Abstract
Accumulating evidence suggested that the risk of preterm births (PTBs) following prenatal exposure to air pollution was inconclusive. The aim of this study is to investigate the relationship between air pollution exposure in the days before delivery and PTB and assess the threshold effect of short-term prenatal exposure to air pollution on PTB. This study collected data including meteorological factors, air pollutants, and information in Birth Certificate System from 9 districts during 2015–2020 in Chongqing, China. Generalized additive models (GAMs) with the distributed lag non-linear models were conducted to assess the acute impact of air pollutants on the daily counts of PTB, after controlling for potential confounding factors. We observed that PM2.5 was related to increased occurrence of PTB on lag 0–3 and lag 10–21 days, with the strongest on the first day (RR = 1.017, 95%CI: 1.000–1.034) and then decreasing. The thresholds of PM2.5 for lag 1–7 and 1–30 days were 100 μg/m3 and 50 μg/m3, respectively. The lag effect of PM10 on PTB was very similar to that of PM2.5. In addition, the lagged and cumulative exposure of SO2 and NO2 was also associated with the increased risk of PTB. The lag relative risk and cumulative relative risk of CO exposure were the strongest, with a maximum RR at lag 0 (RR = 1.044, 95%CI: 1.018, 1.069). Importantly, the exposure–response curve of CO showed that RR increased rapidly when the concentration exceeded 1000 μg/m3. This study indicated significant associations between air pollution and PTB. The relative risk decreases with day lag, while the cumulative effect increases. Thus, pregnant women should understand the risk of air pollution and try to avoid high concentration exposure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preterm birth (PTB) is a serious complication of pregnancy and is used as a predictor of neonatal mortality (Rocha et al. 2022). Due to the imperfect development of various body systems, premature infants are prone to severe multiple systems diseases, and high mortality and disability (Hamilton et al. 2015; McCormick et al. 2011). In the past 20 years, the incidence of PTB is increasing worldwide, making PTB a global problem in public health. According to the reports, more than one in ten babies are born prematurely each year worldwide. In China, the PTB rate ranges from 5% to 15%, the second highest in the world, with more than 1.17 million premature babies born each year (Lim et al. 2012; Zhao et al. 2015).
Previous epidemiologic researches have suggested that PTB is the outcome of the combined action of multiple factors, such as life behavior, psychological behavior, and genetic factors (Falah et al. 2013). Although there is such a growing body of studies assessing the influence of air pollutant exposure on PTB, some of these studies only focus on a certain single pollutant or use a sample size of PTB that is relatively limited. Further still, the results of the correlation between air pollution and PTB are inconsistent and not suitable to directly extrapolate them to areas with higher levels of air pollution. Moreover, the environmental air pollution components and concentrations in these studies have also varied (Li et al. 2021a, 2021b; Siddika et al. 2020; Smith et al. 2020; Warren et al. 2020). In summary, therefore, in rapidly developing countries with high concentrations of air pollutants, extremely high levels of air pollutants may increase the risk of PTB (Li et al. 2018; Qian et al. 2016).
However, the research on acute effects and analysis of air pollutants exposure on PTB has been less reported. It has also been hypothesized that the short-term relationship between PTB and air pollutants might relatively difficult to detect because of the seasonal character of PTB rates (Darrow et al. 2009; Stieb et al. 2019).
The goal of this paper, therefore, was to assess the influence of acute maternal exposure to air pollution on PTB in Chongqing, China, for the years 2015–2020. It is also meaningful to explore the thresholds for the risk of PTB due to short-term prenatal air pollution exposure, and thereby improve the understanding of PTB prevention overall.
Material and methods
Study area
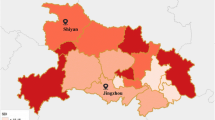
This study was conducted in Chongqing, China, using 6-year daily data from a retrospective cohort study with multicenter. Chongqing has an area of 82,400 km2 and is located between 105°11′ N and 28°11′ E. It is an iron, petrochemical and aluminum industrial center in the southwest of China. Chongqing is known as the “Fog City” because of its special basin topography and meteorological conditions that impede the diffusion of ambient air pollutants. According to data gathered from the Chongqing Municipal Bureau of Statistics in 2020, Chongqing has a total population of 32.05 million. Its urban population accounts for 65.9% of that total, which ensures the stability of the population characteristics in this research effort. The main urban area had closely connected districts: Yuzhong, Jiangbei, Dadukou, Shapingba, Jiulongpo, Nanan, Beibei, Yubei, and Banan.
Data collection
In this study, we obtained the birth outcome data from the Chongqing Birth Certificate System, collected between 2015 and 2020. The birth certificate data includes the child’s date of birth, permanent address, gestational age, etc. After childbirth, birth information of the baby is filled by health care attendants or midwives in the Neonatal Care Record System, which is then would be verified logically and specifically and uploaded to the information system. Before the birth certificate is issued, the parents and the Healthcare Commission confirm the information. We excluded those data that lacked gestational age and non-urban residents. Our analyses were based on 59,8018 births after exclusions, and a total of 35,044 premature babies were included. PTB was defined as a birth with less than 37 weeks of gestational (Blencowe et al. 2012; Warren et al. 2020). The birth certificate data was used to evaluate the number of PTB babies in Chongqing during the designated research period.
Exposure assessment
During the study period, ambient air pollutant concentrations were obtained from the Chinese National Urban Air Quality Monitoring Platform (http://zhb.gov.cn) for 17 ground-based monitoring stations in Chongqing. We calculated the 24-h average particles with a diameter < 2.5 and < 10 μm (PM2.5, PM10), nitrogen dioxide (NO2), sulfur dioxide (SO2), and carbon monoxide (CO); ozone (O3) was an 8 h maximum value concentration. For each day, we averaged the data from the available monitors to compute mean values for the whole city. Daily average relative humidity and temperature were available from the China Greenhouse Data Sharing Platform (http://data.sheshiyuanyi.com). Imputation of missing data was done using multiple linear interpolation based on other monitors’ values.
Statistical analysis
We used a quasi-Poisson GAM with the distributed lag non-linear models (DLNMs) to estimate associations of daily new case of PTB with air pollution exposure. The model was the following:
where \(t\) as the observation day, the outcome \(E\left({Y}_{t}\right)\) refers to the observed daily PTB counts. \(\propto\) is the intercept, \({Pollution}_{t}\) represents the pollutant concentration on day \(t\), \({Temp}_{t}\) represents the temperature, \({RH}_{t}\) represents the relative humidity; \({Time}_{t}\) is time trend. \(cb\left({Temp}_{t},lag\right)\), \(cb\left({RH}_{t},lag\right)\) and \(cb\left({Pollution}_{t},lag\right)\) indicates the matrix of temperature, relative humidity and air pollutants, respectively. Then, we use the DLNMs by the definition of a “cross-basis” function, a two dimensional function space expresing the influence of the predictor range and in its lag dimention. ns() denotes a natural cubic smooth spline function that removes unmeasured long-term and seasonal trend from the time series data set. \({DOW}_{t}\) represent the day of week; \({holiday}_{t}\) represent dummy variable (0 indicates non-holiday, and 1 indicates a holiday).
The maximum lag day was determined according to the Akaike information criterion for quasi-likelihood models (QAIC). The formula of QAIC was shown as follows:
where \(c\) is the variance expansion factor, \(L\) is the likelihood function, and k is the formula parameters. In fact, the longer the lag time, the smaller QAIC would be, and too long a lag time might create a large bias. Therefore, we selected the maximum lag day up to 30 days according to the local minimum QAIC. Sensitivity analyses were made by changing the degree of freedom (df) for time (6–8 df/year). Finally, we selected the df of the natural cubic smooth splines of time were 7 per year in all the models. We assessmented relative risk (RR) and cumulative relative risk (CRR) for each ambient air pollutant in relation to preterm birth after an adjustment for two meteorological factors: daily mean value of temperature and relative humidity.
We used Microsoft Excel software and ArcGIS software 10.0 to organize and establish the dataset; the DLNM was employed by using the package dlnm Version 2.3.6 within R 4.0.1 software (Vienna, Australia).
Results
Baseline characteristics
Table 1 shows the daily descriptive results. During this time, the total number of births was 598,018, and there were 35,044 premature births. The daily new case of premature births was 16, ranging from 1 to a maximum of 48. Average concentration of PM2.5, PM10, SO2, NO2, O3, and CO in the six years was 42.44 μg/m3, 66.37 μg/m3, 10.21 μg/m3, 39.99 μg/m3, 39.75 μg/m3, and 916.08 μg/m3, respectively. The mean concentration of daily relative humidity and temperature was 75.12% and 19.92 °C, respectively.
The number of PTB and mean concentration of air pollutants fluctuated with months and weeks. Except for O3, the average monthly concentration of air pollutants varied obviously with season, with low concentrations in summer and high concentrations in winter. What is more, the preterm birth also occurred more often in winter and less so in summer. To be specific, O3 peaked in the summer (Fig. 1, Supplementary Fig. 1).
Spearman correlation
Table 2 depicts the correlation coefficient (r) between meteorological factors and air pollutants. The majority of the air pollutants (PM2.5, PM10, SO2, NO2, and CO) were positively and strongly correlated to others. The correlation between PM2.5 and PM10 was very close (r = 0.96). O3 was weekly and negatively correlated to other pollutants with r range from − 0.15 to − 0.51. Moreover, correlations were observed negative, moderate and significant between meteorological factors and air pollutants.
Associations between air pollutant exposure and PTB
Figure 2 shows exposure-lag-response surfaces as RR describing the non-linear relationship between premature births and air pollutants along 30 lag days. The lag days is represented by one bottom edge of the cube, and the air pollution is represented by the other bottom edge. The height of the cube represents the RR of PTB.
Figure 3 demonstrates the RR and 95% CI of PTB with every 10 μg/m3 increase of each air pollutant in single-day (lag 0–30). The curve confirms a positive correlation between PM2.5 and PTB on lag 0–3 and lag 10–21 days, and the strongest influence in PTB associated with a 10 μg/m3 increase was at lag 0 (RR = 1.017, 95%CI: 1.000–1.034). The lag response curve of PM10 was similar to that of PM2.5, and the significant effect for PM10 on PTB was observed on lag 0–4 and lag 10–22 days. An obviously positive correlation between premature birth and maternal exposure with per 10 μg/m3 increase of SO2 was observed on lag 1–11 and lag 16–17 days. For NO2, an increased risk of PTB was observed on lag 0–3 and lag 16–27 days and peaking at the lag day 23 (RR = 1.017, 95%CI: 1.007–1.027).
O3 had a negative correlation with the risk of PTB between 0 and 4 days. Short-term exposure to CO did increase the risk of PTB, and the maximum RR values of CO with a 100 μg/m3 increment was found at lag 0 (RR = 1.044, 95%CI: 1.018–1.069) and then fell gradually. By lag day 23, the effect of CO was no longer present (see Table 1 of Supplementary Information).
Figure 4 shows the overall CRR of air pollutants exposure and PTB with a lag of 1–3 days, 1–7 days, and 1–30 days. Analysis of the relationship revealed that the overall cumulative relative risk (CRR) of PTB had an approximately J-shape with PM2.5 and PM10. The cumulative relative risk of PM2.5 over 100 μg/m3 (CRR = 1.058, 95% CI: 1.000–1.120) from lag 1–7 and over 50 μg/m3 (CRR = 1.021, 95%CI: 1.006–1.036) from 1 to 30 was statistically significant. Similarly, the cumulative relative risk of PM10 over 70 μg/m3 (CRR = 1.010, 95%CI: 1.003–1.016) from lag 1–30 was significant. The highest risk of SO2 from lag 1–3 days was at 20 μg/m3 (CRR = 1.069, 95% CI: 1.023–1.117) during 15–25 μg/m3. The cumulative relative risk of SO2 over 15 μg/m3 from lag 1–7 (CRR = 1.074, 95% CI: 1.035–1.115) and lag 1–30 (CRR = 1.252, 95% CI: 1.174–1.335) were statistically significant. The 1–30 days cumulative relative risk effect of NO2 was statistically significant at a concentration above 45 μg/m3. Notably, the overall cumulative relative risk of O3 was a U-shape. When the concentration was lower than 30 μg/m3 or higher than 80 μg/m3, the CRR value was statistically significant, and the concentration between 40 and 70 μg/m3 negatively correlated with PTB. The cumulative relative risk effect of CO exposure showed that CRR increased significantly after 1000 μg/m3, with significant statistical significance in lag for 1–3 days, 1–7 days, and 1–30 days (Table 3).
Exposure–response curves for the effect of air pollutants on daily counts of PTB at 1–3, 1–7, and 1–30 lag days. X-axis: the concentration of each air pollutant; y-axis: the relative risk of air pollution on PTB. Reference value: PM2.5 at 42.44 μg/m3; PM10 at 66.37 μg/m3; SO2 at 10.21 μg/m3; NO2 at 39.99 μg/m3; O3 at 39.75 μg/m3; CO at 916.08 μg/m.3
Discussion
This study suggested that the daily exposures to PM2.5, PM10, SO2, CO, and NO2 and during pregnancy were positively correlated with the increased risk of PTB after adjusting for mean relative humidity and temperature at lag 0–30 days. At the time of this study, both the levels of PM2.5 and PM10 were exceeded the first-level of National Air Quality Standards (NAQS) values (PM2.5: 35 μg/m3; PM10: 50 μg/m3). That means the particulate matter pollution was quite severe in Chongqing, China. Furthermore, compared with developed countries, China had a longer particulate matter exposure duration and a higher magnitude (Guan et al. 2016; Sun et al. 2021). The levels of CO, O3, NO2, and SO2 were below the primary standard (CO: 4000 μg/m3; O3: 100 μg/m3; NO2: 80 μg/m3; SO2: 50 μg/m3) in the NAQS. As far as we know, this is the first study to assess the impact of short-term air pollutants exposure on PTB with such a pollution level in Chongqing.
Previous researches suggested that the risk of preterm births (PTBs) following prenatal exposure to air pollution was inconclusive. Huang et al. found that an interquartile range increases in NO2, SO2 and O3 were related with 0.46% (95%CI: − 0.25 ~ 1.23), 0.37% (95%CI: − 1.77 ~ 2.57) and 2.09% (95%CI: − 8.00 ~ 13.29) increase risk for PTB at lag 2, respectively (Huang et al. 2020). One large study in Changsha, China, covering 78 midwifery institutions and 344,880 live births, reported that NO2 was associated with PTBs on lag 0–2, lag 4, and lag 5 (Xiong et al. 2019). In another study, Lee et al. suggested that cumulative exposure to O3 and PM10 from 0 to 6 days before birth was not associated with the risk of PTBs (Lee et al. 2008). The threshold for the impact of air pollution is generally expected to protect people’s health by controlling pollutants below this concentration (Li et al. 2016). Fleischer et al. reported that the possible threshold effect of PM2.5 on PTB is 36.5 mg/m3 (Fleischer et al. 2014). DeFranco et al. observed that maternal exposure to high concentrations of PM2.5 in excess of 15 μg/m3 was associated with PTB significantly (DeFranco et al. 2016). A Spanish study observed that perinatal exposure to a certain high concentration of traffic-related air pollution (such as NO2 > 46.2 mg/m3) was associated with PTB (Llop et al. 2010). While, the results of a Beijing research suggested that there was a correlation between pollutants and preterm birth, but with no evidence of a threshold (Guan et al. 2019).
In this paper, short-term air pollution exposure was significantly associated with a higher risk of PTB in few days before birth. For a 10 μg/m3 increment in PM2.5 concentration, the strongest effect on PTB was on lag 0 day (RR = 1.017, 95%CI: 1.000–1.014), which was higher than in Xuzhou and Beijing (Guan et al. 2019; Li et al. 2021b). Similarly, exposure to PM10 can also acutely affect PTB. Moreover, Leem et al. observed that exposure to SO2 in the last trimester of maternal with percutaneous transluminal dilatation (PTD) was statistically significant (Leem et al. 2006). Moreover, our results showed that exposure to SO2 positively correlated with premature birth, and SO2 has a long effect of 20 days. There was a positive correlation between PTB and NO2 on lag 0–3 and 16–27 days, and peaking on the 23th day. In contrast, Ji et al. suggested that the relationship between PTB and NO2 exposure was not significant during the first and second trimesters, compared to significant correlations in the last week and last month before labor (Ji et al. 2019). We found the highest risk for PTB occurred with CO in the short term, and the relative risk value was highest at lag 0 (RR = 1.119, 95%CI: 1.049–1.194). The proposed mechanism of action related to tissue oxygenation, especially CO binding to fetal hemoglobin to reduce the availability of oxygen. The unexpected negative relationship between O3 and PTB was found between the 0–4 lag days. This may be interpreted by the inverse association between O3 and other assessed air pollutants (Nobles et al. 2019; Reynolds et al. 2019). Conversely, some studies found that O3 and CO were not associated with PTB (Guan et al. 2019; Liu et al. 2019). Interestingly, we observed that although the relative risk of PM2.5, PM10, NO2, SO2, and CO fluctuated with lag days, and the overall relative risk did show a downward trend.
This current study indicates that the cumulative relative risk of air pollutants increases with the increase of lag days, with evidence of a threshold. The cumulative relative risk of PM2.5 and PM10 exposure lags 1–7 days and 1–30 days, showing that the effect was strong after 50 μg/m3. In Huang’s analysis, when air pollution level was high in terms of PM2.5 (75 μg/m3), the risk of PTB was higher, and the curve presented as a rapid growth (Huang et al. 2020). The cumulative relative risk of SO2 over 15 μg/m3 from lag 1–7 and lag 1–30 was statistically significant. Moreover, in Li’s study, the curve of SO2 was similar to that in our analysis, but the relationships between PM10 and PM2.5 were not significant (Li et al. 2016). Increased concentrations of NO2 above 45 μg/m3 were positively associated with an increased risk of PTB in this paper. However, Llop’s study suggested that exposure to NO2 above 46.2 mg/m3 was associated with PTB (Llop et al. 2010). Our analysis found that the associations between O3 and PTB were generally U-shaped. That is, a threshold effect of O3 was indicated. Exposure to CO has the strongest effect on the occurrence of PTB, and the cumulative relative effect increases greatly after CO level over 1000 μg/m3, whether there is a lag of 1–3 days or 1–7 days or 1–30 days. In addition, we found the overall accumulative relative curves relatively flattened out at low levels and were steep at higher levels, which is inconsistent with the results in previous researches (Giorgis-Allemand et al. 2017; Guan et al. 2019; Pope et al. 2009). However, it is worth mentioning that we should be cautious about this result because high levels of air pollution are rarely observed.
Associations between air pollutants short-term exposures and risk for PTBs may indicate that air pollutants could trigger the biologic mechanism of parturition quickly, bringing out PTB in the following days. There are several potential biologic mechanisms that could support this association via a series of causes, such as inflammation, endocrine disruption, oxidative stress, blood coagulation, and hemodynamic responses (Kumar et al. 2019; Li et al. 2008; Pope et al. 2004; Slama et al. 2008). Air pollutants can translocate to the placenta through villous tissue and thus lead to preterm premature rupture of membranes (PPROM) (Bove et al. 2019; Li et al. 2021a). Simultaneously, when air pollutants are inhaled, cytokines trigger oxidative stress, which can cause endothelial dysfunction and the development of pregnancy preeclampsia (Yorifuji et al. 2015). In addition, trace metals and polycyclic aromatic hydrocarbons (PAHs) bound to particulate matter may create potential health risk (Ambade et al. 2022a, 2022b; Kumar et al. 2020; Vithanage et al. 2022).
There are many underlying factors responsible for the different results found from study to study. Firstly, air pollution levels in Chongqing were higher than in most literature. From 2015 to 2020, the concentrations of PM2.5 and PM10 were 42.44 μg/m3 and 66.37 μg/m3 in Chongqing, which exceeded the NAQS standard. Secondly, the social and demographic conditions of the inhabitants of each area may be diverse, such as lifestyles, disease patterns, or genetic backgrounds. Thirdly, the study period, air pollutant unit and statistical model were selected differently in the other literature.
Compared to the previous studies, when analyzing the relationship between premature birth and air pollution, our study has several advantages. We used a large sample size of nearly 600,000 total births and 35,044 premature delivery cases. This number is at least an order of magnitude more than offered in the previous research papers on this topic (Chen et al. 2021; Ji et al. 2019; Li et al. 2021b, 2019). The dataset included the total number of all eligible birth actual occurrences in study areas, covering air pollution data gathered from 17 air monitoring sites in Chongqing’s main urban area, which effectively reduced any selection bias. Moreover, the application of weekly or trimestral data had to face the fact that the effect of extreme pollution events would be underestimated, thereby averaging their effects over long time scales. Additionally, the spatial variability of exposure can be effectively reflected by the individual exposure estimation based on the detailed home address of the mother in this study.
There were some limitations to mention. First of all, we obtained the air pollution data from available monitors that may not fully represent the maternal exposure level. The measured value may overestimate the maternal exposure level because pregnant women spend most of their time indoors. Secondly, the individual risk factors, such as maternal health status and maternal age, were not adjusted because of information shortage. Future studies should include personal risk factors because of their potential changes for the correlation between PTB and air pollution (Kingsley et al. 2017). Moreover, we did not analyze the relationship between air pollutants and very preterm birth (VPTB) in this study. Some researches demonstrated that air pollution can also increase the incidence of VPTB (Guo et al. 2018; Ju et al. 2021; Wang et al. 2018). Meanwhile, we only studied the short-term effects of a single pollutant and PTBs, and the interactive effect of air pollutants also deserves further attention. Therefore, we cannot conclude whether the interactive effect of air pollutants introduced potential bias or just simply confounded effects with each other.
Conclusion
In conclusion, we found that maternal air pollution exposure had short-term and delayed effects on PTB, thereby increasing the risk of PTB. This study provides evidence from a study of a large population that reducing air pollution level to a certain threshold might greatly benefit birth outcomes. Pregnant women should be aware of the risk of air pollution and avoid exposure to high levels, if possible, especially in the last few weeks of pregnancy. This study thus has particular important public health significance for policy makers who design and implement air pollution preventive measures.
Data availability
The datasets that support the findings of this study are openly available from the corresponding author on reasonable request.
Abbreviations
- PTB:
-
Preterm birth
- PM2.5 :
-
Particulate matter 2.5
- PM10 :
-
Particulate 10
- SO2 :
-
Sulfur dioxide
- NO2 :
-
Nitrogen dioxide
- CO:
-
Carbon monoxide
- O3 :
-
Ozone
- DLNM:
-
Distributed lag non-linear models
- SD:
-
Standard deviation
- IQR:
-
Inter-quartile range
- RR:
-
Relative risk
- CRR:
-
Cumulative relative risk
- CI:
-
Confidence interval
References
Ambade B, Sethi SS, Chintalacheruvu MR. Distribution, risk assessment, and source apportionment of polycyclic aromatic hydrocarbons (PAHs) using positive matrix factorization (PMF) in urban soils of East India. Environ Geochem Health 2022a
Ambade B, Sethi SS, Kurwadkar S, Mishra P, Tripathee L (2022b) Accumulation of polycyclic aromatic hydrocarbons (PAHs) in surface sediment residues of Mahanadi River Estuary: abundance, source, and risk assessment. Mar Pollut Bull 183:114073
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R et al (2012) National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379:2162–2172
Bove H, Bongaerts E, Slenders E, Bijnens EM, Saenen ND, Gyselaers W et al (2019) Ambient black carbon particles reach the fetal side of human placenta. Nat Commun 10:3866
Chen Q, Ren Z, Liu Y, Qiu Y, Yang H, Zhou Y, et al. The association between preterm birth and ambient air pollution exposure in Shiyan, China, 2015–2017. Int J Environ Res Public Health 2021; 18
Darrow LA, Strickland MJ, Klein M, Waller LA, Flanders WD, Correa A et al (2009) Seasonality of birth and implications for temporal studies of preterm birth. Epidemiology 20:699–706
DeFranco E, Moravec W, Xu F, Hall E, Hossain M, Haynes EN et al (2016) Exposure to airborne particulate matter during pregnancy is associated with preterm birth: a population-based cohort study. Environ Health 15:6
Falah N, McElroy J, Snegovskikh V, Lockwood CJ, Norwitz E, Murray JC et al (2013) Investigation of genetic risk factors for chronic adult diseases for association with preterm birth. Hum Genet 132:57–67
Fleischer NL, Merialdi M, van Donkelaar A, Vadillo-Ortega F, Martin RV, Betran AP et al (2014) Outdoor air pollution, preterm birth, and low birth weight: analysis of the world health organization global survey on maternal and perinatal health. Environ Health Perspect 122:425–430
Giorgis-Allemand L, Pedersen M, Bernard C, Aguilera I, Beelen RM, Chatzi L et al (2017) The influence of meteorological factors and atmospheric pollutants on the risk of preterm birth. Am J Epidemiol 185:247–258
Guan T, Xue T, Gao S, Hu M, Liu X, Qiu X et al (2019) Acute and chronic effects of ambient fine particulate matter on preterm births in Beijing, China: a time-series model. Sci Total Environ 650:1671–1677
Guan WJ, Zheng XY, Chung KF, Zhong NS (2016) Impact of air pollution on the burden of chronic respiratory diseases in China: time for urgent action. Lancet 388:1939–1951
Guo T, Wang Y, Zhang H, Zhang Y, Zhao J, Wang Q, et al. The association between ambient PM2.5 exposure and the risk of preterm birth in China: A retrospective cohort study. Sci Total Environ 2018; 633: 1453–1459
Hamilton BE, Martin JA, Osterman MJ, Curtin SC, Matthews TJ (2015) Births: Final Data for 2014. Natl Vital Stat Rep 64:1–64
Huang S, Lin D, Huang Z, Yang L, Ding X, Chen Q (2020) Acute effects of exposure to ambient air pollutants on preterm birth in Xiamen City (2015–2018) China. ACS Omega 5:7462–7467
Ji X, Meng X, Liu C, Chen R, Ge Y, Kan L et al (2019) Nitrogen dioxide air pollution and preterm birth in Shanghai China. Environ Res 169:79–85
Ju L, Li C, Yang M, Sun S, Zhang Q, Cao J et al (2021) Maternal air pollution exposure increases the risk of preterm birth: Evidence from the meta-analysis of cohort studies. Environ Res 202:111654
Kingsley SL, Eliot MN, Glazer K, Awad YA, Schwartz JD, Savitz DA et al (2017) Maternal ambient air pollution, preterm birth and markers of fetal growth in Rhode Island: results of a hospital-based linkage study. J Epidemiol Community Health 71:1131–1136
Kumar A, Ambade B, Sankar TK, Sethi SS, Kurwadkar SJSC, Society. Source identification and health risk assessment of atmospheric PM2.5-bound polycyclic aromatic hydrocarbons in Jamshedpur, India. Sustainable Cities and Society 2019; 52: 101801
Kumar A, Sankar TK, Sethi SS, Ambade B (2020) Characteristics, toxicity, source identification and seasonal variation of atmospheric polycyclic aromatic hydrocarbons over East India. Environ Sci Pollut Res Int 27:678–690
Lee SJ, Hajat S, Steer PJ, Filippi V (2008) A time-series analysis of any short-term effects of meteorological and air pollution factors on preterm births in London UK. Environ Res 106:185–194
Leem JH, Kaplan BM, Shim YK, Pohl HR, Gotway CA, Bullard SM et al (2006) Exposures to air pollutants during pregnancy and preterm delivery. Environ Health Perspect 114:905–910
Li C, Xu JJ, He YC, Chen L, Dennis CL, Huang HF et al (2021a) Effects of acute ambient pollution exposure on preterm prelabor rupture of membranes: A time-series analysis in Shanghai. China Environ Pollut 276:116756
Li N, Xia T, Nel AE (2008) The role of oxidative stress in ambient particulate matter-induced lung diseases and its implications in the toxicity of engineered nanoparticles. Free Radic Biol Med 44:1689–1699
Li S, Guo Y, Williams G (2016) Acute impact of hourly ambient air pollution on preterm birth. Environ Health Perspect 124:1623–1629
Li S, Peng L, Wu X, Xu G, Cheng P, Hao J et al (2021b) Long-term impact of ambient air pollution on preterm birth in Xuzhou, China: a time series study. Environ Sci Pollut Res Int 28:41039–41050
Li S, Wang H, Hu H, Wu Z, Chen K, Mao Z (2019) Effect of ambient air pollution on premature SGA in Changzhou city, 2013–2016: a retrospective study. BMC Public Health 19:705
Li X, Liu Y, Liu F, Wang Y, Yang X, Yu J et al (2018) Analysis of short-term and sub-chronic effects of ambient air pollution on preterm birth in central China. Environ Sci Pollut Res Int 25:19028–19039
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2224–2260
Liu Y, Xu J, Chen D, Sun P, Ma X (2019) The association between air pollution and preterm birth and low birth weight in Guangdong China. BMC Public Health 19:3
Llop S, Ballester F, Estarlich M, Esplugues A, Rebagliato M, Iniguez C (2010) Preterm birth and exposure to air pollutants during pregnancy. Environ Res 110:778–785
McCormick MC, Litt JS, Smith VC, Zupancic JA (2011) Prematurity: an overview and public health implications. Annu Rev Public Health 32:367–379
Nobles CJ, Grantz KL, Liu D, Williams A, Ouidir M, Seeni I et al (2019) Ambient air pollution and fetal growth restriction: Physician diagnosis of fetal growth restriction versus population-based small-for-gestational age. Sci Total Environ 650:2641–2647
Pope CA 3rd, Burnett RT, Krewski D, Jerrett M, Shi Y, Calle EE et al (2009) Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation 120:941–948
Pope CA 3rd, Hansen ML, Long RW, Nielsen KR, Eatough NL, Wilson WE et al (2004) Ambient particulate air pollution, heart rate variability, and blood markers of inflammation in a panel of elderly subjects. Environ Health Perspect 112:339–345
Qian Z, Liang S, Yang S, Trevathan E, Huang Z, Yang R et al (2016) Ambient air pollution and preterm birth: a prospective birth cohort study in Wuhan China. Int J Hyg Environ Health 219:195–203
Reynolds CME, Egan B, Kennedy RA, O’Malley E, Sheehan SR, Turner MJ (2019) The implications of high carbon monoxide levels in early pregnancy for neonatal outcomes. Eur J Obstet Gynecol Reprod Biol 233:6–11
Rocha AS, de Cassia Ribeiro-Silva R, Fiaccone RL, Paixao ES, Falcao IR, Alves FJO, et al. Differences in risk factors for incident and recurrent preterm birth: a population-based linkage of 3.5 million births from the CIDACS birth cohort. BMC Med 2022; 20: 111.
Siddika N, Rantala AK, Antikainen H, Balogun H, Amegah AK, Ryti NRI et al (2020) Short-term prenatal exposure to ambient air pollution and risk of preterm birth - A population-based cohort study in Finland. Environ Res 184:109290
Slama R, Darrow L, Parker J, Woodruff TJ, Strickland M, Nieuwenhuijsen M et al (2008) Meeting report: atmospheric pollution and human reproduction. Environ Health Perspect 116:791–798
Smith RB, Beevers SD, Gulliver J, Dajnak D, Fecht D, Blangiardo M et al (2020) Impacts of air pollution and noise on risk of preterm birth and stillbirth in London. Environ Int 134:105290
Stieb DM, Lavigne E, Chen L, Pinault L, Gasparrini A, Tjepkema M (2019) Air pollution in the week prior to delivery and preterm birth in 24 Canadian cities: a time to event analysis. Environ Health 18:1
Sun S, Zhang Q, Sui X, Ding L, Liu J, Yang M et al (2021) Associations between air pollution exposure and birth defects: a time series analysis. Environ Geochem Health 43:4379–4394
Vithanage M, Bandara PC, Novo LAB, Kumar A, Ambade B, Naveendrakumar G et al (2022) Deposition of trace metals associated with atmospheric particulate matter: environmental fate and health risk assessment. Chemosphere 303:135051
Wang Q, Benmarhnia T, Zhang H, Knibbs LD, Sheridan P, Li C et al (2018) Identifying windows of susceptibility for maternal exposure to ambient air pollution and preterm birth. Environ Int 121:317–324
Warren JL, Kong W, Luben TJ, Chang HH (2020) Critical window variable selection: estimating the impact of air pollution on very preterm birth. Biostatistics 21:790–806
Xiong L, Xu Z, Tan J, Wang H, Liu Z, Wang A et al (2019) Acute effects of air pollutants on adverse birth outcomes in Changsha, China: a population data with time-series analysis from 2015 to 2017. Medicine (baltimore) 98:e14127
Yorifuji T, Naruse H, Kashima S, Murakoshi T, Doi H. Residential proximity to major roads and obstetrical complications. Sci Total Environ 2015; 508: 188–92
Zhao N, Qiu J, Zhang Y, He X, Zhou M, Li M et al (2015) Ambient air pollutant PM10 and risk of preterm birth in Lanzhou China. Environ Int 76:71–77
Funding
This work was supported by the Chongqing Science and Technology Commission Project: The Association between Exposure to Ambient Air Pollution and Premature Birth and Low Birth Weight Outcomes in Chongqing Based on Birth Cohort [grant number: cstc2020jcyj-msxmX0511] and the foundation of Chongqing Health Center for Women and Children [grant number: 2019YJMS04].
Author information
Authors and Affiliations
Contributions
XM: methodology, data curation, writing—original draft. ZH: conceptualization, data curation, validation. YL: data curation, software. YH: data curation. YY: data curation. HC: writing—review and editing. QC: supervision. HY: writing—review. WZ: conceptualization, methodology, writing—review and editing, funding acquisition.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the institutional ethical committee board of Women and Children’s Hospital of Chongqing Medical University (CQMU-WCH).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ming, X., He, Z., Li, Y. et al. The short-term effects of air pollution exposure on preterm births in Chongqing, China: 2015–2020. Environ Sci Pollut Res 30, 51679–51691 (2023). https://doi.org/10.1007/s11356-023-25624-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-25624-2