Abstract
Background
Migration to Scotland has increased since 2002 with an increase in European residents and participation in the Asylum dispersal scheme. Scotland has become more ethnically diverse, and 10% of the current population were born abroad. Migration and ethnicity are determinants of health, and information on the health status of migrants to Scotland and their access to and barriers to care facilitates the planning and delivery of equitable health services. This study aimed to scope existing peer-reviewed research and grey literature to identify gaps in evidence regarding the health of migrants in Scotland.
Methods
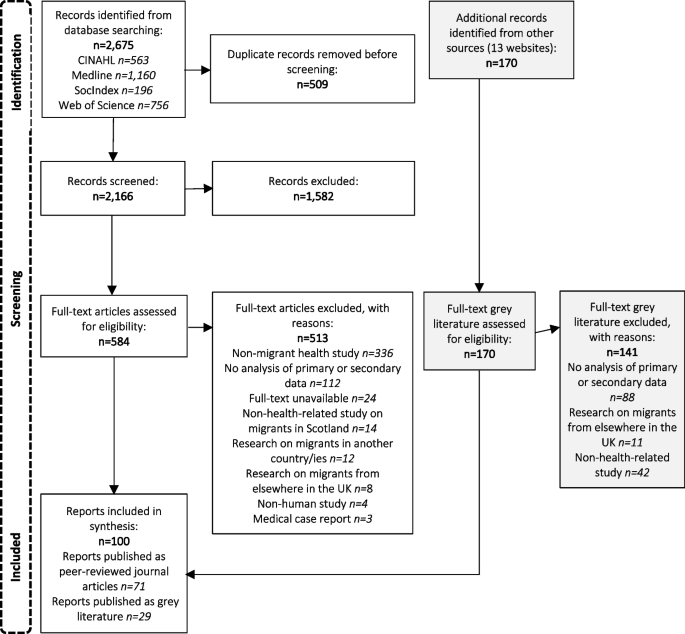
A scoping review on the health of migrants in Scotland was carried out for dates January 2002 to March 2023, inclusive of peer-reviewed journals and grey literature. CINAHL/ Web of Science/SocIndex and Medline databases were systematically searched along with government and third-sector websites. The searches identified 2166 journal articles and 170 grey literature documents for screening. Included articles were categorised according to the World Health Organisation’s 2016 Strategy and Action Plan for Refugee and Migrant Health in the European region. This approach builds on a previously published literature review on Migrant Health in the Republic of Ireland.
Results
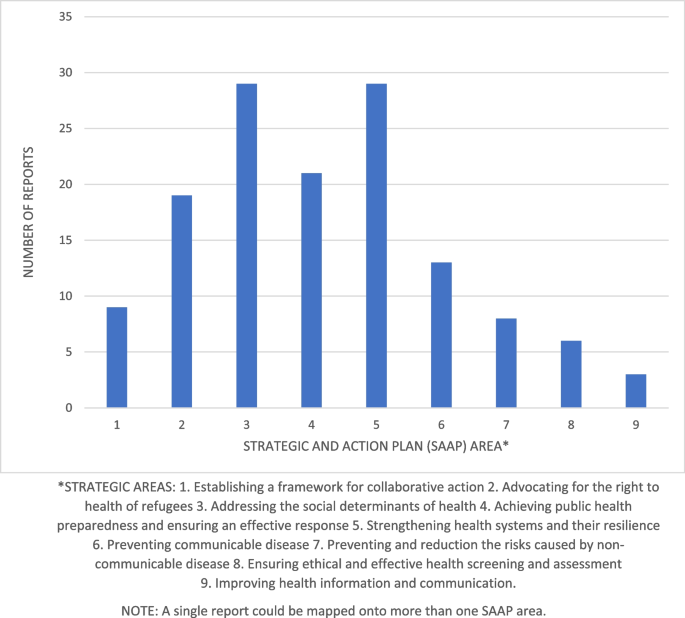
Seventy-one peer reviewed journal articles and 29 grey literature documents were included in the review. 66% were carried out from 2013 onwards and the majority focused on asylum seekers or unspecified migrant groups. Most research identified was on the World Health Organisation’s strategic areas of right to health of refugees, social determinants of health and public health planning and strengthening health systems. There were fewer studies on the strategic areas of frameworks for collaborative action, preventing communicable disease, preventing non-communicable disease, health screening and assessment and improving health information and communication.
Conclusion
While research on migrant health in Scotland has increased in recent years significant gaps remain. Future priorities should include studies of undocumented migrants, migrant workers, and additional research is required on the issue of improving health information and communication.
Similar content being viewed by others
Background
The term migrant is defined by the International Organisation for Migration as “a person who moves away from his or her place of usual residence, whether within a country or across an international border, temporarily or permanently, and for a variety of reasons. The term includes several well-defined legal categories of people, including migrant workers; persons whose particular types of movements are legally-defined, such as smuggled migrants; as well as those whose status are not specifically defined under international law, such as international students.” [1] Internationally there are an estimated 281 million migrants – 3.6% of the world population, including 26.4 million refugees and 4.1 million asylum seekers – the highest number ever recorded [2]. The UN Refugee Society defines the term refugee as “someone who has been forced to flee his or her country because of persecution, war or violence…most likely, they cannot return home or are afraid to do so.” The term asylum-seeker is defined as “someone whose request for sanctuary has yet to be processed.” [3].
Net-migration to Europe was negative in the 19th century due to higher levels of emigration, however in the mid-20th century immigration began to rise, because of an increase in migrant workers and following conflicts in the Middle East and North Africa [4]. Current migration drivers include conflicts alongside world-wide economic instability, exacerbated by the Covid-19 pandemic [5]. Environmental damage due to climate change is expected to inflate the number of asylum seekers entering Europe in future [6]. The increase in migration to Europe is not a short-term influx but a long-term phenomenon, and European nations must adapt and find solutions to resulting financial, safeguarding and health challenges [7].
Data on healthcare use by migrants in Europe is variable, which means cross-country comparisons are inadequate [8]. Many countries do not record migration information within health records and all use disparate criteria to classify migrant status. The lack of comparative data hinders public health surveillance and effective interventions [9]. Even where information is available, results can be contradictory due to the multifarious migrant population. Migrants have a wide range of origin countries, socio-economic position, age and journeys undertaken which can affect health status [10].
Migrants initially may have better health than the general population, known as the ‘Healthy Migrant effect’ [11]. However, health declines with increasing length of residence [12] and over time to levels comparable with the general population [13]. Second generation immigrants may have higher mortality than average [14]. The process of acculturation to the host country, with adoption of unhealthy lifestyle and behaviours, increases the risk for chronic disease [15]. In addition, inequalities in health of migrants compared to host populations has been confirmed by wide-ranging research [16].
Host countries may limit healthcare access, with undocumented migrants sometimes only entitled to emergency care [17]. Even when access is granted, inequitable services can affect quality of care due to language barriers and cultural factors [18]. Poor working/living conditions and discrimination can exacerbate health inequalities [12]. Processing facilities for asylum seekers are frequently overpopulated, stressful environments [19] and threat of deportation, lack of citizenship rights and integration can negatively affect health and access to care [20]. Undocumented workers are unprotected by health and safety legislation leading to dangerous working conditions and injuries [15].
A systematic review of migrant health in the European Union (EU) found migrants have worse self-perceived health than the general population [21]. Research evidence indicates increased prevalence of cardiovascular disease, diabetes, mental health disorders and adverse pregnancy outcomes. Exposure to conflict, harsh travel conditions and suboptimal vaccine programmes can mean higher risk of communicable disease [22]. Scoping reviews have also been conducted to describe trends within migration health research in the United Kingdom (UK) [23] and identify gaps for future research agendas in the UK [23] and in the Republic of Ireland [24].
Almost three-quarters (73%) of published migration health research in the UK has been conducted in England, focusing primarily on infectious diseases and mental health. There is limited evidence on the social determinants of health, access to and use of healthcare and structural and behavioural factors behaviours that influence migrant health in the UK [23]. By contrast, a large amount of the migration research conducted in the Republic of Ireland has focused on the social determinants of health, and on health system adaptations, with a paucity of research focusing on improving health information systems [24].
Migration and Health in Scotland
Immigration to Scotland began to rise in 2003 with the expansion of the EU [25]. The population in Scotland increased from 5.11 million to 5.47 million between 2005 and 2020 and is predicted to continue rising until 2028 [26] despite low birth rates, with the increased population resulting from inward migration [27]. Scotland’s population is becoming more ethnically diverse [28] and susceptibility to different health conditions varies by ethnic group, which has implications for the planning and provision of health services [29]. 7% of the current Scottish population are non-UK nationals and 10% were born outside Britain. The commonest countries of origin were Poland, Ireland, Italy, Nigeria and India [30].
Within Scotland, linking health data to ethnicity is standard in order to monitor and improve health of minority groups [31]. Ethnic background can differ from country of birth which means migration status cannot be assumed [32], although health inequalities experienced by migrants often extend to affect all ethnic minority groups [33]. The Scottish Health and Ethnicity Linkage Study (SHELS) linked census data to health records of 91% of the population which has provided information on mortality and morbidity by ethnic group and country of birth [34]. SHELS research indicates that the white-Scottish population have a higher mortality rate than other ethnic groups. This may be consequent to the comparatively poor health of the Scottish population relative to other European nations: high mortality rates in the general population may cause a perception that the health of minorities is more advantageous than in reality [35].
Cezard et al’s [13] analysis of self-perceived health among people in Scotland found that being born abroad had a positive impact on health status. Health declined with increased length of residence, which may be explained by cultural convergence with the majority population. Allik et al. [36] compared health inequalities by ethnic background and found that with increasing age, health differences reduced thus people aged over 75 of all ethnicities had similar or worse health status than White-Scottish people. While working-age migrants appear to be healthier than the White Scottish population, it cannot be assumed that in future this would extend to older age groups.
Research has shown deprivation as a cause of heath inequalities among ethnic minority and migrant groups [37]. The socio-economic status of minority ethnic groups in Scotland is unusual, as most are of similar or higher status than the white-Scottish population [38]. Therefore, public health interventions targeting deprivation may not address risk-factors for ethnic minorities and migrants [36]. Further research on determinants of health in migrants can help with planning and design of inclusive policies.
The 2011 census indicated that 50% of immigrants lived in the cities of Edinburgh, Glasgow, and Aberdeen. Glasgow had a greater percentage of non-European immigrants due to participation in the Asylum dispersal programme [39]. 10% of UK asylum seekers are placed in Glasgow, but records are not kept following approval of asylum claims, therefore the size of the refugee population is unknown [40]. While immigration is controlled by the British government, in policy areas devolved to the Scottish government, refugees and asylum seekers have more rights than elsewhere in UK, including access to primary healthcare for undocumented migrants [40]. Despite the mitigating effect of Scottish policies, asylum seekers’ health is worsened by the asylum process and associated poverty, marginalisation, and discrimination [40]. Health deteriorates with increasing length of time in the asylum system [40] and asylum seekers and refugees have additional health needs and require enhanced support [41]. Research on the health needs of asylum seekers in Scotland is required to ensure adequate healthcare.
Aim and objectives
While scoping reviews on migrant health have been carried out in Europe [12], Ireland [24] and the UK [23] none are currently specific to the Scottish context. Given the devolved government of Scotland and demographics described above, a targeted review would help to clarify research priorities, with the aim of improving health and health care within the migrant community in Scotland. This work therefore builds on the published scoping review of migrant health in the Republic of Ireland [24]. The authors recommend replication of the study in other countries to facilitate cross-country comparison. Our aim was to scope peer-reviewed research and grey literature on migrant health conducted in Scotland and identify any gaps in the evidence. Our objectives were to: [1] understand the extent of the available research by topic area [2] summarise the types of research already conducted, populations studied, topics covered and approaches taken [3], map the existing research conducted in Scotland and [4] identify areas for future research based on any gaps in the evidence identified.
Methods
A scoping review was conducted as they can aid detection of evidence gaps [42] and allow incorporation of grey literature in topics with insufficient published research [43]. Arksey and O’Malley’s [44] five stage scoping review framework was used.
Stage 1: identifying the research question
Arskey and O’Malley [44] suggest maintaining a broad approach to identifying the research question, in order to generate breadth of coverage. On this basis, and in line with the research question identified in the Villarroel et al. [24] scoping review, our research question was framed as follows: What is the scope, main topics and gaps in evidence in the existing literature on health of international migrants living in Scotland? Arksey and O’Malley [44] highlight the importance of defining terminology at the outset of scoping reviews. For consistency, we used the broad definition of ‘migrant’ as per Villaroel et al. [24], from the International Organisation for Migration (IOM) [1]. References to refugees or asylum seekers followed the United Nations Refugee Agency definitions [3].
Stage 2: identifying relevant studies
Electronic database searches identified reports alongside a grey literature search, in line with Arskey and O’Malley’s [44] guidance to search for evidence via different sources. CINAHL, Web of Science, SocIndex and Medline academic databases were selected with input from co-authors. Search terms for the review were based upon those used by Villaroel et al. [24] with additional relevant terms from Hannigan et al. [9] The strategy combined three sets of terms for: Migrants (e.g., refugee, migrant, immigrant or newcomer), Scotland and Health. Both free text terms and index terms were used and adapted to the 4 academic databases and searches were run on 10th March 2023 (see Additional File 1 for database search strategies). Thirteen Government, University, and third-sector websites in Scotland were scoped for selection then hand-searched for grey literature (listed in Additional File 1).
Stage 3: study selection
Net-migration to Scotland increased in the 2000s [27] hence a date range of January 2002-March 2023 was used to identify evidence. The search was limited to English only. Inclusion/exclusion criteria for the studies were based on those used by Villaroel et al. [24] and expanded upon following discussion with co-authors (see Table 1). Reports were included if based on primary or secondary research on the health of international migrants in Scotland and used qualitative, quantitative or mixed methods research design. International or UK based reports were only included if Scottish results were documented separately. Reports on the health of ethnic minority groups in Scotland was included if place of birth was recorded. Research on internal (non-international) migrants within Scotland, either moving from one Scottish area to another or from another part of the United Kingdom to Scotland, were excluded.
Stage 4: data charting
All records were saved to RefWorks for screening. Records were first screened at title/abstract stage with 10% independently checked by the co-authors. The remaining reports were single screened using full text by the first author. Data from the included records was extracted and organised in tabular form under the following headings, which were agreed by team members: article type (peer-reviewed article or grey literature), publication date, geographical setting, study/intervention’s target population, funding, primary research focus on migrant health (y/n), study objective, data collection method, study design (qualitative/quantitative/mixed) and main finding. Reports were not critically appraised in this scoping review.
Stage 5: collating, summarising and reporting results
A report (either a peer-reviewed journal article or grey literature report) is used as our unit of analysis. In order to present the range of research identified, reports were grouped by the different headings in our data charting table and the outcomes considered for relevance to our scoping review’s aim. Our Results summarise the recency, focus, study designs and funding sources of the identified research, followed by the geographical settings and whether Scotland was included in international research reports. Reports were grouped by their study population and further sub-divided by publication type and geographical area for summarising. Finally, the WHO’s European strategy and action plan (SAAP) for refugee and migrant health [7] is a policy framework designed to help governments and other stakeholders monitor and improve migrant health in Europe. There are nine strategic areas in the WHO’s SAAP, which prioritise the most salient issues. In line with Villaroel et al’s [24] approach and in order to compare scoping review outcomes, these areas were used to categorise the findings of this review. Each report was matched to the most appropriate SAAP:
-
1.
Establishing a Framework for Collaborative Action.
-
2.
Advocating for the right to health of refugees.
-
3.
Addressing the social determinants of health.
-
4.
Achieving public health preparedness and ensuring an effective response.
-
5.
Strengthening health systems and their resilience.
-
6.
Preventing communicable disease.
-
7.
Preventing and reducing the risks caused by non-communicable disease.
-
8.
Ensuring ethical and effective health screening and assessment.
-
9.
Improving health information and communication.
The primary focus (aims and objectives) of each report was used to identify the relevant SAAP area/areas. To improve reliability, results were compared using coding criteria used in Villaroel et al’s study (MacFarlane 2023, personal communication, 31st May). 10% of the reports were checked by one co-author to ensure consistent coding to SAAP categories. Any instances of uncertainty in mapping reports to the relevant SAAP area/areas were discussed and resolved by team members.
Results
This scoping review of the literature on migrant health in Scotland identified 2166 records from academic literature databases, following duplicate removal, and 170 records from website searches (see Fig. 1). Following screening, a total of 71 peer-reviewed journal articles and 29 grey literature studies (totalling 100 reports) were included for analysis (Results table and reference list are presented in Additional File 2).
Overall findings
The majority of reports were published between 2013 and 2022. Fifty-eight reports (58%) focused exclusively on migrant health [18, 39, 45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102]. 23 centred on health but included other populations in addition to migrants – for example research on ethnic minorities or other vulnerable groups [13, 31, 35, 103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122]. Seventeen reports were included where the sample population were migrants, but the primary topic was not health – for example destitution, integration, and service needs [27, 73, 74, 123,124,125,126,127,128,129,130,131,132,133,134,135]. Health data was reported as part of the wider subject matter. One report [136] looked at the social determinants of breastfeeding including migrant status and one [137] compared attitudes to aging and family support between countries.
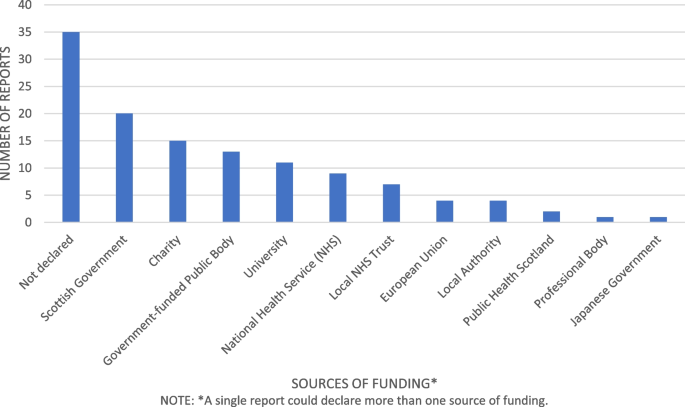
Funding sources were not declared for 35 (35%) of reports. The Scottish Government funded 20 reports (20%) [13, 27, 32, 39, 45,46,47, 66, 77, 88, 99,100,101,102, 113, 116, 119, 121, 129, 134]. Other common sources of funding included Government funded public bodies (n = 13) [45, 48,49,50,51,52,53, 104, 107, 113, 116, 131, 136], the Scottish Health Service (n = 18) (either the National Health Service (NHS) [13, 54, 56,57,58,59, 102, 113, 116], local NHS trusts [45, 60, 61, 77, 102, 103, 112] or by Public Health Scotland [13, 113]) Eleven reports (11%) were funded by Universities. The charity sector financed 15 (15%) reports [53, 63, 66, 69,70,71,72,73,74, 103, 111, 123, 125, 132, 138] and the EU and Scottish local authorities funded four reports each [45, 62, 75,76,77, 102, 125, 135]. Professional bodies financed one report [126] as did the Japanese government [64]. No reports received funding from the business sector. The biggest sources of funding for grey literature were Refugee charities (40%) and the Scottish government (30%) (see Fig. 2).
Research methods and data collection
52% of reports used qualitative research methods. Forty-five reports (86%) collected data using 1–1 interviews and 24 (46%) used focus groups. Other methods of data collection included questionnaires (six studies (11%)), workshops (two studies (3.85%)) and observation (two studies (3.85%)). Oral/written evidence, guided play sessions, family case studies and participatory activity sessions were used in one report each.
28% of reports used quantitative research methods, most commonly cross section design (ten studies (36%)) and cohort design (18 studies (64%)). Information was obtained from databases including medical records, Census data and national records in 21 reports (75%). Questionnaires were used in six reports (21%). Other methods including body measurements, food diaries, blood samples, interviews and case reviews were used in 1 report each.
20% of reports used mixed methods. The most common method of data collection was questionnaires in 14 reports (70%), interviews in ten reports (50%), focus groups in seven reports (35%), workshops in three reports (13.6%), and databases in three reports (13.6%). Other methods included literature review in two reports (10%), case note reviews in two reports (10%) and one reports each used mapping and school records.
Geographical areas of study
Ninety-one reports were situated in Scotland, of which 35 (38.5%) covered the whole country and 56 (61.5%) specified a city or area where research was undertaken. Some UK and international reports also specified the area of Scotland. The largest share of research within Scotland overall was in Glasgow with 36 reports, followed by Edinburgh with 16 reports, Lothian with six reports, Aberdeen with five reports and Grampian with three reports. The Northeast, Stirling, Highlands, Inverness, Lanarkshire, Motherwell and Selkirk had one report in each area.
There were seven international reports, three on mortality by country of birth [75, 76, 78], one on cross cultural communication [79], one on maternity care in Poland and Scotland [99], one comparing attitudes to aging in China and Scotland [137] and one on the link between birthweights and integration of migrants [64]. The remaining two reports were UK based, one on immunisation of Roma and traveller communities [117] and one on the link between ethnic diversity and mortality [104]. All the included international and UK reports documented the Scottish data separately within results.
Migrant population
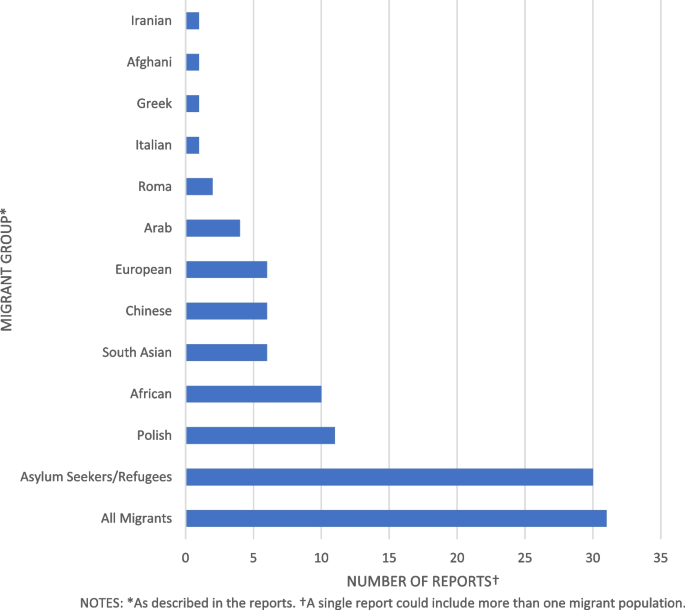
Thirty-one reports included all migrants in the study population. The remaining reports included 30 studies on asylum seekers/refugees, 11 on Polish migrants, ten on Africans, six each on South Asians/Chinese/European, three on Arabs, and two on Roma populations (see Fig. 3). Most reports did not specify the country of origin for Asylum seekers and refugees - where country of birth was specified, reports were also included in the appropriate category.
Grey literature and peer-reviewed reports differed in population focus. The most common populations of interest in grey literature were asylum seekers/refugees consisting of 18 reports (62%) [27, 47, 54, 55, 59, 63, 70,71,72,73,74, 123, 125, 127, 128, 132, 134, 138] while for peer-reviewed journals 24 reports (34%) focused on all migrants [13, 35, 45, 48, 64, 76, 78,79,80,81, 104, 105, 108, 109, 113,114,115,116, 118, 120,121,122, 136].
Migrant study population also differed by local area; Glasgow city, where the majority of research occurred, had 18 reports of 36 (50%) on Asylum seekers/refugees [47, 48, 52,53,54,55, 58, 63, 70,71,72, 82, 83, 127, 128, 130, 138, 139] eight reports (22%) on Africans [52, 53, 84,85,86,87, 106, 107], seven reports (19%) on all migrants [45, 48, 80, 102, 104, 105, 121] and two reports (5.5%) on Roma migrants [103, 117]. Other populations had one reports each. In Edinburgh five reports of 16 (31%) were on the Polish population [56, 67, 68, 89, 90], and two reports (12.5%) on Asylum seekers/refugees [60, 133], Chinese [62, 137], South Asian [46, 119], all migrants [105, 121] and Africans [87, 107]. The remaining migrant groups had one report each. Other areas of Scotland show no clear pattern with studies in disparate migrant population groups.
SAAP Area mapping
1. Establishing a framework for collaborative action
Nine reports had a primary focus on collaborative action and were categorised under SAAP area 1 (see Fig. 4) [66, 70, 72, 73, 103, 125, 129, 132, 134]. Four reports (33%) used a mixed methods study design, the remaining five reports (67%) used a qualitative design. One report [66] focused on the epidemiology of female genital mutilation and a proposed intervention strategy. One report [66] focused on the epidemiology of female genital mutilation and a proposed intervention strategy. One report [103] evaluated service provision to the Roma community in Glasgow. The remaining reports focused on refugees and asylum seekers: four [73, 125, 132, 134] evaluations of refugee integration projects, one [70] on services available to pregnant women, and one [72] an assessment of a peer-education service. One report [129] was a review of service provisions for migrants during the Covid-19 pandemic. All reports in SAAP area 1 were grey literature and three (37.5%) had a primary focus on migrant health while four (50%) focused on integration, one (11%) included data on ethnic minorities and one (11%) on services during the covid-19 pandemic. The majority (seven reports (78%)) were also categorised to another SAAP area most commonly area 2 (five studies (55%)) or area 5 (four studies (44%)).
2. Advocating for the right to health of refugees
Nineteen reports focused on SAAP area 2, advocating for the right to health of refugees (see Fig. 4) [47, 52,53,54,55, 63, 70, 71, 83, 103, 123,124,125, 127,128,129, 134, 138, 140]. Sixteen reports (84%) had a qualitative study design and the remaining three (16%) reports used mixed methods. Nine reports (47%) focused on the health impact of the asylum system [52, 55, 71, 74, 123, 127,128,129, 138], five (26%) on health and access to care [47, 54, 83, 103, 124], two (10.5%) on maternity care [63, 70], two (10.5%) on integration services [125, 134] and one report on mental health in HIV positive migrants [53]. Nine reports (47%) had a primary focus on migrant health while the remaining 10 (53%) also involved wider social issues. The majority (15 (79%)) of reports were grey literature. All the articles in this group overlapped with another SAAP area. Area 3 is the most common joint category with ten reports (53%) followed by area 5 with seven reports (37%), area 1 shares five reports (26%), while areas 4 and 8 share one report each (5%).
3. Addressing the social determinants of health
Twenty-nine reports were categorised to SAAP area 3 – addressing the social determinants of health (see Fig. 4) [13, 27, 45, 50, 52, 55, 60, 62, 63, 65, 68, 71, 74, 80,81,82, 91,92,93, 102, 112, 123, 124, 127, 128, 136,137,138]. The majority (14 (48%)) used a qualitative study method, eight (28%) used quantitative methodology and the remaining seven reports (24%) used mixed methods. Nineteen reports (65.5%) were peer-reviewed journals [13, 45, 50, 52, 60, 62, 63, 65, 68, 80,81,82, 91,92,93, 104, 112, 124, 136, 137] and ten (34.5%) were grey literature [27, 55, 63, 71, 74, 102, 123, 127, 128, 138]. Ten reports (34.5%) discussed the effects of the asylum system on health [27, 52, 63, 71, 74, 123, 124, 127, 128, 137] and one (3.5%) migration and health [50]. Six reports (21%) focused on culture and ethnicity [82, 92, 102, 104, 112, 137], five reports (17%) discussed economic and environmental determinants of health [13, 45, 67, 81, 93] and five reports (17%) the health impact of social activities [55, 60, 62, 80, 91]. Of the remaining reports, one [65] discussed Brexit and mental health of European migrants and one discussed the effect of coping strategies on wellbeing in Polish migrants [68]. Most reports, 18 (62%) had a primary focus on migrant health [45, 50, 52, 55, 60, 62, 63, 65, 67, 68, 71, 80,81,82, 91,92,93, 102], six reports (21%) discussed wider social factors in addition to health [74, 123, 124, 127, 128, 138]. Of the remaining reports three (10%) looked at ethnic background and country of birth [13, 112, 136], one [27] included other vulnerable groups and one [137] included people living in China and Chinese migrants to Scotland. Thirteen reports were also categorised to one or more additional SAAP area - ten (34%) were also applicable to area 2 [52, 55, 63, 71, 74, 123, 124, 127, 128, 138], three (10%) to area 5 [63, 82, 92] and one (7%) to area 4 [27].
4. Achieving public health preparedness and ensuring an effective response
Twenty-one reports were assigned to SAAP area 4 (see Fig. 4) [27, 31, 35, 39, 47, 57, 64, 75,76,77,78, 94, 104, 108, 109, 111, 113, 114, 116, 120, 135] of which fourteen (67%) used quantitative research methods, four (19%) mixed methods and three (14%) qualitative methods. Thirteen (62%) reports were peer-reviewed journals [35, 59, 64, 75, 78, 104, 108, 109, 111, 113, 114, 116, 120] and eight (38%) grey literature [27, 31, 39, 47, 57, 77, 94, 135]. Most reports (12 (57%)) focused on morbidity and mortality in migrant populations [31, 35, 64, 75, 76, 78, 104, 108, 109, 113, 114, 116]. Six (29%) investigated health status and healthcare needs in migrant groups in Scotland [39, 47, 57, 77, 94, 135]. Two reports (9.5%) analysed the epidemiology of HIV infections [111, 120] and the remaining report focused on the health needs of young people during the covid-19 pandemic [27]. Nine reports (43%) had a primary focus on migrant health [39, 47, 55, 64, 75,76,77,78, 94] while eight (38%) also analysed data by ethnicity [31, 35, 104, 108, 109, 113, 114, 116]. Of the remaining reports, three (14%) included other populations within Scotland [27, 111, 120] and one (5%) included other characteristics in addition to health information [135]. Ten reports (48%) were also categorised to another SAAP area; one to area 2 [47], one to area 3 [27], four to area 5 [47, 57, 77, 135], two to area 6 [111, 120] and two to area 9 [31, 108].
5. Strengthening health systems and their resilience
Twenty-nine reports were assigned to SAAP area 5 (see Fig. 4) [18, 47,48,49, 54, 57, 63, 69, 70, 72, 77, 79, 82, 83, 92, 95,96,97, 99, 101, 103, 118, 119, 126, 129, 131, 133, 135, 141] of which 23 (79%) used qualitative research methods. Three reports used quantitative methods (10.3%) and the remaining three used mixed methods (10.3%). Twelve reports (41%) examined migrants needs and experiences of health care [47, 49, 54, 57, 58, 77, 83, 95, 103, 119, 129, 135], eight (24%) focused on pregnancy and childcare [63, 70, 92, 96, 97, 99, 101, 118] and two (7%) on barriers to healthcare access [48, 131]. Two reports (7%) evaluated healthcare programmes [72, 133] and two focused on communication in primary care [79] and maternity services [69]. The remaining three reports (10%) covered sexual health [82], health information needs of Syrian refugees [126] and general practitioner training [18]. Nineteen (65.5%) were peer reviewed journals [18, 48, 49, 58, 69, 79, 82, 83, 92, 95,96,97, 99, 101, 118, 119, 125, 131, 133] and ten (34.5%) were grey literature [47, 54, 57, 63, 70, 72, 77, 103, 129, 135]. Twenty-one (72%) had a primary focus on migrant health [18, 47,48,49, 54, 57, 58, 63, 69, 70, 72, 77, 79, 82, 83, 92, 95,96,97, 99, 101]. Six reports (21%) included research on other characteristics or services [103, 126, 129, 131, 133, 135]. The remaining two reports (7%) included ethnic groups as well as migrants in the data [118, 119]. Nineteen reports (65.5%) were also assigned to one or more other category areas: five reports (17%) to area 1 [47, 70, 72, 103, 129], five reports (17%) to area 2 [54, 63, 83, 103, 129], three reports (10%) to area 3 [63, 82, 92], four reports (14%) to area 4 [47, 57, 77, 135], one (3.5%) to area 7 [119] and one (3.5%) to area 9 [48].
6. Preventing communicable diseases
Fourteen reports were assigned to SAAP area 6 (see Fig. 4) [56, 61, 87,88,89,90, 105,106,107, 111, 115, 117, 120, 122] of which four (31%) used quantitative methods, five (38%) used qualitative methods and five (38%) used mixed methods. Five reports (38.5%) examined immunisation behaviour [56, 61, 89, 90, 117], five (38%) on epidemiology and treatment of HIV [106, 107, 111, 120, 122]. The remaining four reports (31%) focused on tuberculosis in healthcare workers [115], malaria [105] and sexual health services [87, 88]. Only one reports was grey literature [88], the remainder were peer-reviewed journals. Six reports (46%) had a primary focus on migrant health [56, 61, 87,88,89,90] while seven reports (54%) also included other at-risk groups in the analysis. Four reports (31%) were also assigned to another SAAP category, two (15%) to area 4 [111, 120] and two (15%) to area 8 [88, 115].
7. Preventing and reducing the risks posed by non-communicable diseases
Eight reports were categorised to SAAP area 7 (see Fig. 4) [46, 51, 59, 84,85,86, 98, 119] of which six (75%) used qualitative research methods, one (12.5%) used quantitative methods and one (12.5%) used mixed methods. Only one report (12.5%) was grey literature [59] the remaining seven reports (87.5%) were peer-reviewed journals [48, 87, 92, 126,127,128, 140]. Three reports (37.5%) focused on health behaviours [51, 85, 98], two (25%) on mental health, two (25%) on diabetes and one (12.5%) on chronic disease. Seven reports(87.5%) had a primary focus on migrant health [46, 51, 59, 84,85,86, 98], with the remaining report (12.5%) including ethnic minority groups [119]. One report (12.5%) was also assigned to SAAP area number 5 [119].
8. Ensuring ethical and effective health screening and assessment
There were six reports assigned to category 8 (see Fig. 4) [53, 88, 100, 110, 115, 121] of which two (33%) used a quantitative research method, three (50%) used a qualitative method and one used mixed methods. One report (14%) was grey literature [88] the remaining five reports (83%) were peer reviewed journals [53, 100, 110, 115, 121]. Three reports (50%) focused on cancer screening in migrant women [21, 100, 110], one (17%) analysed access to HIV testing among African migrants [53], one (17%) on T.B in healthcare workers [72] and one (17%) on sexual health [36]. Three reports (50%) had a primary focus on migrant health [53, 88, 100] while the remaining three reports (50%) included other at-risk groups in the analysis [110, 115, 121]. There were three reports which overlapped with other SAAP areas: one [53] (17%) was categorised to area 2 while two [88, 115] (33%) were categorised to area 6.
9. Improving health information and communication
Three reports were assigned to SAAP area 9 (see Fig. 4) [31, 108, 130]. One of these (33%) used a qualitative approach, one (33%) used a quantitative approach and one (33%) used mixed methods. Two [108, 130] (66%) were peer-reviewed journal articles and one [31] (33%) was grey literature. Two reports (66%) focused on improving migrant demographics and health information using databases [31, 108] while one (33%) described an information-needs matrix for refugees and asylum seekers [130]. Two [31, 108] included ethnicities in the data while one [130] had a primary focus on migrant health. Two reports [31, 108] (66%) also applied to SAAP area 4 while one report [130] (33%) was in SAAP area 9 only.
Discussion
To our knowledge this is the first scoping review conducted on migrant health in Scotland. A previous rapid literature review [94] found most research focused on health behaviours, mental health, communicable disease and use of and access to healthcare; however, the review limited migrant definition to those who had immigrated within five years and asylum seekers were not included.
In our review, the majority of reports were published from 2013 onwards, aligning with the expansion in migrant research internationally [142]. 52% used qualitative research methods, 28% used quantitative methods and 20% used mixed methods. 58% focused on migrant health: the remaining papers included other populations or health as part of a wider remit. Research funding was mostly provided by the Scottish Government, NHS, refugee charities and Universities. No studies received funding from the private sector, although this sector has the potential resource and capacity to play a key role in funding future research to improve migrant health in Scotland. Geographically, most studies took place in Glasgow (36%), nationwide (38.5%) or Edinburgh (16%) – other areas were under-represented including Aberdeen (5%), despite being the city with the largest migrant population [30]. There was a lack of studies in rural localities. These findings concur with a UK migrant health review by Burns et al. [23] where research was concentrated in larger cities and data was sparse in rural areas relative to the migrant population.
Half of the research identified that was conducted in Glasgow focused on asylum seekers/refugees. Glasgow was previously the only Scottish city to host asylum seekers [143] and currently supports the most asylum seekers of any local authority in the UK [29]. In April 2022, the UK government widened the Asylum dispersal scheme to all local authorities [144]. Around 70% of Scotland’s refugee support services are based in Glasgow and the South-west [145]. As reduced access to services may impact the health of asylum seekers, research in Glasgow may not be generalizable to other regions of Scotland.
Almost one-third (30%) of all reports focused on asylum seekers and refugees – an overrepresentation given that only 18% of migrants to the UK are asylum seekers [146] and as low as 2% of all migrants in Scotland [147]. Asylum seekers and refugees are at risk of poor health due to trauma, difficult journeys, overcrowded camps, poor nutrition and lack of access to healthcare [148]. They have worse maternity outcomes and increased rates of mental illness [149]. Increased research on health of asylum seekers and refugees is necessary due to their additional vulnerabilities [142]. However, asylum seeker’s country of origin was generally not specified. Asylum seekers have heterogenic backgrounds [150] and nationality and trauma experience affect health status [151]. Further research focused on specific nationalities of asylum seekers would enhance understanding of the health needs in this population.
Almost one-third (31%) of studies did not specify a migrant group. This concurs with a Norwegian migrant health study by Laue et al. [152] where 36% of research did not identify country of birth. Where nationality was identified, Polish, African and South Asian were most prevalent. Poles are the largest migrant group in Scotland, however for the other most common immigrant groups of Irish, Italian and Nigerian [30] there was an absence of research. No studies took place on Nigerian migrants – nine studies indicated African populations, but country of birth was not specified. Since March 2022, 23,000 Ukrainians have migrated to Scotland [153], however no studies on Ukrainians were identified currently. Research may be underway which is yet to be published.
Only one study explored the impact of Brexit on European migrants’ health despite 56% of migrants to Scotland being EU nationals [30]. Again, research may be taking place currently, which is yet to be published. No studies involved undocumented migrants despite this populations’ high rates of poor physical/mental health exacerbated by poor housing and working conditions [154]. An estimated 7.2–9.5% of the workforce in the UK are migrant workers who have higher risks of poor working conditions and injury [155]. Scotland depends on a migrant workforce for some industries such as agriculture [156] but only two research papers specified migrant workers.
Most research papers related to the right to health of refugees (SAAP 2), social determinants of health (SAAP 3), public health planning (SAAP 4) and strengthening health systems (SAAP 5). Areas with less research were frameworks for collaborative action (SAAP 1), preventing communicable disease (SAAP 6), preventing non-communicable disease (SAAP 7) and health screening and assessment (SAAP 8). Only three studies related to improving health information and communication (SAAP 9). Lebano et al. [12] conducted a literature review of migrant health in Europe and found data collection unreliable and disorganised. There is a lack of data on the numbers and types of migrants entering Scotland and research tends not to differentiate between ethnic minorities and migrants [94]. As poor-quality information hinders surveillance and planning of services SAAP area 9 is an important consideration for increased research.
Villarroel et al. [24] also found more research in SAAP areas 3 to 5 and less in areas 6 to 9. However, their study returned no results in category 1, collaborative action, or 2, the right to health of refugees, while this study assigned 9% of articles to category 1 and 19% to category 2. Most articles in our study relating to categories 1 and 2 were grey literature, which was excluded from the original Irish scoping review. This highlights a potential difference in the focus of peer-reviewed articles compared to government/refugee charity commissioned reports. Collaborative action and the right to health of refugees and asylum seekers are entwined in Scotland due to the complex policy environment; the social determinants of health such as housing, education, welfare rights and social integration are influenced by a variety of UK and Scottish statutory bodies as well as third sector organisations [157]. Despite this complexity, organisations work well together [158]. Further academic research in this area would enhance joint working practices and networks.
A scoping review in the UK [23] found similar quantities of research corresponding to SAAP areas 3, 2 and 9. However in Scotland areas 1, 5 and 8 were a combined 44% of included papers compared with 27.8% of results on health systems and structures in Burns et al’s [23] study. Almost half of the articles in SAAP areas 1,5 and 8 were grey literature, which was not included in Burns et al’s [23] review. Conversely, Burns et al. [23] found 81.9% of research in the UK related to epidemiology, equivalent to SAAP categories 4,6 and 7. In a Norwegian scoping review of migrant health [152] 65% of research was related to epidemiological data on health and disease. Only 42% of the research in this current study related to epidemiological data; the quantity of evidence was reduced by excluding combined research from the UK. As Scotland has higher mortality and morbidity than elsewhere in the UK [29] it is important to undertake further epidemiological research limited to Scotland.
Strengths and weaknesses
Strengths of this review include the use of the WHO’s SAAP categories [7] to classify data, in accordance with the Villarroel et al’s [24] study: this means results are linked to policy on migrant health and facilitates comparability to the Irish study results. Additionally results include data on migrant groups, locality, and funding of included papers; these highlight potential omissions for future research consideration. Results include diverse research methods and published and grey literature giving a wide overview of available evidence, reported using the Preferred Reporting Items for Systematic reviews and Meta-Analyses for Scoping Reviews (PRISMA-ScR) checklist (see Additional File 3) [159].
Limitations included the lack of an open-access protocol and search limitations of English language and selected databases. This means some relevant reports may be omitted. Due to time and resource limitations no quality appraisal was planned for included reports. Whilst we did not synthesise the findings for each topic area and migrant group, future systematic reviews could be undertaken to address this limitation and build on this work.
Conclusions
Immigration and ethnic diversity in Scotland have increased since 2002 which is reflected in the expansion of migrant health research. This review highlights evidence gaps including a lack of research in rural areas, undocumented migrants and migrant workers. There is a tendency to cluster asylum seekers together rather than differentiate between national groups. Within the SAAP areas there is less evidence relating to collaborative action, preventing communicable disease, preventing non-communicable disease and health screening and assessment. Further research is required on improving health information and communication for migrant populations in Scotland – a significant omission given the importance of accurate information for health service planning.
Availability of data and materials
All data analysed during this review comes from the papers listed in Additional file 2.
Abbreviations
- EU:
-
European Union
- HIV:
-
Human Immunodeficiency Virus
- NHS:
-
National Health Service
- SAAP:
-
Strategy and Action Plan
- SHELS:
-
The Scottish Health and Ethnicity Linkage Study
- UK:
-
United Kingdom
- WHO:
-
World Health Organisation
References
International Organisation for Migration (IOM). IOM Definition of Migrant. 2024. Available from: https://www.iom.int/about-migration.Cited 2024 Feb 8.
International Organisation for Migration United Nations. World Migration Report. 2022. Available from: available: https://worldmigrationreport.iom.int/wmr-2022-interactive/.
The United Nations Refugee Angency. Refugee facts: What is a refugee? 2024. Available from: https://www.unrefugees.org/refugee-facts/what-is-a-refugee/. Cited 2024 Feb 8.
Migration Data Portal. Migration data in Europe. 2023. Available from: https://www.migrationdataportal.org/regional-data-overview/europe#past-and-present-trends. Cited 2023 Aug 22.
International Centre for Migration Policy Development. Migration Outlook 2022 Twelve migration issues to look out for in 2022 Origins, key events and priorities for Europe. 2022. Available from: https://www.icmpd.org/file/download/56783/file/ICMPD%2520Migration%2520Outlook%25202022.pdf.
European Parliament. Exploring migration causes: why people migrate. 2023. Available from: https://www.europarl.europa.eu/news/en/headlines/world/20200624STO81906/exploring-migration-causes-why-people-migrate.
World Health Organisation. Strategic plan: Strategy and Action Plan for Refugee and Migrant Health in the WHO European Region 2016–2022. 2016. Available from: https://www.who.int/publications/i/item/strategic-plan-strategy-and-action-plan-for-refugee-and-migrant-health-in-the-who-european-region-2016-2022.
Graetz V, Rechel B, Groot W, Norredam M, Pavlova M. Utilization of health care services by migrants in Europe—a systematic literature review. Br Med Bull. 2017;121(1):5–18. Available from: https://www.academic.oup.com/bmb/article-lookup/doi/10.1093/bmb/ldw057.
Hannigan A, O'Donnell P, O'Keeffe M, MacFarlane A. How do Variations in Definitions of “Migrant” and their Application Influence the Access of Migrants to Health Care Services? Copenhagen: WHO Regional Office for Europe; 2016. (Health Evidence Network Synthesis Report, No. 46.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK391032/.
Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381(9873):1235–45. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673612620868.
Giannoni M, Franzini L, Masiero G. Migrant integration policies and health inequalities in Europe. BMC Public Health. 2016;16(1):463. Available from: http://www.bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-3095-9.
Lebano A, Hamed S, Bradby H, Gil-Salmerón A, Durá-Ferrandis E, Garcés-Ferrer J, et al. Migrants’ and refugees’ health status and healthcare in Europe: a scoping literature review. BMC Public Health. 2020;20(1):1039. Available from: https://www.bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-08749-8.
Cézard G, Finney N, Kulu H, Marshall A. Ethnic differences in self-assessed health in Scotland: The role of socio-economic status and migrant generation. Popul Space Place. 2022;28(3):e2403. Available from: https://onlinelibrary.wiley.com/doi/10.1002/psp.2403.
Anson J. The migrant mortality advantage: a 70 month follow-up of the brussels population. Eur J Popul. 2004;20(3):191–218.
World Health Organisation. Health of refugees and migrants. WHO European Region. 2018. Available from: https://www.who.int/publications/i/item/health-of-refugees-and-migrants---who-european-region-(2018).
Mladovsky P. A framework for analysing migrant health policies in Europe. Health Policy (New York). 2009;93(1):55–63. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0168851009001444.
De Vito E, de Waure C, Specchia ML, Parente P, Azzolini E, Frisicale EM, et al. Are undocumented migrants’ entitlements and barriers to healthcare a public health challenge for the European Union? Public Health Rev. 2016;37(1):13. Available from: http://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-016-0026-3.
Katikireddi SV, Bhopal R, Quickfall JA. GPs need training and funding in caring for refugees and asylum seekers. BMJ. 2004;328(7442):770.1. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.328.7442.770.
Carballo M, Hargreaves S, Gudumac I, Maclean EC. Evolving migrant crisis in Europe: implications for health systems. Lancet Glob Heal. 2017;5(3):e252-253. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2214109X17300402.
Juárez SP, Honkaniemi H, Dunlavy AC, Aldridge RW, Barreto ML, Katikireddi SV et al. Effects of non-health-targeted policies on migrant health: a systematic review and meta-analysis. Lancet Glob Heal. 2019;7(4):e420–35. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2214109X18305606.
Nielsen SS, Krasnik A. Poorer self-perceived health among migrants and ethnic minorities versus the majority population in Europe: a systematic review. Int J Public Health. 2010;55(5):357–71. Available from: (http://link.springer.com/10.1007/s00038-010-0145-4).
World Health Organsation. World report on the health of refugees and migrants. 2022. Available from: https://www.who.int/publications/i/item/9789240054462.
Burns R, Zhang CX, Patel P, Eley I, Campos-Matos I, Aldridge RW. Migration health research in the United Kingdom: a scoping review. J Migr Heal. 2021;4:100061. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2666623521000283.
Villarroel N, Hannigan A, Severoni S, Puthoopparambil S, MacFarlane A. Migrant health research in the Republic of Ireland: a scoping review. BMC Public Health. 2019;19(1):324. Available from: (https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-6651-2).
Scottish Government. Demographic Change in Scotland. 2010. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/research-and-analysis/2010/11/demographic-change-scotland/documents/0108163-pdf/0108163-pdf/govscot%3Adocument/0108163.pdf.
National Records of Scotland. Projected Population of Scotland (Interim) 2020-based. 2022. Available from: https://www.nrscotland.gov.uk/files/statistics/population-projections/2020-based/pop-proj-2020-scot-nat-pub.pdf.
Scottish Government. Coronavirus (COVID-19) - experiences of vulnerable children, young people, and parents: research. 2021. Available from: https://www.gov.scot/publications/experiences-vulnerable-children-young-people-parents-during-covid-19-pandemic/.
Scotland’s Census. Scotland’s Census: Ethnicity. 2011. Available from: https://www.scotlandscensus.gov.uk/census-results/at-a-glance/ethnicity/#:~:text=Scotland’spopulationwas96.0%25.
Walsh D. The changing ethnic profiles of Glasgow and Scotland, and the implications for population health. 2017. Available from: https://www.gcph.co.uk/assets/0000/6255/The_changing_ethnic_profiles_of_Glasgow_and_Scotland.pdf.
National Records of Scotland. Migration Statistics Quarterly Summary for Scotland. 2021. Available from: https://www.nrscotland.gov.uk/files/statistics/migration/quarterly-summary/miration-statistics-quarterly-summary-february-2021.pdf.
The Scottish Ethnicity and Health Research Strategy Working Group. Health in our Multi-ethnic Scotland Future Research Priorities. 2009. Available from: https://www.healthscotland.scot/media/1842/health-in-our-multi-ethnic-scotland-full-report.pdf .
The Scottish Public Health Observatory. Ethnic minorities: defining ethnicity and race. 2023. Available from: https://www.scotpho.org.uk/population-groups/ethnic-minorities/defining-ethnicity-and-race/. Cited 2023 Aug 22.
Krasnik A, Bhopal RS, Gruer L, Kumanyika SK. Advancing a unified, global effort to address health disadvantages associated with migration, ethnicity and race. Eur J Public Health. 2018;28(suppl_1). Available from: https://academic.oup.com/eurpub/article/doi/10.1093/eurpub/cky046/4956664 .
Bhopal R, Fischbacher C, Povey C, Chalmers J, Mueller G, Steiner M, et al. Cohort profile: scottish health and ethnicity linkage study of 4.65 million people exploring ethnic variations in disease in Scotland. Int J Epidemiol. 2011;40(5):1168–75. Available from: https://academic.oup.com/ije/article-lookup/doi/10.1093/ije/dyq118.
Bhopal RS, Gruer L, Cezard G, Douglas A, Steiner MFC, Millard A, et al. Mortality, ethnicity, and country of birth on a national scale, 2001–2013: a retrospective cohort (Scottish Health and Ethnicity Linkage Study). Basu S, editor. Plos Med. 2018;15(3):e1002515. https://doi.org/10.1371/journal.pmed.1002515. Basu S, editor.
Allik M, Brown D, Dundas R, Leyland AH. Differences in ill health and in socioeconomic inequalities in health by ethnic groups: a cross-sectional study using 2011 Scottish census. Ethn Health. 2022;27(1):190–208. https://doi.org/10.1080/13557858.2019.1643009 (https://www.tandfonline.com/doi/full/).
Watkinson RE, Sutton M, Turner AJ. Ethnic inequalities in health-related quality of life among older adults in England: secondary analysis of a national cross-sectional survey. Lancet Public Hea. 2021;6(3):e145-154.
Fischbacher CM, Cezard G, Bhopal RS, Pearce J, Bansal N. Measures of socioeconomic position are not consistently associated with ethnic differences in cardiovascular disease in Scotland: methods from the Scottish Health and Ethnicity Linkage Study (SHELS). Int J Epidemiol. 2014;43(1):129–39. Available from: https://academic.oup.com/ije/article-lookup/doi/10.1093/ije/dyt237.
Scottish Government. Characteristics of Recent and Established EEA and non-EEA migrants in Scotland: Analysis of the 2011 Census. 2015. Available from: https://www.gov.scot/publications/characteristics-recent-established-eea-non-eea-migrants-scotland-analysis-2011-census/.
House of Lords Library. Refugees and asylum-seekers: UK policy. 2022. https://lordslibrary.parliament.uk/refugees-and-asylum-seekers-uk-policy/.
British Medical Association. Refugee and asylum seeker patient health toolkit. Unique health challenges for refugees and asylum seekers. 2022. Available from: https://www.bma.org.uk/advice-and-support/ethics/refugees-overseas-visitors-and-vulnerable-migrants/refugee-and-asylum-seeker-patient-health-toolkit/unique-health-challenges-for-refugees-and-asylum-seekers.
Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D. An evidence-based approach to scoping reviews. Worldviews Evidence-Based Nurs. 2016;13(2):118–23. Available from: https://doi.org/10.1111/wvn.12144.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. Available from: (http://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-5-69).
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.Available from: http://www.tandfonline.com/doi/abs/10.1080/1364557032000119616).
Kearns A, Whitley E, Egan M, Tabbner C, Tannahill C. Healthy migrants in an unhealthy city? The Effects of time on the health of migrants living in deprived areas of glasgow. J Int Migr Integr. 2017;18(3):675–98. Available from: http://link.springer.com/10.1007/s12134-016-0497-6.
Porqueddu T. Herbal medicines for diabetes control among Indian and Pakistani migrants with diabetes. Anthropol Med. 2017;24(1):17–31. Available from: https://www.tandfonline.com/doi/full/10.1080/13648470.2016.1249338.
Roshan N. Supporting new communities: a qualitative study of health needs among asylum seekers and refugee communities in North Glasgow final report. 2005. Available from: https://www.stor.scot.nhs.uk/handle/11289/579930.
Piacentini T, O’Donnell C, Phipps A, Jackson I, Stack N. Moving beyond the ‘language problem’: developing an understanding of the intersections of health, language and immigration status in interpreter-mediated health encounters. Lang Intercult Commun. 2019;19(3):256–71. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829214001233.
Sime D. ‘I think that Polish doctors are better’: Newly arrived migrant children and their parents׳ experiences and views of health services in Scotland. Health Place. 2014;30:86–93. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829214001233.
Steven K, Munoz S, Migrants, Matter. Report of a Peer Researched Project on EU Migrant Health in the Highlands of Scotland. University of the Highlands and Islands. 2016. Available from: https://www.spiritadvocacy.org.uk/assets/Birchwood-Highland-HUG-Migrants-Matter-study-2015-2016.pdf.
Anderson AS, Bush H, Lean M, Bradby H, Williams R, Lea E. Evolution of atherogenic diets in South Asian and Italian women after migration to a higher risk region. J Hum Nutr Diet. 2005;18(1):33–43. Available from: (https://onlinelibrary.wiley.com/doi/10.1111/j.1365-277X.2004.00584.x).
Isaacs A, Burns N, Macdonald S, O’Donnell CA. ‘I don’t think there’s anything I can do which can keep me healthy’: how the UK immigration and asylum system shapes the health and wellbeing of refugees and asylum seekers in Scotland. Crit Public Health. 2022;32(3):422–32. Available from: https://www.tandfonline.com/doi/full/10.1080/09581596.2020.1853058.
Palattiyil G, Sidhva D. Caught in a web of multiple jeopardy: post-traumatic stress disorder and HIV-positive asylum seekers in Scotland. Clin Soc Work J. 2015;43(4):362–74. Available from: http://link.springer.com/10.1007/s10615-015-0542-5).
Abdulkadir J, Azzudin A, Buick A, Curtice L, Dzingisai M, Easton D, et al. What do you mean, I have a right to health? Participatory action research on health and human rights. 2016. Available from: https://strathprints.strath.ac.uk/58209/1/Abdulkadir_etal_IPPI_2016_What_do_you_mean_I_have_a_right_to_health.pdf.
Strang A, Quinn N. Integration or isolation? Mapping social connections and well-being amongst refugees in Glasgow. 2014. Available from: https://eresearch.qmu.ac.uk/bitstream/handle/20.500.12289/4139/eResearch%25204139.pdf?sequence=1&isAllowed=y.
Gorman DR, Bielecki K, Larson HJ, Willocks LJ, Craig J, Pollock KG. Comparing vaccination hesitancy in polish migrant parents who accept or refuse nasal flu vaccination for their children. Vaccine. 2020;38(13):2795–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X20302255.
Love J, Vertigans S, Domaszk E, Zdeb K, Love A, Sutton P. Health & ethnicity in Aberdeenshire: a study of Polish in-migrants; a report for the Scottish Health Council. 2007. Available from: https://rgu-repository.worktribe.com/output/247667.
O’Donnell CA, Higgins M, Chauhan R, Mullen K. Asylum seekers’ expectations of and trust in general practice: a qualitative study. Br J Gen Pract. 2008;58(557):e1-11. Available from: https://bjgp.org/lookup/doi/10.3399/bjgp08X376104.
Quinn N, Shirjeel S, Siebelt L, Donnelly R, Pietka E. An evaluation of the sanctuary community conversation programme to address mental health stigma with asylum seekers and refugees in Glasgow. 2011. Available from: https://www.healthscotland.com/uploads/documents/5584-SanctuaryCommunityConversationEvaluation.pdf.
Ager A. Community contact and mental health amongst socially isolated refugees in Edinburgh. J Refug Stud. 2002;15(1):71–80. Available from: https://academic.oup.com/jrs/article-lookup/doi/10.1093/jrs/15.1.71.
Sim JA, Ulanika AA, Katikireddi SV, Gorman D. Out of two bad choices, I took the slightly better one’: Vaccination dilemmas for Scottish and Polish migrant women during the H1N1 influenza pandemic. Public Health. 2011;125(8):505–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350611001697.
Zhao S, Patuano A. International Chinese Students in the UK: association between use of green spaces and lower stress levels. Sustainability. 2021;4(1):89. Available from: https://www.mdpi.com/2071-1050/14/1/89.
Da Lomba S, Murray N. Women and Children First? Refused asylum seekers’ access to and experiences of maternity care in Glasgow. 2014. Available from: https://strathprints.strath.ac.uk/58655/1/Lomba_Murray_SRC_2014_Women_and_Children_First_Refused_Asylum_Seekers_Access_to_and_Experiences.pdf.
Sørbye IK, Vangen S, Juarez SP, Bolumar F, Morisaki N, Gissler M, et al. Birthweight of babies born to migrant mothers - What role do integration policies play? SSM - Popul Heal. 2019;9:100503. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2352827319301971.
Teodorowski P, Woods R, Czarnecka M, Kennedy C. Brexit, acculturative stress and mental health among EU citizens in Scotland. Popul Space Place. 2021;27(6). Available from: https://onlinelibrary.wiley.com/doi/10.1002/psp.2436.
Baillot H, Murray N, Connelly E, Howard N. Tackling Female Genital Mutilation in Scotland: A Scottish model of intervention. 2014. Available from: https://www.celcis.org/application/files/8116/2185/5421/Tackling_Female_Genital_Mutilation_-_A_Scottish_Model_of_Intervention.pdf.
Weishaar HB. Consequences of international migration: a qualitative study on stress among Polish migrant workers in Scotland. Public Health. 2008;122(11):1250–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350608000942.
Weishaar HB. You have to be flexible—coping among polish migrant workers in Scotland. Health Place. 2010;16(5):820–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829210000432.
Crowther S, Lau A. Migrant polish women overcoming communication challenges in scottish maternity services: a qualitative descriptive study. Midwifery. 2019;72:30–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613819300361.
Fassetta G, Da Lomba S, Quinn N. A healthy start? Experiences of pregnant refugee and asylum seeking women in Scotland. 2016. Available from: https://www.redcross.org.uk/-/media/documents/about-us/research-publications/refugee-support/a-healthy-start-report.pdf.
Positive Action in Housing. 12 months since the Park Inn Tragedy in Glasgow, one in three hotel asylum seekers say their mental health has deteriorated. 2021. Available from: https://www.paih.org/one-in-three-glasgow-asylum-seekers-suffering-depression-and-anxiety.
Strang A. Refugee Peer Education for Health and Well-being. Evaluation Report. 2015. Available from: https://www.scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Peer-Education-Evaluation-Report.pdf.
Strang A, Marsden R, Mignard E. The Holistic Integration Service: Learning and Evaluation Year 1. 2014. Available from: https://www.scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Holistic-Integration-Service-year-1-evaluation-report.pdf.
British Red Cross. How will we survive? Steps to preventing destitution in the asylum system. 2021. Available from: https://www.redcross.org.uk/-/media/documents/about-us/how-will-we-survive-preventing-destitution-in-the-asylum-system.pdf.
Bhopal RS, Rafnsson SB, Agyemang C, Fagot-Campagna A, Giampaoli S, Hammar N, et al. Mortality from circulatory diseases by specific country of birth across six European countries: test of concept. Eur J Public Health. 2012;22(3):353–9. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckr062.
Rafnsson SB, Bhopal RS, Agyemang C, Fagot-Campagna A, Harding S, Hammar N, et al. Sizable variations in circulatory disease mortality by region and country of birth in six European countries. Eur J Public Health. 2013;23(4):594–605. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckt023).
de Lima P, Masud Chaudhry M, Whelton R, Arshad R. A study of migrant workers in Grampian. 2007. Available from: .http://www.communitiesscotland.gov.uk/stellent/groups/public/%0Adocuments/webpages/pubcs_019731.pdff.
Ikram UZ, Mackenbach JP, Harding S, Rey G, Bhopal RS, Regidor E, et al. All-cause and cause-specific mortality of different migrant populations in Europe. Eur J Epidemiol. 2016;31(7):655–65. Available from: http://link.springer.com/10.1007/s10654-015-0083-9.
de Brún T, De-Brún MO, van Weel-Baumgarten E, van Weel C, Dowrick C, Lionis C, et al. Guidelines and training initiatives that support communication in cross-cultural primary-care settings: appraising their implementability using Normalization Process Theory. Fam Pract. 2015;cmv022. Available from: https://academic.oup.com/fampra/article-lookup/doi/10.1093/fampra/cmv022.
García-Medrano S, Panhofer H. Improving migrant well-being: spontaneous movement as a way to increase the creativity, spontaneity and welfare of migrants in Glasgow. Body Mov Danc Psychother. 2020;15(3):189–203. Available from: https://www.tandfonline.com/doi/full/10.1080/17432979.2020.1767208.
Jamil NA, Gray SR, Fraser WD, Fielding S, Macdonald HM. The relationship between vitamin D status and muscle strength in young healthy adults from sunny climate countries currently living in the northeast of Scotland. Osteoporos Int. 2017;28(4):1433–43. Available from: http://link.springer.com/10.1007/s00198-016-3901-3.
Kaneoka M, Spence W. The cultural context of sexual and reproductive health support: an exploration of sexual and reproductive health literacy among female Asylum Seekers and Refugees in Glasgow. Int J Migr Heal Soc Care. 2019;16(1):46–64. Available from: https://www.emerald.com/insight/content/doi/10.1108/IJMHSC-01-2019-0002/full/html.
O’Donnell CA, Higgins M, Chauhan R, Mullen K. They think we’re OK and we know we’re not. A qualitative study of asylum seekers’ access, knowledge and views to health care in the UK. BMC Health Serv Res. 2007;7(1):75. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-7-75.
Cooper M, Harding S, Mullen K, O’Donnell C. ‘A chronic disease is a disease which keeps coming back … it is like the flu’: chronic disease risk perception and explanatory models among French- and Swahili-speaking African migrants. Ethn Health. 2012;17(6):597–613. Available from: http://www.tandfonline.com/doi/abs/10.1080/13557858.2012.740003.
Ezika EA. An exploration of smoking behavior of african male immigrants living in glasgow. Tob Use Insights. 2014;7:TUI .S13262. Available from: http://journals.sagepub.com/doi/10.4137/TUI.S13262.
Karadzhov D, White R. Between the whispers of the devil and the revelation of the word : christian clergy’s mental health literacy and pastoral support for BME congregants. J Spiritual Ment Heal. 2020;22(2):147–72. Available from: https://www.tandfonline.com/doi/full/10.1080/19349637.2018.1537755).
Yakubu BD, Simkhada P, van Teijlingen E, Eboh W. Sexual health information and uptake of sexual health services by African women in Scotland: a pilot study. Int J Heal Promot Educ. 2010;48(3):79–84. Available from: http://www.tandfonline.com/doi/abs/10.1080/14635240.2010.10708186.
Goff J, Kay K, Lima M, Shallangwa S, We All Have A. Different Consciousness About It: Exploring the Sexual Health Needs of People From African Communities in Scotland. 2021. Available from: https://www.waverleycare.org/wp-content/uploads/2023/05/We_All_Have_Different_Consciousness_About_It_Report.pdf.
Bielecki K, Craig J, Willocks LJ, Pollock KG, Gorman DR. Impact of an influenza information pamphlet on vaccination uptake among Polish pupils in Edinburgh, Scotland and the role of social media in parental decision making. BMC Public Health. 2020;20(1):1381. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09481-z.
Gorman DR, Bielecki K, Willocks LJ, Pollock KG. A qualitative study of vaccination behaviour amongst female Polish migrants in Edinburgh, Scotland. Vaccine. 2019;37(20):2741–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X19304220.
Bak-Klimek A, Karatzias T, Elliott L, MacLean R. The determinants of well-being among polish economic immigrants. Testing the sustainable happiness model in migrant population. J Happiness Stud. 2018;19(6):1565–88. Available from: http://link.springer.com/10.1007/s10902-017-9877-7.
Cheung NF. The cultural and social meanings of childbearing for Chinese and Scottish women in Scotland. Midwifery. 2002;18(4):279–95. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613802903281.
Papadaki A, Scott J. The impact on eating habits of temporary translocation from a Mediterranean to a Northern European environment. Eur J Clin Nutr. 2002;56(5):455–61. Available from: https://www.nature.com/articles/1601337.
McCann A, Mackie P. Improving the Health of Migrants to Scotland: An update for Scottish Directors of Public Health. 2016. Available from: https://www.scotphn.net/wp-content/uploads/2016/04/2016_03_23-Migrant-Health-Report-FINAL-1.pdf.
Ahmed A, Cameron S, Dickson C, Mountain K. Arabic-speaking students’ primary care experiences in Scotland. Community Pract J Community Pract Heal Visit Assoc. 2010;83(2):23–6.
Bray J, Gorman D, Dundas K, Sim J. Obstetric care of New European migrants in Scotland: an audit of antenatal care, obstetric outcomes and communication. Scott Med J. 2010;55(3):26–31. Available from: (http://journals.sagepub.com/doi/10.1258/rsmsmj.55.3.26.
Cheung NF. Choice and control as experienced by Chinese and Scottish childbearing women in Scotland. Midwifery. 2002;18(3):200–13. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613802903153.
Spence W, Zhu L. Perceptions of smoking cessation among Glasgow’s Chinese community. Tob Prev Cessat. 2017;3(October). Available from: http://www.journalssystem.com/tpc/Perceptions-of-smoking-cessation-among-Glasgow-s-Chinese-community,77942,0,2.html.
Gorman DR, Katikireddi SV, Morris C, Chalmers JWT, Sim J, Szamotulska K, et al. Ethnic variation in maternity care: a comparison of Polish and Scottish women delivering in Scotland 2004–2009. Public Health. 2014;128(3):262–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350613003910.
Gorman DR, Porteous LA. Influences on Polish migrants’ breast screening uptake in Lothian, Scotland. Public Health. 2018;158:86–92. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350617304018.
Hogg R, de Kok B, Netto G, Hanley J, Haycock-Stuart E. Supporting Pakistani and Chinese families with young children: perspectives of mothers and health visitors. Child Care Health Dev. 2015;41(3):416–23. Available from: https://onlinelibrary.wiley.com/doi/10.1111/cch.12154.
Kearns A, Whitley E. Health, Wellbeing and Social Inclusion of Migrants in North Glasgow. 2010. Available from: https://www.gowellonline.com/assets/0000/0521/Health_Wellbeing_and_Social_Inclusion_of_Migrants_in_North_Glasgow.pdf.
Poole L, Adamson K. Report on the Situation of the Roma Community in Govanhill, Glasgow. 2008. Available from: https://www.bemis.org.uk/resources/gt/scotland/reportonthesituationoftheromacommunityingovanhill,Glasgow.pdf.
Schofield L, Walsh D, Feng Z, Buchanan D, Dibben C, Fischbacher C, et al. Does ethnic diversity explain intra-UK variation in mortality? A longitudinal cohort study. BMJ Open. 2019;9(3):e024563. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2018-024563.
Unger HW, McCallum AD, Ukachukwu V, McGoldrick C, Perrow K, Latin G, et al. Imported malaria in Scotland – an overview of surveillance, reporting and trends. Travel Med Infect Dis. 2011;9(6):289–97. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1477893911001074.
Young I, Flowers P, McDaid LM. Barriers to uptake and use of pre-exposure prophylaxis (PrEP) among communities most affected by HIV in the UK: findings from a qualitative study in Scotland. BMJ Open. 2014;4(11):e005717. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2014-005717.
Young I, Flowers P, McDaid LM. Key factors in the acceptability of treatment as prevention (TasP) in Scotland: a qualitative study with communities affected by HIV. Sex Transm Infect. 2015;91(4):269–74. Available from: https://sti.bmj.com/lookup/doi/10.1136/sextrans-2014-051711.
Bhopal R, Cm FI, Teiner SM, Halmers CJ, Ovey PC, Amieson J. Ethnicity and health in Scotland: Can we fill the information gap ? A demonstration project focusing on coronary heart disease and linkage of census and health records. Ethics. 2005. Available from: http://www.cphs.mvm.ed.ac.uk/docs/Retrocodingfinalreport.pdf.
Cezard GI, Bhopal RS, Ward HJT, Bansal N, Bhala N. Ethnic variations in upper gastrointestinal hospitalizations and deaths: the Scottish Health and Ethnicity Linkage Study. Eur J Public Health. 2016;26(2):254–60. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckv182.
Christie-de Jong F, Kotzur M, Amiri R, Ling J, Mooney JD, Robb KA. Qualitative evaluation of a codesigned faith-based intervention for muslim women in Scotland to encourage uptake of breast, colorectal and cervical cancer screening. BMJ Open. 2022;12(5):e058739. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-058739.
Cree VE, Sidhva D. Children and HIV in Scotland: findings from a cross-sector needs assessment of children and young people infected and affected by HIV in Scotland. Br J Soc Work. 2011;41(8):1586–603. Available from: https://academic.oup.com/bjsw/article-lookup/doi/10.1093/bjsw/bcr036.
Gallimore A, Irshad T, Cooper M, Cameron S. Influence of culture, religion and experience on the decision of Pakistani women in Lothian, Scotland to use postnatal contraception: a qualitative study. BMJ Sex Reprod Heal. 2021;47(1):43–8. Available from: https://jfprhc.bmj.com/lookup/doi/10.1136/bmjsrh-2019-200497.
Gruer LD, Cézard GI, Wallace LA, Hutchinson SJ, Douglas AF, Buchanan D, et al. Complex differences in infection rates between ethnic groups in Scotland: a retrospective, national census-linked cohort study of 1.65 million cases. J Public Health (Bangkok). 2022;44(1):60–9. Available from: https://academic.oup.com/jpubhealth/article/44/1/60/6106111.
Bhala N, Cézard G, Ward HJT, Bansal N, Bhopal R. Ethnic variations in liver- and alcohol-related disease hospitalisations and mortality: the Scottish health and ethnicity linkage study. Alcohol Alcohol. 2016;51(5):593–601. Available from: https://academic.oup.com/alcalc/article-lookup/doi/10.1093/alcalc/agw018.
Pollock KG, McDonald E, Smith-Palmer A, Johnston F, Ahmed S. Tuberculosis in healthcare workers, Scotland. Scott Med J. 2017;62(3):101–3. Available from: http://journals.sagepub.com/doi/10.1177/0036933017727963.
Gruer LD, Millard AD, Williams LJ, Bhopal RS, Katikireddi SV, Cézard GI, et al. Differences in all-cause hospitalisation by ethnic group: a data linkage cohort study of 4.62 million people in Scotland, 2001–2013. Public Health. 2018;161:5–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350618301501.
Jackson C, Bedford H, Cheater FM, Condon L, Emslie C, Ireland L, et al. Needles, Jabs and Jags: a qualitative exploration of barriers and facilitators to child and adult immunisation uptake among Gypsies, Travellers and Roma. BMC Public Health. 2017;17(1):254. Available from: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4178-y.
John JR, Curry G, Cunningham-Burley S. Exploring ethnic minority women’s experiences of maternity care during the SARS-CoV-2 pandemic: a qualitative study. BMJ Open. 2021;11(9):e050666. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-050666.
Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. Diabetes service provision: a qualitative study of the experiences and views of Pakistani and Indian patients with Type 2 diabetes. Diabet Med. 2006;23(9):1003–7. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1464-5491.2006.01922.x.
Livingston MR, Shaw LE, Codere G, Goldberg DJ. Human immunodeficiency virus acquired heterosexually abroad: expert panel assessment of the indigenous/nonindigenous to the united kingdom status of cases. J Travel Med. 2006;12(1):19–25. Available from: https://academic.oup.com/jtm/article-lookup/doi/10.2310/7060.2005.00005.
Nelson M, Patton A, Robb K, Weller D, Sheikh A, Ragupathy K, et al. Experiences of cervical screening participation and non-participation in women from minority ethnic populations in Scotland. Heal Expect. 2021;24(4):1459–72. Available from: https://onlinelibrary.wiley.com/doi/10.1111/hex.13287.
Noble G, Okpo E, Tonna I, Fielding S. Factors associated with late HIV diagnosis in North-East Scotland: a six-year retrospective study. Public Health. 2016;139:36–43. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350616301020.
Gillespie M. Trapped: Destitution and Asylum in Scotland. 2012. Available from: http://www.rst.org.uk/wp-content/uploads/2012/11/Trapped-destitution-and-asylum-summary-final-compressed-pictures.pdf.
Hopkins P, Hill M. The needs and strengths of unaccompanied asylum-seeking children and young people in Scotland. Child Fam Soc Work. 2010;15(4):399–408. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2206.2010.00687.x.
Marsden R, Harris C. “We started life again”: Integration experiences of refugee families reuniting in Glasgow. 2015. Available from: https://www.refworld.org/docid/560cde294.html.
Martzoukou K, Burnett S. Exploring the everyday life information needs and the socio-cultural adaptation barriers of Syrian refugees in Scotland. J Doc. 2018;74(5):1104–32. Available from: https://www.emerald.com/insight/content/doi/10.1108/JD-10-2017-0142/full/html.
McKenna R. From pillar to post: Destitution among people refused asylum in Scotland. 2019; Available from: https://www.rst.org.uk/wp-content/uploads/2019/03/From-Pillar-to-Post-Feb-2019.pdf.
Independent Commission of Inquiry. Failings in the provision of care to New Scots during the Covid pandemic: Part 2. 2022. Available from: https://static1.squarespace.com/static/62af1289a666c80e00b17253/t/636b9190408f81778746eaa7/1667994032702/AIS+Phase+2+Report+Full.pdf.
Trevena P, Gawlewicz A, Wright S. Addressing the needs of Scotland’s migrant and minority ethnic populations under Covid-19: lessons for the future. 2022. Available from: https://migrantessentialworkers.com/wp-content/uploads/2022/11/SC-Migrant-C19-Innovations.pdf.
Oduntan O, Ruthven I. The information needs matrix: a navigational guide for refugee integration. Inf Process Manag. 2019;56(3):791–808. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0306457318306939.
Sime D, Fox R, Migrant C. Social capital and access to services post-migration: transitions, negotiations and complex agencies. Child Soc. 2015;29(6):524–34. Available from: https://onlinelibrary.wiley.com/doi/10.1111/chso.12092.
Strang A, Baillot H, Mignard E. Insights into integration pathways. New Scots and the Holistic Integration Service. A report drawing on year two of the Holistic Integration Service. 2015. Available from: https://scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Holistic-Integration-Service-Year-2-report.pdf.
Weir KEA, Wilson SJ, Gorman DR. The Syrian vulnerable person resettlement programme: evaluation of Edinburgh’s reception arrangements. J Public Health (Bangkok). 2018;40(3):451–60. Available from: https://academic.oup.com/jpubhealth/article/40/3/451/4600209.
Hammond CN. Scots 2- Engagement analysis of the New Scot Refugee Integration Strategy 2018–2022. 2018. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/research-and-analysis/2018/06/news-scots-2-engagement-analysis-new-scots-refugee-integration-strategy/documents/00537019-pdf/00537019-pdf/govscot%3Adocument/00537019.pdf.
Blake Stevenson. A8 Nationals in Glasgow. 2007. Available from: http://crosshillandgovanhill.org.uk/grindocs/A8NationalsinGlasgow.pdf.
Ajetunmobi O, Whyte B, Chalmers J, Fleming M, Stockton D, Wood R. Informing the ‘early years’ agenda in Scotland: understanding infant feeding patterns using linked datasets. J Epidemiol Community Health. 2014;68(1):83–92. Available from: https://jech.bmj.com/lookup/doi/10.1136/jech-2013-202718.
Laidlaw K, Wang D, Coelho C, Power M. Attitudes to ageing and expectations for filial piety across Chinese and British cultures: a pilot exploratory evaluation. Aging Ment Health. 2010;14(3):283–92. Available from: http://www.tandfonline.com/doi/abs/10.1080/13607860903483060.
Marsden R, Aldegheri E, Khan A, Lowe M, Strang A, Salinas E, et al. “What’s going on?” A study into destitution and poverty faced by asylum seekers and refugees in Scotland. 2005. Available from: http://www.rst.org.uk/wp-content/uploads/2012/11/Whats_going_on_A_study.pdf.
Quinn N. Participatory action research with asylum seekers and refugees experiencing stigma and discrimination: the experience from Scotland. Disabil Soc. 2014;29(1):58–70. Available from: http://www.tandfonline.com/doi/abs/10.1080/09687599.2013.769863.
British Red Cross, Refugee Survival Trust. How will we survive? Steps to preventing destitution in the asylum system. 2021. Available from: https://mcusercontent.com/c17c136fc126588cb51e5471d/files/a35dd0e1-d785-f962-6a41-01e928493775/DASS_Research_Report_2021.pdf.
O’Donnell R, Angus K, McCulloch P, Amos A, Greaves L, Semple S. Fathers’ views and experiences of creating a smoke-free home: a scoping review. Int J Environ Res Public Health. 2019;16(24):5164. Available from: https://www.mdpi.com/1660-4601/16/24/5164.
Sweileh WM, Wickramage K, Pottie K, Hui C, Roberts B, Sawalha AF, et al. Bibliometric analysis of global migration health research in peer-reviewed literature (2000–2016). BMC Public Health. 2018;18(1):777. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5689-x.
Wren K. Supporting asylum seekers and refugees in glasgow: the role of multi-agency networks. J Refug Stud. 2007;20(3):391–413. Available from: https://academic.oup.com/jrs/article-lookup/doi/10.1093/jrs/fem006.
UK Government Home Office. A Fairer Asylum Accommodation System. 2022. Available from: https://www.emcouncils.gov.uk/write/Migration/Asylum_Dispersal_Factsheet_PDF.pdf.
Scottish Refugee Council. Scotland’s Welcome: an analysis of community support for refugee integration. 2020. Available from https://scottishrefugeecouncil.org.uk/wp-content/uploads/2021/01/Community-support-analysis-2020.pdf.
Sturge G, UK Parliament House of Commons Library Asylum statistics Research Briefing. 2023. Available from: https://commonslibrary.parliament.uk/research-briefings/sn01403/#:~:text=IntheyearendingJune,ofimmigrantstotheUK.
The Migration Observatory. Where do migrants live in the UK? The Migration Observatory at the University of Oxford. 2022. Available from: https://migrationobservatory.ox.ac.uk/resources/briefings/where-do-migrants-live-in-the-uk.
Pavli A, Maltezou H. Health problems of newly arrived migrants and refugees in Europe. J Travel Med. 2017;24(4). Available from: http://academic.oup.com/jtm/article/doi/10.1093/jtm/tax016/3095987/Health-problems-of-newly-arrived-migrants-and.
Humphris R, Bradby H. Health Status of Refugees and Asylum Seekers in Europe. In: Oxford Research Encyclopedia of Global Public Health. Oxford University Press; 2017. Available from: https://oxfordre.com/publichealth/view/10.1093/acrefore/9780190632366.001.0001/acrefore-9780190632366-e-8.
Bradby H, Humphris R, Newall D, Phillimore J. Public Health Aspects of Migrant Health: A Review of the Evidence on Health Status for Refugees and Asylum Seekers in the European Region. (Health Evidence Network Synthesis Report, No. 44.) ANNEX 2, DEFINITIONS OF REFUGEES, ASYLUM SEEKERS AND MIGRANTS IN THE LITERATURE. Copenhagen: Eerat; 2015. Available from: https://www.ncbi.nlm.nih.gov/books/NBK379415/.
Gerritsen AAM, Bramsen I, Devillé W, van Willigen LHM, Hovens JE, van der Ploeg HM. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2006;41(1):18–26. Available from: http://link.springer.com/10.1007/s00127-005-0003-5.
Laue J, Diaz E, Eriksen L, Risør T. Migration health research in Norway: a scoping review. Scand J Public Health. 2023;51(3):381–90. Available from: http://journals.sagepub.com/doi/10.1177/14034948211032494.
Scottish Refugee Council. Ukraine response one year on. 2023. Available from: https://scottishrefugeecouncil.org.uk/ukraine-response-one-year-on/. Cited 2023 Aug 26.
Woodward A, Howard N, Wolffers I. Health and access to care for undocumented migrants living in the European Union: a scoping review. Health Policy Plan. 2014;29(7):818–30. Available from: https://academic.oup.com/heapol/article-lookup/doi/10.1093/heapol/czt061.
Simon J, Kiss N, Laszewska A, Mayer S. Public health aspects of migrant health: a review of the evidence on health status for labour migrants in the European Region. Health Evidence Network Synthesis Report 43. 2015. Available from: http://www.epgencms.europarl.europa.eu/cmsdata/upload/114f16b6-1667-44ab-802b-a5a83dd50af0/WHO-HEN-Report-A5-1-Labour-FINAL_EN.pdf.
Scottish Government. Seasonal migrant workers in Scottish agriculture: research report. 2023. Available from: https://www.gov.scot/publications/seasonal-migrant-workers-scottish-agriculture/pages/10/.
Scottish Government. New Scots: refugee integration strategy 2018–2022. 2018. Available from: https://www.gov.scot/publications/new-scots-refugee-integration-strategy-2018-2022/pages/11/.
Oliva A, Palavra V, Caloun J. Refugees in Scotland: understanding the policy domain. 2016. Available from: https://www.academia.edu/34097718/REFUGEES_IN_SCOTLAND_UNDERSTANDING_THE_POLICY_DOMAIN.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. Available from: https://www.acpjournals.org/doi/10.7326/M18-0850.
Acknowledgements
Thank-you to Professor Anne MacFarlane and PHD student Anne Cronin, of the University of Limerick, Ireland for sharing the coding guidelines currently used in an update to Villarroel et. al’s 2019 study on Migrant Health in the Republic of Ireland.
Funding
No funding was received for this work, which was undertaken as G. Petrie’s Master of Public Health dissertation module at the University of Stirling.
Author information
Authors and Affiliations
Contributions
KA, RO and GP finalised the study design collectively. GP conducted the searches, analysis and write up, with support from KA and RO. All three authors read and approved the manuscript prior to submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Petrie, G., Angus, K. & O’Donnell, R. A scoping review of academic and grey literature on migrant health research conducted in Scotland. BMC Public Health 24, 1156 (2024). https://doi.org/10.1186/s12889-024-18628-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18628-1