing Health Center for Women and Children.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ming, X., Yang, Y., Li, Y. et al. Association between risk of preterm birth and long-term and short-term exposure to ambient carbon monoxide during pregnancy in chongqing, China: a study from 2016-2020. BMC Public Health 24, 1411 (2024). https://doi.org/10.1186/s12889-024-18913-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18913-z